Emergency Department as the Entry Point to Inpatient Care: A Nationwide, Population-Based Study in South Korea, 2016–2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Population
2.3. Measures
2.4. Data Analysis
3. Results
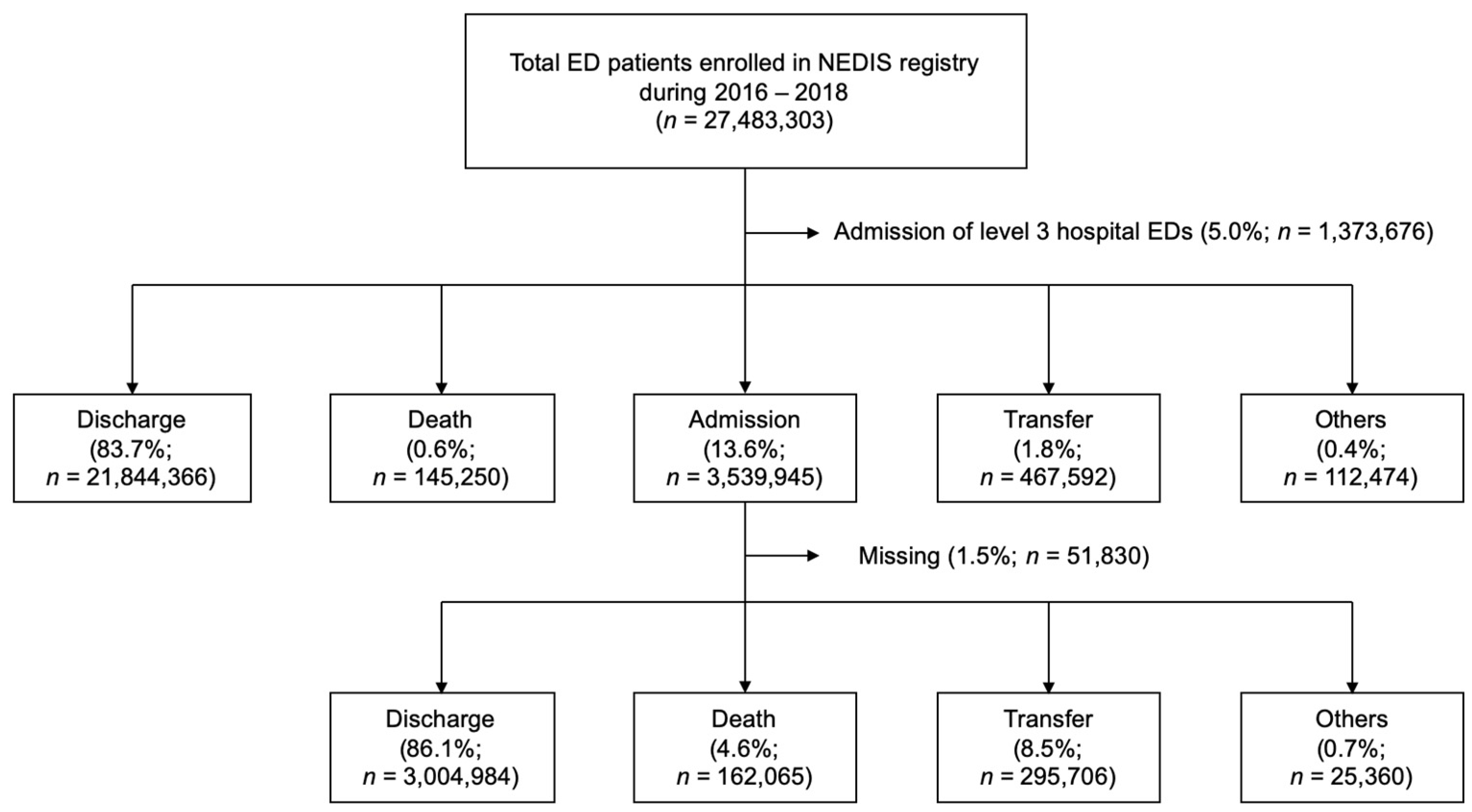
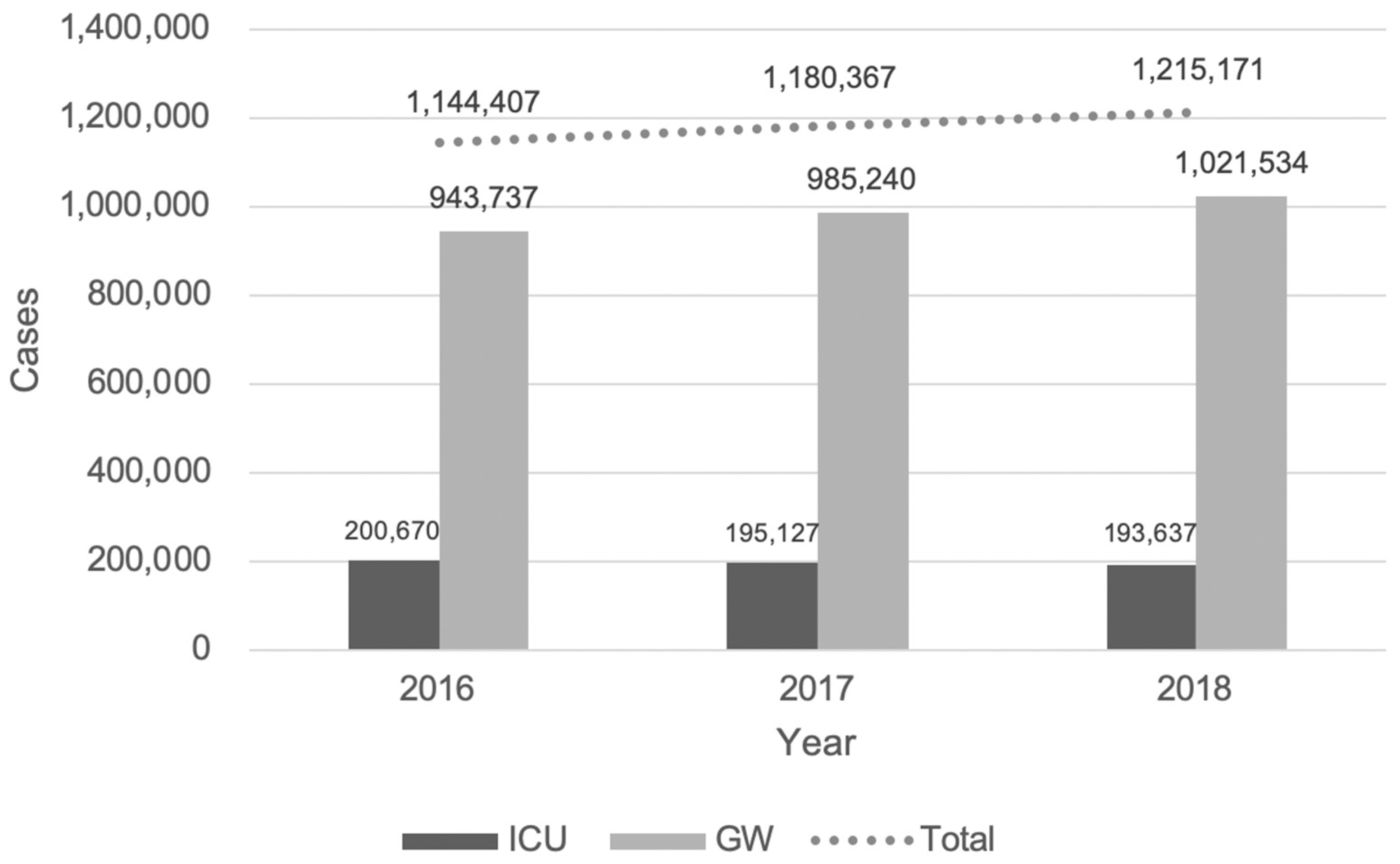
3.1. Baseline Characteristics of the Study Population
3.2. Frequencies of Disease Classes
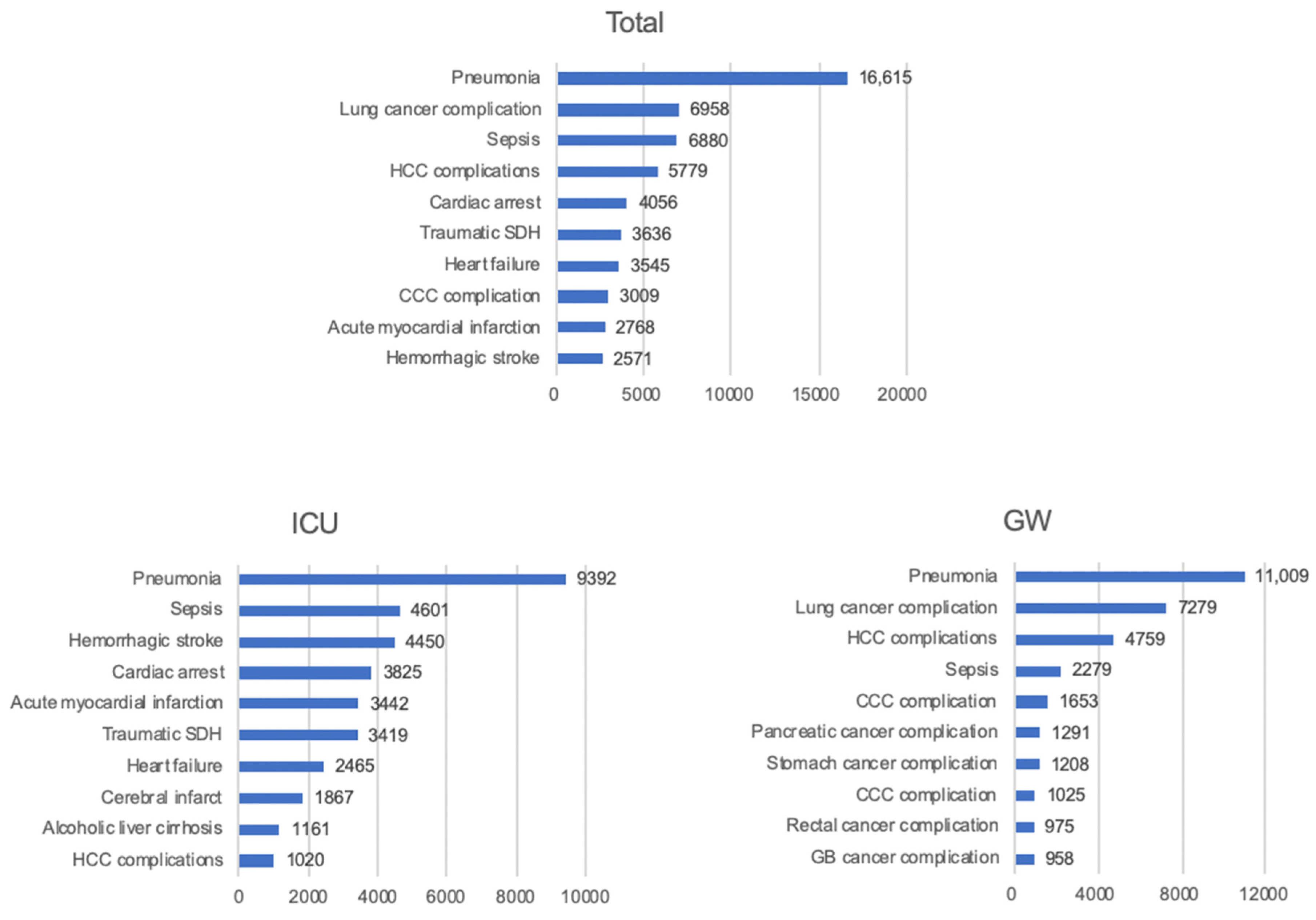
3.3. Common Specific Diagnoses
3.4. Causes of Death Classification
3.5. Causes of Death Diagnoses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borgia, F.; Goodman, S.G.; Halvorsen, S.; Cantor, W.J.; Piscione, F.; Le May, M.R.; Fernandez-Aviles, F.; Sanchez, P.L.; Dimopoulos, K.; Scheller, B.; et al. Early routine percutaneous coronary intervention after fibrinolysis vs. standard therapy in ST-segment elevation myocardial infarction: A meta-analysis. Eur. Heart J. 2010, 31, 2156–2169. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Demaerschalk, B.M.; et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Karaiskakis, M.; Velmahos, G.; Alo, K.; Newton, E.; Murray, J.; Asensio, J.; Belzberg, H.; Berne, T.; Shoemaker, W. Effect on outcome of early intensive management of geriatric trauma patients. Br. J. Surg. 2002, 89, 1319–1322. [Google Scholar] [CrossRef] [PubMed]
- Owens, P.L.; Barrett, M.L.; Gibson, T.B.; Andrews, R.M.; Weinick, R.M.; Mutter, R.L. Emergency department care in the United States: A profile of national data sources. Ann. Emerg. Med. 2010, 56, 150–165. [Google Scholar] [CrossRef]
- Habib, M.I.; Khan, K.M.A. Profile and outcomes of critically ill children in a lower middle-income country. Emerg. Med. J. 2017, 35, 52–55. [Google Scholar] [CrossRef]
