The Comparison of Outcomes of Transvaginal Mesh Surgery with and without Midline Fascial Plication for the Treatment of Anterior Vaginal Prolapse: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
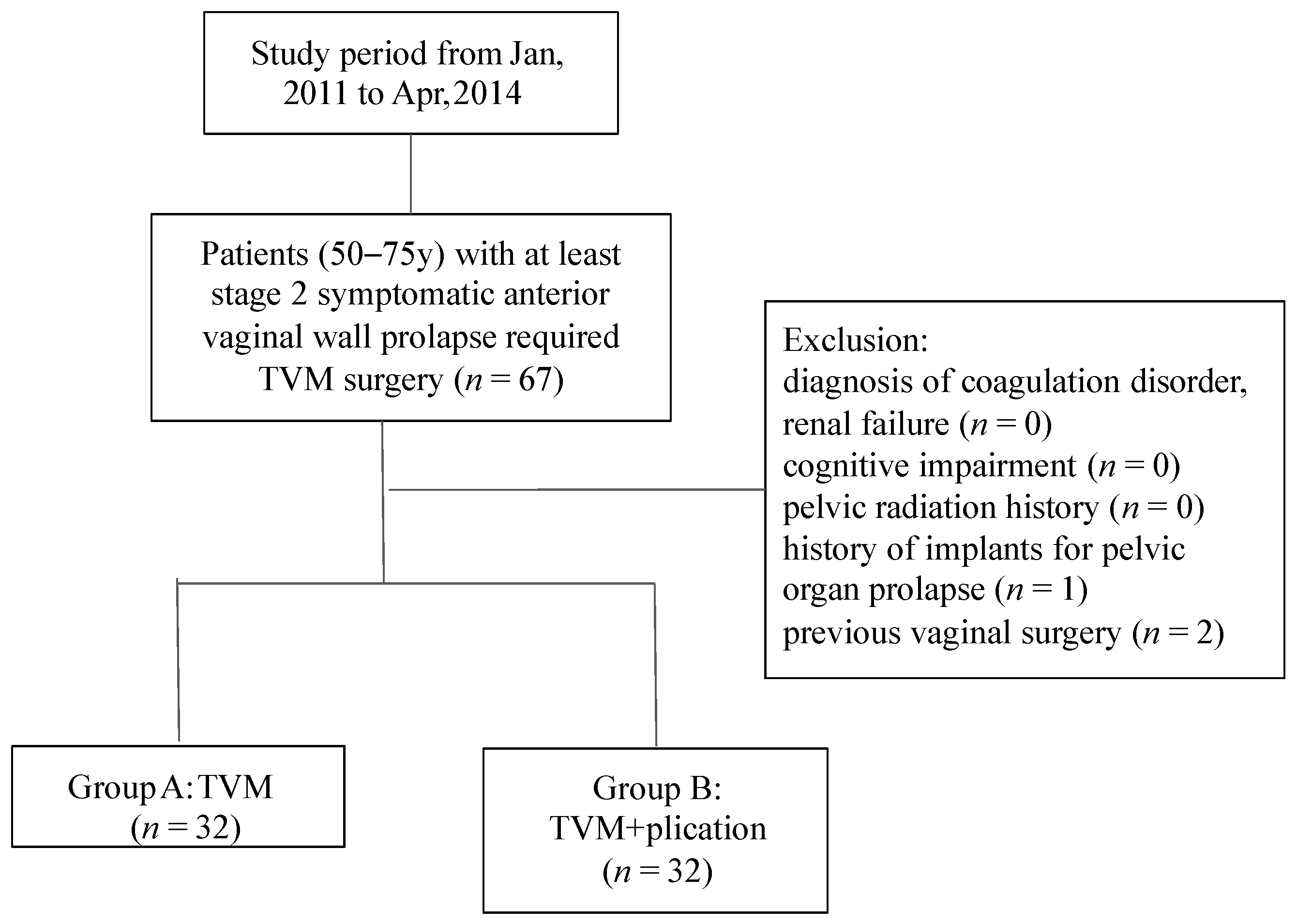
2.1. Patients
2.2. Trial Design and Interventions
2.3. Surgical Technique
2.4. Outcomes
2.5. Statistics
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| POP | pelvic organ prolapse |
| TVM | transvaginal mesh |
| POP-Q | pelvic organ prolapse-quantification system; |
| BMI | body mass index |
| PFDI-20 | Pelvic Floor Distress Inventory, Short Form 20 |
| POPDI-6 | Pelvic Organ Prolapse Distress Inventory-6 |
| CRADI-8 | Colorectal-anal Distress Inventory-8 |
| UDI-6 | Urogenital Distress Inventory-6 |
| PFIQ-7 | Pelvic Floor Impact Questionnaire, Short Form 7 |
| POPIQ-7 | Pelvic Organ Prolapse Impact Questionnaire-7 |
| CRAIQ-7 | Colorectal-anal Impact Questionnaire-7 |
| UIQ-7 | Urinary Impact Questionnaire-7 |
| SD | standard deviation |
| VTH | vaginal total hysterectomy |
| SSS | sacrospinous ligament suspension |
| TVL | total vaginal length |
| Gh | genital hiatus |
| Pb | perineal body |
References
- Cooper, J.; Annappa, M.; Dracocardos, D.; Cooper, W.; Muller, S.; Mallen, C. Prevalence of genital prolapse symptoms in primary care: A cross-sectional survey. Int. Urogynecol. J. 2015, 26, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Matthews, C.A.; Conover, M.M.; Pate, V.; Jonsson Funk, M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet. Gynecol. 2014, 123, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.J.; Holman, C.D.J.; Moorin, R.E.; Tsokos, N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet. Gynecol. 2010, 116, 1096–1100. [Google Scholar] [CrossRef]
- Digesu, G.A.; Khullar, V.; Cardozo, L.; Robinson, D.; Salvatore, S. P-QOL: A validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2005, 16, 176–181. [Google Scholar] [CrossRef]
- Barber, M.D.; Maher, C. Epidemiology and outcome assessment of pelvic organ prolapse. Int. Urogynecol. J. 2013, 24, 1783–1790. [Google Scholar] [CrossRef]
- Vergeldt, T.F.M.; Weemhoff, M.; IntHout, J.; Kluivers, K.B. Risk factors for pelvic organ prolapse and its recurrence: A systematic review. Int. Urogynecol. J. 2015, 26, 1559–1573. [Google Scholar] [CrossRef]
- Cartwright, M.A.R.; Kirby, A.C.; Tikkinen, K.A.O.; Mrcs, A.M.; Mrcog, G.T.; Mrcs, P.R.; Pesonen, J.; Ambrose, M.B.B.S.C.; Gonzalez-Maffe, J.; Bennett, M.D.P.; et al. Systematic review and metaanalysis of genetic association studies of urinary symptoms and prolapse in women. Am. J. Obstet. Gynecol. 2015, 212, 199.e1–199.e24. [Google Scholar] [CrossRef]
- Altman, D.; Forsman, M.; Falconer, C.; Lichtenstein, P. Genetic influence on stress urinary incontinence and pelvic organ prolapse. Eur. Urol. 2008, 54, 918–922. [Google Scholar] [CrossRef]
