1. Introduction
Inflammatory bowel disease (IBD) is a diagnosis encompassing numerous chronic diseases impacting the human bowel, including Crohn’s disease (CD) and ulcerative colitis (UC). The impact of IBD is wide-ranging and symptoms include diarrhoea, rectal bleeding, unintended weight loss, and fatigue, while IBD also confers an increased risk of certain cancers [
1,
2]. Co-morbid psychological difficulties are also prevalent, including elevated stress, depression, anxiety, and body image impairment [
3,
4,
5,
6,
7]. This further exacerbates the impact on the individual’s quality of life, but also impacts disease management. Indeed, comorbid psychological difficulties are associated with disease activity, flares, treatment response, and the necessity of surgical intervention [
2,
6,
8,
9,
10,
11,
12,
13,
14,
15]. Growing evidence suggests that stress—in particular—is associated with disease activity and severity while conflicting evidence suggests that stress may also be involved in the initial development of IBD [
9,
15]. Given such convincing evidence of a psychological component and impact in and of IBD, psychological support is now considered an integral component of modern IBD management [
16,
17].
Myriad interventions are available to intervene with stress in those diagnosed with IBD, ranging from psychoeducational programs, stress management and relaxation strategies, hypnotherapy, mindfulness-based stress reduction treatments, and cognitive behavioural therapy (CBT) [
18,
19]. Gracie et al. and Knowles et al. suggested a varying rate of effectiveness of these interventions, with psychoeducation and CBT tending to convey the greatest improvement in psychological distress and wellbeing. Moreover, the benefits of psychological interventions tended not to extend to disease-related outcomes (e.g., disease activity and severity). However, the findings of Gracie et al. and Knowles et al. contrast somewhat with those of earlier reviews, which observed minimal-to-no effectiveness of psychotherapeutic interventions in intervening with depression, quality of life (QoL), coping, and anxiety [
20,
21]. A concern common to reviews to date centres on methodological rigor and reporting. Many studies are observed to be non-randomized, devoid of inclusion and exclusion criteria, neglect to report salient participant data (e.g., IBD type), and neglect to report sufficient intervention program detail [
18,
19,
20,
21].
More recently, studies have investigated the impact of acceptance and commitment therapy on psychological suffering in those experiencing chronic health conditions. Acceptance and commitment therapy (ACT) is a process-orientated therapy that proposes psychopathology or psychological suffering emerges from psychological inflexibility whereby individuals’ efforts to control, escape, and avoid unwanted thoughts and feelings act as a barrier to valued and effective behaviour [
22]. ACT aims not to change or reduce distressing and unwanted internal experiences, but to shape ways of limiting the influence of those thoughts and feelings on day-to-day living and goal achievement by increasing psychological flexibility [
23]. Therefore, ACT targets ineffective and unhelpful behaviour which functions to avoid internal events (e.g., unwanted thoughts, emotions, and stress), and introduces mindfulness and acceptance-based skills to facilitate behaviour change and reduce psychological suffering [
22,
24]. Growing evidence has supported the effectiveness of ACT for myriad psychological and health conditions including anxiety, depression, stress, chronic pain, irritable bowel syndrome (IBS) and smoking cessation [
25,
26,
27,
28,
29,
30].
Initial evidence suggests ACT may be an appropriate intervention to target psychological suffering in people with an IBD diagnosis. For example, the ACT process of cognitive fusion—the tendency to perceive and act on thoughts through a context of literality—has been observed to be negatively associated with psychological and physical health in IBD and mediates the relationship between chronic-illness-related stigma and psychological QoL [
31,
32]. Moreover, changes in cognitive fusion rather than IBD symptomatology predicted improvements in psychological health. Similar findings have been observed for experiential avoidance, with experiential avoidance mediating the relationship between IBD symptomatology and physical and psychological QoL [
33]. ACT interventions, particularly brief ACT interventions, appear to be acceptable to people with IBD and other chronic health conditions [
34,
35,
36]. Lastly, the first trials of ACT in people with IBD suggest it may be effective in intervening with psychological distress [
34,
37]. The latter, Wynne et al., investigated the effectiveness of an eight-week ACT group targeting psychological distress in people with IBD. They observed that the ACT intervention produced reductions in stress and depression while also resulting in increased QoL and psychological flexibility. Indeed, early evidence suggests ACT is an appropriate, effective, and acceptable model to intervene with distress in IBD.
Despite the promise of interventions such as those employed by Wynne et al., such intensive and medium- to long-term interventions may not always be suitable. Reasons for this range from limited clinical and economic resources in healthcare systems, willingness to access psychological support, and feasibility for people with IBD themselves [
38]. Such challenges have influenced the development of accessible, brief, low-intensity, and self-directed interventions for a range of psychological concerns. Indeed, growing evidence suggests briefer interventions can effect substantial change for clients. For example, almost half of clients with depression and anxiety exhibit sudden large gains within the first two to four CBT treatment sessions [
39,
40]. Similar gains are observed in CBT for post-traumatic stress disorder (PTSD; 53 percent of clients), adolescent depression, binge eating (62 percent of clients), and irritable bowel syndrome (30 percent of clients) [
41,
42,
43,
44]. Furthermore, this rapid response is associated with long-term improvements in functioning and a reduction in long-term relapse rates [
39,
43,
45]. Similar gains have been observed in brief ACT interventions. For example, 90 min and three-hour focused acceptance and commitment therapy (FACT) interventions produced substantial and lasting reductions in depression which were comparable to a one-day (i.e., six-hour) FACT workshop [
46,
47]. Similar effects have been observed following brief ACT interventions for other presented concerns, including repetitive negative thinking and psychotic depression [
48,
49]. While little attention has been devoted to brief ACT interventions for IBD, early evidence suggests they are acceptable and potentially effective [
34,
35,
36,
39]. Taken as a whole, these findings suggest that for many individuals, significant treatment benefits are conferred after as little as two to four hours of intervention, while such brief interventions (including brief ACT interventions) appear acceptable to people with long-term health conditions including IBD.
