Mallampati Score Is an Independent Predictor of Active Oxygen Therapy in Patients with COVID-19
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Population
2.2. The Facility
2.3. The Study Outcomes
2.4. The Statistical Analyses
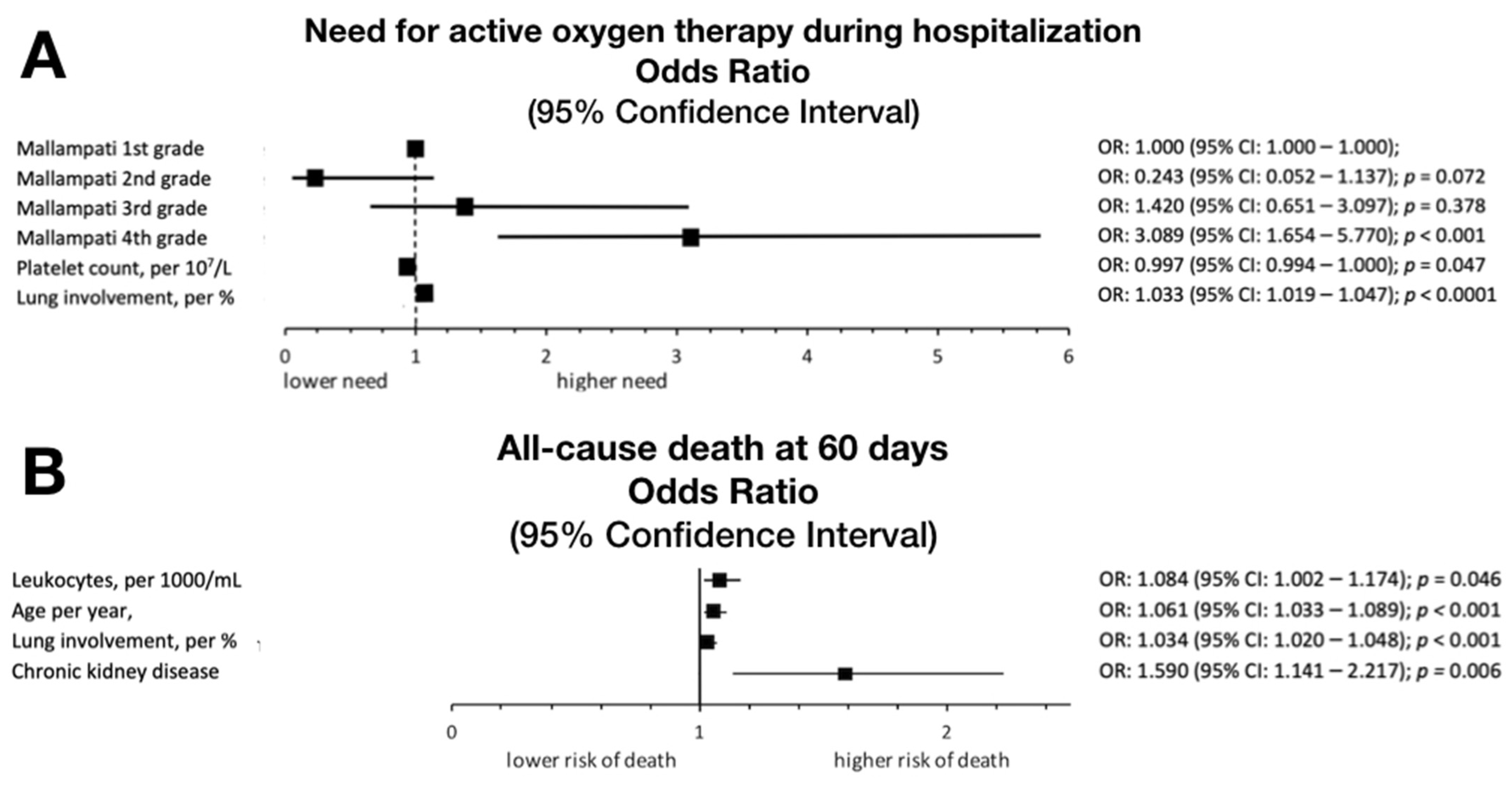
3. Results
4. Discussion
4.1. Limitations
4.2. Areas for Future Research
4.3. Interpretation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Dattani, S.; Roser, M. Coronavirus (COVID-19) Hospitalizations. Available online: https://ourworldindata.org/covid-hospitalizations (accessed on 24 March 2022).
