Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Heart Failure: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Study Protocol
2.3. Outcome Measures
2.4. Statistical Analysis
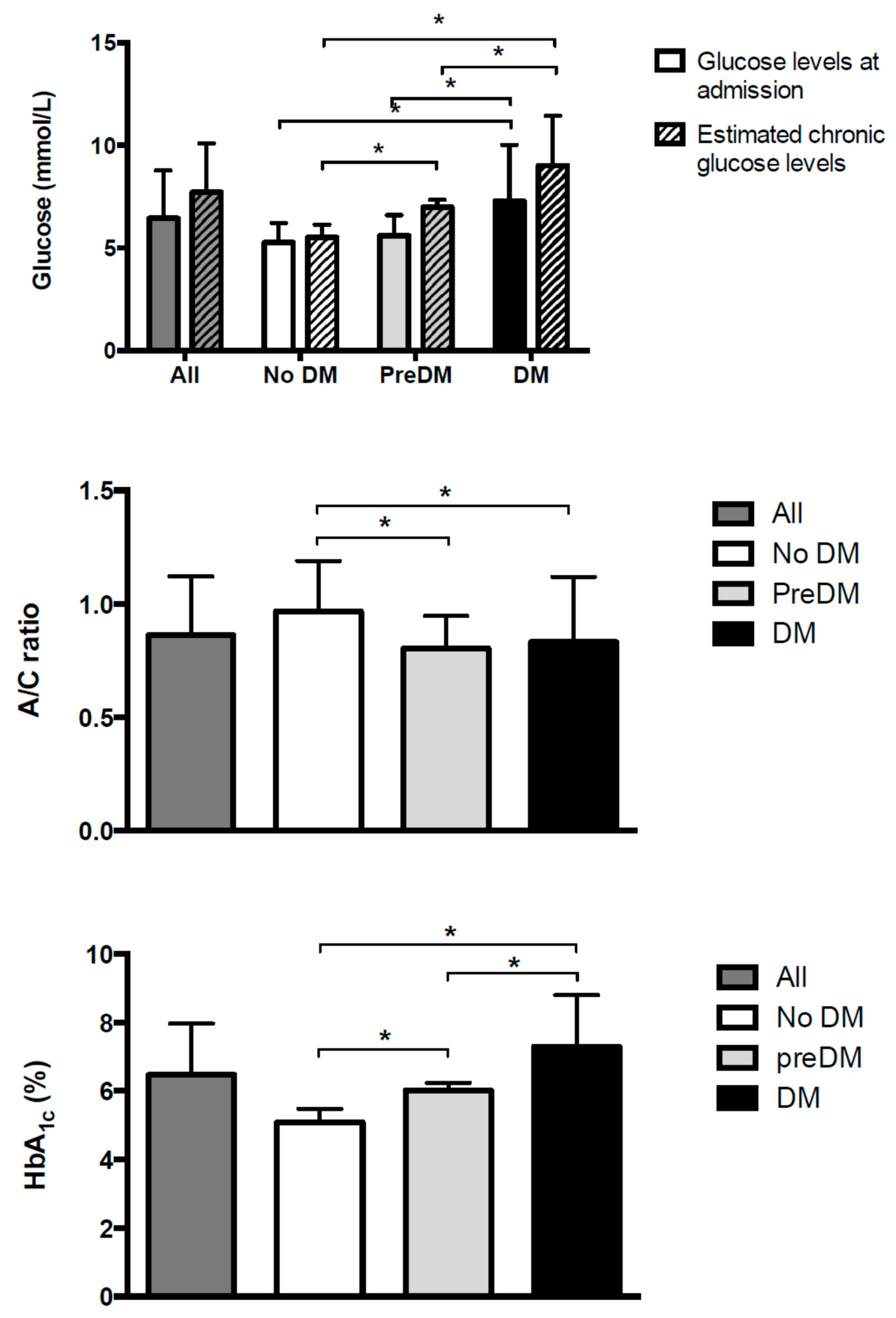
3. Results
3.1. Baseline Characteristics
3.2. Mortality during the Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef]
- Soriguer, F.; Goday, A.; Bosch-Comas, A.; Bordiú, E.; Calle-Pascual, A.; Carmena, R.; Casamitjana, R.; Castaño, L.; Castell, C.; Catalá, M.; et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: The Di@betes Study. Diabetologia 2012, 55, 88–93. [Google Scholar] [CrossRef] [Green Version]
- Rojo-Martínez, G.; Valdés, S.; Soriguer, F.; Vendrell, J.; Urrutia, I.; Pérez, V.; Ortega, E.; Ocón, P.; Montanya, E.; Menéndez, E.; et al. Incidence of diabetes mellitus in Spain as results of the nation-wide cohort di@betes study. Sci. Rep. 2020, 10, 2765. [Google Scholar] [CrossRef] [Green Version]
- Rawshani, A.; Rawshani, A.; Franzén, S.; Eliasson, B.; Svensson, A.-M.; Miftaraj, M.; McGuire, D.K.; Sattar, N.; Rosengren, A.; Gudbjörnsdottir, S. Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N. Engl. J. Med. 2017, 376, 1407–1418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kannel, W.B.; Hjortland, M.; Castelli, W.P. Role of diabetes in congestive heart failure: The Framingham study. Am. J. Cardiol. 1974, 34, 29–34. [Google Scholar] [CrossRef]
- Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.-M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; Rosengren, A.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Cavender, M.A.; Steg, P.G.; Smith, S.C.; Eagle, K.; Ohman, E.M.; Goto, S.; Kuder, J.; Im, K.; Wilson, P.W.; Bhatt, D.L. REACH Registry Investigators. Impact of Diabetes Mellitus on Hospitalization for Heart Failure, Cardiovascular Events, and Death. Circulation 2015, 132, 923–931. [Google Scholar] [CrossRef]
- Echouffo-Tcheugui, J.B.; Xu, H.; DeVore, A.D.; Schulte, P.J.; Butler, J.; Yancy, C.W.; Bhatt, D.L.; Hernandez, A.F.; Heidenreich, P.A.; Fonarow, G.C. Temporal trends and factors associated with diabetes mellitus among patients hospitalized with heart failure: Findings from Get With The Guidelines–Heart Failure registry. Am. Heart J. 2016, 182, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Gayat, E.; Lassus, J.; Meas, T.; Mueller, C.; Maggioni, A.; Peacock, F.; Spinar, J.; Harjola, V.P.; van Kimmenade, R.; et al. Association between elevated blood glucose and outcome in acute heart failure: Results from an international observational cohort. J. Am. Coll. Cardiol. 2013, 61, 820–829. [Google Scholar] [CrossRef] [Green Version]
