Oral Health of COVID-19 Patients Using Extracorporeal Membrane Oxygenation: A Clinical Study of 19 Cases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Oral Health Care
2.3. Statistical Methods
2.4. Ethical Considerations
3. Results
3.1. Characteristics of COVID-19 Patients Who Received ECMO
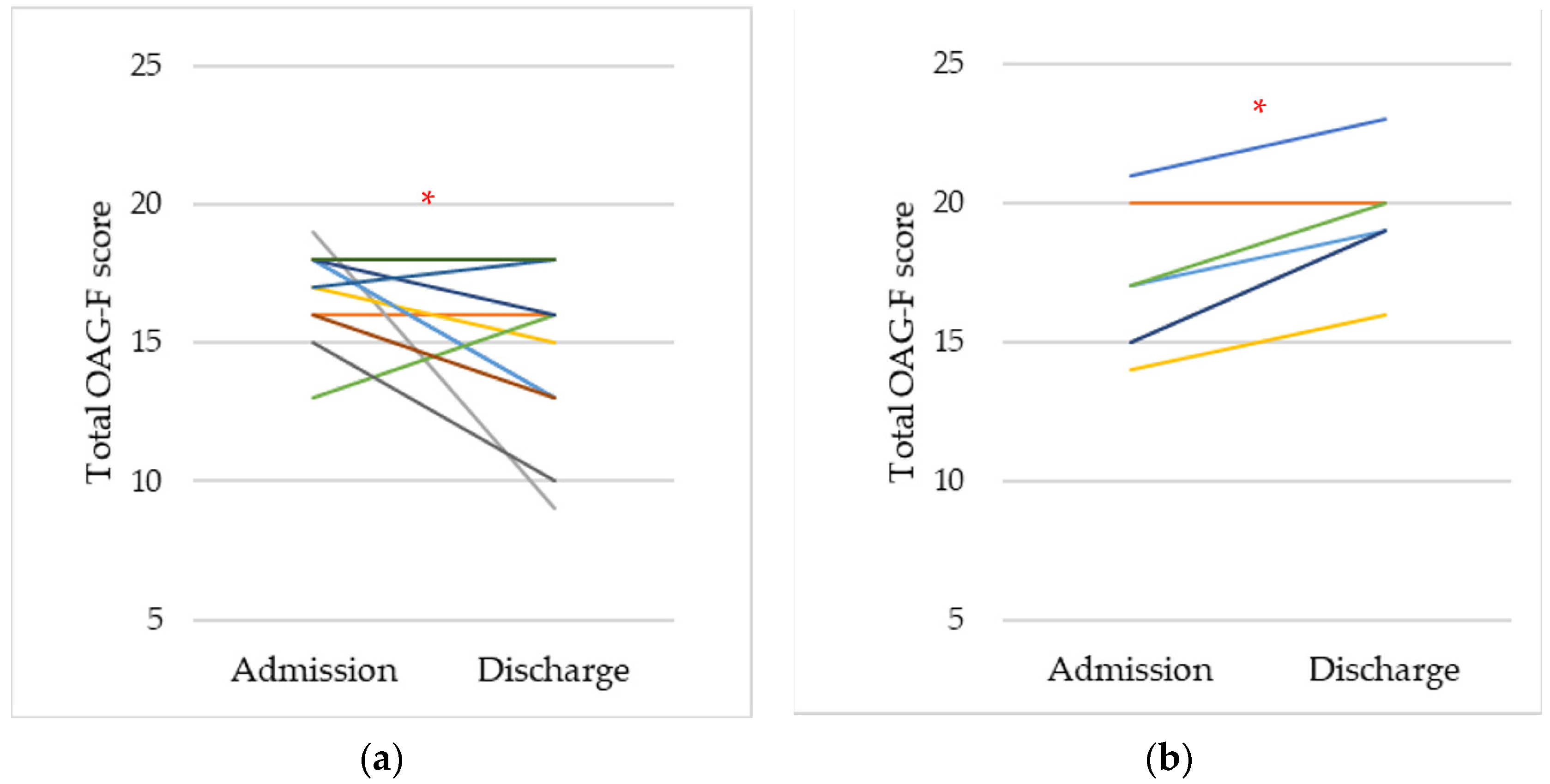
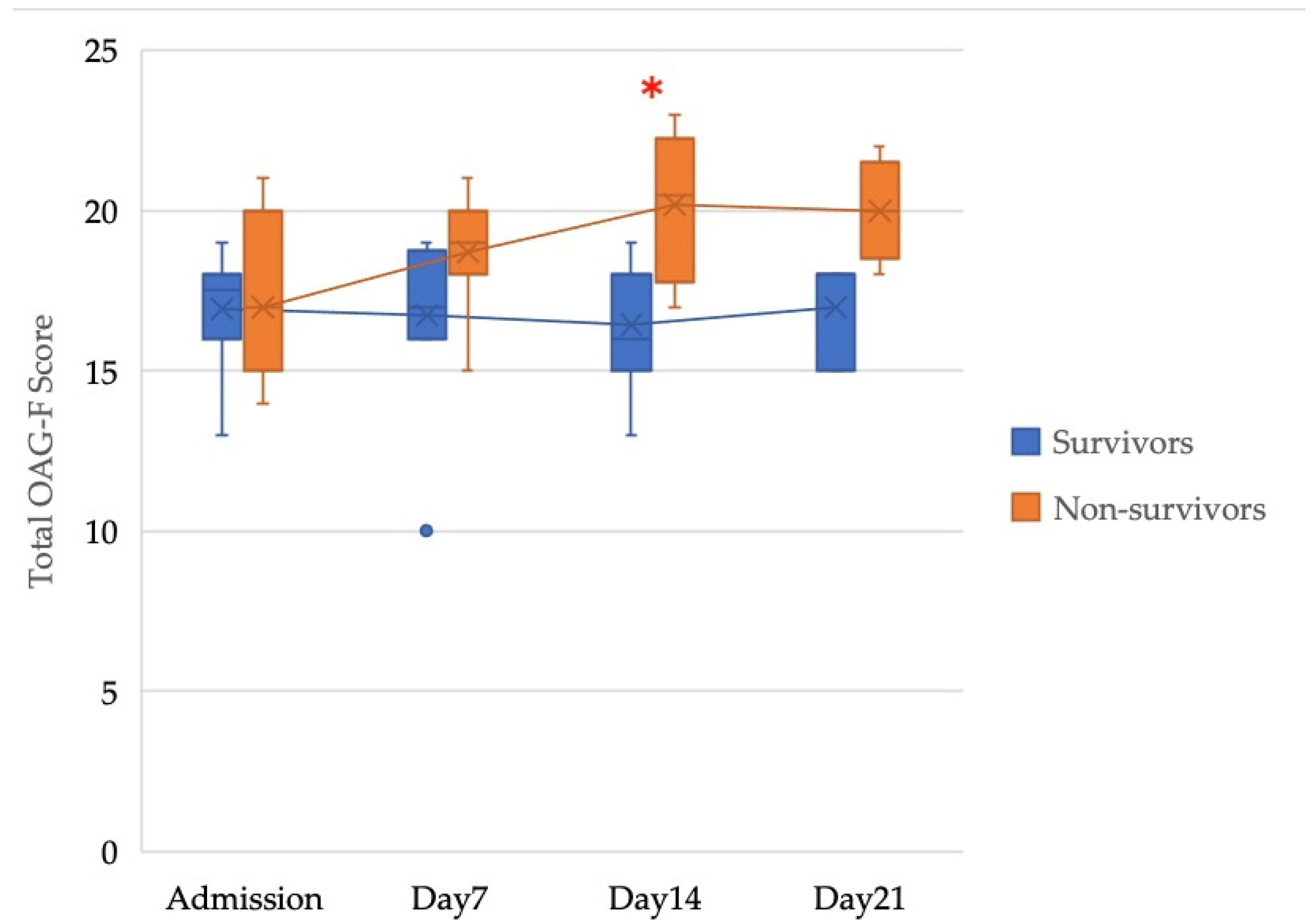
3.2. Oral Conditions of COVID-19 Patients Who Received ECMO
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dziedzic, A.; Wojtyczka, R. The impact of coronavirus infectious disease 19 (COVID-19) on oral health. Oral Dis. 2021, 27 (Suppl. 3), 703–706. [Google Scholar] [CrossRef] [PubMed]
- Sampson, V. Oral hygiene risk factor. Br. Dent. J. 2020, 228, 569. [Google Scholar] [CrossRef] [PubMed]
- Pitones-Rubio, V.; Chávez-Cortez, E.G.; Hurtado-Camarena, A.; González-Rascón, A.; Serafín-Higuera, N. Is periodontal disease a risk factor for severe COVID-19 illness? Med. Hypotheses 2020, 144, 109969. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (2019-nCoV) Infection is Suspected: Interim Guidance, 28 January 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Thomas, J.; Kostousov, V.; Teruya, J. Bleeding and Thrombotic Complications in the Use of Extracorporeal Membrane Oxygenation. Semin. Thromb. Hemost. 2018, 44, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Luyt, C.E.; Sahnoun, T.; Gautier, M.; Vidal, P.; Burrel, S.; Pineton de Chambrun, M.; Chommeloux, J.; Desnos, C.; Arzoine, J.; Nieszkowska, A.; et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: A retrospective cohort study. Ann. Intensive Care 2020, 10, 158. [Google Scholar] [CrossRef] [PubMed]