Given the barriers to extended forms of psychological support, brief and low-intensity interventions are needed which are relatively low-cost, evidence-based, and produce reductions in stress, depression, and anxiety in people with IBD that are clinically meaningful. The present paper intended to understand the required dosage to reduce psychological distress in people with comorbid IBD. Given its significant prevalence and impact on QoL and disease activity, stress was given the greatest focus with a lesser focus on depression and anxiety. Under the present research, two cohorts of patients with an IBD diagnosis were delivered a single-session and two-session ACT intervention, respectively. Both interventions were trialled via single-case experimental designs (SCEDs) which facilitate the investigation of individual benefit and risk conferred by the brief ACT interventions and generalizable intervention effectiveness. Given existing findings on ACT for IBD populations and brief ACT interventions, it was predicted that the interventions would produce reduced stress and increases in psychological flexibility on daily ecological-sampling-style measures of both and validated questionnaires measuring stress [
35,
37,
46,
50]. It was predicted that the interventions would also lead to reductions in depression.
2. Materials and Methods
The following describes two studies trialling a single-session and two-session telehealth ACT intervention, respectively, and commences with methodological and analytic detail shared by both studies. This is followed by methodological detail, results, and discussion specific to studies one and two, respectively.
2.1. Design
The present study employed a single-case experimental design (SCED) wherein each participant is treated as an individual study. In doing this, SCEDs provide evidence of the effectiveness of interventions, drawing on substantially fewer participants than nomothetic approaches (such as RCTs) [
51,
52,
53,
54,
55,
56,
57,
58]. The specific SCED employed was randomized multiple baseline designs with the temporal staggering and randomized onset of intervention. Under this design, experimental control is demonstrated when change is evident in the data across participants with staggered intervention starting points [
59]. The independent variable for each participant was the pre–post intervention stage. As per Kratochwill and Levin, the onset of the ACT intervention was randomized across a 5- to 7-day period [
60]. The dependent variables were stress and psychological flexibility (experiential avoidance in study 1). Participants reported stress and psychological flexibility daily for a minimum of two weeks and three weeks, respectively, before intervention and for up to 10 weeks post-intervention via two to four Likert-style items.
2.2. Randomization
The temporal onset of ACT interventions was randomized with the aid of the web-based tool “Research Randomizer” [
61]. Randomization was performed by the first author while naive to the participant’s stress scores or clinical presentation. On occasion, it was necessary to breach the randomized order of intervention delivery to ensure the timely progression of the research and to minimize the burden on participants. Typically, this occurred due to participant illness and/or hospitalization.
2.3. Institutional Context and Ethics
The present SCEDs were conducted at a single academic teaching hospital in Dublin, Ireland, between October 2019 and August 2021. The teaching hospital in question hosts the Centre for Colorectal Disease and is considered a centre of excellence in the treatment and management of colorectal diseases including IBD. At the time of participation, all participants received care at the hospital’s gastroenterology service.
Ethical approval was granted by the institutional ethics committee (at Saint Vincent’s University Hospital Dublin, Dublin, Ireland) and exemptions from full ethical review were granted at University College Dublin, Dublin, Ireland (HS-E-19-112; HS-E-21-63).
2.4. Inclusion and Exclusion Criteria
Prospective participants aged 18–65 with mild stress or above as measured by the DASS-21 and a histological and radiological diagnosis of Crohn’s disease or ulcerative colitis were eligible to participate [
62]. Prospective participants were excluded from participation if they had previously participated in research trialling an ACT intervention.
