PTSD Symptoms and Coping with COVID-19 Pandemic among Treatment-Seeking Veterans: Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Demographics and War-Related Characteristics
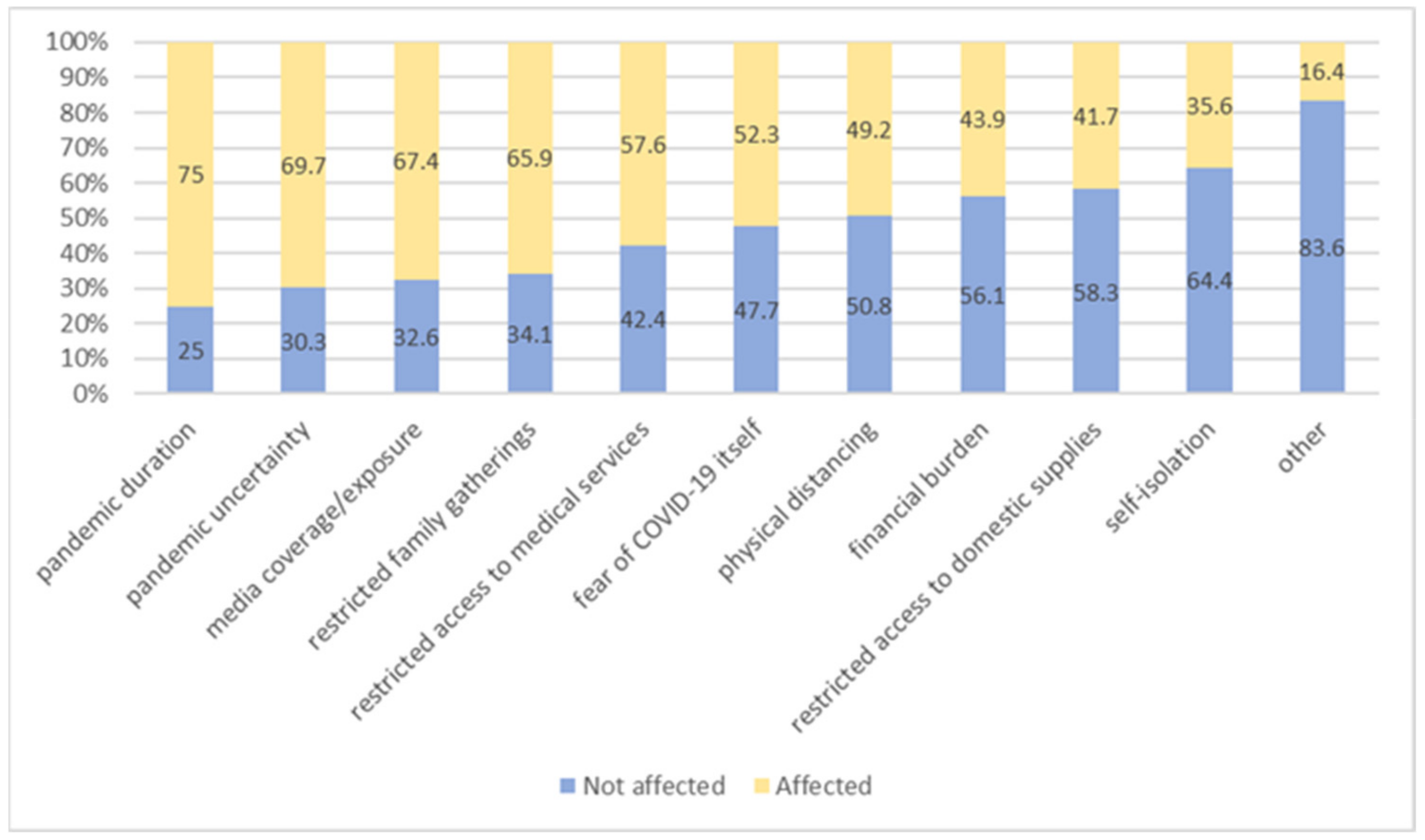
3.2. COVID-19 Related Characteristics
3.3. PTSD Symptom Severity
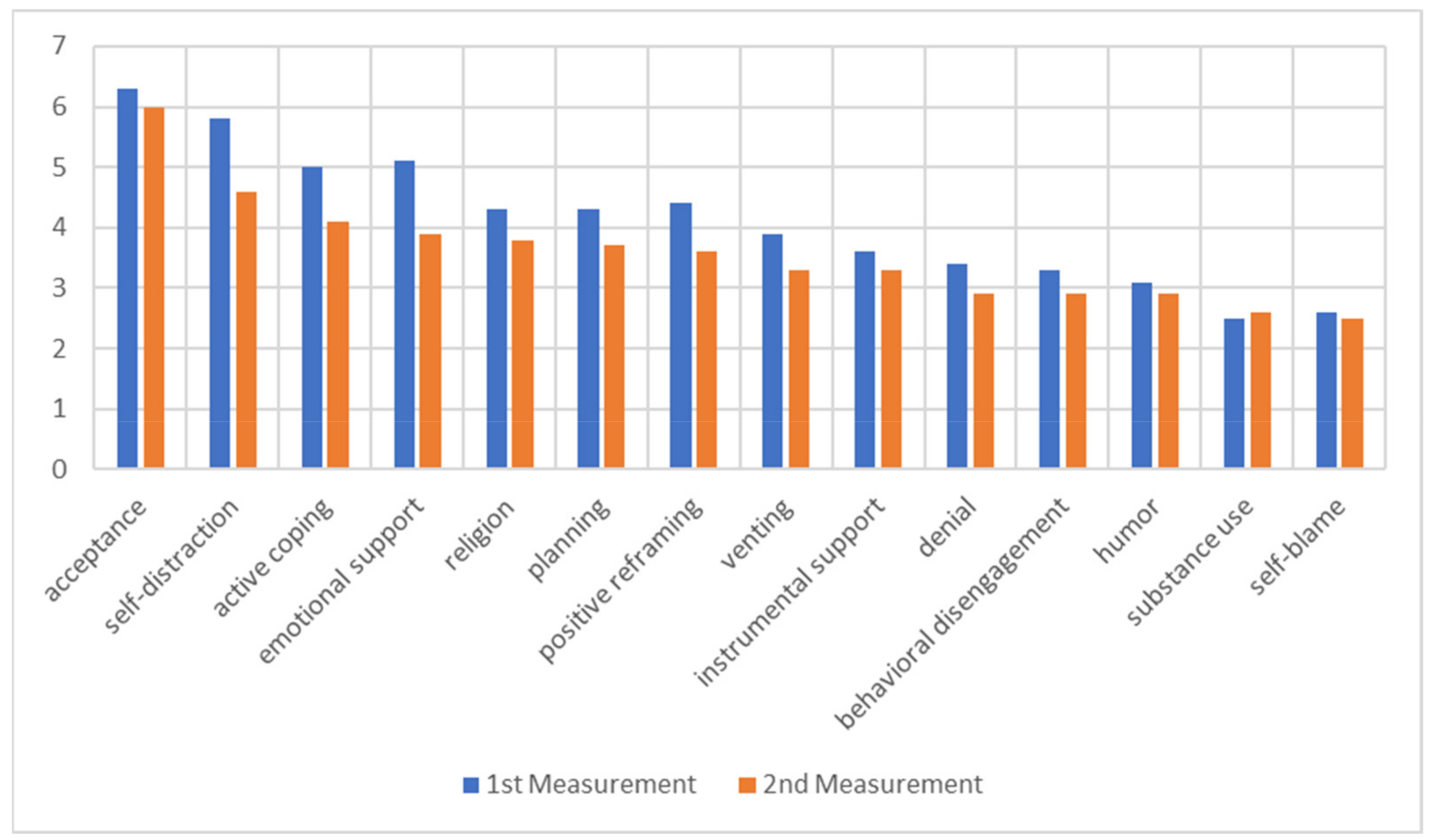
3.4. Coping with COVID-19-Related Issues
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gersons, B.P.R.; Smid, G.E.; Smit, A.S.; Kazlauskas, E.; McFarlane, A. Can a ‘second disaster’ during and after the COVID-19 pandemic be mitigated? Eur. J. Psychotraumatol. 2020, 11, 1815283. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, Y.; Nagarajan, R.; Saya, G.K.; Menon, V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020, 293, 113382. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Emodi-Perlman, A.; Eli, I.; Uziel, N.; Smardz, J.; Khehra, A.; Gilon, E.; Wieckiewicz, G.; Levin, L.; Wieckiewicz, M. Public Concerns during the COVID-19 Lockdown: A Multicultural Cross-Sectional Study among Internet Survey Respondents in Three Countries. J. Clin. Med. 2021, 10, 1577. [Google Scholar] [CrossRef]
- Campion, J.; Javed, A.; Sartorius, N.; Marmot, M. Addressing the public mental health challenge of COVID-19. Lancet 2020, 7, 657–659. [Google Scholar] [CrossRef]
