Challenges of Acute Ischemic Stroke Treatment in Orally Anticoagulated Patients via Telemedicine
Abstract
1. Introduction
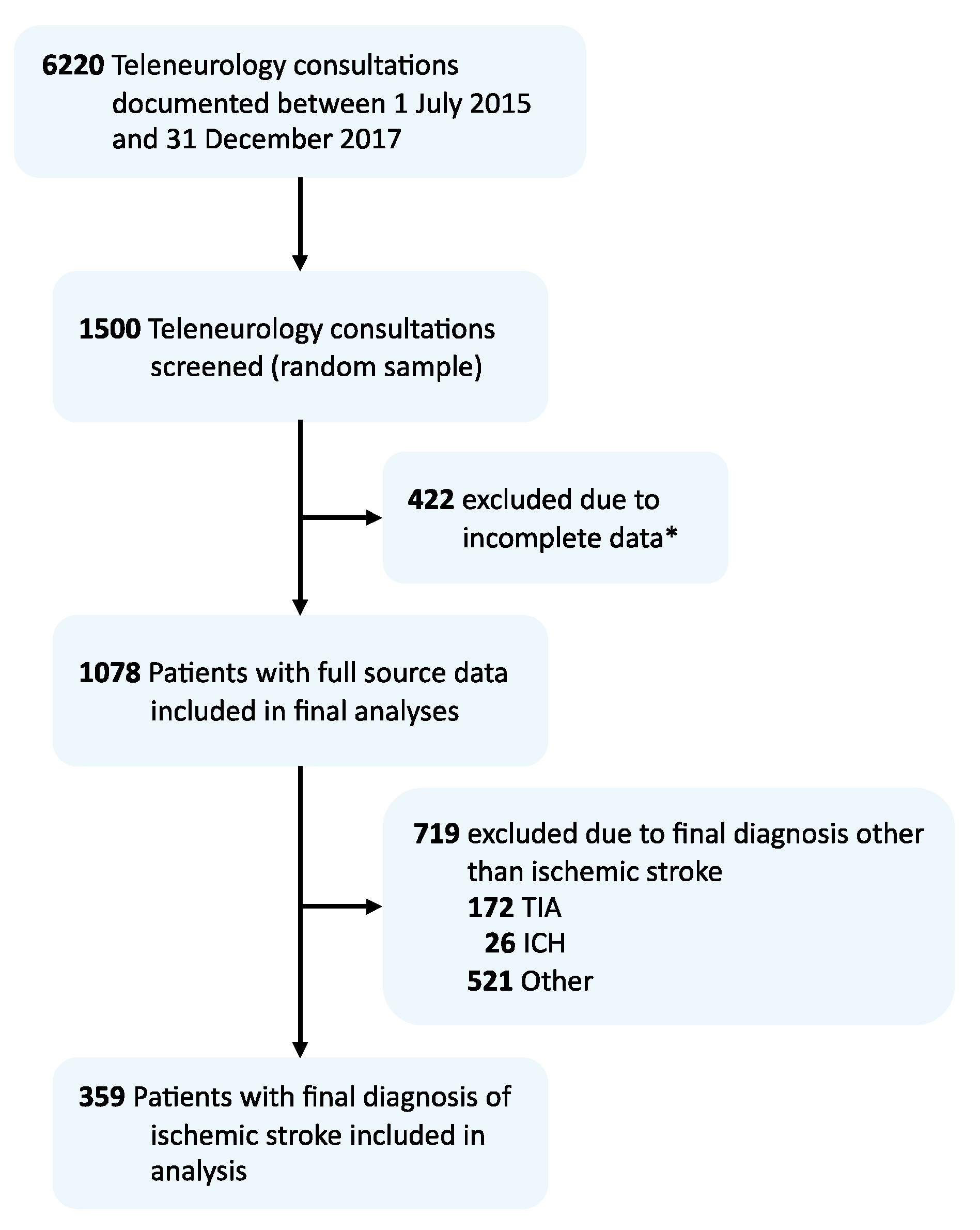
2. Methods
2.1. Study Design and Setting
2.2. Data Acquisition
2.3. Statistical Analysis
3. Results
3.1. Coagulation Status
3.2. Acute Ischemic Stroke Management
3.3. Reasons for Withholding Intravenous Thrombolysis
3.4. Adaptation of Oral Anticoagulation after Stroke
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| No Prior OAC n = 132 | Prior OAC n = 32 | p-Value | |
|---|---|---|---|
| Age | 74.4 (63.9–81.8) | 77.6 (71.9–85.1) | 0.041 |
| Female sex | 64 (48.5) | 18 (56.3) | 0.555 |
| Medical history | |||
| Atrial fibrillation | 21 (15.9) | 26 (81.3) | <0.001 |
| DVT or PE | 4 (3.0) | 8 (25.0) | <0.001 |
| Malignancy | 13 (9.8) | 10 (31.3) | 0.004 |
| Mechanical heart valve | 1 (0.8) | 1 (3.1) | 0.353 |
| Arterial hypertension | 88 (66.7) | 30 (93.8) | 0.002 |
| Diabetes mellitus | 40 (30.3) | 7 (21.9) | 0.391 |
| Hyperlipidemia | 31 (23.5) | 7 (21.9) | >0.99 |
| Ischemic heart disease | 18 (13.6) | 9 (28.1) | 0.062 |
| Peripheral artery disease | 17 (12.9) | 6 (18.8) | 0.400 |
| Stroke/TIA | 31 (23.5) | 14 (43.8) | 0.028 |
| Prior medication | |||
| Antiplatelet | 50 (37.9) | 3 (9.3) | 0.007 |
| VKA | - | 14 (43.8) | - |
| NOAC | - | 18 (56.2) | - |
| Functional status | |||
| Premorbid Mrs a | 1 (0–3) | 2 (1–3) | 0.066 |
| mRS at discharge b | 2 (1–4) | 3 (2–4) | 0.086 |
| NIHSS at admission c | 5 (2–10) | 6 (2–13) | 0.350 |
| NIHSS at discharge d | 1 (0–4) | 3 (0–6) | 0.263 |
| No Prior OAC n = 132 | Prior OAC n = 32 | p-Value | |
|---|---|---|---|
| Large vessel occlusion | 31 (23.5) | 3 (9.4) | 0.091 |
| Acute vascular imaging | 38 (28.8) | 8 (25.0) | 0.827 |
| Acute Management | |||
| Acute interhospital transfer | 28 (21.2) | 7 (21.9) | >0.99 |
| IVT | 58 (43.9) | 2 (6.3) | <0.001 |
| EVT | 15 (11.4) | 2 (6.3) | 0.530 |
| Admitting ward | |||
| General ward | 3 (2.3) | 1 (3.1) | 0.584 |
| Stroke unit | 108 (81.8) | 28 (87.5) | 0.603 |
| Intensive care unit | 20 (15.2) | 3 (9.4) | 0.572 |
| Complications | |||
| Any complication | 28 (21.2) | 7 (21.9) | >0.99 |