- Schuur, J.D.; Venkatesh, A.K. The growing role of emergency departments in hospital admissions. N. Engl. J. Med. 2012, 367, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Morganti, K.G.; Bauhoff, S.; Blanchard, J.C.; Abir, M.; Iyer, N.; Smith, A.; Vesely, J.V.; Okeke, E.N.; Kellermann, A.L. The evolving role of emergency departments in the United States. Rand Health Q. 2013, 3, 3–5. [Google Scholar] [PubMed]
- Greenwald, P.W.; Estevez, R.M.; Clark, S.; Stern, M.E.; Rosen, T.; Flomenbaum, N. The ED as the primary source of hospital admission for older (but not younger) adults. Am. J. Emerg. Med. 2016, 34, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Stein, J.; Hsia, R.Y.; Maselli, J.H.; Gonzales, R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA 2010, 304, 664–670. [Google Scholar] [CrossRef]
- Yap, X.H.; Ng, C.J.; Hsu, K.H.; Chien, C.Y.; Leonard Goh, Z.N.; Li, C.H.; Weng, Y.M.; Hsieh, M.S.; Chen, H.Y.; Seak, J.C.; et al. Predicting need for intensive care unit admission in adult emphysematous pyelonephritis patients at emergency departments: Comparison of five scoring systems. Sci Rep. 2019, 9, 16618. [Google Scholar] [CrossRef] [PubMed]
- Peyrony, O.; Chevret, S.; Meert, A.P.; Perez, P.; Kouatchet, A.; Pene, F.; Mokart, D.; Lemiale, V.; Demoule, A.; Nyunga, M.; et al. Direct admission to the intensive care unit from the emergency department and mortality in critically ill hematology patients. Ann. Intensive Care 2019, 9, 110–119. [Google Scholar] [CrossRef]
- Kwak, Y.H.; Kim, D.K.; Jang, H.Y. Utilization of emergency department by children in Korea. J. Korean Med. Sci. 2012, 27, 1222–1227. [Google Scholar] [CrossRef]
- Chen, S.X.; Chen, S.X.; Fan, K.; Fan, K.; Leung, L.P.; Leung, L.P. Epidemiological characteristics and disease spectrum of emergency patients in two cities in China: Hong Kong and Shenzhen. World J. Emerg. Med. 2020, 11, 48–56. [Google Scholar] [CrossRef]