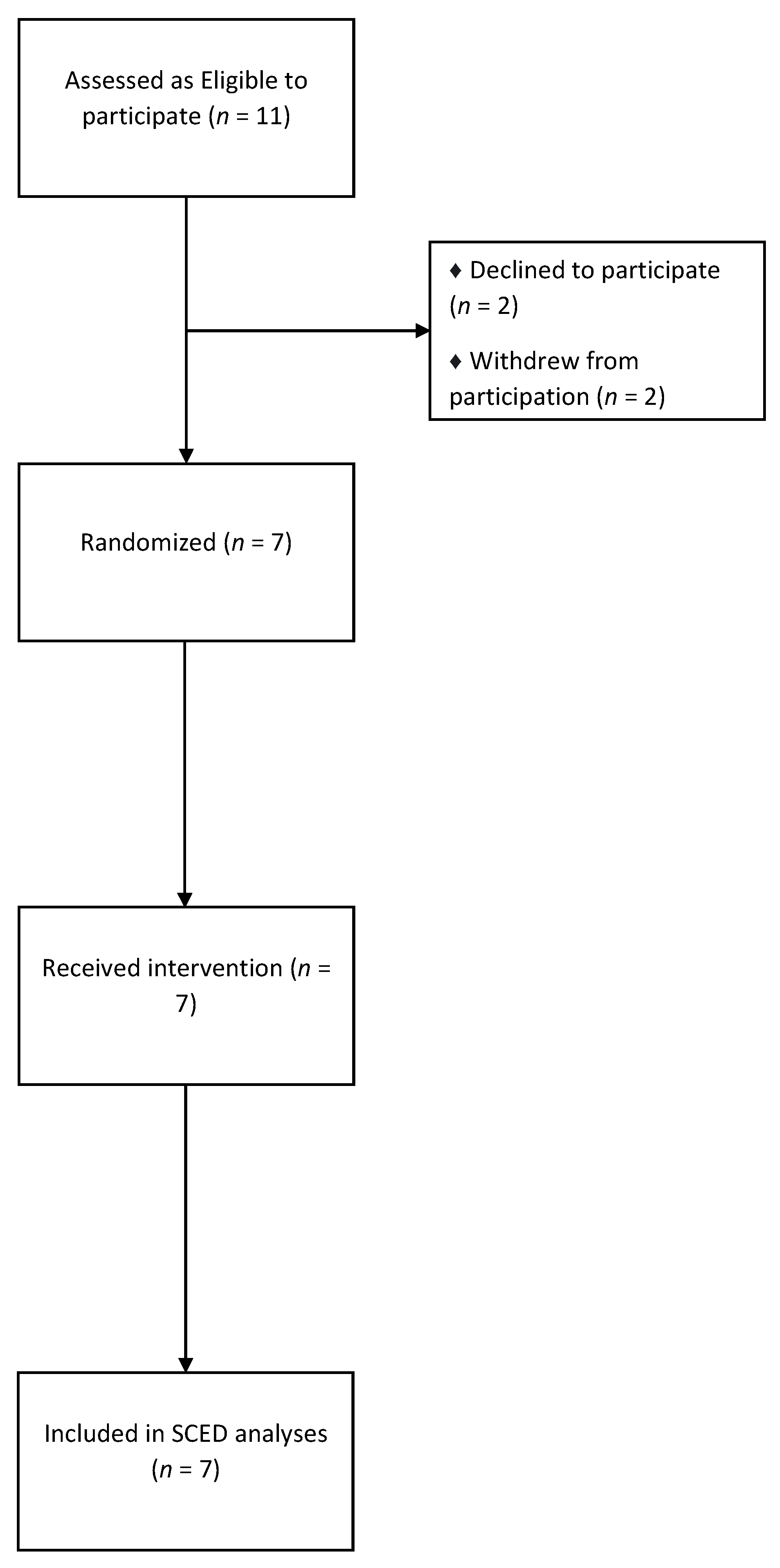
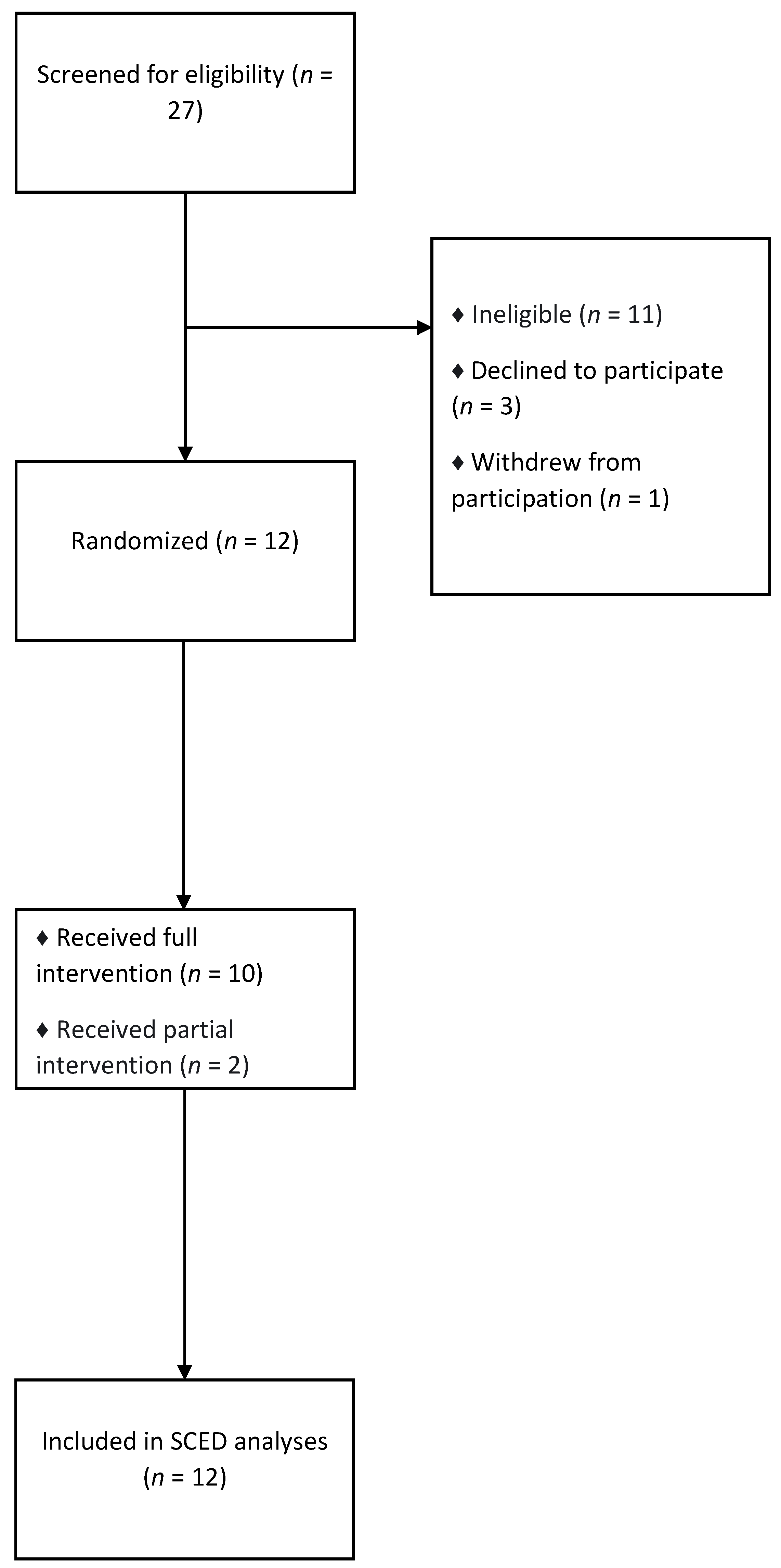
2.5. Recruitment
Recruitment was led by IBD specialists at the above-named academic teaching hospital in September 2019 and January 2021. Said IBD specialists were briefed by the first, second, and second-last authors regarding inclusion and exclusion criteria and participation activities. Said IBD specialists subsequently broached participation with those attending their clinics. It was made clear to all prospective participants that refusal to participate would not impact their care in any manner. Those who remained interested were screened per the stress inclusion criteria with those eligible being permitted a further week to consider participation.
2.6. Measures of Stress
Two measures of stress were employed in both experiments, namely DASS-21 and an adapted “Stressometer”. DASS-21 was administered on three occasions: screening, week zero (immediately before study commencement; pre-study from hereon in), and at the end of the study. The adapted “Stressometer” was completed daily in an ecological-sampling-style format with the measure and response delivered via SMS [
50].
2.6.1. Depression Anxiety Stress Scale (DASS-21)
The DASS-21 was employed as a measure of stress, depression, and anxiety. The measure includes three seven-item scales assessing each construct. Respondents report the extent to which they experienced various symptoms of stress, depression, and anxiety over the past week on a four-point Likert scale. Responses ranged from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time) with the measure taking approximately ten minutes to complete. The measure has been observed to be valid, reliable (depression subscale α = 0.96, anxiety subscale α = 0.89, and stress subscale α = 0.93), and have a well-supported three-factor structure, and has been trialled in clinical and non-clinical populations [
