Differences in Diagnosis and Management of Hypertensive Urgencies and Emergencies According to Italian Doctors from Different Departments Who Deal With Acute Increase in Blood Pressure—Data from Gear (Gestione Dell’emergenza e Urgenza in ARea Critica) Study
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
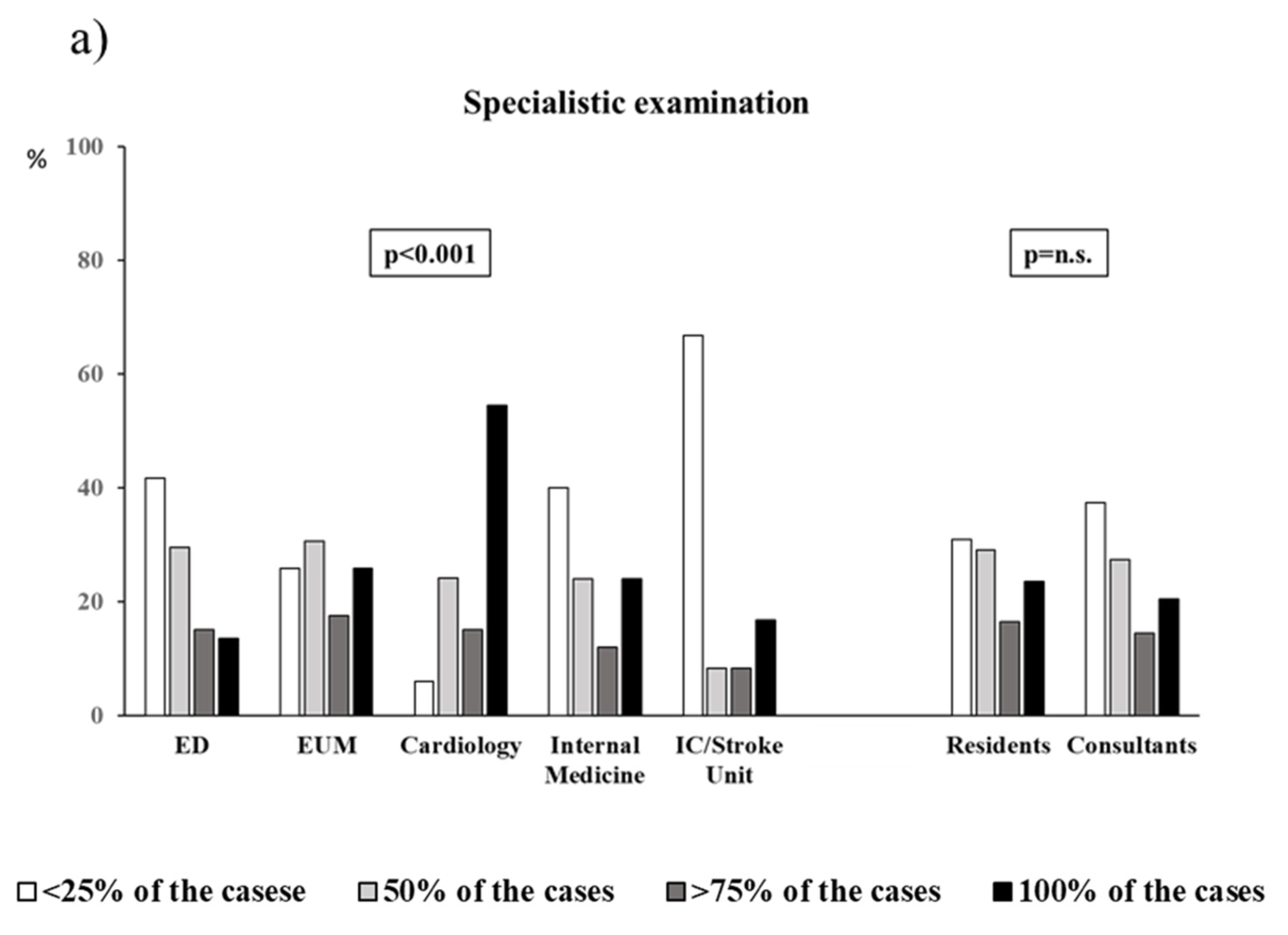
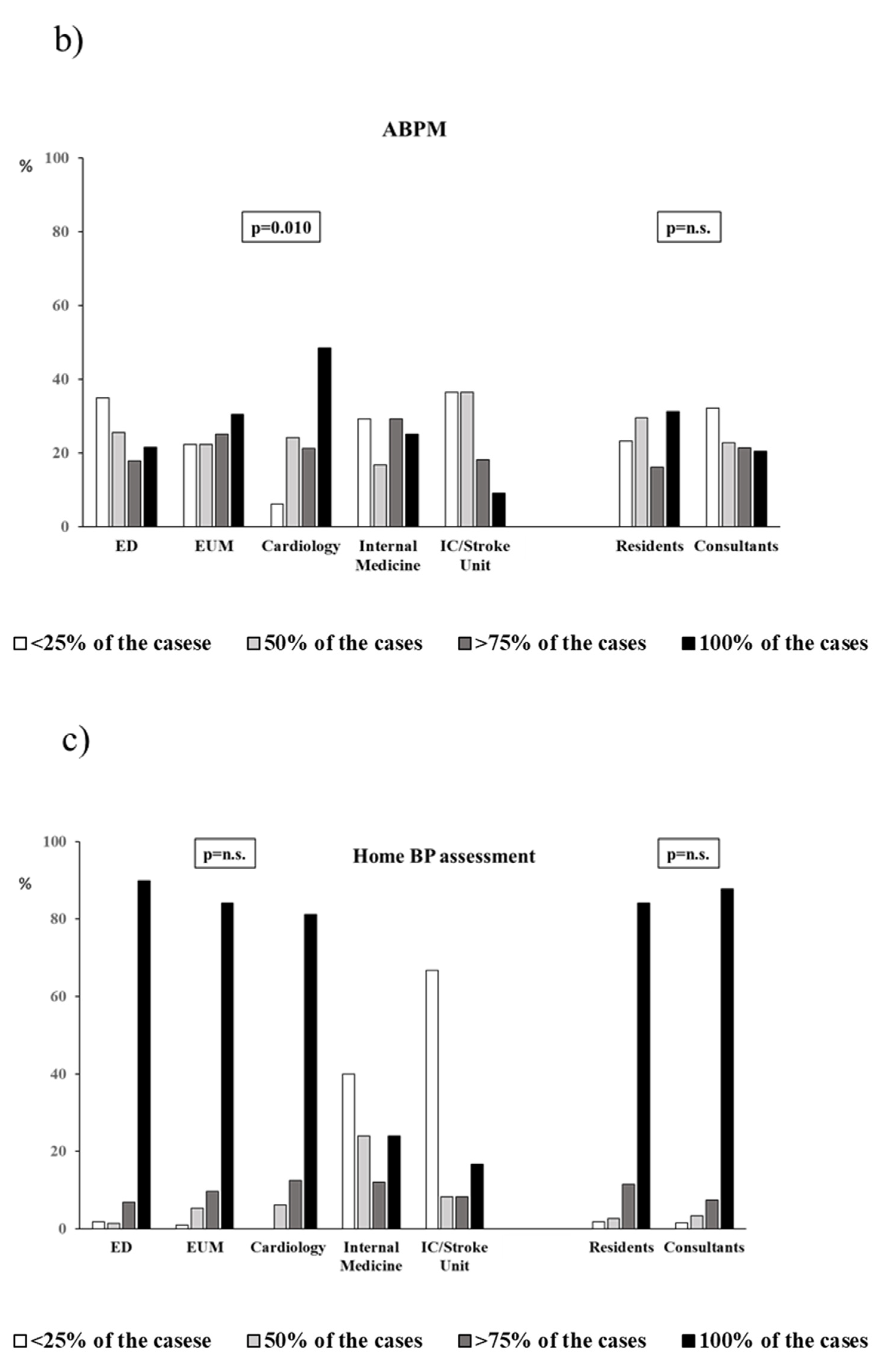
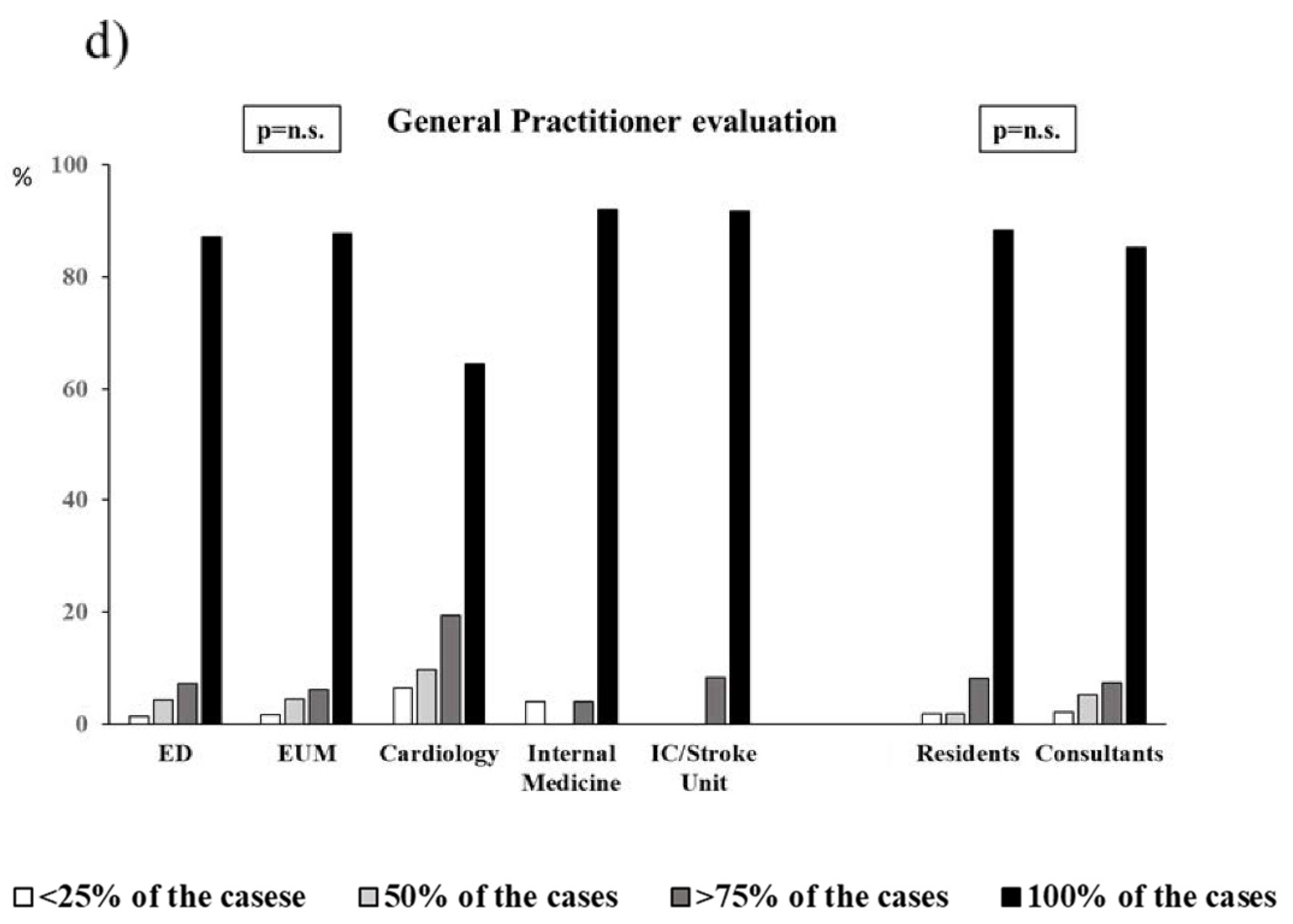
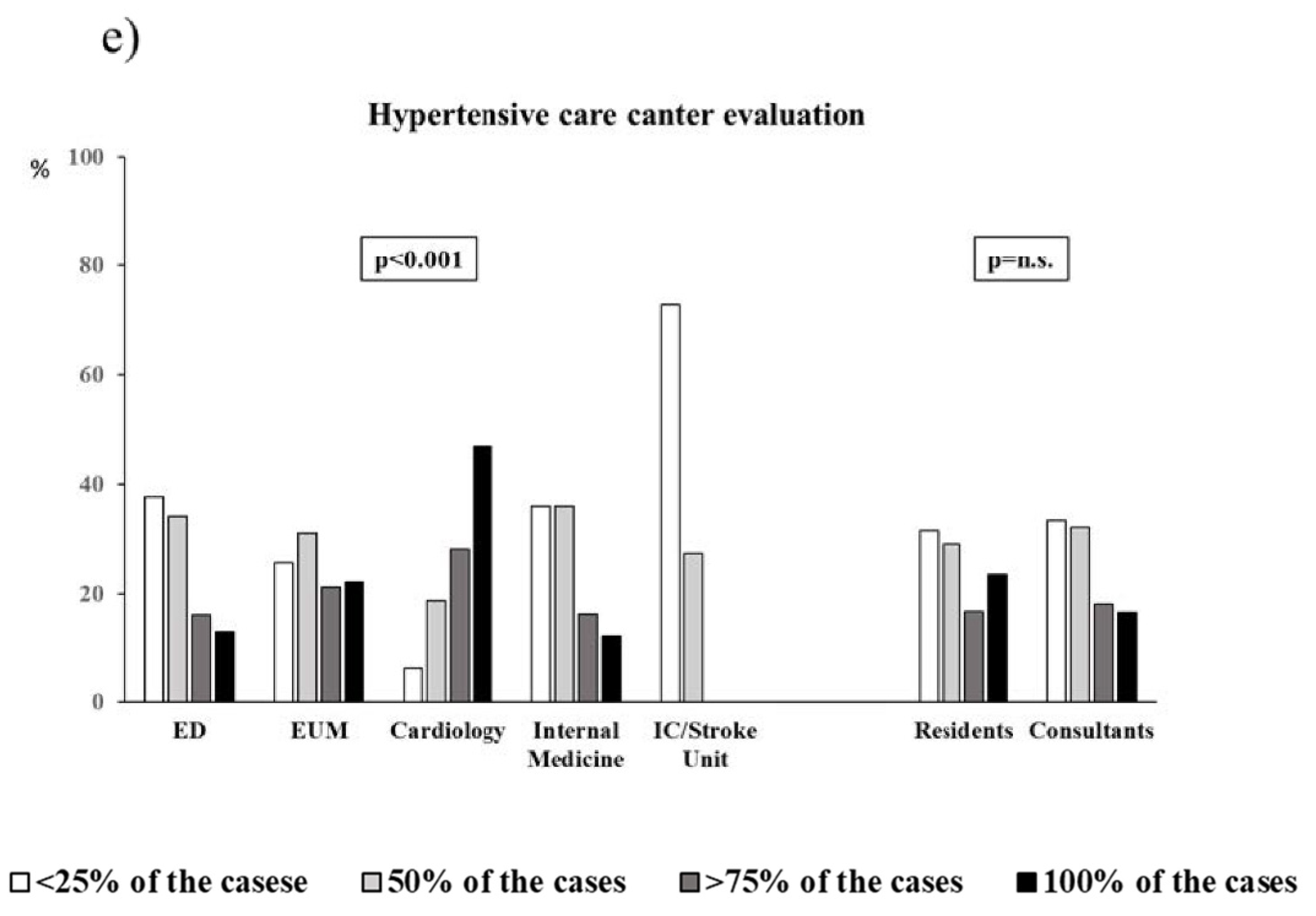
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Gore, J.M.; Amin, A.; Anderson, F.A.; Dasta, J.F.; Ferguson, J.J.; Kleinschmidt, K.; Mayer, S.A.; Multz, A.S.; Peacock, W.F.; et al. Practice patterns, outcomes, and end-organ dysfunction for patients with acute severe hypertension: The Studying the Treatment of Acute hyperTension (STAT) registry. Am. Heart J. 2009, 158, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics—2018 Update: A Report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D.P.; Sanidas, E.A.; Viniou, N.A.; Gennimata, V.; Chantziara, V.; Barbetseas, I.; Makris, T.K. Cardiovascular hypertensive emergencies. Curr. Hypertens. Rep. 2015, 17, 5. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- Van den Born, B.H.; Lip, G.Y.H.; Brguljan-Hitij, J.; Cremer, A.; Segura, J.; Morales, E.; Mahfoud, F.; Amraoui, F.; Persu, A.; Kahan, T.; et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Heart J. Cardiovasc. Pharmacother. 2019, 5, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [Green Version]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Muiesan, M.L.; Salvetti, M.; Amadoro, V.; Di Somma, S.; Perlini, S.; Semplicini, A.; Borghi, C.; Volpe, M.; Saba, P.S.; Cameli, M.; et al. An update on hypertensive emergencies and urgencies. J. Cardiovasc. Med. 2015, 16, 372–382. [Google Scholar] [CrossRef] [Green Version]
