Multi-Modality Imaging for Prevention of Coronary Artery Disease and Myocardial Infarction in the General Population: Ready for Prime Time?
Abstract
:1. Introduction
2. Targets beyond Clinical Risk Factors and Coronary Calcium Burden
3. Coronary Computed Tomography Angiography for Identification of the At-Risk Population
4. Myocardial Perfusion Imaging for Identification of the At-Risk Population
4.1. Myocardial Ischemia
4.2. Unrecognized Myocardial Infarction and Reduced Left Ventricular Ejection Fraction
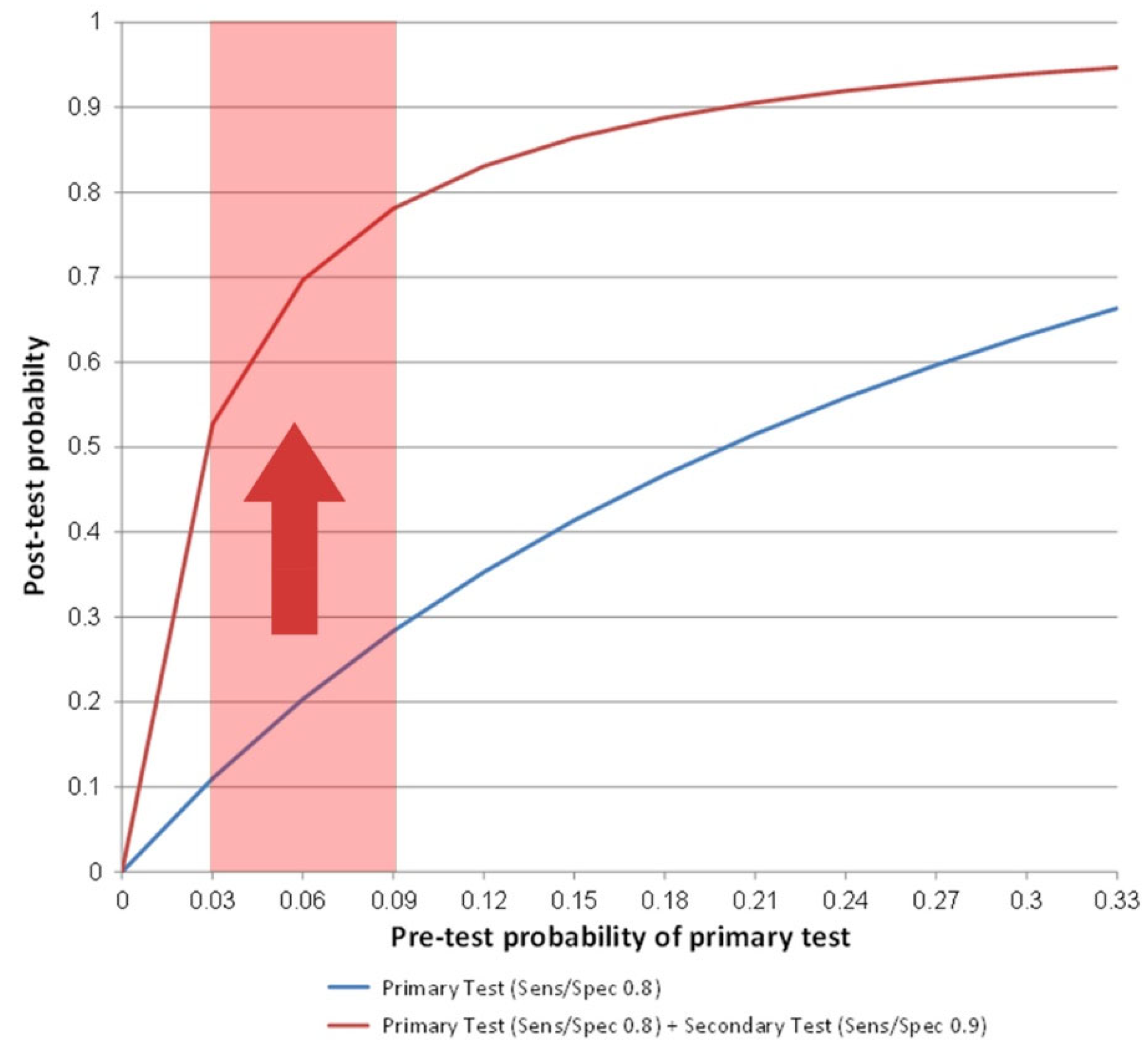
5. Multi-Modality Imaging for Identification of the At-Risk Population and Increased Statistical Power of Trials
6. Screening the General Population for Risk Status
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/American heart association task force on practice guidelines. Circulation 2014, 129, 49–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart, J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the American college of cardiology/american heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2019, 74, e177–e232. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Geisel, M.H.; Bauer, M.; Hennig, F.; Hoffmann, B.; Lehmann, N.; Möhlenkamp, S.; Kröger, K.; Kara, K.; Müller, T.; Moebus, S.; et al. Comparison of coronary artery calcification, carotid intima-media thickness and ankle-brachial index for predicting 10-year incident cardiovascular events in the general population. Eur. Heart J. 2017, 38, 1815–1822. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.; Ajani, U.; Croft, J.; Critchley, J.; Phil, D.; Labarte, D.; Kottke, T.E.; Giles, W.H.; Capewell, S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000: Commentary. N. Engl. J. Med. 2007, 356, 2388–2398. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevar, M.; Abbastavar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastavar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar]
- Odden, M.C.; Coxson, P.G.; Moran, A.; Lightwood, J.M.; Goldman, L.; Bibbins-Domingo, K. The impact of the aging population on coronary heart disease in the United States. Am. J. Med. 2011, 124, 827–833. [Google Scholar] [CrossRef] [Green Version]
- Falk, E.; Shah, P.K.; Fuster, V. Coronary plaque disruption. Circulation 1995, 92, 657–671. [Google Scholar] [CrossRef]
- Ahmadi, A.; Argulian, E.; Leipsic, J.; Newby, D.E.; Narula, J. From Subclinical atherosclerosis to plaque progression and acute coronary events: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019, 74, 1608–1617. [Google Scholar] [CrossRef] [PubMed]
- Vergallo, R.; Crea, F. Atherosclerotic Plaque Healing. N. Engl. J. Med. 2020, 383, 846–857. [Google Scholar] [CrossRef]
- Manoharan, G.; Ntalianis, A.; Muller, O.; Hamilos, M.; Sarno, G.; Melikian, N.; Vanderheyden, M.; Heyndrickx, G.R.; Wyffels, E.; Wijns, W.; et al. Severity of coronary arterial stenoses responsible for acute coronary syndromes. Am. J. Cardiol. 2009, 103, 1183–1188. [Google Scholar] [CrossRef] [PubMed]