- Jack, G.S.; Nikolova, G.; Vilain, E.; Raz, S.; Rodríguez, L.V. Familial transmission of genitovaginal prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2006, 17, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Buchsbaum, G.M.; Duecy, E.E.; Kerr, L.A.; Huang, L.-S.; Perevich, M.; Guzick, D.S. Pelvic organ prolapse in nulliparous women and their parous sisters. Obstet. Gynecol. 2006, 108, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.M.; Velez Edwards, D.R.; Edwards, T.; Giri, A.; Jerome, R.N.; Wu, J.M. Genetic epidemiology of pelvic organ prolapse: A systematic review. Am. J. Obstet. Gynecol. 2014, 211, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, S.L.; Clark, A.; Nygaard, I.; Aragaki, A.; Barnabei, V.; McTiernan, A. Pelvic organ prolapse in the Women’s Health Initiative: Gravity and gravidity. Am. J. Obstet. Gynecol. 2002, 186, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Handa, V.L.; Garrett, E.; Hendrix, S.; Gold, E.; Robbins, J. Progression and remission of pelvic organ prolapse: A longitudinal study of menopausal women. Am. J. Obstet. Gynecol. 2004, 190, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.J.; Lee, K.-S. Current surgical management of pelvic organ prolapse: Strategies for the improvement of surgical outcomes. Investig. Clin. Urol. 2019, 60, 413–424. [Google Scholar] [CrossRef]
- Maher, C.; Feiner, B.; Baessler, K.; Christmann-Schmid, C.; Haya, N.; Marjoribanks, J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst. Rev. 2016, 2, CD012079. [Google Scholar] [CrossRef]
- Maher, C. Anterior vaginal compartment surgery. Int. Urogynecol. J. 2013, 24, 1791–1802. [Google Scholar] [CrossRef]
- Karp, D.R.; Peterson, T.V.; Mahdy, A.; Ghoniem, G.; Aguilar, V.C.; Davila, G.W. Biologic grafts for cystocele repair: Does concomitant midline fascial plication improve surgical outcomes? Int. Urogynecol. J. 2011, 22, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Bump, R.C.; Mattiasson, A.; Bø, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Culligan, P.J.; Littman, P.M.; Salamon, C.G.; Priestley, J.L.; Shariati, A. Evaluation of a transvaginal mesh delivery system for the correction of pelvic organ prolapse: Subjective and objective findings at least 1 year after surgery. Am. J. Obstet. Gynecol. 2010, 203, 1–6. [Google Scholar] [CrossRef]
- McCracken, G.R.; Lefebvre, G. Mesh-free anterior vaginal wall repair: History or best practice? Obstet. Gynaecol. 2007, 9, 233–242. [Google Scholar] [CrossRef]
- Haylen, B.T.; Freeman, R.M.; Swift, S.E.; Cosson, M.; Davila, G.W.; Deprest, J.; Dwyer, P.L.; Fatton, B.; Kocjancic, E.; Lee, J.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol. Urodyn. 2011, 30, 2–12. [Google Scholar] [PubMed]