- Perez, M.I.; Musini, V.M. Pharmacological interventions for hypertensive emergencies. Cochrane Database Syst. Rev. 2008, 2008, CD003653. [Google Scholar] [CrossRef]
- Martin, J.F.; Higashiama, E.; Garcia, E.; Luizon, M.R.; Cipullo, J.P. Hypertensive crisis profile. Prevalence and clinical presentation. Arq. Bras. Cardiol. 2004, 83, 125–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zampaglione, B.; Pascale, C.; Marchisio, M.; Cavallo-Perin, P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension 1996, 27, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Vilela-Martin, J.F.; Vaz-de-Melo, R.O.; Kuniyoshi, C.H.; Abdo, A.N.; Yugar-Toledo, J.C. Hypertensive crisis: Clinical-epidemiological profile. Hypertens. Res. 2011, 34, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Pinna, G.; Pascale, C.; Fornengo, P.; Arras, S.; Piras, C.; Panzarasa, P.; Carmosino, G.; Franza, O.; Semeraro, V.; Lenti, S.; et al. Hospital admissions for hypertensive crisis in the emergency departments: A large multicenter Italian study. PLoS ONE 2014, 9, e93542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salvetti, M.; Paini, A.; Colonetti, E.; Tarozzi, L.; Bertacchini, F.; Aggiusti, C.; Stassaldi, D.; Rosei, C.A.; Rosei, E.A.; Muiesan, M.L. Hypertensive emergencies and urgencies: A single-centre experience in Northern Italy 2008–2015. J. Hypertens. 2020, 38, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Saladini, F.; Mancusi, C.; Bertacchini, F.; Spannella, F.; Maloberti, A.; Giavarini, A.; Rosticci, M.; Bruno, R.M.; Pucci, G.; Grassi, D.; et al. Diagnosis and treatment of hypertensive emergencies and urgencies among Italian emergency and intensive care departments. Results from an Italian survey: Progetto GEAR (Gestione dell’Emergenza e urgenza in ARea critica). Eur. J. Intern. Med. 2020, 71, 50–56. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef] [Green Version]