- Coke, C.J.; Davison, B.; Fields, N.; Fletcher, J.; Rollings, J.; Roberson, L.; Challagundla, K.B.; Sampath, C.; Cade, J.; Farmer-Dixon, C.; et al. SARS-CoV-2 Infection and Oral Health: Therapeutic Opportunities and Challenges. J. Clin. Med. 2021, 10, 156. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, W.; Kubota, N.; Shimizu, T.; Saruta, J.; Fuchida, S.; Kawata, A.; Yamamoto, Y.; Sugimoto, M.; Yakeishi, M.; Tsukinoki, K. Existence of SARS-CoV-2 Entry Molecules in the Oral Cavity. Int. J. Mol. Sci. 2020, 21, 6000. [Google Scholar] [CrossRef]
- Hocková, B.; Riad, A.; Valky, J.; Šulajová, Z.; Stebel, A.; Slávik, R.; Bečková, Z.; Pokorná, A.; Klugarová, J.; Klugar, M. Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases. J. Clin. Med. 2021, 10, 518. [Google Scholar] [CrossRef]
- Marouf, N.; Cai, W.; Said, K.N.; Daas, H.; Diab, H.; Chinta, V.R.; Hssain, A.A.; Nicolau, B.; Sanz, M.; Tamimi, F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J. Clin. Periodontol. 2021, 48, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Winning, L.; Patterson, C.C.; Cullen, K.M.; Kee, F.; Linden, G.J. Chronic periodontitis and reduced respiratory function. J. Clin. Periodontol. 2019, 46, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Eilers, J.; Berger, A.M.; Petersen, M.C. Development, testing, and application of the oral assessment guide. Oncol. Nurs. Forum 1988, 15, 325–330. [Google Scholar] [PubMed]
- Gaeckle, N.T.; Pragman, A.A.; Pendleton, K.M.; Baldomero, A.K.; Criner, G.J. The Oral-Lung Axis: The Impact of Oral Health on Lung Health. Respir. Care 2020, 65, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Kilian, M.; Chapple, I.L.; Hannig, M.; Marsh, P.D.; Meuric, V.; Pedersen, A.M.; Tonetti, M.S.; Wade, W.G.; Zaura, E. The oral microbiome—An update for oral healthcare professionals. Br. Dent. J. 2016, 221, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.A. Role of oral bacteria in respiratory infection. J. Periodontol. 