- Yang, H.J.; Kim, G.W.; Kim, H.; Cho, J.S.; Rho, T.H.; Yoon, H.D.; Lee, M.J. Epidemiology and outcomes in out-of-hospital cardiac arrest: A report from the NEDIS-based cardiac arrest registry in Korea. J. Korean Med. Sci. 2015, 30, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Kim, Y.J.; Jo, Y.H.; Lee, J.H.; Kim, J.; Hwang, J.E.; Jeong, J.; Choi, Y.J. The Korean Triage and Acuity Scale: Associations with admission, disposition, mortality and length of stay in the emergency department. Int. J. Qual. Health Care 2018, 31, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Park, J.B.; Lee, J.; Kim, Y.J.; Lee, J.H.; Lim, T.H. Reliability of Korean Triage and Acuity Scale: Interrater agreement between two experienced nurses by real-time triage and analysis of influencing factors to disagreement of triage levels. J. Korean Med. Sci. 2019, 34, e189. [Google Scholar] [CrossRef]
- Carr, B.G.; Kaye, A.J.; Wiebe, D.J.; Gracias, V.H.; Schwab, C.W.; Reilly, P.M. Emergency department length of stay: A major risk factor for pneumonia in intubated blunt trauma patients. J. Trauma 2007, 63, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Lee, Y.R.; Chae, Y.; Park, S.Y.; Oh, I.H.; Jang, B.H. Translation of Korean medicine use to ICD-codes using National Health Insurance Service-national sample cohort. Evid. Based Complement. Altern. Med. 2016, 2016, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vashi, A.A.; Urech, T.; Carr, B.; Greene, L.; Warsavage Jr, T.; Hsia, R.; Asche, S.M. Identification of emergency care–sensitive conditions and characteristics of emergency department utilization. JAMA Netw. Open 2019, 2, e198642-15. [Google Scholar] [CrossRef]
- Walker, A.S.; Mason, A.; Quan, T.P.; Fawcett, N.J.; Llewelyn, M.; Stoesser, N.; Finney, J.; Davies, J.; Wyllie, D.H.; Crook, D.W.; et al. Mortality risks associated with emergency admissions during weekends and public holidays: An analysis of electronic health records. Lancet 2017, 390, 62–72. [Google Scholar] [CrossRef]