- Mancusi, C.; Carlino, M.V.; Sforza, A. Point-of-care ultrasound with pocket-size devices in emergency department. Echocardiography 2019, 36, 1755–1764. [Google Scholar] [CrossRef]
- Picano, E.; Pellikka, P.A. Ultrasound of extravascular lung water: A new standard for pulmonary congestion. Eur. Heart J. 2016, 37, 2097–2104. [Google Scholar] [CrossRef] [Green Version]
- Sicari, R.; Galderisi, M.; Voigt, J.U.; Habib, G.; Zamorano, J.L.; Lancellotti, P.; Badano, L.P. The use of pocket-size imaging devices: A position statement of the European Association of Echocardiography. Eur. J. Echocardiogr. 2011, 12, 85–87. [Google Scholar] [CrossRef] [Green Version]
- Burton, T.J.; Wilkinson, I.B. The dangers of immediate-release nifedipine in the emergency treatment of hypertension. J. Hum. Hypertens. 2008, 22, 301–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, D.W.; Deming, D.D.; Hamada, N.; Perkin, R.M.; Sahney, S. Evaluation of the safety of short-acting nifedipine in children with hypertension. Pediatr. Nephrol. 2002, 17, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, Y.; Shimada, T.; Yoshitomi, H.; Sano, K.; Oyake, N.; Umeno, T.; Sakane, T.; Murakami, Y.; Morioka, S. Sublingual nifedipine in elderly patients: Even a low dose induces myocardial ischaemia. Clin. Exp. Pharmacol. Physiol. 1999, 26, 404–410. [Google Scholar] [CrossRef]
- Gemici, K.; Baran, I.; Bakar, M.; Demircan, C.; Ozdemir, B.; Cordan, J. Evaluation of the effect of the sublingually administered nifedipine and captopril via transcranial doppler ultrasonography during hypertensive crisis. Blood Press. 2003, 12, 46–48. [Google Scholar] [PubMed]