| Pneumonia | 13 (9.8) | 5 (15.6) | 0.351 |
| Intracerebral hemorrhage | 6 (4.5) | 1 (3.1) | >0.99 |
| Malignant infarction | 5 (3.8) | - | 0.584 |
| Discharge to | |||
| Patient’s home | 46 (34.8) | 9 (28.1) | 0.536 |
| Rehabilitation unit | 47 (35.6) | 12 (37.5) | 0.840 |
| Nursing home | 11 (8.3) | 6 (18.8) | 0.104 |
| Other hospital | 15 (11.4) | 5 (15.6) | 0.548 |
| Length of stay in days | 5 (3–9) | 9 (3–18) | 0.011 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Age | 0.994 | 0.96–1.029 | 0.732 |
| Premorbid mRS | 0.428 | 0.3–0.611 | <0.001 |
| NIHSS at admission | 1.248 | 1.172–1.318 | <0.001 |
| History of malignancy | 1.359 | 0.458–4.029 | 0.58 |
| Prior OAC treatment | 2.306 | 0.958–5.552 | 0.062 |
References
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef]
- Purrucker, J.C.; Hölscher, K.; Kollmer, J.; Ringleb, P.A. Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants. J. Clin. Med. 2020, 9, 2938. [Google Scholar] [CrossRef] [PubMed]
- Meinel, T.R.; Branca, M.; De Marchis, G.M.; Nedeltchev, K.; Kahles, T.; Bonati, L.; Arnold, M.; Heldner, M.R.; Jung, S.; Carrera, E.; et al. Prior Anticoagulation in Patients with Ischemic Stroke and Atrial Fibrillation. Ann. Neurol. 2021, 89, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Meinel, T.; Purrucker, J.C.; Kaesmacher, J.; Fischer, U.; Wilson, D.; Wu, T.Y. Recanalisation therapies for acute ischaemic stroke in patients on direct oral anticoagulants. J. Neurol. Neurosurg. Psychiatry 2021, 92, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Purrucker, J.C.; Haas, K.; Rizos, T.; Khan, S.; Poli, S.; Kraft, P.; Kleinschnitz, C.; Dziewas, R.; Binder, A.; Palm, F.; et al. Coagulation Testing in Acute Ischemic Stroke Patients Taking Non–Vitamin K Antagonist Oral Anticoagulants. Stroke 2017, 48, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Wilson, D.; Wu, T.Y.-H. Administering Thrombolysis for Acute Ischemic Stroke in Patients Taking Direct Oral Anticoagulants: To Treat or How to Treat. JAMA Neurol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Audebert, H.; Turc, G.; Cordonnier, C.; Christensen, H.; Sacco, S.; Sandset, E.C.; Ntaios, G.; Charidimou, A.; Toni, D.; et al. Consensus statements and recommendations from the ESO-Karolinska Stroke Update Conference, Stockholm 11–13 November. Eur. Stroke J. 2019, 4, 307–317. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Purrucker, J.C.; Steiner, T. Management of acute stroke in patients on oral anticoagulants. Curr. Opin. Neurol. 2017, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Traenka, C.; Polymeris, A.; Hert, L.; Fisch, U.; Peters, N.; De Marchis, G.M.; Guzman, R.; Nickel, C.H.; Lyrer, P.A.; et al. Feasibility of rapid measurement of Rivaroxaban plasma levels in patients with acute stroke. J. Thromb. Thrombolysis 2016, 43, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Escolà, J.K.; Nagel, S.; Sola, C.V.; Doroszewski, E.; Jaschonek, H.; Gutschalk, A.; Gumbinger, C.; Purrucker, J. Diagnostic Accuracy in Teleneurological Stroke Consultations. J. Clin. Med. 2021, 10, 1170. [Google Scholar] [CrossRef] [PubMed]
- Kermer, P.; Eschenfelder, C.C.; Diener, H.-C.; Grond, M.; Abdalla, Y.; Abraham, A.; Althaus, K.; Becks, G.; Berrouschot, J.; Berthel, J.; et al. Antagonizing dabigatran by idarucizumab in cases of ischemic stroke or intracranial hemorrhage in Germany—Updated series of 120 cases. Int. J. Stroke 2020, 15, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Barber, P.A.; Wu, T.Y.; Ranta, A. Stroke reperfusion therapy following dabigatran reversal with idarucizumab in a national cohort. Neurology 2020, 94, e1968–e1972. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Traenka, C.; Polymeris, A.A.; Thilemann, S.; Wagner, B.; Hert, L.; Müller, M.D.; Gensicke, H.; Peters, N.; Nickel, C.H.; et al. Intravenous Thrombolysis in Patients with Stroke Taking Rivaroxaban Using Drug Specific Plasma Levels: Experience with a Standard Operation Procedure in Clinical Practice. J. Stroke 2017, 19, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Gumbinger, C.; German Stroke Society. Telemedical Stroke Care: Why Especially Patients in Rural Areas Benefit. Available online: https://www.dsg-info.de/images/stories/DSG/Presse/PDF/2020/PM_DSG-PK_Teleneurologie.pdf (accessed on 9 March 2021).