- Holman, E.A.; Thompson, R.R.; Garfin, D.R.; Silver, R.C. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Sci. Adv. 2020, 6, eabd5390. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021, 136, 603–609. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Tsai, J.; Southwick, S.M. Association of symptoms of posttraumatic stress disorder with posttraumatic psychological growth among US veterans during the COVID-19 pandemic. JAMA 2021, 4, e214972. [Google Scholar] [CrossRef]
- Nichter, B.; Hill, M.L.; Na, P.J.; Kline, A.C.; Norman, S.B.; Krystal, J.H.; Southwick, S.M.; Pietrzak, R.H. Prevalence and trends in suicidal behavior among US Military veterans during the COVID-19 pandemic. JAMA 2021, 78, 1218–1227. [Google Scholar] [CrossRef]
- Hill, M.L.; Nichter, B.; Na, P.J.; Norman, S.B.; Morland, L.A.; Krystal, J.H.; Pietrzak, R.H. Mental health impact of the COVID-19 pandemic in U.S. military veterans: A population-based, prospective cohort study. Psychol. Med. 2021, 1–12. [Google Scholar] [CrossRef]
- Hendrikx, L.J.; Williamson, C.; Baumann, J.; Murphy, D. The impact of the COVID-19 pandemic on treatment-seeking veterans in the United Kingdom with preexisting mental health difficulties: A longitudinal study. J. Trauma. Stress 2022, 35, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Letica-Crepulja, M.; Stevanović, A.; Grković, J.; Rončević-Gržeta, I.; Jovanović, N.; Frančišković, T. Posttraumatic stress disorder symptoms and coping with the lockdown among help-seeking veterans before and during the COVID-19 pandemic. Croat. Med. J. 2021, 62, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Nemeroff, C.B.; Bremner, J.D.; Foa, E.B.; Mayberg, H.S.; North, C.S.; Stein, M.B. Posttraumatic stress disorder: A state-of-the-science review. J. Psychiatr. Res. 2006, 40, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Badour, C.L.; Blonigen, D.M.; Boden, M.T.; Feldner, M.T.; Bonn-Miller, M.O. A longitudinal test of the bi-directional relations between avoidance coping and PTSD severity during and after PTSD treatment. Behav. Res. Ther. 2012, 50, 610–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, V.J.; Boykin, G.; Jeter, A.; Villarreal, J. How do I handle my life now? Coping and the post traumatic stress disorder checklist—Military version. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2014, 58, 1252–1256. [Google Scholar] [CrossRef]
- Croatian Institute of Public Health. Indicators of Health Status and Use of Health Care of Croatian Veterans of the Homeland War—The State of 2020 [Translated Title]. Croatian Institute of Public Health. 2021. Available online: https://www.hzjz.hr/wp-content/uploads/2021/09/Branitelji_2020.pdf (accessed on 4 April 2021).
- Letica-Crepulja, M.; Stevanović, A.; Protuđer, M.; Grahovac Juretić, T.; Rebić, J.; Frančišković, T. Complex PTSD among treatment-seeking veterans with PTSD. Eur. J. Psychotraumatol. 2020, 11, 1716593. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. Available online: www.ptsd.va.gov (accessed on 15 March 2020).