- Frøbert, O.; Veer, M.V.; Aarnoudse, W.; Simonsen, U.; Koolen, J.J.; Pijls, N.H. Acute myocardial infarction and underlying stenosis severity. Catheter. Cardiovasc. Interv. 2007, 70, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.H.; Chawantanpipat, C.; Gattorna, T.; Chantadansuwan, T.; Kirby, A.; Madden, A.; Keech, A.; Ng, M.K. The relationship between coronary stenosis severity and compression type coronary artery movement in acute myocardial infarction. Am. Heart J. 2010, 159, 584–592. [Google Scholar] [CrossRef]
- Narula, J.; Nakano, M.; Virmani, R.; Kolodgie, F.D.; Petersen, R.; Newcomb, R.; Malik, S.; Fuster, V.; Finn, A.V. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J. Am. Coll. Cardiol. 2013, 61, 1041–1051. [Google Scholar] [CrossRef] [Green Version]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of subclinical coronary artery atherosclerosis in the general population. Circulation 2021, 144, 916–929. [Google Scholar] [CrossRef]
- Nasir, K.; Cainzos Achirica, M.; Budoff, M.; Cury, R.C.; Elizondo, J.V.; Ali, S.S.; Arias, L.; Shapiro, M.D.; Blaha, M.J.; Blankstein, R.; et al. Prevalence and characterization of occult coronary atherosclerotic disease among middle aged individuals free of clinical cardiovascular disease—results from miami heart study (miheart) at baptist health south florida. Circulation 2021, 144, A12542. [Google Scholar]
- Cho, I.; Chang, H.J.; Hartaigh, B.O.; Shin, S.; Sung, J.M.; Lin, F.Y.; Achenbach, S.; Heo, R.; Berman, D.S.; Budoff, M.J.; et al. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: Results from the coronary CT angiography evaluation for clinical outcomes international multicenter (CONFIRM) Study. Eur. Heart J. 2015, 36, 501–508. [Google Scholar]
- Mortensen, M.B.; Dzaye, O.; Steffensen, F.H.; Bøtker, H.E.; Jensen, J.M.; Sand, N.P.R.; Kragholm, K.H.; Sørensen, H.T.; Leipsic, J.; Mæng, M.; et al. Impact of plaque burden versus stenosis on ischemic events in patients with coronary atherosclerosis. J. Am. Coll. Cardiol. 2020, 76, 2803–2813. [Google Scholar] [CrossRef]
- Muhlestein, J.B.; Lappé, D.L.; Lima, J.A.C.; Rosen, B.D.; May, H.T.; Knight, S.; Bluemke, D.A.; Towner, S.R.; Le, V.; Bair, T.L.; et al. Effect of screening for coronary artery disease using ct angiography on mortality and cardiac events in high-risk patients with diabetes: The FACTOR-64 randomized clinical trial. JAMA 2014, 312, 2234–2243. [Google Scholar] [CrossRef] [PubMed]
- Stocker, T.J.; Deseive, S.; Leipsic, J.; Hadamitzky, M.; Chen, M.Y.; Rubinshtein, R.; Heckner, M.; Bax, J.J.; Fang, X.-M.; Grove, E.L.; et al. Reduction in radiation exposure in cardiovascular computed tomography imaging: Results from the prospective multicenter registry on radiation dose estimates of cardiac CT angiography in daily practice in 2017 (PROTECTION VI). Eur. Hear. J. 2018, 39, 3715–3723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalisz, K.; Buethe, J.; Saboo, S.S.; Abbara, S.; Halliburton, S.; Rajiah, P. Artifacts at Cardiac CT: Physics and solutions. RadioGraphics 2016, 36, 2064–2083. [Google Scholar] [CrossRef] [PubMed]