- Morselli, S.; Li Marzi, V.; Verrienti, P.; Serati, M.; Di Camillo, M.; Tosto, A.; Milanesi, M.; Serni, S. Transvaginal mesh surgery for pelvic organ prolapse does not affect sexual function at long term follow up. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Balzarro, M.; Rubilotta, E.; Antonelli, A. Cystocele Repair by a Modified Surgical Technique of Bilateral Pubococcygeus Plication: Long-Term Surgical and Functional Results. J. Clin. Med. 2020, 9, 3318. [Google Scholar] [CrossRef] [PubMed]
- Köse, O.; Sağlam, H.S.; Kumsar, Ş.; Budak, S.; Aydemir, H.; Adsan, Ö. Early results of a novel technique for anterior vaginal wall prolapse repair: Anterior vaginal wall darn. BMC Urol. 2014, 14, 51. [Google Scholar] [CrossRef][Green Version]
- Dahlgren, E.; Kjølhede, P. RPOP-PELVICOL Study Group. Long-term outcome of porcine skin graft in surgical treatment of recurrent pelvic organ prolapse. An open randomized controlled multicenter study. Acta Obstet. Gynecol. Scand. 2011, 90, 1393–1401. [Google Scholar] [CrossRef]
- Cheng, Y.-W.; Su, T.-H.; Wang, H.; Huang, W.-C.; Lau, H.-H. Risk factors and management of vaginal mesh erosion after pelvic organ prolapse surgery. Taiwan. J. Obstet. Gynecol. 2017, 56, 184–187. [Google Scholar] [CrossRef]
- Barski, D.; Otto, T.; Gerullis, H. Systematic review and classification of complications after anterior, posterior, apical, and total vaginal mesh implantation for prolapse repair. Surg. Technol. Int. 2014, 24, 217–224. [Google Scholar]
- Barber, M.D.; Brubaker, L.; Nygaard, I.; Wheeler, T.L., 2nd; Schaffer, J.; Chen, Z.; Spino, C. Pelvic Floor Disorders Network Defining success after surgery for pelvic organ prolapse. Obstet. Gynecol. 2009, 114, 600–609. [Google Scholar] [CrossRef]
- van Raalte, H.M.; Lucente, V.R.; Molden, S.M.; Haff, R.; Murphy, M. One-year anatomic and quality-of-life outcomes after the Prolift procedure for treatment of posthysterectomy prolapse. Am. J. Obstet. Gynecol. 2008, 199, 694.e1–694.e6. [Google Scholar] [CrossRef]
- Elmér, C.; Altman, D.; Engh, M.E.; Axelsen, S.; Väyrynen, T.; Falconer, C. Nordic Transvaginal Mesh Group Trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet. Gynecol. 2009, 113, 117–126. [Google Scholar] [CrossRef]
- Gauruder-Burmester, A.; Koutouzidou, P.; Rohne, J.; Gronewold, M.; Tunn, R. Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2007, 18, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Fattah, M.; Ramsay, I. West of Scotland Study Group Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG 2008, 115, 22–30. [Google Scholar] [CrossRef]
- Nieminen, K.; Hiltunen, R.; Takala, T.; Heiskanen, E.; Merikari, M.; Niemi, K.; Heinonen, P.K. Outcomes after anterior vaginal wall repair with mesh: A randomized, controlled trial with a 3 year follow-up. Am. J. Obstet. Gynecol. 2010, 203, 235.e1–235.e8. [Google Scholar] [CrossRef]