1999, 70, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Manger, D.; Walshaw, M.; Fitzgerald, R.; Doughty, J.; Wanyonyi, K.L.; White, S.; Gallagher, J.E. Evidence summary: The relationship between oral health and pulmonary disease. Br. Dent. J. 2017, 222, 527–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, H.; Hirasawa, H.; Oda, S.; Shiga, H.; Matsuda, K.; Nakamura, M. Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med. 2006, 32, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Z.; Koo, H.; Chen, Q.; Zhou, X.; Liu, Y.; Simon-Soro, A. Potential implications of SARS-CoV-2 oral infection in the host microbiota. J. Oral Microbiol. 2020, 13, 1853451. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.S. From focal sepsis to periodontal medicine: A century of exploring the role of the oral microbiome in systemic disease. J. Physiol. 2017, 595, 465–476. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, C.; Bocchieri, S.; Stefano, R.; Gorassini, F.; Surace, G.; Amoroso, G.; Scoglio, C.; Mastroieni, R.; Gambino, D.; Amantia, E.M.; et al. Dental Office Prevention of Coronavirus Infection. Eur. J. Dent. 2020, 14, S146–S151. [Google Scholar] [CrossRef]
| Category | Tools for Assessment | Method of Measurement | Score | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Voice | Auditory assessment | Converse with patient | Normal | Deeper or Rusty | Difficulty talking or painful |
| Swallow | Observation | Ask patient to swallow | Normal swallow | Some pain on swallow | Unable swallow |
| Lips | Visual/ palpatory | Observe and feel tissue | Smooth and pink moist | Dry or cracked | Ulcerated or bleeding |
| Tongue | Visual/ palpatory | Feel and observe appearance of tissue | Pink and moist and papillae present | Coated or loss of papillae with shiny appearance with or without redness | Blistered or cracked |
| Saliva | Visual/ palpatory | Observe and feel saliva | Watery | Thick or ropy | Absent |
| Mucous Membranes | Visual assessment | Observe appearance of tissue | Pink and moist | Reddened or coated (increased whiteness) without ulcerations | Ulcerations with or without bleeding |