- Rubio-Guerra, A.F.; Vargas-Ayala, G.; Lozano-Nuevo, J.J.; Narvaez-Rivera, J.L.; Rodriguez-Lopez, L. Comparison between isosorbide dinitrate aerosol and nifedipine in the treatment of hypertensive emergencies. J. Hum. Hypertens. 1999, 13, 473–476. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Liu, Y. The effect of Nifedipine on postpartum blood loss in patients with pregnancy induced hypertension. Zhonghua Fu Chan Ke Za Zhi 2000, 35, 151–152. [Google Scholar] [PubMed]
- Sánchez, M.; Sobrino, J.; Ribera, L.; Adrián, M.J.; Torres, M.; Coca, A. Long-acting lacidipine versus short-acting nifedipine in the treatment of asymptomatic acute blood pressure increase. J. Cardiovasc. Pharmacol. 1999, 33, 479–484. [Google Scholar] [CrossRef]
- Fami, M.J.; Ho, N.T.; Mason, C.M. Another report of adverse reactions to immediate-release nifedipine. Pharmacotherapy 1998, 18, 1133–1135. [Google Scholar] [PubMed]
- Grossman, E.; Messerli, F.H.; Grodzicki, T.; Kowey, P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA 1996, 276, 1328–1331. [Google Scholar] [CrossRef] [PubMed]
- Funder, J.W.; Carey, R.M.; Mantero, F.; Murad, M.H.; Reincke, M.; Shibata, H.; Stowasser, M.; Young, W.F., Jr. The management of primary aldosteronism: Case detection, diagnosis, and treatment: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2016, 101, 1889–1916. [Google Scholar] [CrossRef]