- Damiani, G.R.; Riva, D.; Pellegrino, A.; Gaetani, M.; Tafuri, S.; Turoli, D.; Croce, P.; Loverro, G. Conventional fascial technique versus mesh repair for advanced pelvic organ prolapse: Analysis of recurrences in treated and untreated compartments. J. Obstet. Gynaecol. 2016, 36, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Bondili, A.; Deguara, C.; Cooper, J. Medium-term effects of a monofilament polypropylene mesh for pelvic organ prolapse and sexual function symptoms. J. Obstet. Gynaecol. 2012, 32, 285–290. [Google Scholar] [CrossRef]
- Barber, M.D.; Walters, M.D.; Bump, R.C. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am. J. Obstet. Gynecol. 2005, 193, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Withagen, M.I.; Vierhout, M.E.; Hendriks, J.C.; Kluivers, K.B.; Milani, A.L. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet. Gynecol. 2011, 118, 629–636. [Google Scholar] [CrossRef]
- Hsiao, T.-W.; Ker, C.-R.; Lin, K.-L.; Juan, Y.-S.; Wu, M.-P.; Liu, Y.-Y.; Long, C.-Y. Changes in Sexual Function Following Uphold Transvaginal mesh Surgery for the Treatment of Urogenital Prolapse. Sci. Rep. 2019, 9, 17047. [Google Scholar] [CrossRef] [PubMed]
- Feiner, B.; Jelovsek, J.E.; Maher, C. Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: A systematic review. BJOG 2009, 116, 15–24. [Google Scholar] [CrossRef]
| Patient Demographic | Group A (n = 32) | Group B (n = 32) | p Value |
|---|---|---|---|
| Age a | 63.7 ± 9.9 | 62.9 ± 10.1 | 0.7 |
| BMI a | 25.4 ± 3.7 | 25.4 ± 2.9 | 0.9 |
| Vaginal parity b | 3 (2–6) | 3 (2–6) | 0.8 |
| Postmenopausal c | 26 (81) | 30 (94) | 0.2 |
| Tobacco use c | 0 (0) | 0 (0) | |
| Sexually active c | 10 (31) | 14 (44) | 0.4 |
| Pre-op Dyspareunia c in sexually active | 4 (40) | 2 (14.3) | 0.1 |
| Post-op Dyspareunia c in sexually active | 7 (70) | 6 (42.8) | 0.2 |
| p for post-op compare to pre-op c | 0.3 | 0.2 | |
| Previous surgery | |||
| Hysterectomy c | 2 (6) | 2 (6) | 1.0 |
| POP-Q Measurements (cm) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Aa | p | Ba | p | C | p | ||||
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Preoperative | 2.50 ± 0.86 | 2.27 ± 0.98 | 0.3 | 3.30 ± 1.78 | 3.16 ± 1.87 | 0.7 | 1.48 ± 4.04 | 0.89 ± 3.66 | 0.5 |
| Postoperative | −2.53 ± 1.12 | −2.19 ± 1.22 | 0.2 | −2.53 ± 1.12 | −2.19 ± 1.22 | 0.2 | −5.84 ± 7.40 | −4.57 ± 2.18 | 0.3 |
| D | p | Ap | p | Bp | p | ||||
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Preoperative | −3.07 ± 2.74 | −3.13 ± 2.71 | 0.9 | −0.91 ± 2.03 | −1.09 ± 1.91 | 0.7 | −0.81 ± 2.91 | −0.50 ± 3.13 | 0.6 |
| Postoperative | −4.85 ± 3.24 | −5.22 ± 3.23 | 0.7 | −2.76 ± 0.38 | −2.73 ± 1.10 | 0.9 | −2.79 ± 0.33 | −2.77 ± 1.00 | 0.9 |
| gh | p | pb | p | tvl | p | ||||
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Preoperative | 3.88 ± 0.74 | 3.94 ± 0.70 | 0.7 | 2.22 ± 0.69 | 2.33 ± 0.66 | 0.5 | 7.23 ± 0.79 | 7.36 ± 0.61 | 0.4 |
| Postoperative | 3.16 ± 0.49 | 2.87 ± 1.16 | 0.2 | 2.87 ± 0.36 | 2.75 ± 1.10 | 0.5 | 6.68 ± 0.81 | 6.48 ± 2.54 | 0.6 |