- Helfand, B.K.I.; Maselli, N.J.; Lessard, D.M.; Yarzebski, J.; Gore, J.M.; McManus, D.D.; Saczynski, J.S.; Goldberg, R.J. Elevated serum glucose levels and survival after acute heart failure: A population-based perspective. Diabetes Vasc. Dis. Res. 2015, 12, 119–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, J.Y.; Kim, K.H.; Lee, S.E.; Cho, H.-J.; Lee, H.-Y.; Choi, J.-O.; Jeon, E.S.; Kim, M.S.; Kim, J.J.; Hwang, K.K.; et al. Admission Hyperglycemia as a Predictor of Mortality in Acute Heart Failure: Comparison between the Diabetics and Non-Diabetics. J. Clin. Med. 2020, 9, 149. [Google Scholar] [CrossRef] [Green Version]
- Itzhaki Ben Zadok, O.; Kornowski, R.; Goldenberg, I.; Klempfner, R.; Toledano, Y.; Biton, Y.; Fisman, E.Z.; Tenenbaum, A.; Golovchiner, G.; Kadmon, E.; et al. Admission blood glucose and 10-year mortality among patients with or without pre-existing diabetes mellitus hospitalized with heart failure. Cardiovasc. Diabetol. 2017, 16, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newton, J.D.; Squire, I.B. Glucose and haemoglobin in the assessment of prognosis after first hospitalisation for heart failure. Heart 2006, 92, 1441–1446. [Google Scholar] [CrossRef] [Green Version]
- Targher, G.; Dauriz, M.; Laroche, C.; Temporelli, P.L.; Hassanein, M.; Seferovic, P.M.M.; Drozdz, J.; Ferrari, R.; Anker, S.; Coats, A.; et al. In-hospital and 1-year mortality associated with diabetes in patients with acute heart failure: Results from the ESC-HFA Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2017, 19, 54–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marenzi, G.; Cosentino, N.; Milazzo, V.; Metrio, M.; De Cecere, M.; Mosca, S.; Rubino, M.; Campodonico, J.; Moltrasio, M.; Marana, I.; et al. Prognostic value of the acute-to-chronic glycemic ratio at admission in acute myocardial infarction: A prospective study. Diabetes Care 2018, 41, 847–853. [Google Scholar] [CrossRef] [Green Version]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T.; et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. J. Am. Med. Assoc. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Standards of medical care in diabetes-2010. Diabetes Care 2010, 33 (Suppl. 1), S11–S61. [CrossRef] [PubMed] [Green Version]
- Nathan, D.M.; Kuenen, J.; Borg, R.; Zheng, H.; Schoenfeld, D.; Heine, R.J. Translating the A1C assay into estimated average glucose values. Diabetes Care 2008, 31, 1473–1478. [Google Scholar] [CrossRef] [Green Version]
- Flores-Le Roux, J.A.; Comin, J.; Pedro-Botet, J.; Benaiges, D.; Puig-de Dou, J.; Chillarón, J.J.; Goday, A.; Bruguera, J.; Cano-Perez, J.F. Seven-year mortality in heart failure patients with undiagnosed diabetes: An observational study. Cardiovasc. Diabetol. 2011, 10, 39. [Google Scholar] [CrossRef] [Green Version]