| No Prior OAC n = 296 | Prior OAC n = 63 | p-Value | |
|---|---|---|---|
| Age | 75.4 (64.1–81.6) | 79.8 (75.3–85.3) | <0.001 |
| Female sex | 146 (49.3) | 36 (57.1) | 0.270 |
| Medical history | |||
| Atrial fibrillation | 34 (11.5) | 53 (84.1) | <0.001 |
| DVT or PE | 8 (2.7) | 13 (20.6) | <0.001 |
| Malignancy | 24 (8.1) | 15 (23.8) | 0.001 |
| Mechanical heart valve | 1 (0.3) | 1 (1.6) | 0.321 |
| Arterial hypertension | 212 (71.6) | 49 (77.8) | 0.354 |
| Diabetes mellitus | 91 (30.7) | 19 (30.2) | >0.99 |
| Hyperlipidemia | 84 (28.4) | 16 (25.4) | 0.757 |
| Ischemic heart disease | 51 (17.2) | 18 (28.6) | 0.052 |
| Peripheral artery disease | 30 (10.1) | 10 (16.1) | 0.185 |
| Stroke/TIA | 73 (24.7) | 23 (36.5) | 0.061 |
| Prior medication | |||
| Antiplatelet | 117 (39.5) | 7 (12.7) | <0.001 |
| VKA | - | 24 (38.0) | - |
| NOAC | - | 39 (62.0) | - |
| Functional status | |||
| Premorbid mRS a | 1 (0–3) | 2 (1–3) | 0.002 |
| mRS at discharge b | 2 (1–4) | 3 (2–4) | 0.018 |
| NIHSS at admission c | 4 (2–9) | 6 (3–13) | 0.014 |
| NIHSS at discharge d | 1 (0–3) | 2 (1–6) | 0.053 |
| Onset to admission at PSC, hours e | 4.2 (1.4–10.5) | 2.4 (1.2–6.8) | 0.067 |
| No Prior OAC n = 296 | Prior OAC n = 63 | p-Value | |
|---|---|---|---|
| Large-vessel occlusion | 48 (16.2) | 9 (14.3) | 0.850 |
| Imaging modality at admission | |||
| CT | 290 (98.0) | 62 (98.4) | >0.99 |
| MRI | 6 (2.0) | 1 (1.6) | >0.99 |
| Acute vascular imaging | 55 (18.6) | 16 (25.4) | 0.225 |
| Acute Management | |||
| Acute interhospital transfer | 41 (13.9) | 15 (23.8) | 0.056 |
| IVT | 60 (20.3) | 2 (3.2) | <0.001 |
| EVT | 22 (7.4) | 8 (12.7) | 0.207 |
| Admitting ward | |||
| General ward | 9 (3.0) | 1 (1.6) | >0.99 |
| Stroke unit | 249 (84.1) | 56 (88.9) | 0.438 |
| Intensive care unit | 36 (12.2) | 6 (9.5) | 0.669 |
| Complications | |||
| Any complication | 51 (17.2) | 11 (17.5) | >0.99 |
| Pneumonia | 21 (7.1) | 7 (11.1) | 0.300 |
| Intracerebral hemorrhage | 9 (3.0) | 2 (3.2) | >0.99 |
| Malignant infarction | 13 (4.4) | - | 0.136 |
| Discharge to | |||
| Patient’s home | 108 (36.5) | 20 (31.7) | 0.563 |
| Rehabilitation unit | 112 (37.8) | 23 (36.5) | 0.887 |
| Nursing home | 21 (7.1) | 8 (12.7) | 0.199 |
| Other hospital | 33 (11.1) | 12 (19.0) | 0.095 |
| Length of stay in days | 6 (3–10) | 6 (3–13) | 0.201 |
| Treatment Interruption in Days * | |
|---|---|
| ≤3 | 35 (66) |
| 4–12 | 11 (21) |
| >12 | 7 (13) |
| Treatment modifications # | |
| No treatment modifications | 30 (48) |
| Adaptation of NOAC dosage | 8 (13) |
| VKA to NOAC | 12 (19) |
| NOAC to VKA | 2 (3) |
| NOAC to different NOAC | 4 (6) |
| Parenteral anticoagulation | 3 (5) |
| No further anticoagulation | 4 (6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kühne Escolà, J.; Nagel, S.; Panitz, V.; Reiff, T.; Gutschalk, A.; Gumbinger, C.; Purrucker, J.C. Challenges of Acute Ischemic Stroke Treatment in Orally Anticoagulated Patients via Telemedicine. J. Clin. Med. 2021, 10, 1956. https://doi.org/10.3390/jcm10091956
Kühne Escolà J, Nagel S, Panitz V, Reiff T, Gutschalk A, Gumbinger C, Purrucker JC. Challenges of Acute Ischemic Stroke Treatment in Orally Anticoagulated Patients via Telemedicine. Journal of Clinical Medicine. 2021; 10(9):1956. https://doi.org/10.3390/jcm10091956
Chicago/Turabian StyleKühne Escolà, Jordi, Simon Nagel, Verena Panitz, Tilman Reiff, Alexander Gutschalk, Christoph Gumbinger, and Jan Christoph Purrucker. 2021. "Challenges of Acute Ischemic Stroke Treatment in Orally Anticoagulated Patients via Telemedicine" Journal of Clinical Medicine 10, no. 9: 1956. https://doi.org/10.3390/jcm10091956
APA StyleKühne Escolà, J., Nagel, S., Panitz, V., Reiff, T., Gutschalk, A., Gumbinger, C., & Purrucker, J. C. (2021). Challenges of Acute Ischemic Stroke Treatment in Orally Anticoagulated Patients via Telemedicine. Journal of Clinical Medicine, 10(9), 1956. https://doi.org/10.3390/jcm10091956