- Menachemi, N.; Dixon, B.E.; Wools-Kaloustian, K.K.; Yiannoutsos, C.T.; Halverson, P.K. How Many SARS-CoV-2–Infected People Require Hospitalization? Using Random Sample Testing to Better Inform Preparedness Efforts. J. Public Health Manag. Pract. 2021, 27, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Wang, L.; Ye, J.; Gu, Z.; Wang, S.; Xia, J.; Xie, Y.; Li, Q.; Xu, R.; Lin, N. Predictors of mortality in patients with coronavirus disease 2019: A systematic review and meta-analysis. BMC Infect. Dis. 2021, 21, 663. Available online: http://www.ncbi.nlm.nih.gov/pubmed/34238232 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Liu, Z.; Li, J.; Huang, J.; Guo, L.; Gao, R.; Luo, K.; Zeng, G.; Zhang, T.; Yi, M.; Huang, Y.; et al. Association Between Diabetes and COVID-19: A Retrospective Observational Study With a Large Sample of 1,880 Cases in Leishenshan Hospital, Wuhan. Front. Endocrinol. 2020, 11, 478. [Google Scholar] [CrossRef] [PubMed]
- AlShahrani, I.; Hosmani, J.; Shankar, V.G.; AlShahrani, A.; Togoo, R.A.; Yassin, S.M.; Khan, S.; Patil, S. COVID-19 and cardiovascular system-a comprehensive review. Rev. Cardiovasc. Med. 2021, 22, 343–351. [Google Scholar] [CrossRef]
- Phelps, M.; Christensen, D.M.; Gerds, T.; Fosbøl, E.; Torp-Pedersen, C.; Schou, M.; Køber, L.; Kragholm, K.; Andersson, C.; Biering-Sørensen, T.; et al. Cardiovascular comorbidities as predictors for severe COVID-19 infection or death. Eur. Heart J.-Qual. Care Clin. Outcomes 2021, 7, 172–180. [Google Scholar] [CrossRef]
- Xue, G.; Gan, X.; Wu, Z.; Xie, D.; Xiong, Y.; Hua, L.; Zhou, B.; Zhou, N.; Xiang, J.; Li, J. Novel serological biomarkers for inflammation in predicting disease severity in patients with COVID-19. Int. Immunopharmacol. 2020, 89, 107065. [Google Scholar] [CrossRef]
- Zhang, H.J.; Qi, G.Q.; Gu, X.; Zhang, X.Y.; Fang, Y.F.; Jiang, H.; Zhao, Y.J. Lymphocyte blood levels that remain low can predict the death of patients with COVID-19. Medicine 2021, 100, e26503. [Google Scholar] [CrossRef]
- Nuckton, T.J.; Glidden, D.V.; Browner, W.S.; Claman, D.M. Physical Examination: Mallampati Score as an Independent Predictor of Obstructive Sleep Apnea. Sleep 2006, 29, 903–908. [Google Scholar] [CrossRef]
- Mallampati, S.R.; Gatt, S.P.; Gugino, L.D.; Desai, S.P.; Waraksa, B.; Freiberger, D.; Liu, P.L. A clinical sign to predict difficult tracheal intubation: A prospective study. Can. Anaesth. Soc. J. 1985, 32, 429–434. Available online: http://www.ncbi.nlm.nih.gov/pubmed/4027773 (accessed on 24 March 2022). [CrossRef] [Green Version]