- Fujino, M.; Ishihara, M.; Honda, S.; Kawakami, S.; Yamane, T.; Nagai, T.; Nakao, K.; Kanaya, T.; Kumasaka, L.; Asaumi, Y.; et al. Impact of acute and chronic hyperglycemia on in-hospital outcomes of patients with acute myocardial infarction. Am. J. Cardiol. 2014, 114, 1789–1793. [Google Scholar] [CrossRef]
- Ramon, J.; Llauradó, G.; Güerri, R.; Climent, E.; Ballesta, S.; Benaiges, D.; López-Montesinos, I.; Navarro, H.; Fernández, N.; Carrera, M.J.; et al. Acute-to-Chronic Glycemic Ratio as a Predictor of COVID-19 Severity and Mortality. Diabetes Care 2021, 44, dc211321. [Google Scholar] [CrossRef]
- Lee, A.K.; Warren, B.; Lee, C.J.; McEvoy, J.W.; Matsushita, K.; Huang, E.S.; Sharrett, A.R.; Coresh, J.; Selvin, E. The association of severe hypoglycemia with incident cardiovascular events and mortality in adults with type 2 diabetes. Diabetes Care 2018, 41, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.H.; Yandrapalli, S.; Aronow, W.S.; Jain, D.; Frishman, W.H.; Panza, J.A.; Cooper, H.A. Severe Hypoglycemia and Risk of Subsequent Cardiovascular Events: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Cardiol. Rev. 2020, 28, 244–249. [Google Scholar] [CrossRef]
- Amiel, S.A.; Aschner, P.; Childs, B.; Cryer, P.E.; de Galan, B.E.; Frier, B.M. International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: Epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol. 2019, 7, 385–396. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Miller, M.E.; Byington, R.P.; Goff, D.C., Jr.; Bigger, J.T.; Buse, J.B.; Cushman, W.C.; Genuth, S.; Ismail-Beigi, F.; Zoungas, S.; et al. Action to Control Cardiovascular Risk in Diabetes Study Group.Effects of Intensive Glucose Lowering in Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2545–2559. [Google Scholar] [CrossRef] [Green Version]
- ADVANCE Collaborative Group; Patel, A.; MacMahon, S.; Chalmers, J.; Neal, B.; Billot, L.; Woodward, M.; Marre, M.; Cooper, M.; Glasziou, P.; et al. Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, L.; Azad, N.; Bahn, G.D.; Ge, L.; Reaven, P.D.; Hayward, R.A.; Reda, D.J.; Emanuele, N.V.; VADT Study Group. Long-term follow-up of intensive glycaemic control on renal outcomes in the Veterans Affairs Diabetes Trial (VADT). Diabetologia 2018, 61, 295–299. [Google Scholar] [CrossRef] [Green Version]
- Meier, M.; Hummel, M. Cardiovascular disease and intensive glucose control in type 2 diabetes mellitus: Moving practice toward evidence-based strategies. Vasc. Health Risk Manag. 2009, 10, 859–871. [Google Scholar] [CrossRef] [Green Version]