- Flojstrup, M.; Henriksen, D.P.; Brabrand, M. An acute hospital admission greatly increases one year mortality—Getting sick and ending up in hospital is bad for you: A multicentre retrospective cohort study. Eur. J. Intern. Med. 2017, 45, 5–7. [Google Scholar] [CrossRef]
- Koller, M.; Nathwani, D.; Merchant, S.; Gast, C.; Quintana, A.; Ketter, N. Medical resource utilization among patients with ventilator-associated pneumonia: Pooled analysis of randomized studies of doripenem versus comparators. Crit. Care 2015, 14, R84. [Google Scholar] [CrossRef] [PubMed]
- Meyfroidt, G.; Bollaert, P.-E.; Marik, P.E. Acute ischemic stroke in the ICU: To admit or not to admit? Intensive Care Med. 2014, 40, 749–751. [Google Scholar] [CrossRef] [PubMed]
- Majzoub, I.E.; Qdaisat, A.; Chaftari, P.S.; Yeung, S.J.; Sawaya, R.D.; Jizzini, M.; Cruz Carreras, M.T.; Abunafeesa, H.; Elsayem, A.F. Association of emergency department admission and early inpatient palliative care consultation with hospital mortality in a comprehensive care center. Support. Care Cancer 2019, 27, 2649–2655. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total (n = 3,539,945) | ICU (n = 589,434) | GW (n = 2,950,511) | p |
|---|---|---|---|---|
| Gender | ||||
| Male (n, %) | 1,908,254 (53.9) | 350,475 (59.5) | 1,557,779 (52.8) | <0.01 |
| Female (n, %) | 1,631,691 (46.1) | 238,959 (40.5) | 1,392,732 (47.2) | <0.01 |
| Age (year) | 53.4 ± 25.7 | 62.5 ± 20.2 | 51.6 ± 26.3 | <0.01 |
| <18 (n, %) | 491,239 (13.9) | 25,916 (4.4) | 465,323 (15.8) | |
| 18–44 (n, %) | 638,695 (18.0) | 71,253 (12.1) | 567,442 (19.2) | |
| 45–64 (n, %) | 1,013,495 (28.6) | 191,046 (32.4) | 2,950,511 (27.9) | |