- Chalmers, J.D.; Crichton, M.L.; Goeminne, P.C.; Cao, B.; Humbert, M.; Shteinberg, M.; Antoniou, K.M.; Ulrik, C.S.; Parks, H.; Wang, C.; et al. Management of hospitalised adults with coronavirus disease 2019 (COVID-19): A European Respiratory Society living guideline. Eur. Respir. J. 2021, 57, 2100048. Available online: http://erj.ersjournals.com/lookup/ (accessed on 24 March 2022). [CrossRef]
- Marti, C.; Garin, N.; Grosgurin, O.; Poncet, A.; Combescure, C.; Carballo, S.; Perrier, A. Prediction of severe community-acquired pneumonia: A systematic review and meta-analysis. Crit. Care 2012, 16, R141. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22839689 (accessed on 24 March 2022). [CrossRef] [PubMed] [Green Version]
- McNally, M.; Curtain, J.; O’Brien, K.K.; Dimitrov, B.D.; Fahey, T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: Systematic review and meta-analysis. Br. J. Gen. Pract. 2010, 60, e423–e433. Available online: http://www.ncbi.nlm.nih.gov/pubmed/20883616 (accessed on 24 March 2022). [CrossRef] [PubMed] [Green Version]
- Fine, M.J.; Auble, T.E.; Yealy, D.M.; Hanusa, B.H.; Weissfeld, L.A.; Singer, D.E.; Coley, C.M.; Marrie, T.J.; Kapoor, W.N. A Prediction Rule to Identify Low-Risk Patients with Community-Acquired Pneumonia. N. Engl. J. Med. 1997, 336, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, S.; Yatera, K.; Kawanami, T.; Fujino, Y.; Moro, H.; Aoki, N.; Komiya, K.; Kadota, J.; Shime, N.; Tsukada, H.; et al. Pneumonia Severity Assessment Tools for Predicting Mortality in Patients with Healthcare-Associated Pneumonia: A Systematic Review and Meta-Analysis. Respiration 2017, 93, 441–450. Available online: https://www.karger.com/Article/FullText/470915 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Chen, S.; Feng, H.; Xu, H.; Huang, S.; Sun, J.; Zhou, L.; He, J.; Song, W.; Wang, R.; Li, X.; et al. Patterns of Deterioration in Moderate Patients With COVID-19 From Jan 2020 to Mar 2020: A Multi-Center, Retrospective Cohort Study in China. Front. Med. 2020, 7, 839. Available online: https://www.frontiersin.org/articles/10.3389/fmed.2020.567296/full (accessed on 24 March 2022). [CrossRef]
- Dhont, S.; Derom, E.; Van Braeckel, E.; Depuydt, P.; Lambrecht, B.N. The pathophysiology of “happy” hypoxemia in COVID-19. Respir. Res. 2020, 21, 198. Available online: http://www.ncbi.nlm.nih.gov/pubmed/32723327 (accessed on 24 March 2022). [CrossRef]