- Arafah, B.M. Review: Hypothalamic pituitary adrenal function during critical illness: Limitations of current assessment methods. J. Clin. Endocrinol. Metab. 2006, 10, 3725–3745. [Google Scholar] [CrossRef] [Green Version]
- Carrasco-Sánchez, F.J.; Gomez-Huelgas, R.; Formiga, F.; Conde-Martel, A.; Trullàs, J.C.; Bettencourt, P.; Arévalo-Lorido, J.C.; Pérez-Barquero, M.M.; RICA, investigators. Association between type-2 diabetes mellitus and post-discharge outcomes in heart failure patients: Findings from the RICA registry. Diabetes Res. Clin. Pract. 2014, 104, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Farré, N.; Vela, E.; Clèries, M.; Bustins, M.; Cainzos-Achirica, M.; Enjuanes, C.; Moliner, P.; Ruiz, S.; Verdú-Rotellar, J.M.; Comín-Colet, J. Real world heart failure epidemiology and outcome: A population-based analysis of 88,195 patients. PLoS ONE 2017, 12, e0172745. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef]
- Neal, B.; Perkovic, V.; Mahaffey, K.W.; de Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R.; et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef] [Green Version]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef] [Green Version]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]



| All (n = 1062) | Patients without Diabetes (n = 278) | Patients with Pre-Diabetes (n = 194) | Patients with Diabetes (n = 590) | p for Trend | |
|---|---|---|---|---|---|
| Male sex (n, %) | 602 (56.7) | 153 (55.0) | 112 (57.7) | 337 (57.1) | 0.803 |
| Age (years) | 72.6 ± 11.2 | 71.2 ± 12.6 | 72.6 ± 13.2 | 73.2 ± 9.7 ¤ | 0.046 |
| Current smokers (n, %) | 157 (14.8) | 39 (14.0) | 34 (17.5) | 84 (14.2) | 0.786 |
| BMI (kg/m2) | 28.4 ± 5.9 | 27.2 ± 5.3 | 28 ± 6.5 | 29.1 ± 5.8 ¤ ¥ | <0.001 |
| Waist (cm) | 103.4 ± 14.2 | 98.9 ± 14.4 | 101.7 ± 13.8 | 105.9 ± 14.2 ¤ ¥ | <0.001 |
| Hypertension (n, %) | 862 (81.2) | 191 (68.7) | 153 (78.9) | 518 (87.8) * ¤ ¥ | <0.001 |
| Systolic blood pressure (mmHg) | 123.5 ± 22.0 | 120.1 ± 21.6 | 120.0 ± 22.2 | 126.1 ± 21.7 ¤ ¥ | <0.001 |
| Diastolic blood pressure (mmHg) | 67.2 ± 12.9 | 67.3 ± 13.2 | 66.6 ± 12.6 | 67.3 ± 12.8 | 0.768 |
| Dyslipidemia (n, %) | 593 (55.8) | 109 (39.2) | 81 (41.8) | 403 (68.3) ¤ ¥ | <0.001 |
| Statin use (n, %) | 633 (59.6) | 124 (44.6) | 101 (52.1) | 408 (69.2) * ¤ ¥ | <0.001 |
| Total cholesterol (mmol/L) | 3.92 ± 0.99 | 4.14 ± 1.04 | 4.08 ± 0.97 | 3.77 ± 1.03 ¤ ¥ | <0.001 |
| LDL-C (mmol/L) | 2.22 ± 0.80 | 2.43 ± 0.81 | 1.55 ± 0.78 | 2.08 ± 0.78 ¤ ¥ | <0.001 |
| HDL-C (mmol/L) | 1.10 ± 0.32 | 1.13 ± 0.33 | 1.17 ± 0.28 | 1.07 ± 0.33 ¥ | <0.001 |