62,
63,
64,
65].
2.6.2. Adapted Stressometer
An adapted form of the “Stressometer” was employed to assess stress daily in an ecological-sampling-style manner. As such, the measure was intended to capture stress in vivo while also minimizing the assessment burden (taking less than one minute to complete). The “Stressometer” is a validated and responsive measure of stress in people with IBD [
66]. The adapted measure read as follows:
Please reply with the number between 0 and 10 that best describes the stress you have experienced today (where a score of 0 indicates “No stress” and a score of 10 indicates “Extreme Stress”).
2.7. Treatment Integrity
Intervention protocols were developed by the first, third, and last authors. All three have experience in delivering ACT interventions, and authors one and three have completed 18-month trainings in ACT and mindfulness-based interventions (MBIs) and training in counselling and clinical skills. The last author is a peer-reviewed ACT trainer who provided their expertise during protocol development and provided supervision to the first author during study 1 and to the first and third authors during study 2.
In addition to the above steps to maximize treatment integrity, audio recordings of intervention sessions were kept with participant consent. Randomly selected sessions were subsequently assessed for treatment fidelity using the ACT Fidelity Measure (ACT-FM) [
67]. The assessor (a member of the Contextual Behavioural Science lab coordinated by the last author but not an author of the present manuscript) was also experienced in ACT and had completed an 18-month training in ACT and MBIs. Sessions were rated as demonstrating a high presence of ACT-consistent interventionist behaviour and a low presence of ACT-inconsistent behaviour.