- Piraino, T. Noninvasive respiratory support in acute hypoxemic respiratory failure. Respir. Care 2019, 64, 638–646. [Google Scholar] [CrossRef]
- Nishimura, M. High-flow nasal cannula oxygen therapy devices. Respir. Care 2019, 64, 735–742. [Google Scholar] [CrossRef]
- Boccatonda, A.; Groff, P. High-flow nasal cannula oxygenation utilization in respiratory failure. Eur. J. Intern. Med. 2019, 64, 10–14. [Google Scholar] [CrossRef]
- Nedel, W.L.; Deutschendorf, C.; Moraes Rodrigues Filho, E. High-Flow Nasal Cannula in Critically Ill Subjects With or at Risk for Respiratory Failure: A Systematic Review and Meta-Analysis. Respir. Care 2017, 62, 123–132. [Google Scholar] [CrossRef]
- Rochwerg, B.; Brochard, L.; Elliott, M.W.; Hess, D.; Hill, N.S.; Nava, S.; Navalesi, P.; Antonelli, M.; Brozek, J.; Conti, G.; et al. Official ERS/ATS clinical practice guidelines: Noninvasive ventilation for acute respiratory failure. Eur. Respir. J. 2017, 50, 1602426. [Google Scholar] [CrossRef] [PubMed]
- Akoumianaki, E.; Ischaki, E.; Karagiannis, K.; Sigala, I.; Zakyn-Thinos, S. The role of noninvasive respiratory management in patients with severe COVID-19 pneumonia. J. Pers. Med. 2021, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Bertaina, M.; Nuñez-Gil, I.J.; Franchin, L.; Fernández Rozas, I.; Arroyo-Espliguero, R.; Viana-Llamas, M.C.; Romero, R.; Maroun Eid, C.; Uribarri, A.; Becerra-Muñoz, V.M.; et al. Non-invasive ventilation for SARS-CoV-2 acute respiratory failure: A subanalysis from the HOPE COVID-19 registry. Emerg. Med. J. 2021, 38, 359–365. Available online: http://www.ncbi.nlm.nih.gov/pubmed/33727235 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Czajkowska-Malinowska, M.; Kania, A.; Kuca, P.J.; Nasiłowski, J.; Skoczyński, S.; Sokołowski, R.; Śliwiński, P.S. Treatment of acute respiratory failure in the course of COVID-19. Practical hints from the expert panel of the Assembly of Intensive Care and Rehabilitation of the Polish Respiratory Society. Adv. Respir. Med. 2020, 88, 245–266. Available online: https://journals.viamedica.pl/advances_in_respiratory_medicine/article/view/69361 (accessed on 24 March 2022). [CrossRef]
- Oczkowski, S.; Ergan, B.; Bos, L.; Chatwin, M.; Ferrer, M.; Gregoretti, C.; Heunks, L.; Frat, J.-P.; Longhini, F.; Nava, S.; et al. ERS Clinical Practice Guidelines: High-flow nasal cannula in acute respiratory failure. Eur. Respir. J. 2022, 59, 2101574. [Google Scholar] [CrossRef]