- Gray, M.J.; Litz, B.T.; Hsu, J.L.; Lombardo, T.W. Psychometric properties of the life events checklist. Assessment 2004, 11, 330–341. [Google Scholar] [CrossRef] [Green Version]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef]
- Sveen, J.; Bondjers, K.; Willebrand, M. Psychometric properties of the PTSD checklist for DSM-5: A pilot study. Eur. J. Psychotraumatol. 2016, 7, 30165. [Google Scholar] [CrossRef] [Green Version]
- Wortmann, J.H.; Jordan, A.H.; Weathers, F.W.; Resick, P.A.; Dondanville, K.A.; Hall-Clark, B.; Foa, E.B.; Young-McCaughan, S.; Yarvis, J.S.; Hembree, E.A.; et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol. Assess. 2016, 28, 1392–1403. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Appl. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Margetić, B.; Peraica, T.; Stojanović, K.; Ivanec, D. Predictors of emotional distress during the COVID-19 pandemic; a Croatian study. Pers. Individ. Differ. 2021, 175, 10691. [Google Scholar] [CrossRef]
- Schock, K.; Böttche, M.; Rosner, R.; Wenk-Ansohn, M.; Knaevelsrud, C. Impact of new traumatic or stressful life events on pre-existing PTSD in traumatized refugees: Results of a longitudinal study. Eur. J. Psychotraumatol. 2016, 9, 32106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, D.C.; Boals, A.; Hoyle, R.H. Narrative centrality and negative affectivity: Independent and interactive contributors to stress reactions. J. Exp. Psychol. Gen. 2014, 143, 1159–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boals, A.; Ruggero, C. Event centrality prospectively predicts PTSD symptoms. Anxiety Stress Coping 2016, 29, 533–541. [Google Scholar] [CrossRef]
- Amsalem, D.; Lazarov, A.; Markowitz, J.C.; Gorman, D.; Dixon, L.B.; Neria, Y. Increasing treatment-seeking intentions of US veterans in the COVID-19 era: A randomized controlled trial. Depress. Anxiety 2021, 38, 639–647. [Google Scholar] [CrossRef]
- Lotzin, A.; Krause, L.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Arnberg, F.; Böttche, M.; Bragesjö, M.; Dragan, M.; Figueiredo-Braga, M.; et al. Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic: First results of the ESTSS COVID-19 pan-European ADJUST study. Eur. J. Psychotraumatol. 2021, 12, 1964197. [Google Scholar] [CrossRef]
- Sharp, M.L.; Serfioti, D.; Jones, M.; Burdett, H.; Pernet, D.; Hull, L.; Murphy, D.; Wessely, S.; Fear, N.T. UK veterans’ mental health and well-being before and during the COVID-19 pandemic: A longitudinal cohort study. Brit. Med. J. 2021, 11, e049815. [Google Scholar] [CrossRef]
- Murphy, D.; Williamson, C.; Baumann, J.; Busuttil, W.; Fear, N.T. Exploring the impact of COVID-19 and restrictions to daily living as a result of social distancing within veterans with pre-existing mental health difficulties. Brit. Med. J. Mil. Health 2020, 168, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Clohessy, S.; Ehlers, A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br. J. Clin. Psychol. 1999, 8, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Hooberman, J.; Rosenfeld, B.; Rasmussen, A.; Keller, A. Resilience in trauma exposed refugees: The moderating effect of coping style on resilience variables. Am. J. Orthopsychiatry 2010, 80, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Linley, P.A.; Joseph, S. Positive change following trauma and adversity: A review. J. Trauma. Stress 2004, 17, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Mahar, A.; Reppas-Rindlisbacher, C.; Edgelow, M.; Siddhpuria, S.; Hallet, J.; Rochon, P.A.; Cramm, H. Concerns and coping strategies of older adult veterans in Canada at the outset of the COVID-19 pandemic. J. Mil. Veteran Fam. Health 2021, 7, e20210712. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Khubchandani, J.; Wiblishauser, M.J.; Price, J.H.; Webb, F.J. COVID-19 related information and psychological distress: Too much or too bad? Brain Behav. Immun. 2021, 12, 100213. [Google Scholar] [CrossRef]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef]