- Stowasser, M.; Ahmed, A.H.; Pimenta, E.; Taylor, P.J.; Gordon, R.D. Factors affecting the aldosterone/renin ratio. Horm. Metab. Res. 2012, 44, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.K.; Young, L.; Howell, E.H.; Hu, B.; Rutecki, G.; Thomas, G.; Rothberg, M.B. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern. Med. 2016, 176, 981–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Correct Definition | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| HU, % | 76.7 | 81.4 | 82.8 | 89.5 | 88.5 | n.s. | 83.2 | 80.4 | n.s. |
| HE, % | 91.8 | 88.2 | 84.5 | 97.4 | 92.3 | n.s. | 92.5 | 88.2 | n.s. |
| Use of anti-anxiety drugs | 37.7 | 34.8 | 34.5 | 34.3 | 26.9 | n.s. | 36.8 | 34.4 | n.s. |
| Investigation of | |||||||||
| Illegal drugs, % | 95.9 | 98.5 | 93.1 | 97.4 | 100 | n.s. | 97.7 | 97.4 | n.s. |
| COX-1, % | 45.9 | 45.1 | 44.8 | 47.4 | 50 | n.s. | 45.6 | 45.3 | n.s. |
| COX-2, % | 47.3 | 43.1 | 43.1 | 44.7 | 38.5 | n.s. | 46.8 | 43.2 | n.s. |
| Steroids, % | 80.8 | 82.1 | 89.6 | 78.9 | 76.9 | n.s. | 84.8 | 81.6 | n.s. |
| Techinque | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke Unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| One sigle detection | 16.4 | 22.9 | 22.4 | 15.8 | 34.6 | 0.004 | 23.4 | 20.7 | n.s. |
| Two detection within 1–3 min | 34.2 | 34.5 | 37.9 | 26.3 | 26.9 | 0.004 | 33.9 | 34.4 | n.s. |
| Several detections in both arms | 45.9 | 37.8 | 37.9 | 47.4 | 30.8 | 0.004 | 35.7 | 40.8 | n.s. |
| Unattended office BP | 2.0 | 3.5 | 0 | 2.6 | 0 | 0.004 | 2.3 | 3.0 | n.s. |
| Several detection or invasive (intra-arterial) detection | 0 | 1.2 | 1.7 | 2.6 | 7.7 | 0.004 | 3.5 | 0.6 | n.s. |
| It depends according to the different patient | 1.4 | 0 | 0 | 5.3 | 0 | 0.004 | 1.2 | 0.4 | n.s. |
| Type of Cuff | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke Unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| Small, % | 62.3 | 57.9 | 34.5 | 63.1 | 53.8 | 0.020 | 59.6 | 56.0 | n.s. |