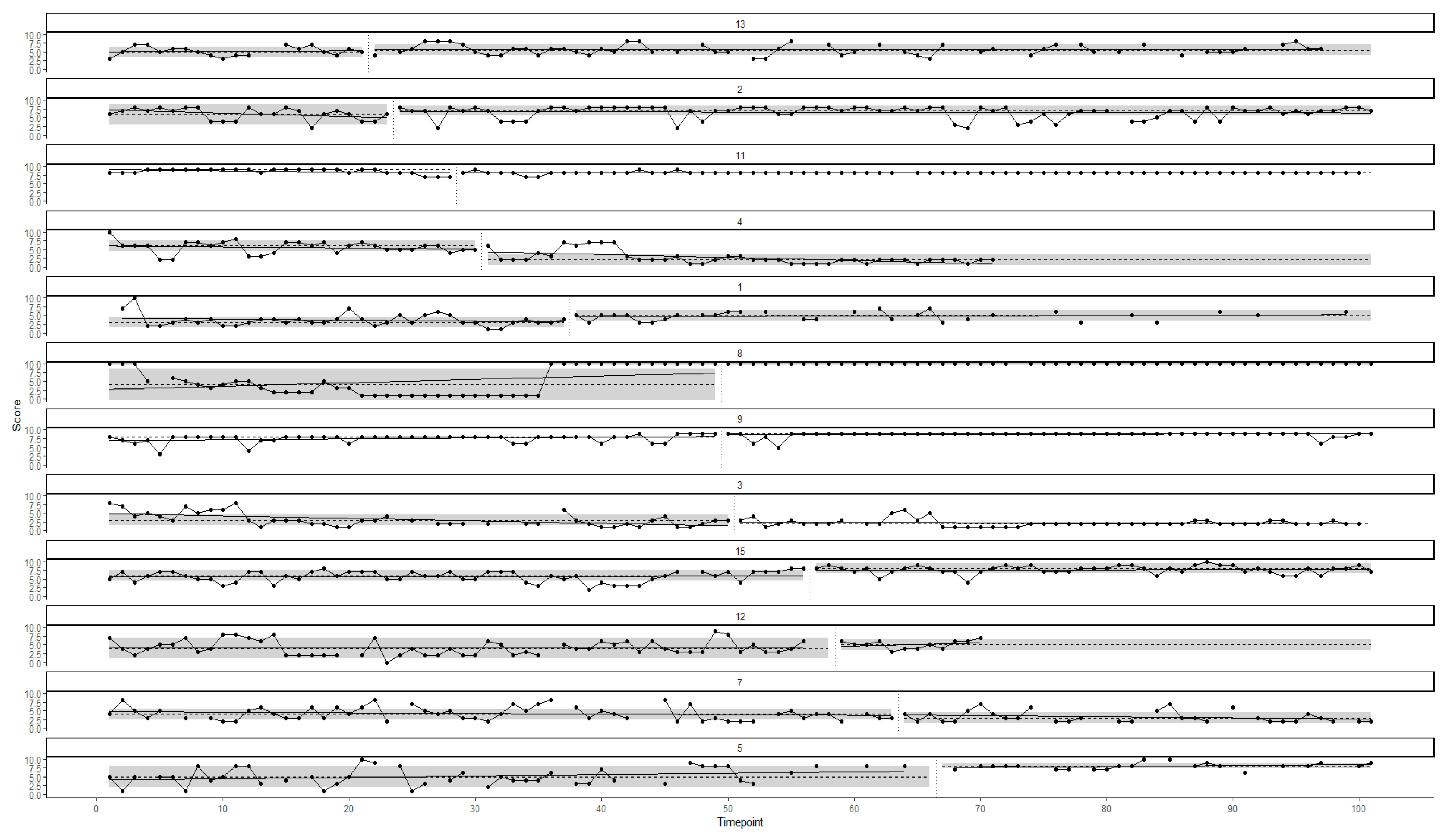
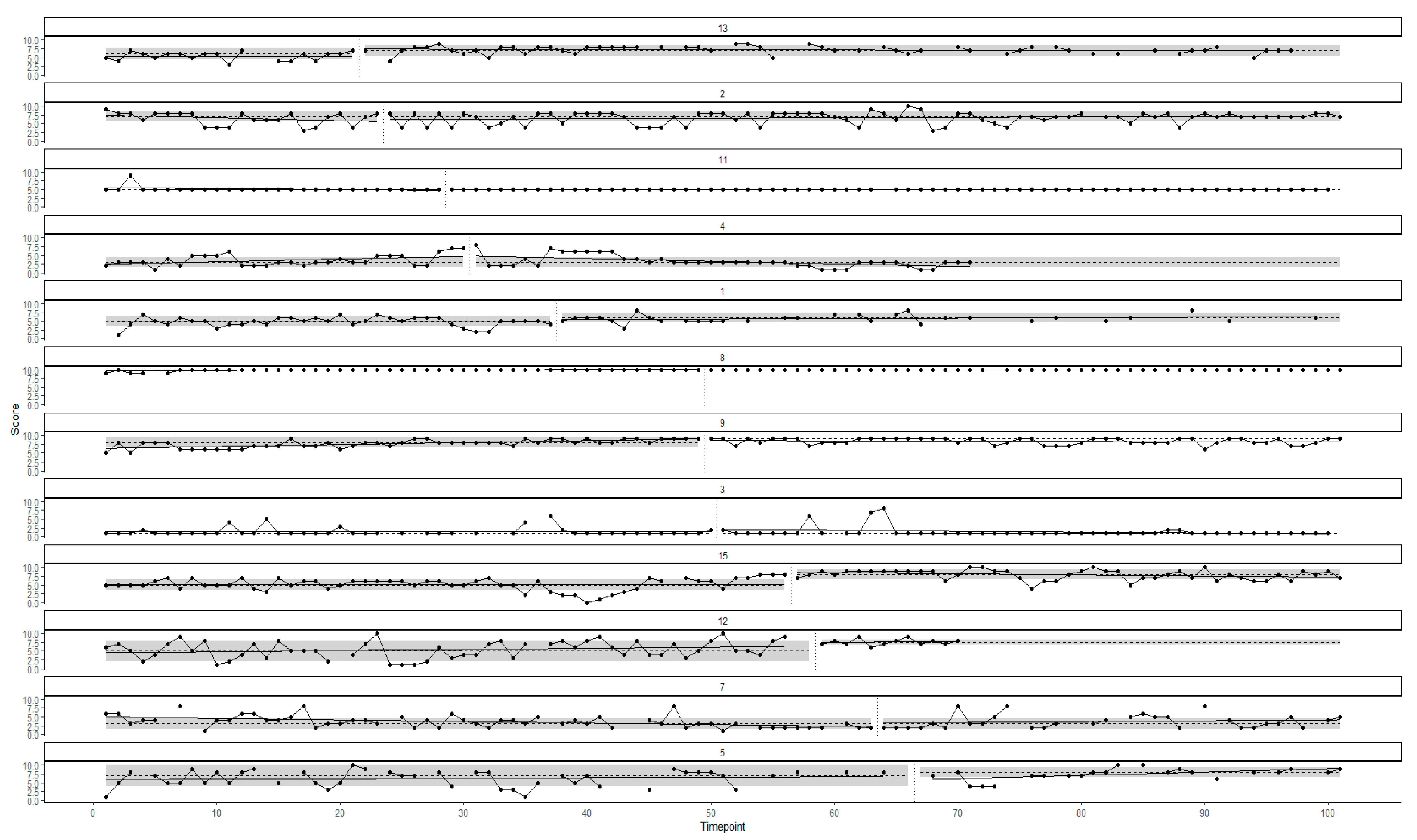
2.8. Analytic Strategy
2.8.1. SCED Analysis
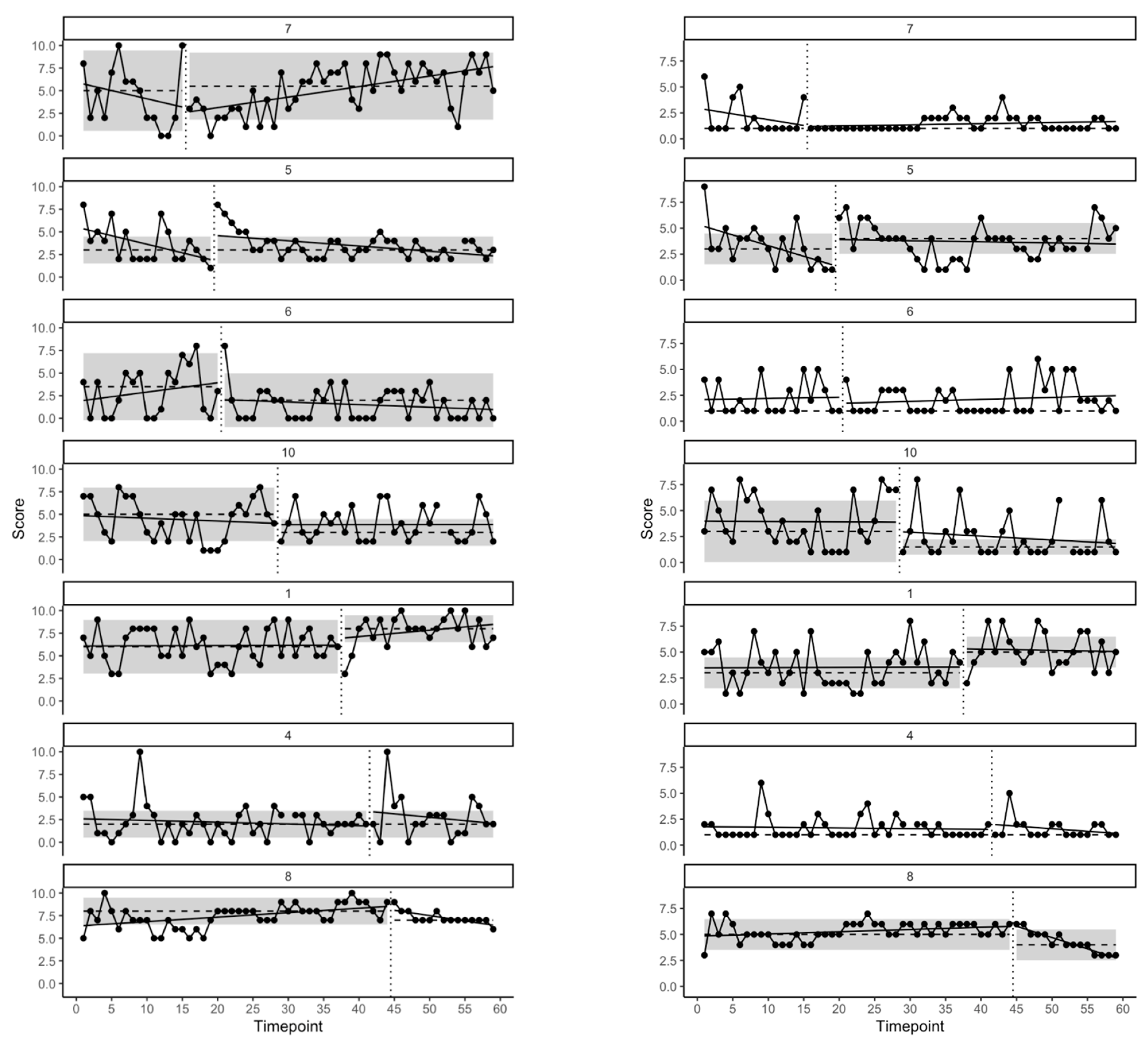
SCED analyses were conducted using the R packages SCED and metafor, which facilitates accessible and robust visualization, analysis, and meta-analysis of A-B SCED data while minimizing researcher degrees of freedom [
68,
69]. A full discussion of the analyses carried out via the R SCED package is available via Hussey and Eswara Murthy et al., and will be summarized here [
68,
70]. To enable visual assessment of between-phase difference, baseline trends, and phase variability, raw data including OLS regression trend lines, median values per phase, and median absolute deviation of scores within each phase were plotted through an in-built function in the SCED package. Given the poor inter-rater reliability of visual assessment of intervention effects through visual analysis, the SCED package also permits quantitative analysis of data [
71,
72]. As such the package calculates
p values via robust, non-parametric permutation tests and calculates three robust effect sizes (for a primer on commonly reported effect sizes in SCED research see Parker et al.): median difference between conditions, Ruscio’s A (also known as the Common Language Effect Size, the Probability of Superiority, and Nonoverlap All Pairs), and Hedge’s
g [
73,
74,
75,
76,
77,
78,
79].