| ≥65 (n, %) | 1,396,515 (39.5) | 301,218 (51.1) | 1,095,297 (37.1) | |
| National insurance (n, %) | 3,038,589 (85.8) | 484,277 (82.2) | 2,554,312 (86.6) | <0.01 |
| Route of arrival | <0.01 | |||
| Directly visit (n, %) | 2,391,715 (67.6) | 359,984 (61.1) | 2,031,731 (68.9) | |
| Referred from OPD (n, %) | 169,338 (4.8) | 14,608 (2.5) | 154,730 (5.2) | |
| From other hospitals (n, %) | 977,557 (27.6) | 214,501 (36.4) | 763,056 (25.9) | |
| Others (n, %) | 1076 (0.0) | 244 (0.0) | 832 (0.0) | |
| Unknown | 259 (0.0) | 97 (0.0) | 162 (0.0) | |
| Disease type | <0.01 | |||
| Medical (n, %) | 2,913,685 (82.3) | 474,860 (80.6) | 2,438,825 (82.7) | |
| Trauma (n, %) | 606,336 (17.1) | 97,452 (16.5) | 508,884 (17.2) | |
| Unknown (n, %) | 19,924 (0.6) | 17,122 (2.9) | 2802 (0.1) | |
| EDLOS (min) | 438.0 ± 665.1 | 353.2 ± 741.4 | 455.0 ± 647.5 | <0.01 |
| Level of hospital | <0.01 | |||
| Regional emergency centers (n, %) | 1,293,935 (36.6) | 252,362 (42.8) | 1,041,573 (35.3) | |
| Local emergency centers (n, %) | 2,246,010 (63.4) | 337,072 (57.2) | 1,908,938 (64.7) | |
| KTAS | <0.01 | |||
| 1 (n, %) | 83,101 (2.3) | 58,811 (10.0) | 24,290 (0.8) | |
| 2 (n, %) | 530,657 (15.0) | 221,319 (37.5) | 309,338 (10.5) | |
| 3 (n, %) | 1,846,874 (52.2) | 236,511 (40.1) | 1,610,363 (54.6) | |
| 4 (n, %) | 941,739 (26.6) | 46,837 (7.9) | 894,902 (30.3) | |
| 5 (n, %) | 115,900 (3.3) | 6429 (1.1) | 109,471 (3.7) | |
| Missing (n, %) | 21,674 (0.6) | 19,527 (3.3) | 2147 (0.1) |
| Rank | Total (n = 3,539,945) | ICU (n = 589,434) | GW (n = 2,950,511) | |||
|---|---|---|---|---|---|---|
| Code | Frequency (%) | Code | Frequency (%) | Code | Frequency (%) | |
| 1 | Injury | 608,555 (17.2) | Circulatory system | 207,850 (35.3) | Injury | 509,450 (17.3) |
| 2 | Digestive system | 539,058 (15.2) | Injury | 99,105 (16.8) | Digestive system | 481,367 (16.3) |