- Pezel, T.; Garot, P.; Kinnel, M.; Unterseeh, T.; Hovasse, T.; Champagne, S.; Toupin, S.; Sanguineti, F.; Garot, J. Prognostic value of stress cardiovascular magnetic resonance in asymptomatic patients without known coronary artery disease. Eur. Radiol. 2021, 31, 6172–6183. [Google Scholar] [CrossRef]
- De Bruyne, B.; Fearon, W.F.; Pijls, N.H.; Barbato, E.; Tonino, P.; Piroth, Z.; Jagic, N.; Mobius-Winckler, S.; Rioufol, G.; Witt, N.; et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N. Eng. J. Med. 2014, 371, 1208–1217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hachamovitch, R.; Hayes, S.W.; Friedman, J.D.; Cohen, I.; Berman, D.S. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003, 107, 2900–2907. [Google Scholar] [CrossRef] [Green Version]
- Gada, H.; Kirtane, A.J.; Kereiakes, D.J.; Bangalore, S.; Moses, J.W.; Généreux, P.; Mehran, R.; Dangas, G.D.; Leon, M.B.; Stone, G.W. Meta-analysis of trials on mortality after percutaneous coronary intervention compared with medical therapy in patients with stable coronary heart disease and objective evidence of myocardial ischemia. Am. J. Cardiol. 2015, 115, 1194–1199. [Google Scholar] [CrossRef]
- Hachamovitch, R.; Rozanski, A.; Shaw, L.J.; Stone, G.W.; Thomson, L.E.J.; Friedman, J.D.; Hayes, S.W.; Cohen, I.; Germano, G.; Berman, D.S. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur. Heart J. 2011, 32, 1012–1024. [Google Scholar] [CrossRef]
- Stone, G.W.; Hochman, J.S.; Williams, D.O.; Boden, W.E.; Ferguson, T.B.; Harrington, R.A.; Maron, D.J. Medical therapy with versus without revascularization in stable patients with moderate and severe ischemia the case for community equipoise. J. Am. Coll. Cardiol. 2016, 67, 81–99. [Google Scholar] [CrossRef] [Green Version]
- Boden, W.E.; O’Rourke, R.A.; Teo, K.K.; Hartigan, P.M.; Maron, D.J.; Kostuk, W.J.; Knudtson, M.; Dada, M.; Casperson, P.; Harris, C.L.; et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 2007, 356, 1503–1516. [Google Scholar] [CrossRef] [Green Version]
- Maron, D.J.; Hochman, J.S.; Reynolds, H.R.; Bangalore, S.; O’Brien, S.M.; Boden, W.E.; Chaitman, B.R.; Senior, R.; López-Sendón, J.; Alexander, K.P.; et al. Initial invasive or conservative strategy for stable coronary disease. N. Engl. J. Med. 2020, 382, 1395–1407. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Fihn, S.D.; Gardin, J.M.; Abrams, J.; Berra, K.; Blankenship, J.C.; Dallas, A.P.; Douglas, P.S.; Foody, J.M.; Gerber, T.C.; Hinderliter, A.L.; et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. J. Am. Coll. Cardiol. 2012, 60, e44–e164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, L.J.; Veledar, E.; Berman, D.S.; Hayes, S.W.; Friedman, J.; Slomka, P.; Germano, G.; Maron, D.J.; Mancini, G.B.J.; Hartigan, P.M.; et al. Response to letters regarding article, “Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (courage) trial nuclear substudy”. Circulation 2008, 117, 1283–1291. [Google Scholar]