| Standard, % | 92.5 | 94.5 | 93.1 | 92.1 | 100 | n.s. | 94.7 | 93.6 | n.s. |
| Large, % | 76.7 | 77.3 | 55.2 | 78.9 | 84.6 | 0.021 | 81.9 | 73.3 | n.s. |
| Extra large, % | 31.5 | 41.6 | 27.6 | 44.7 | 46.1 | n.s. | 32.7 | 40.4 | n.s. |
| Universal, % | 26.7 | 31.5 | 36.2 | 26.3 | 30.8 | n.s. | 28.6 | 31.6 | n.s. |
| Sign/Symptom | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke Unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| Epistaxis, % | 32.2 | 33.2 | 55.2 | 29.0 | 26.9 | 0.012 | 34.5 | 34.2 | n.s. |
| Visual disturbances, % | 90.4 | 88.9 | 93.1 | 84.2 | 100 | n.s. | 93.6 | 88.5 | 0.05 |
| Tinnitus, % | 41.8 | 35.0 | 50.0 | 42.1 | 34.6 | n.s. | 43.3 | 37.4 | n.s. |
| Dyspnea, % | 84.2 | 84.1 | 67.2 | 78.9 | 92.3 | 0.014 | 79.5 | 83.1 | n.s. |
| Headache, % | 84.2 | 80.6 | 86.2 | 86.8 | 76.9 | n.s. | 81.9 | 82.3 | n.s. |
| Conjunctival haemorrhages, % | 41.1 | 38.5 | 70.7 | 39.5 | 26.9 | <0.001 | 47.4 | 39.5 | n.s. |
| Dizziness, % | 53.4 | 50.9 | 60.3 | 47.4 | 50 | n.s. | 49.7 | 52.6 | n.s. |
| Chest pain, % | 91.1 | 91.2 | 72.4 | 84.2 | 88.5 | 0.001 | 87.7 | 89.3 | n.s. |
| Test | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke Unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| Fundoscopy, % | 22.6 | 25.4 | 48.3 | 28.9 | 30.8 | 0.006 | 31.0 | 26.9 | n.s. |
| TTE, % | 63.7 | 65.7 | 67.2 | 52.6 | 76.9 | n.s. | 66.7 | 64.5 | n.s. |
| Renal function (creatinine), % | 93.1 | 91.2 | 91.4 | 89.5 | 88.5 | n.s. | 93.0 | 91.2 | n.s. |
| Urinary protein, % | 50.0 | 54.2 | 63.8 | 52.6 | 73.1 | n.s. | 56.1 | 56.0 | n.s. |
| Brain CT scan, % | 66.4 | 56.7 | 39.6 | 50.0 | 61.5 | n.s. | 53.2 | 58.5 | n.s. |
| BNP/NT-pro-BNP, % | 42.5 | 34.3 | 31.0 | 36.8 | 42.3 | n.s. | 38.0 | 36.5 | n.s. |