Finally, a random-effects meta-analysis was conducted via the R packages SCED and metafor [
68,
69]. Following standard meta-analytic practices, the SCED package calculates 95% confidence intervals on the meta effect size, metrics of heterogeneity, and 95% credibility intervals on the effect size [
68,
70].
2.8.2. Clinically Significant Change (CSC)
Clinically significant and reliable changes in depression, anxiety, stress, experiential avoidance, and psychological flexibility were assessed per Jacobson and Truax’s (1991) guidelines via The Leeds Reliable Change Indicator [
80,
81,
82]. Reliable and clinically significant changes were calculated using available psychometric and normative data. Reliable change was observed wherein a participant’s score was increased or reduced by 1.96 standard deviations at post-study. CSC was achieved when a reliable change was observed, and the participant’s score had crossed a cut-off point denoting that their post-intervention score on the measure in question was now closer to the mean of a non-clinical population than that of a clinical population.
2.8.3. Missing Data
Missing data varied across studies and participants from 0% missingness to 35% missingness. Data analysis was conducted using available data. Given the substantial number of datapoints (59 and 101 per participant in studies 1 and 2, respectively) it was deemed that there were sufficient data to assess the effect of the intervention despite the presence of missingness. Moreover, a clear consensus to address missing data in SCEDs does not yet exist nor does it feature under the SCRIBE reporting guidelines or risk of bias tools for SCEDs [
83,
84,
85,
86].
5. Discussion
Study 2 employed a randomized multiple baseline design to investigate the effectiveness of a two-session telehealth ACT intervention supplemented by an ACT-based workbook and phone call consultation for IBD. It was predicted that the ACT intervention would produce reductions in stress and promote increased engagement in openness to internal experiences, awareness, and valued action. At the individual level, 6 of 12 participants demonstrated reduced stress (participants 3, 4, 7, 8, 9, and 15; 50%), 5 of 12 demonstrated increased openness to experience (participants 1, 2, 5, 13, and 15; 42%), 6 of 12 demonstrated increased awareness (participants 1, 5, 9, 11, 13, and 15; 50%), and 7 of 12 demonstrated increased engagement in valued action (participants 1, 5, 8, 9, 12, 13, and 15; 58%) on single-item measures of stress and PF. Moreover, three participants (participants 1, 2, and 15) demonstrated reliable improvements in DASS-21 measured stress (which was clinically significant for participant 15). Participant two demonstrated a reliable improvement in anxiety. Neither reliable nor clinically significant changes were evident in DASS-21-measured depression, and facets of CompACT-measured PF. Deteriorations were evident for 4 of 12 participants (participants 3, 4, 7, and 11; 33.33%) and 2 of 12 participants (participants 4 and 7; 17%) on single-item-measured openness to experience and awareness, respectively. However, findings must be approached with caution given significant missing data for some participants (participants 1, 4, 12, and 13) and the minimal variation in participant 8’s data. Meta-analysis across participants suggested reductions in stress and increased valued action as a function of the intervention.
Improvements in openness to experience, awareness, and particularly stress and valued action are broadly congruent with the existing literature on brief interventions and improvements early in therapy. For example, sudden improvements for 40 to 60% of clients following brief interventions and initial therapy sessions are a well-observed effect in the cognitive behavioural therapies [
41,
42,
43,
44]. While ostensibly used as a measure of valued action, the single-item measure of the same also functioned as a proxy for functioning. Given this, we suggest that the intervention functioned to decrease stress and increase functioning and is congruent with previous research on brief ACT interventions [
34,
35,
92]. Moreover, these findings seem conceptually congruent with findings linking increased valued action (and reduced avoidance functioning behaviour) with improved psychological health and functioning in IBD and chronic conditions [
33,
100,
102,
103].