- Bansal, S.; Wackers, F.J.T.; Inzucchi, S.E.; Chyun, D.A.; Davey, J.A.; Staib, L.H.; Young, S.L.; DIAD Study Investigators. Five-year outcomes in high-risk participants in the detection of ischemia in asymptomatic diabetics (diad) study: A post hoc analysis. Diabetes Care 2011, 34, 204–209. [Google Scholar] [CrossRef] [Green Version]
- Ties, D.; van Dorp, P.; Pundziute, G.; van der Aalst, C.M.; Gratama, J.W.C.; Braam, R.L.; Kuijpers, D.; Lubbers, D.D.; van der Bilt, I.A.C.; Westenbrink, D.; et al. Early detection of obstructive coronary artery disease in the general population: Objectives and study design of the EARLY-SYNERGY trial. Am. Heart J. 2022, 246, 166–177. [Google Scholar] [CrossRef]
- Antiochos, P.; Ge, Y.; Steel, K.; Bingham, S.; Abdullah, S.; Mikolich, J.R.; Arai, A.E.; Bandettini, W.P.; Patel, A.R.; Farzaneh-Far, A.; et al. Imaging of clinically unrecognized myocardial fibrosis in patients with suspected coronary artery disease. J. Am. Coll. Cardiol. 2020, 76, 945–957. [Google Scholar] [CrossRef]
- Acharya, T.; Aspelund, T.; Jonasson, T.F.; Schelbert, E.B.; Cao, J.J.; Sathya, B.; Dyke, C.K.; Aletras, A.H.; Sigurdsson, S.; Thorgeirsson, G.; et al. Association of unrecognized myocardial infarction with long-term outcomes in community-dwelling older adults: The ICELAND MI study. JAMA Cardiol. 2018, 3, 1101–1106. [Google Scholar] [CrossRef] [Green Version]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Smith, S.C.; Benjamin, E.; Bonow, R.O.; Braun, L.T.; Creager, M.A.; Franklin, B.A.; Gibbons, R.J.; Grundy, S.M.; Hiratzka, L.F.; Jones, D.W.; et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. Circulation 2011, 58, 2432–2446. [Google Scholar] [CrossRef] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M.; et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart failure society of america. J. Am. Coll. Cardiol. 2017, 70, 776–803. [Google Scholar] [PubMed]
- Mezei, A.; Armstrong, H.; Pedersen, H.N.; Campos, N.G.; Mitchell, S.M.; Sekikubo, M.; Byamugisha, J.K.; Kim, J.J.; Bryan, S.; Ogilvie, G.S. Cost-effectiveness of cervical cancer screening methods in low- and middle-income countries: A systematic review. Int. J. Cancer 2017, 141, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, L.G.M.; Van Rijn, A.F.; Verbeek, A.L.M.; Van Oijen, M.G.H.; Laheij, R.J.F.; Fockens, P.; Jansen, J.B.M.J.; Agang, E.M.M.; Dekker, E. Colorectal cancer screening comparing no screening, immunochemical and guaiac fecal occult blood tests: A cost-effectiveness analysis. Int. J. Cancer 2011, 128, 1908–1917. [Google Scholar] [CrossRef]