| Triglycerides (mmol/L) | 1.40 ± 0.66 | 1.40 ± 0.74 | 1.30 ± 0.54 | 1.44 ± 0.66 ¥ | 0.049 |
| COPD (n, %) | 237 (22.3) | 51 (18.3) | 44 (22.7) | 142 (24.1) | 0.152 |
| Previous stroke (n, %) | 119 (11.2) | 28 (10.1) | 18 (9.2) | 73 (12.4) | 0.379 |
| Peripheral vasculopathy (n, %) | 176 (16.6) | 33 (11.9) | 21 (10.8) | 122 (20.7) ¤ ¥ | <0.001 |
| Laboratory values | |||||
| Creatinine (mmol/L) | 0.12 ± 0.06 | 0.12 ± 0.05 | 0.011 ± 0.05 | 0.12 ± 0.07 ¥ | 0.004 |
| eGFR MDRD < 60 (mL/min/1.73m2) | 277 (26.1) | 61 (21.9) | 35 (18.0) | 18 (3.1) ¤ ¥ | <0.001 |
| Hemoglobin (g/L) | 12.6 ± 2.8 | 12.7 ± 1.9 | 12.9 ± 2.1 | 13.4 ± 3.3 | 0.047 |
| Albumin (g/dL) | 3.78 ± 0.48 | 3.78 ± 0.45 | 3.90 ± 0.51 | 3.76 ± 0.48 * ¥ | 0.001 |
| NT-proBNP (pg/mL) | 1626 (700–4051) | 1412 (639–3425) | 1537 (652–3246) | 1775 (719–4456) | 0.103 |
| LVEF ≤40% (n, %) | 485 (45.7) | 144 (51.8) | 81 (41.8) | 260 (44.1) | 0.057 |
| NYHA class (n, %) | 0.011¤ | ||||
| -Class l | 146 (13.7) | 38 (13.7) | 45 (23.2) | 65 (11.0) | |
| -Class II | 440 (41.4) | 128 (46.0) | 70 (36.1) | 240 (40.8) | |
| -Class III | 388 (36.5) | 94 (33.8) | 58 (29.9) | 236 (40.0) | |
| -Class IV | 88 (8.3) | 18 (6.5) | 21 (10.8) | 49 (8.3) | |
| HF etiology (n, %) | <0.001 | ||||
| -Ischemic | 428 (40.3) | 83 (29.9) | 60 (30.9) | 285 (48.3) ¤ ¥ | |
| -Hypertensive | 372 (35.0) | 94 (33.8) | 72 (37.1) | 206 (34.9) | |
| -Others | 262 (24.7) | 101 (36.3) | 62 (32.0) | 189 (32.0) | |
| Atrial fibrillation (n, %) | 354 (33.3) | 100 (36.0) | 74 (38.1) | 180 (30.5) | 0.083 |
| Implantable cardioverter defibrillator (n, %) | 15 (1.4) | 8 (2.9) | 0 (0) | 7 (1.2) | 0.011 |
| Last-year acute heart failure admission (n, %) | 858 (80.8) | 212 (76.3) | 149 (76.8) | 497 (84.2) | 0.005 |
| Cardiovascular medication | |||||
| -ACE inhibitors (n, %) | 632 (59.5) | 182 (65.5) | 110 (56.7) | 340 (57.6)¤ | 0.029 |
| -ARBs (n, %) | 172 (16.2) | 44 (15.8) | 39 (20.1) | 89 (15.1) | 0.308 |
| -β-Blockers (n, %) | 927 (87.3) | 251 (90.3) | 161 (83.0) | 515 (87.3) * ¤ | 0.047 |
| -Nitrates (n, %) | 327 (30.8) | 54 (19.4) | 41 (21.1) | 233 (39.5) ¤ ¥ | <0.001 |
| -Aldosterone antagonists (n, %) | 397 (37.4) | 115 (41.4) | 71 (36.6) | 211 (35.8) | 0.287 |
| -Diuretics (n, %) | 958 (90.2) | 247 (88.8) | 173 (89.2) | 538 (91.2) | 0.433 |
| -Antiagregant (n, %) | 494 (46.5) | 92 (33.1) | 73 (37.6) | 329 (55.8) ¤ ¥ | <0.001 |
| -Amiodarone (n, %) | 102 (9.6) | 33 (11.9) | 18 (9.3) | 51 (8.6) ¤ ¥ | 0.334 |
| Variables | HR (95% CI) | p Value |
|---|---|---|
| Age (years) | 1.04 (1.03–1.05) | <0.001 |
| Sex (female vs. male) | 1.04 (0.88–1.23) | 0.637 |