Despite between 40% and 58% of participants experiencing improvements across various stress and psychological flexibility outcomes, many participants experienced minimal change or saw deterioration following exposure to the ACT intervention. While assumed to be exclusively beneficial, psychological, and behavioural therapies may on occasion confer deterioration and harm [
104,
105,
106]. While the present study is not well placed to ascertain factors and processes associated with improvement and deterioration, we note that adherence to treatment protocol and content may have influenced deterioration. That is, for some participants deterioration occurred in context of poorer adherence or not having engaged in all intervention components. Regarding the absence of changes, we note that in some cases change may have been obfuscated by that participant’s dropout. That is, treatment effects may have emerged had the participant continued to report data throughout the study period. In other cases, participants experienced improvement between screening and the start of the study, potentially causing a floor effect. For example, participant 11 presented at the start of the study with higher psychological flexibility relative to most other participants and had moved into the normal range for stress (i.e., had met inclusion criteria at screening but no longer met the same at the study’s start). Lastly, we note that the presence of baseline improvement trends may, on occasion, have obfuscated improvement and deterioration as a function of the intervention. Such trends may follow from assessment wherein assessment functions as an intervention. For example, reporting low engagement in valued action may elicit dissonance for an individual and motivate greater engagement in valued action on the subsequent day(s) [
107,
108]. While ineffectiveness and deterioration occurred following the intervention, we argue that adherence to protocol, dropout, and improvement trends in response to assessment as plausible and competing explanations for these effects being the function of the ACT intervention.
While approximately half of the participants experienced improvements in stress and valued action, these trends were not reliably matched by reliable and clinically significant changes in DASS-21-measured stress and CompACT-measured PF. This discordance between daily single-item indices of stress and PF and established measures of the same suggests that changes in single-item measures were of a small magnitude. While changes for some participants were statistically significant, these changes may not be associated with clinically meaningful change. However, it could be argued that a change of this magnitude such that participants’ scores fall into the range of healthy peers may be unreasonable given the persistence and impact of lifelong illness in the form of IBD [
80]. Moreover, a change of a smaller magnitude may still confer personally meaningful benefits and facilitate more purposeful and vital living in the context of long-term illness.
5.1. Strengths and Limitations
The strengths of the present studies centre on the design used and the approach to data sampling. Firstly, single-case experimental designs facilitated the investigation of two novel and brief ACT interventions. Given the novel nature of the interventions and the paucity of evidence for their use in populations of people with IBD, it was important to be enabled to assess both the benefit and risk conferred by exposure to the brief interventions. Such investigations (especially of risk) are typically not feasible via nomothetic group-based designs [
55]. Moreover, the use of concurrent baselines minimized the effect of factors such as the passage of time and maturation [
109]. Lastly, the collection of daily self-reported stress, EA, and PF at specified times (i.e., ecological momentary assessment) increased ecological validity and minimized biases such as recall bias which may impact other types of self-report measures [
50]. Such phenomena and the variables of study were measured as they occurred or in close temporal proximity to their occurrence rather than retrospectively (as is the case with measures such as the DASS-21).
A limitation of the present study was the absence of a comparator intervention. As such, improvement may simply reflect the receipt of an intervention rather than the active components of the intervention being studied. However, we argue that the findings of study 1 attenuate this limitation somewhat given that the delivery of an intervention, in that case, did not convey significant improvement. A second limitation was that existing psychological diagnoses and the receipt of psychological support were not screened for. No participants disclosed existing conditions or the receipt of psychological therapy (e.g., via demographic questionnaires or to their interventionist); however, some may have chosen not to disclose this information. As such, some effectiveness or lack thereof of the interventions trialled under studies 1 and 2 may be attributable to concurrent therapies and undisclosed mental health conditions. While not a limitation per se, an important caveat to the findings of study 2 was the evolving COVID-19 situation. As noted under
Section 4.1.2, some improvement may have been attributable to the easing of restrictions on social and economic life.
A further limitation centres on the generalizability of findings. While adequately powered for SCED methodology and employing a relatively large number of participants and data points (many SCEDs include three or fewer participants and three datapoints per phase), the samples for studies 1 and 2 remain relatively small and homogenous (participants were predominantly young adults and female) [
83,
84]. While the meta-analysis of effects across participants enhances generalizability somewhat, larger studies and further replications are necessary to afford greater generalizability. Moreover, generalizability and replicability may be hampered by the single-item measures used. At present, little consensus exists with respect to measurement in SCEDs, which impedes the comparison and generalizability of findings [
51]. As such, SCEDs may study the same or similar outcomes using different measures of outcomes, hampering the generalizability and synthesis of findings.
5.2. Implications and Future Research
The present studies lend further evidence that brief, telehealth ACT interventions with blended delivery components including workbooks and phone consultations are feasible for people with long-term health conditions and, specifically, IBD. Moreover, the findings of study 2 suggest such brief, blended and remote interventions to be potentially efficacious.
The present study saw interventions delivered by interventionists with training in ACT and counselling and clinical skills. Interventionists, however, did not have recognized professional training in clinical psychology, psychotherapy, or counselling. As such, it may be feasible for psychology graduates or other allied health professionals to deliver this intervention (or similar interventions) within healthcare services catering to people with IBD. As such, future research should investigate the feasibility and efficacy of this approach to intervention delivery given the potential for improved access to psychological therapies for people with IBD.
Future research should replicate the methodology of the present studies and investigate the acceptability and efficacy of these and other blended components. For example, other adjuncts might include digital self-help programs, bibliotherapy, or chatbot-delivered interventions. Lastly, further research is necessary to elucidate factors that influence suitability for brief interventions. As observed in study 2, approximately 40% to 58% of people with IBD may benefit from a brief ACT intervention. Future research is necessary to better identify those who may benefit most to facilitate the prescription of the same.