- Cainzos-Achirica, M.; Bittencourt, M.S.; Osei, A.D.; Haque, W.; Bhatt, D.L.; Blumenthal, R.S.; Blankstein, R.; Ray, K.K.; Blaha, M.J.; Nasir, K. Coronary artery calcium to improve the efficiency of randomized controlled trials in primary cardiovascular prevention. JACC Cardiovasc. Imaging 2020, 14, 1005–1016. [Google Scholar] [CrossRef]
- Hecht, H.S. Coronary artery calcium scanning: Past, present, and future. JACC Cardiovasc. Imaging 2015, 8, 579–596. [Google Scholar] [CrossRef]
- Lauer, M.S. Primary prevention of atherosclerotic cardiovascular disease. JAMA 2007, 297, 1376–1378. [Google Scholar] [CrossRef]
- Lakoski, S.G.; Greenland, P.; Wong, N.D.; Schreiner, P.J.; Herrington, D.M.; Kronmal, R.A.; Liu, K.; Blumenthal, R.S. Coronary artery calcium scores and risk for cardiovascular events in women classified as “low risk” based on Framingham risk score: The multi-ethnic study of atherosclerosis (MESA). Arch. Intern. Med. 2007, 167, 2437–2442. [Google Scholar] [CrossRef] [Green Version]
- Karim, R.; Hodis, H.N.; Detrano, R.; Liu, C.-R.; Liu, C.-H.; Mack, W.J. Relation of framingham risk score to subclinical atherosclerosis evaluated across three arterial sites. Am. J. Cardiol. 2008, 102, 825–830. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Friera, L.; Peñalvo, J.L.; Fernández-Ortiz, A.; Ibañez, B.; López-Melgar, B.; Laclaustra, M.; Oliva, B.; Mocoroa, A.; Mendiguren, J.; De Vega, V.M.; et al. Prevalence, vascular distribution, and multiterritorial extent of subclinical atherosclerosis in a middle-aged cohort the PESA (Progression of early subclinical atherosclerosis) study. Circulation 2015, 131, 2104–2113. [Google Scholar] [CrossRef] [Green Version]
- García-Lledó, A.; Moya-Mur, J.L.; Ponz-Mir, V.; Novo-Aparicio, S.; Sanz-Barrio, A.; Álvarez-Sanz, C.; De Santiago-Nocito, A. Relationship among risk score systems and coronary atherosclerosis determined by multislice computed tomography. Clin. Cardiol. 2016, 39, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Adibi, A.; Sadatsafavi, M.; Ioannidis, J. Validation and utility testing of clinical predictionmodels time to change the approach. JAMA 2020, 324, 235–236. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.C.; Blankstein, R.; Shaw, L.J.; Padula, W.V.; Arrieta, A.; Fialkow, J.A.; Blumenthal, R.S.; Blaha, M.J.; Krumholz, H.M.; Nasir, K. Implications of coronary artery calcium testing for treatment decisions among statin candidates according to the ACC/AHA Cholesterol Management Guidelines: A cost-effectiveness analysis. JACC Cardiovasc. Imaging 2017, 10, 938–952. [Google Scholar] [CrossRef] [PubMed]
- Pletcher, M.J.; Pignone, M.; Earnshaw, S.; McDade, C.; Phillips, K.A.; Auer, R.; Zablotska, L.; Greenland, P. Using the coronary artery calcium score to guide statin therapy a cost-effectiveness analysis. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 276–284. [Google Scholar] [CrossRef] [Green Version]