- Hanidziar, D.; Robson, S.C. Hyperoxia and modulation of pulmonary vascular and immune responses in COVID-19. Am. J. Physiol. Cell. Mol. Physiol. 2021, 320, L12–L16. [Google Scholar] [CrossRef]
- McNicholas, W.T. Impact of sleep on respiratory muscle function. Monaldi Arch. Chest Dis. 2002, 57, 277–280. Available online: http://www.ncbi.nlm.nih.gov/pubmed/12814041 (accessed on 24 March 2022).
- Gerayeli, F.V.; Milne, S.; Cheung, C.; Li, X.; Yang, C.W.T.; Tam, A.; Choi, L.H.; Bae, A.; Sin, D.D. COPD and the risk of poor outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2021, 33, 100789. [Google Scholar] [CrossRef]
- Shi, L.; Xu, J.; Xiao, W.; Wang, Y.; Jin, Y.; Chen, S.; Duan, G.; Yang, H.; Wang, Y. Asthma in patients with coronavirus disease 2019: A systematic review and meta-analysis. Ann. Allergy Asthma Immunol. 2021, 126, 524–534. [Google Scholar] [CrossRef]
- Singh, J.; Alam, A.; Samal, J.; Maeurer, M.; Ehtesham, N.Z.; Chakaya, J.; Hira, S.; Hasnain, S.E. Role of multiple factors likely contributing to severity-mortality of COVID-19. Infect. Genet. Evol. 2021, 96, 105101. Available online: https://linkinghub.elsevier.com/retrieve/pii/S1567134821004 (accessed on 24 March 2022). [CrossRef]
- Zhang, J.-J.; Dong, X.; Liu, G.-H.; Gao, Y.-D. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 2022, 1–18. Available online: http://www.ncbi.nlm.nih.gov/pubmed/35044620 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Singh, J.; Malik, P.; Patel, N.; Pothuru, S.; Israni, A.; Chakinala, R.C.; Hussain, M.R.; Chidharla, A.; Patel, H.; Patel, S.K.; et al. Kidney disease and COVID-19 disease severity—systematic review and meta-analysis. Clin. Exp. Med. 2022, 22, 125–135. Available online: https://link.springer.com/10.1007/s10238-021-00715-x (accessed on 24 March 2022). [CrossRef] [PubMed]
- Kunutsor, S.K.; Laukkanen, J.A. Renal complications in COVID-19: A systematic review and meta-analysis. Ann. Med. 2020, 52, 345–353. Available online: https://www.tandfonline.com/doi/full/10.1080/07853890.2020.1790643 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Tenforde, M.W.; Self, W.H.; Adams, K.; Gaglani, M.; Ginde, A.A.; McNeal, T.; Ghamande, S.