| Gingiva | Visual/ palpatory | Gently press tissue | Pink and stippled and film | Edematous with or without redness | Spontaneous bleeding or bleeding with pressure |
| Teeth, Dentures | Visual assessment | Observe appearance of teeth or denture bearing area | Clean and no debris | Plaque or debris in localized areas (between teeth if present) | Plaque or debris generalized along gum line or denture bearing area |
| Mechanical Ventilation | Total OAG-F Score | Time 0:00 | 1:00 | 2:00 | 3:00 | 4:00 | 5:00 | 6:00 | 7:00 | 8:00 | 9:00 | 10:00 | 11:00 | 12:00 | 13:00 | 14:00 | 15:00 | 16:00 | 17:00 | 18:00 | 19:00 | 20:00 | 21:00 | 22:00 | 23:00 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | –8 | ○ | ▲ | ○ | ○ | ||||||||||||||||||||
| 9–12 | □ | ○□ | □ | ▲ | ○□ | □ | ○□ | □ | |||||||||||||||||
| 13– | □ | ○□ | □ | ▲ | ○□ | □ | ○□ | □ | □ | ||||||||||||||||
| Yes | –12 | □ | ○□ | ▲ | ○□ | ○□ | □ | ||||||||||||||||||
| 13–14 or MM * > 1 | □ | ○□ | □ | ▲ | ○□ | □ | ○□ | □ | |||||||||||||||||
| 15– or MM * = 3 | □ | ○□ | □ | ▲ | ○□ | □ | ○□ | □ | □ |
| All Cases N = 19 | Survivors N = 12 | Non-Survivors N = 7 | ||
|---|---|---|---|---|
| Sex 1 | Male | 16 (84.2%) | 10 (83.3%) | 6 (85.7%) |
| Female | 3 (15.8%) | 2 (16.7%) | 1 (14.3%) | |
| Age 2 | 62 (51–69) | 59 (39–64) | 69 (59–71) | |
| BMI 1 | Adequate weight (<25) | 8 (42.1%) | 5 (41.7%) | 3 (42.9%) |
| Overweight/Obese (≥25) | 11 (57.9%) | 7 (58.3%) | 4 (57.1%) | |
| Number of teeth 2 | 27 (24–28) | 27 (26–27) | 28 (23–28) | |
| Duration of ECMO treatment (days) 2 | 10 (7–29) | 8 (5–11.5) | 34 (12–74) * | |
| Survivors | Non-Survivors | |
|---|---|---|
| Voice | 3 (3–3) | 3 (3–3) |
| Swallow | 3 (3–3) | 3 (3–3) |
| Lips | 2 (2–2) | 2 (2–3) |
| Tongue | 2 (2–2) | 2 (1–2) |
| Saliva | 2 (2–2) | 2 (2–2) |
| Mucous membranes | 2 (1–2) | 1 (1–2) |