- Patel, M.J.; de Lemos, J.A.; McGuire, D.K.; See, R.; Lindsey, J.B.; Murphy, S.A.; Grundy, S.M.; Khera, A. Evaluation of coronary artery calcium screening strategies focused on risk categories: The Dallas heart study. Am. Heart J. 2009, 157, 1001–1009. [Google Scholar] [CrossRef] [Green Version]
- Ceasar, J.N.; Ayers, C.; Andrews, M.R.; Claudel, S.E.; Tamura, K.; Das, S.; De Lemos, J.; Neeland, I.J.; Powell-Wiley, T.M. Unfavorable perceived neighborhood environment associates with less routine healthcare utilization: Data from the Dallas heart study. PLoS ONE 2020, 15, e0230041. [Google Scholar] [CrossRef]
- Van Der Aalst, C.M.; Vonder, M.; Gratama, J.; Adriaansen, H.J.; Kuijpers, D.; Denissen, S.J.; Van der Harst, P.; Braam, R.L.; Van Dijkman, P.R.M.; Bruggen, R.V.; et al. Risk or benefit in screening for cardiovascular disease (ROBINSCA): The rationale and study design of a population-based randomized-controlled screening trial for cardiovascular disease. J. Clin. Trials 2019, 9, 1–8. [Google Scholar]
- Voros, S.; Rivera, J.J.; Berman, D.S.; Blankstein, R.; Budoff, M.J.; Cury, R.C.; Desai, M.Y.; Dey, D.; Halliburton, S.S.; Hecht, H.S.; et al. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography: A report by the society for atherosclerosis imaging and prevention tomographic imaging and prevention counci. J. Cardiovasc. Comput. Tomogr. 2011, 5, 75–83. [Google Scholar] [CrossRef]
- Baron, K.B.; Choi, A.D.; Chen, M.Y. Low radiation dose calcium scoring: Evidence and techniques. Curr. Cardiovasc. Imaging Rep. 2016, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Dzaye, O.; Razavi, A.C.; Dardari, Z.A.; Shaw, L.J.; Berman, D.S.; Budoff, M.J.; Miedema, M.D.; Nasir, K.; Rozanski, A.; Rumberger, J.A.; et al. Modeling the recommended age for initiating coronary artery calcium testing among at-risk young adults. JACC 2021, 78, 1573–1583. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ties, D.; van Dorp, P.; Pundziute, G.; Lipsic, E.; van der Aalst, C.M.; Oudkerk, M.; de Koning, H.J.; Vliegenthart, R.; van der Harst, P. Multi-Modality Imaging for Prevention of Coronary Artery Disease and Myocardial Infarction in the General Population: Ready for Prime Time? J. Clin. Med. 2022, 11, 2965. https://doi.org/10.3390/jcm11112965
Ties D, van Dorp P, Pundziute G, Lipsic E, van der Aalst CM, Oudkerk M, de Koning HJ, Vliegenthart R, van der Harst P. Multi-Modality Imaging for Prevention of Coronary Artery Disease and Myocardial Infarction in the General Population: Ready for Prime Time? Journal of Clinical Medicine. 2022; 11(11):2965. https://doi.org/10.3390/jcm11112965
Chicago/Turabian StyleTies, Daan, Paulien van Dorp, Gabija Pundziute, Erik Lipsic, Carlijn M. van der Aalst, Matthijs Oudkerk, Harry J. de Koning, Rozemarijn Vliegenthart, and Pim van der Harst. 2022. "Multi-Modality Imaging for Prevention of Coronary Artery Disease and Myocardial Infarction in the General Population: Ready for Prime Time?" Journal of Clinical Medicine 11, no. 11: 2965. https://doi.org/10.3390/jcm11112965