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; et al. Association Between mRNA Vaccination and COVID-19 Hospitalization and Disease Severity. JAMA 2021, 326, 2043–2054. Available online: http://www.ncbi.nlm.nih.gov/pubmed/34734975 (accessed on 24 March 2022). [CrossRef] [PubMed]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Robertson, C.; Stowe, J.; Tessier, E.; Simmons, R.; Cottrell, S.; Roberts, R.; O’Doherty, M.; et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. BMJ 2021, 373, n1088. Available online: http://www.ncbi.nlm.nih.gov/pubmed/33985964 (accessed on 24 March 2022). [CrossRef]
- Szarpak, L.; Zaczynski, A.; Kosior, D.; Bialka, S.; Ladny, J.R.; Gilis-Malinowska, N.; Smereka, J.; Kanczuga-Koda, L.; Gasecka, A.; Filipiak, K.J.; et al. Evidence of diagnostic value of ferritin in patients with COVID-19. Cardiol. J. 2020, 27, 886–887. Available online: https://journals.viamedica.pl/cardiology_journal/article/view/71765 (accessed on 24 March 2022). [CrossRef]
- Santa Cruz, A.; Mendes-Frias, A.; Oliveira, A.I.; Dias, L.; Matos, A.R.; Carvalho, A.; Capela, C.; Pedrosa, J.; Castro, A.G.; Silvestre, R. Interleukin-6 Is a Biomarker for the Development of Fatal Severe Acute Respiratory Syndrome Coronavirus 2 Pneumonia. Front. Immunol. 2021, 12, 263. [Google Scholar] [CrossRef]
- Zhang, J.; Hao, Y.; Ou, W.; Ming, F.; Liang, G.; Qian, Y.; Cai, Q.; Dong, S.; Hu, S.; Wang, W.; et al. Serum interleukin-6 is an indicator for severity in 901 patients with SARS-CoV-2 infection: A cohort study. J. Transl. Med. 2020, 18, 406. Available online: https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02571-x (accessed on 24 March 2022). [CrossRef]
- Sabaka, P.; Koščálová, A.; Straka, I.; Hodosy, J.; Lipták, R.; Kmotorková, B.; Kachlíková, M.; Kušnírová, A. Role of interleukin 6 as a predictive factor for a severe course of Covid-19: Retrospective data analysis of patients from a long-term care facility during COVID-19 outbreak. BMC Infect. Dis. 2021, 21, 308. Available online: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-05945-8 (accessed on 24 March 2022). [CrossRef]
| Parameter | Overall | Mallampati I | Mallampati II | Mallampati III | Mallampati IV | p |
|---|---|---|---|---|---|---|
| Female sex, n/N (%) | 220/493 (44.8%) | 26/69 (37.7%) | 27/57 (47.4%) | 36/78 (46.2%) | 131/289 (45.4%) | 0.64 |
| Age, years | 69 (61–79) | 65 (55–77) | 67 (58–73) | 69 (63–78) | 69 (61–77) | 0.29 |
| CKD | 128/493 (26.0%) | 14/69 (20.3%) | 9/57 (15.8%) | 17/78 (21.8%) | 88/289 (30.5%) | 0.046 |
| Asthma | 40/493 (8.1%) | 6/69 (8.7%) | 3/57 (5.3%) | 3/78 (3.9%) | 28/289 (9.7%) | 0.32 |
| COPD | 31/493 (6.3%) | 2/69 (2.9%) | 5/57 (8.8%) | 5/78 (6.4%) | 19/289 (6.6%) | 0.57 |