| Gingiva | 1.5 (1–2) | 2 (1–2) |
| Teeth and dentures | 2 (2–2) | 2 (1–2) |
| Total | 17.5 (16–18) | 17 (15–20) |
| Survivors | Non-Survivors | |
|---|---|---|
| Voice | 3 (2–3) | 3 (3–3) |
| Swallow | 3 (1–3) | 3 (3–3) |
| Lips | 2 (1–2) | 2 (2–3) |
| Tongue | 2 (2–2) | 2 (2–2) |
| Saliva | 2 (1.25–2) | 2 (2–3) * |
| Mucous membranes | 1.5 (1–2) | 2 (2–3) * |
| Gingiva | 1 (1–1.75) | 2 (2–3) * |
| Teeth and dentures | 1.5 (1–2) | 2 (1–2) |
| Total | 15.5 (13–17.5) | 19 (19–20) * |
| Variable | Coefficient | 95%CI * | p Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| ECMO center outcome (dead) | 3.295 | 1.361 | 5.229 | 0.002 |
| Duration of ECMO (days) | −0.053 | −0.128 | 0.022 | 0.154 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshino, A.; Nakamura, Y.; Irie, Y.; Kitamura, T.; Takata, T.; Ishikura, H.; Kondo, S. Oral Health of COVID-19 Patients Using Extracorporeal Membrane Oxygenation: A Clinical Study of 19 Cases. J. Clin. Med. 2022, 11, 42. https://doi.org/10.3390/jcm11010042
Yoshino A, Nakamura Y, Irie Y, Kitamura T, Takata T, Ishikura H, Kondo S. Oral Health of COVID-19 Patients Using Extracorporeal Membrane Oxygenation: A Clinical Study of 19 Cases. Journal of Clinical Medicine. 2022; 11(1):42. https://doi.org/10.3390/jcm11010042
Chicago/Turabian StyleYoshino, Aya, Yoshihiko Nakamura, Yuhei Irie, Taisuke Kitamura, Tohru Takata, Hiroyasu Ishikura, and Seiji Kondo. 2022. "Oral Health of COVID-19 Patients Using Extracorporeal Membrane Oxygenation: A Clinical Study of 19 Cases" Journal of Clinical Medicine 11, no. 1: 42. https://doi.org/10.3390/jcm11010042
APA StyleYoshino, A., Nakamura, Y., Irie, Y., Kitamura, T., Takata, T., Ishikura, H., & Kondo, S. (2022). Oral Health of COVID-19 Patients Using Extracorporeal Membrane Oxygenation: A Clinical Study of 19 Cases. Journal of Clinical Medicine, 11(1), 42. https://doi.org/10.3390/jcm11010042