| Concurrent Procedures n (%) | Group A (n = 32) | Group B (n = 32) | p Value |
|---|---|---|---|
| VTH | 16 (50) | 12 (37.5) | 0.4 |
| Sling | 12 (37.5) | 18 (56.2) | 0.2 |
| Posterior Avulta | 14 (43) | 16 (50) | 0.8 |
| SSS | 14 (43) | 8 (25) | 0.1 |
| Posterior repair | 28 (87.5) | 28 (87.5) | 1.0 |
| Subjective Questionnaire Scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Questionnaire | PFDI-20 | p | POPDI-6 | p | CRADI-8 | p | |||
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Preoperative | 40.75 ± 20.91 | 37.43 ± 16.47 | 0.4 | 20.05 ± 12.45 | 19.79 ± 10.36 | 0.9 | 3.91 ± 5.49 | 1.76 ± 3.45 | 0.01 |
| Postoperative | 5.92 ± 5.81 | 7.36 ± 7.03 | 0.3 | 1.43 ± 2.9 | 1.96 ± 3.17 | 0.5 | 0.59 ± 1.47 | 0.59 ± 1.47 | 1 |
| UDI-6 | p | PFIQ-7 | p | POPIQ-7 | p | ||||
| Group A | Group B | Group A | Group B | Group A | Group B | ||||
| Preoperative | 16.80 ± 9.07 | 15.89 ± 7.95 | 0.6 | 25.60 ±17.52 | 27.98 ± 15.43 | 0.7 | 17.26 ±11.39 | 17.11 ± 10.81 | 0.9 |
| Postoperative | 3.91 ± 3.81 | 4.82 ± 4.98 | 0.4 | 0 | 1.64 ± 4.62 | 0.05 | 0 | 0.15 ± 0.84 | 0.3 |
| CRAIQ-7 | p | UIQ-7 | p | ||||||
| Group A | Group B | Group A | Group B | ||||||
| Preoperative | 0.89 ± 2.24 | 1.04 ± 5.09 | 0.8 | 7.44 ± 9.67 | 9.82 ± 10.75 | 0.3 | |||
| Postoperative | 0 | 0 | 0 | 0 | 1.49 ± 4.60 | 0.1 | |||
| 6 Months Post Operation | 12 Months Post Operation | |||||
|---|---|---|---|---|---|---|
| N | n (%) | p * | N | n (%) | p * | |
| Group A | 32 | 4 (12.5) | 0.4 | 31 | 5 (16.1) | 0.19 |
| Group B | 31 | 0 (0) | 30 | 1 (3.3) | ||
| total | 63 | 4 (6.3) | 61 | 6 (9.8) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, C.-H.; Hsu, C.-S.; Ding, D.-C. The Comparison of Outcomes of Transvaginal Mesh Surgery with and without Midline Fascial Plication for the Treatment of Anterior Vaginal Prolapse: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 1888. https://doi.org/10.3390/jcm10091888
Chiang C-H, Hsu C-S, Ding D-C. The Comparison of Outcomes of Transvaginal Mesh Surgery with and without Midline Fascial Plication for the Treatment of Anterior Vaginal Prolapse: A Randomized Controlled Trial. Journal of Clinical Medicine. 2021; 10(9):1888. https://doi.org/10.3390/jcm10091888
Chicago/Turabian StyleChiang, Ching-Hsiang, Chun-Shuo Hsu, and Dah-Ching Ding. 2021. "The Comparison of Outcomes of Transvaginal Mesh Surgery with and without Midline Fascial Plication for the Treatment of Anterior Vaginal Prolapse: A Randomized Controlled Trial" Journal of Clinical Medicine 10, no. 9: 1888. https://doi.org/10.3390/jcm10091888
APA StyleChiang, C.-H., Hsu, C.-S., & Ding, D.-C. (2021). The Comparison of Outcomes of Transvaginal Mesh Surgery with and without Midline Fascial Plication for the Treatment of Anterior Vaginal Prolapse: A Randomized Controlled Trial. Journal of Clinical Medicine, 10(9), 1888. https://doi.org/10.3390/jcm10091888