| Markers of cardiomyocyte necrosis, % | 67.1 | 66.2 | 63.8 | 63.2 | 69.2 | n.s. | 70.1 | 65.6 | n.s. |
| Chest radiography, % | 54.8 | 49.9 | 24.1 | 68.4 | 73.1 | 0.001 | 51.5 | 50.2 | n.s. |
| ECG, % | 97.9 | 97.7 | 93.1 | 92.1 | 100 | n.s. | 97.4 | 97.1 | n.s. |
| Lung ultrasound, % | 33.6 | 43.8 | 17.2 | 36.8 | 50.0 | 0.004 | 35.1 | 41.0 | n.s. |
| Drugs | EUM n = 146 | ED n = 397 | Cardiology n = 58 | Internal Medicine n = 38 | IC or Stroke Unit n = 26 | p | Residents n = 174 | Consultants n = 491 | p |
|---|---|---|---|---|---|---|---|---|---|
| i.v. Sodium Nitroprusside, % | 16.4 | 19.1 | 31.0 | 15.8 | 19.2 | 0.05 | 18.1 | 19.9 | n.s. |
| i.v. Nitroglycerine, % | 79.4 | 79.1 | 74.1 | 78.9 | 88.5 | n.s. | 80.1 | 78.6 | n.s. |
| i.v. Labetalol, % | 67.8 | 66.5 | 39.6 | 73.7 | 73.1 | 0.003 | 63.7 | 65.0 | n.s. |
| i.v. Urapidil, % | 65.1 | 67.8 | 22.4 | 71.0 | 46.1 | <0.001 | 60.8 | 63.7 | n.s. |
| i.v. or i.m. Clonidine, % | 64.4 | 67.5 | 75.9 | 60.5 | 34.6 | 0.008 | 62.6 | 66.9 | n.s. |
| Oral Captopril, % | 30.8 | 52.6 | 46.5 | 60.5 | 38.5 | <0.001 | 40.3 | 48.9 | 0.05 |
| i.v. Furosemide, % | 65.1 | 54.4 | 79.3 | 57.9 | 61.5 | 0.018 | 65.5 | 58.3 | n.s. |
| s.l. Nifedipine, % | 17.8 | 22.7 | 43.1 | 5.3 | 11.5 | <0.001 | 25.1 | 20.5 | n.s. |
| i.v. Nicardipine, % | 4.8 | 4.0 | 8.6 | 2.6 | 3.8 | n.s. | 7.6 | 3.6 | n.s. |
| i.v. Fenoldopam, % | 2.7 | 6.8 | 10.3 | 2.6 | 3.8 | n.s. | 5.8 | 6.2 | n.s. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saladini, F.; Mancusi, C.; Bertacchini, F.; Spannella, F.; Maloberti, A.; Giavarini, A.; Rosticci, M.; Bruno, R.M.; Pucci, G.; Grassi, D.; et al. Differences in Diagnosis and Management of Hypertensive Urgencies and Emergencies According to Italian Doctors from Different Departments Who Deal With Acute Increase in Blood Pressure—Data from Gear (Gestione Dell’emergenza e Urgenza in ARea Critica) Study. J. Clin. Med. 2022, 11, 2986. https://doi.org/10.3390/jcm11112986