| OSA | 14/493 (2.9%) | 1/69 (1.5%) | 0/57 (0.0%) | 2/78 (2.6%) | 11/289 (3.8%) | 0.37 |
| DM | 121/493 (24.5%) | 12/69 (17.4%) | 11/57 (19.3%) | 15/78 (19.2%) | 83/289 (28.7%) | 0.08 |
| HA | 277/493 (56.2%) | 46/69 (66.7%) | 29/57 (50.9%) | 39/78 (50.0%) | 163/289 (56.4%) | 0.18 |
| CAD | 131/493 (26.6%) | 16/69 (23.2%) | 11/57 (19.3%) | 19/78 (24.4%) | 85/289 (29.4%) | 0.34 |
| Stroke | 47/493 (9.5%) | 5/69 (7.2%) | 3/57 (5.3%) | 6/78 (7.7%) | 33/289 (11.4%) | 0.37 |
| Malignancy | 59/493 (12.0%) | 7/69 (10.1%) | 8/57 (14.0%) | 9/78 (11.5%) | 35/289 (12.1%) | 0.98 |
| Smoking | 76/493 (15.4%) | 5/69 (7.2%) | 12/57 (21.1%) | 14/78 (18.0%) | 45/289 (15.6%) | 0.14 |
| Obesity | 130/493 (26.3%) | 14/69 (20.3%) | 16/57 (28.1%) | 22/78 (28.2%) | 78/289 (26.9%) | 0.66 |
| Full vaccination | 154/493 (31.2%) | 23/69 (33.3%) | 15/57 (26.3%) | 27/78 (34.6%) | 89/289 (30.8%) | 0.80 |
| Parameter | Overall | Mallampati I | Mallampati II | Mallampati III | Mallampati IV | p |
|---|---|---|---|---|---|---|
| BMI, kg/m2 (Q1–Q3) | 27.5 (24.6–30.9) | 26.4 (24.2–29.4) | 27.3 (24.2–31.7) | 27.0 (24.3–30.5) | 27.8 (25.0–31.1) | 0.20 |
| Pneumonia volume, % | 30 (10–50) | 20 (10–40) | 20 (15–35) | 25 (10–50) | 30 (10–50) | 0.23 |
| Platelets; median (Q1–Q3) | 195 (147–273) | 196 (148–270) | 196 (153–313) | 192 (153–277) | 200 (151–276) | 0.87 |
| Hemoglobin median (Q1–Q3) | 13.8 (12.3–16.1) | 14.2 (13.2–16.4) | 13.3 (11.9–16.0) | 13.5 (12.2–15.9) | 13.7 (12.2–15.4) | 0.49 |
| WBC median (Q1–Q3) | 6.5 (4.7–9.1) | 6.0 (4.1–8.9) | 5.5 (4.4–7.6) | 6.4 (4.6–8.8) | 6.7 (4.8–9.0) | 0.1 |
| CRP median (Q1–Q3) | 89 (50–146) | 65 (36–114) | 90 (59–131) | 95 (54–133) | 86 (48–147) | 0.19 |
| PCT median (Q1–Q3) | 0.14 (0.07–0.31) | 0.09 (0.05–0.24) | 0.11 (0.06–0.26) | 0.13 (0.06–0.27) | 0.13 (0.07–0.3) | 0.34 |
| IL-6 median (Q1–Q3) | 46.9 (21.3–92.0) | 34.7 (15.9–80.2) | 42.5 (22.1–79.2) | 38.6 (17.2–65.8) | 48.3 (21.3–95.6) | 0.14 |
| D-Dimer median (Q1–Q3) | 1160 (670–2120) | 845 (492–1955) | 1035 (695–2075) | 945 (640–2100) | 1160 (670–2000) | 0.45 |
| Pulse oximeter oxygen saturation, %, median (Q1–Q3); [n/N] * | 88 (83–93) [279/494] | 90 (85–95) [44/69] | 90 (85–94) [36/57] | 88 (84–93) [48/78] | 88 (82–93) [151/289] | 0.14 |
| Parameter | Overall | Mallampati I | Mallampati II | Mallampati III | Mallampati IV | p |
|---|---|---|---|---|---|---|
| Transfer to ICU, n/N (%) | 66/493 (13.4%) | 11/69 (15.9%) | 3/57 (5.3%) | 7/78 (9.0%) | 45/289 (15.7%) | 0.10 |