| The 1st Measurement Participants n = 176 | Statistics | |||
|---|---|---|---|---|
| Participants Assessed at T1 and T2 n = 132 | Participants Missing at T2 n = 44 | |||
| X (SD) | X (SD) | |||
| Age | 53.38 (6.39) | 54.16 (5.97) | t = −0.201 | p = 0.113 |
| n (%) | n (%) | |||
| Educational level | ||||
| Elementary school | 11 (8.3) | 4 (9.1) | χ2 = 0.042 | p = 0.979 |
| High school | 108 (81.8) | 36 (81.8) | ||
| Higher education | 13 (9.9) | 4 (9.1) | ||
| Work status | ||||
| Employed | 34 (25.8) | 6 (13.6) | χ2 = 4.658 | p = 0.097 |
| Unemployed | 16 (12.1) | 10 (22.7) | ||
| Retired | 82 (62.1) | 28 (63.6) | ||
| Marital status | ||||
| Married/cohabitating | 93 (70.5) | 36 (81.8) | χ2 = 2.767 | p = 0.429 |
| Single | 20 (15.2) | 5 (11.4) | ||
| Divorced | 16 (12.1) | 2 (4.5) | ||
| Other | 3 (2.3) | 1 (2.3) | ||
| Economic status (self-reported) | ||||
| High | 2 (1.5) | 0 (0) | χ2 = 0.762 | p = 0.683 |
| Medium | 83 (62.9) | 27 (61.4) | ||
| Low | 47 (35.6) | 17 (38.6) | ||
| X(SD) | X(SD) | |||
| Treatment duration (in years) | 17.8 (8.61) | 15.71 (8.55) | t = 1.370 | p = 0.173 |
| Deployment duration (in months) | 31.5 (19.43) | 30.86 (22.73) | t = 0.164 | p = 0.870 |
| Life events (LEC-5) | 10.04 (4.6) | 9.44 (4.34) | t = 0.748 | p = 0.455 |
| T1 | T2 | |||||
|---|---|---|---|---|---|---|
| Range | Mean (SD) | Range | Mean (SD) | t | p | |
| Cluster B symptoms (intrusion symptoms) | 2–20 | 13.31 (4.05) | 0–20 | 12.83 (4.60) | 1.081 | 0.282 |
| Cluster C symptoms (avoidance symptoms) | 2–8 | 5.84 (1.78) | 0–8 | 5.29 (2.24) | 2.380 | 0.019 |
| Cluster D symptoms (negative alterations in cognitions and mood) | 1–29 | 16.83 (6.49) | 0–32 | 15.45 (6.3) | 1.998 | 0.048 |
| Cluster E symptoms (alterations in arousal and reactivity) | 2–24 | 13.18 (4.84) | 2–24 | 12.41 (5.02) | 1.440 | 0.152 |
| PCL-5 total score | 16–75 | 47.24 (12.87) | 7–76 | 44.1 (14.09) | 2.234 | 0.027 |
| T1 | T2 | |||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | t | p | |
| Emotion focused | 4.64 (1.06) | 4.07 (1.01) | 4.718 | <0.001 |
| Problem focused | 4.31 (1.40) | 3.71 (1.57) | 3.589 | <0.001 |
| Dysfunctional | 3.51 (0.87) | 3.13 (0.96) | 3.447 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Letica-Crepulja, M.; Stevanović, A.; Palaić, D.; Vidović, I.; Frančišković, T. PTSD Symptoms and Coping with COVID-19 Pandemic among Treatment-Seeking Veterans: Prospective Cohort Study. J. Clin. Med. 2022, 11, 2715. https://doi.org/10.3390/jcm11102715
Letica-Crepulja M, Stevanović A, Palaić D, Vidović I, Frančišković T. PTSD Symptoms and Coping with COVID-19 Pandemic among Treatment-Seeking Veterans: Prospective Cohort Study. Journal of Clinical Medicine. 2022; 11(10):2715. https://doi.org/10.3390/jcm11102715
Chicago/Turabian StyleLetica-Crepulja, Marina, Aleksandra Stevanović, Diana Palaić, Iva Vidović, and Tanja Frančišković. 2022. "PTSD Symptoms and Coping with COVID-19 Pandemic among Treatment-Seeking Veterans: Prospective Cohort Study" Journal of Clinical Medicine 11, no. 10: 2715. https://doi.org/10.3390/jcm11102715
APA StyleLetica-Crepulja, M., Stevanović, A., Palaić, D., Vidović, I., & Frančišković, T. (2022). PTSD Symptoms and Coping with COVID-19 Pandemic among Treatment-Seeking Veterans: Prospective Cohort Study. Journal of Clinical Medicine, 11(10), 2715. https://doi.org/10.3390/jcm11102715