| Smoking (yes vs. no) | 0.97 (0.89–1.05) | 0.421 |
| BMI (kg/m2) | 0.97 (0.96–0.99) | <0.001 |
| Hypertension (yes vs. no) | 1.36 (1.08–1.71) | <0.010 |
| Dyslipidemia (yes vs. no) | 1.01 (0.85–1.20) | 0.884 |
| Statin use (yes vs. no) | 1.06 (0.89–1.26) | 0.532 |
| CKD (yes vs. no) | 1.68 (1.41–2.02) | <0.001 |
| Hemoglobin (g/dL) | 0.93 (0.89–0.97) | <0.001 |
| Albumin (g/dL) | 0.56 (0.47–0.68) | <0.001 |
| Troponin T | 1.14 (1.06–1.24) | 0.001 |
| NT-proBNP (pg/mL) | 2.31 (1.98–2.70) | <0.001 |
| LVEF ≤ 40% (yes vs. no) | 0.93 (0.79–1.11) | 0.431 |
| NYHA class (III–IV vs. I–II) | 1.79 (1.50–2.13) | <0.001 |
| HF of ischemic etiology (yes vs. no) | 1.49 (1.26–1.77) | <0.001 |
| Previous stroke (yes vs. no) | 1.29 (0.99–1.65) | 0.050 |
| Previous peripheral artery disease (yes vs. no) | 1.42 (1.15–1.75) | 0.001 |
| Previous COPD (yes vs. no) | 1.34 (1.11–1.63) | 0.003 |
| Last-year acute heart failure admission (yes vs. no) | 1.88 (1.46–2.42) | <0.001 |
| Variables | HR (95% CI) | p Value |
|---|---|---|
| Age (years) | 1.03 (1.02–1.04) | <0.001 |
| HF of ischemic etiology (yes vs. no) | 1.38 (1.12–1.71) | 0.003 |
| NT-proBNP (pg/mL) | 2.05 (1.68–2.51) | <0.001 |
| A/C glycemic ratio (third tertile) | 0.79 (0.64–0.99) | 0.040 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrera, M.J.; Moliner, P.; Llauradó, G.; Enjuanes, C.; Conangla, L.; Chillarón, J.-J.; Ballesta, S.; Climent, E.; Comín-Colet, J.; Flores-Le Roux, J.-A. Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Heart Failure: A Prospective Study. J. Clin. Med. 2022, 11, 6. https://doi.org/10.3390/jcm11010006
Carrera MJ, Moliner P, Llauradó G, Enjuanes C, Conangla L, Chillarón J-J, Ballesta S, Climent E, Comín-Colet J, Flores-Le Roux J-A. Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Heart Failure: A Prospective Study. Journal of Clinical Medicine. 2022; 11(1):6. https://doi.org/10.3390/jcm11010006
Chicago/Turabian StyleCarrera, Mª José, Pedro Moliner, Gemma Llauradó, Cristina Enjuanes, Laura Conangla, Juan-José Chillarón, Silvia Ballesta, Elisenda Climent, Josep Comín-Colet, and Juana-Antonia Flores-Le Roux. 2022. "Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Heart Failure: A Prospective Study" Journal of Clinical Medicine 11, no. 1: 6. https://doi.org/10.3390/jcm11010006
APA StyleCarrera, M. J., Moliner, P., Llauradó, G., Enjuanes, C., Conangla, L., Chillarón, J.-J., Ballesta, S., Climent, E., Comín-Colet, J., & Flores-Le Roux, J.-A. (2022). Prognostic Value of the Acute-to-Chronic Glycemic Ratio at Admission in Heart Failure: A Prospective Study. Journal of Clinical Medicine, 11(1), 6. https://doi.org/10.3390/jcm11010006