| In-hospital death n/N (%) | 100/493 (20.3%) | 13/69 (18.8%) | 7/57 (12.3%) | 17/78 (21.8%) | 63/289 (21.8%) | 0.40 |
| PE during hospitalization; n/N (%) | 33/493 (6.7%) | 3/69 (4.3%) | 1/57 (1.8%) | 5/77 (6.4%) | 24/289 (8.3%) | 0.27 |
| Active oxygen therapy; n/N (%) | 133/493 (27.0%) | 12/69 (17.4%) | 10/57 (17.5%) | 16/78 (20.5%) | 95/289 (32.9%) | 0.005 |
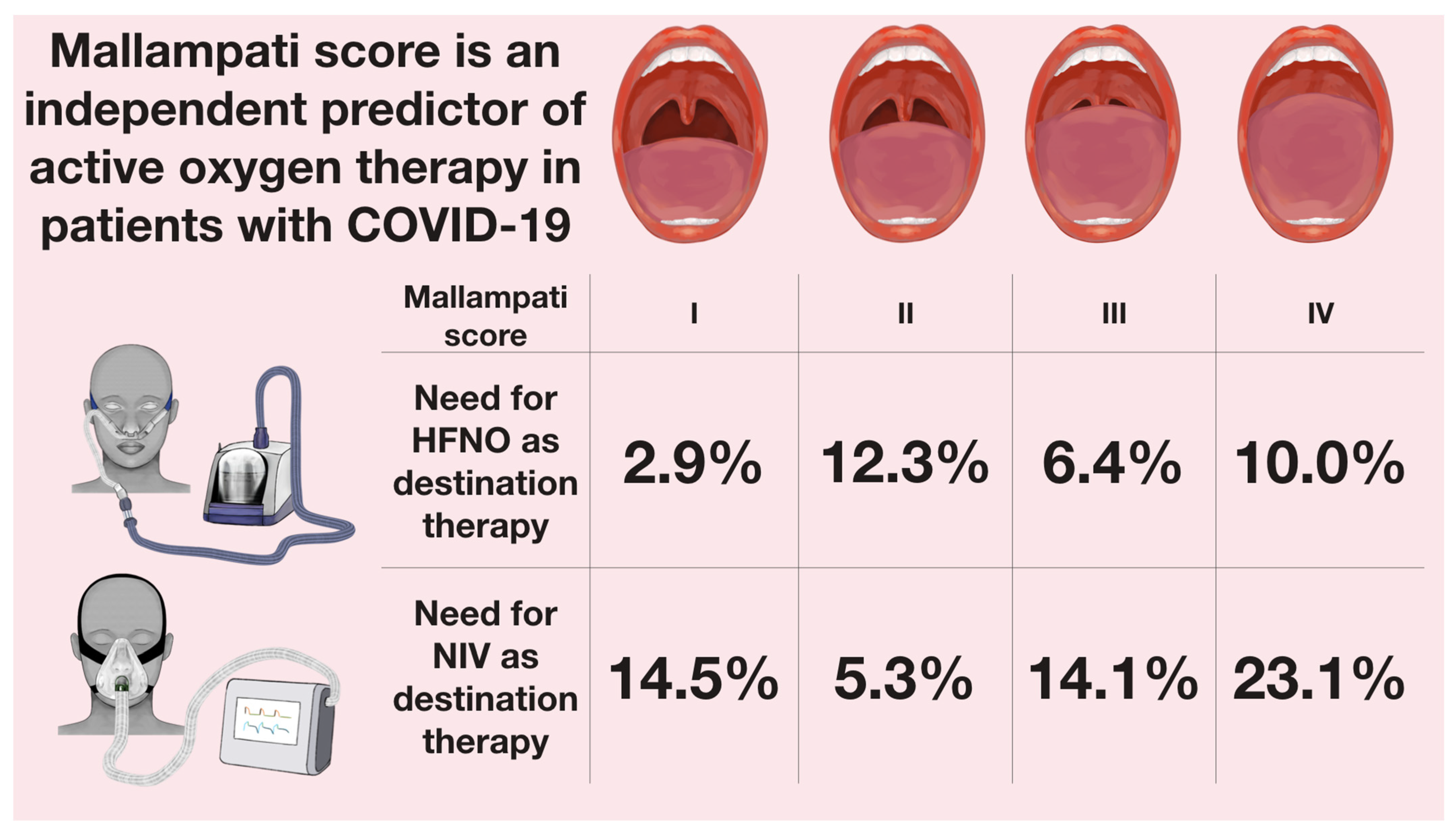
| HFNO as destination therapy | 43/493 (8.7%) | 2/69 (2.9%) | 7/57 (12.3%) | 5/78 (6.4%) | 29/289 (10.0%) | 0.024 |
| NIV as destination therapy | 91/493 (18.5%) | 10/69 (14.5%) | 3/57 (5.3%) | 11/78 (14.1%) | 67/289 (23.2%) | |
| Days to HFNO | 1 (0–3) | 1 (0–3) | 2 (1–3) | 2 (1–4) | 1 (0–3) | 0.8 |
| Days to NIV | 1 (0–3) | 4 (2–5) | 1 (1–1) | 1.5 (1–3.5) | 2 (1–4) | 0.53 |
| Death at median of 60 days n/N (%) | 154/493 (31.2%) | 19/69 (27.5%) | 9/57 (15.8%) | 25/78 (32.1%) | 101/289 (35.0%) | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dyrbuś, M.; Oraczewska, A.; Szmigiel, S.; Gawęda, S.; Kluszczyk, P.; Cyzowski, T.; Jędrzejek, M.; Dubik, P.; Kozłowski, M.; Kwiatek, S.; et al. Mallampati Score Is an Independent Predictor of Active Oxygen Therapy in Patients with COVID-19. J. Clin. Med. 2022, 11, 2958. https://doi.org/10.3390/jcm11112958
Dyrbuś M, Oraczewska A, Szmigiel S, Gawęda S, Kluszczyk P, Cyzowski T, Jędrzejek M, Dubik P, Kozłowski M, Kwiatek S, et al. Mallampati Score Is an Independent Predictor of Active Oxygen Therapy in Patients with COVID-19. Journal of Clinical Medicine. 2022; 11(11):2958. https://doi.org/10.3390/jcm11112958
Chicago/Turabian StyleDyrbuś, Maciej, Aleksandra Oraczewska, Szymon Szmigiel, Szymon Gawęda, Paulina Kluszczyk, Tomasz Cyzowski, Marek Jędrzejek, Paweł Dubik, Michał Kozłowski, Sebastian Kwiatek, and et al. 2022. "Mallampati Score Is an Independent Predictor of Active Oxygen Therapy in Patients with COVID-19" Journal of Clinical Medicine 11, no. 11: 2958. https://doi.org/10.3390/jcm11112958
APA StyleDyrbuś, M., Oraczewska, A., Szmigiel, S., Gawęda, S., Kluszczyk, P., Cyzowski, T., Jędrzejek, M., Dubik, P., Kozłowski, M., Kwiatek, S., Celińska, B., Wita, M., Trejnowska, E., Swinarew, A., Darocha, T., Barczyk, A., & Skoczyński, S. (2022). Mallampati Score Is an Independent Predictor of Active Oxygen Therapy in Patients with COVID-19. Journal of Clinical Medicine, 11(11), 2958. https://doi.org/10.3390/jcm11112958