Saladini F, Mancusi C, Bertacchini F, Spannella F, Maloberti A, Giavarini A, Rosticci M, Bruno RM, Pucci G, Grassi D, et al. Differences in Diagnosis and Management of Hypertensive Urgencies and Emergencies According to Italian Doctors from Different Departments Who Deal With Acute Increase in Blood Pressure—Data from Gear (Gestione Dell’emergenza e Urgenza in ARea Critica) Study. Journal of Clinical Medicine. 2022; 11(11):2986. https://doi.org/10.3390/jcm11112986
Chicago/Turabian StyleSaladini, Francesca, Costantino Mancusi, Fabio Bertacchini, Francesco Spannella, Alessandro Maloberti, Alessandra Giavarini, Martina Rosticci, Rosa Maria Bruno, Giacomo Pucci, Davide Grassi, and et al. 2022. "Differences in Diagnosis and Management of Hypertensive Urgencies and Emergencies According to Italian Doctors from Different Departments Who Deal With Acute Increase in Blood Pressure—Data from Gear (Gestione Dell’emergenza e Urgenza in ARea Critica) Study" Journal of Clinical Medicine 11, no. 11: 2986. https://doi.org/10.3390/jcm11112986
APA StyleSaladini, F., Mancusi, C., Bertacchini, F., Spannella, F., Maloberti, A., Giavarini, A., Rosticci, M., Bruno, R. M., Pucci, G., Grassi, D., Pengo, M., & Muiesan, M. L. (2022). Differences in Diagnosis and Management of Hypertensive Urgencies and Emergencies According to Italian Doctors from Different Departments Who Deal With Acute Increase in Blood Pressure—Data from Gear (Gestione Dell’emergenza e Urgenza in ARea Critica) Study. Journal of Clinical Medicine, 11(11), 2986. https://doi.org/10.3390/jcm11112986