| 3 | Circulatory system | 472,996 (13.4) | Respiratory system | 59,857 (10.2) | Respiratory system | 389,908 (13.2) |
| 4 | Respiratory system | 449,765 (12.7) | Digestive system | 57,691 (9.8) | Neoplasms | 268,486 (9.1) |
| 5 | Neoplasms | 291,911 (8.2) | Not classified | 33,385 (5.7) | Circulatory system | 265,146 (9.0) |
| 6 | Genitourinary system | 246,785 (7.0) | Genitourinary system | 27,721 (4.7) | Infectious disease | 221,594 (7.5) |
| 7 | Infectious disease | 243,932 (6.9) | Neoplasms | 23,425 (4.0) | Genitourinary system | 219,064 (7.4) |
| 8 | Not classified | 225,347 (6.4) | Infectious disease | 22,338 (3.8) | Not classified | 191,962 (6.5) |
| 9 | Nervous system | 95,396 (2.7) | Nervous system | 17,118 (2.9) | Skin disorders | 78,314 (2.7) |
| 10 | Musculoskeletal system | 81,880 (2.3) | Metabolic diseases | 16,067 (2.7) | Nervous system | 78,278 (2.7) |
| 11 | Metabolic diseases | 76,389 (2.2) | Contact health services | 5976 (1.0) | Metabolic diseases | 60,322 (2.0) |
| 12 | Pregnancy | 42,813 (1.2) | Mental disorders | 5051 (0.9) | Pregnancy | 40,064 (1.4) |
| 13 | Ear disease | 32,286 (0.9) | Musculoskeletal system | 3566 (0.6) | Ear disease | 31,657 (1.1) |
| 14 | Mental disorders | 31,028 (0.9) | Pregnancy | 2749 (0.5) | Diseases of the skin | 28,155 (1.0) |
| 15 | Skin disorders | 29,394 (0.8) | Blood disorders | 2042 (0.4) | Mental disorders | 25,977 (0.9) |
| 16 | Blood disorders | 25,806 (0.7) | Perinatal disorders | 1720 (0.3) | Blood disorders | 23,764 (0.8) |
| 17 | Contact health services | 18,692 (0.5) | Developmental anomalies | 1503 (0.3) | Contact health services | 16,972 (0.6) |
| 18 | Visual system disease | 11,191 (0.3) | Skin disorders | 1239 (0.2) | Visual system disease | 10,945 (0.4) |
| 19 | Perinatal disorders | 8375 (0.2) | Ear disease | 629 (0.1) | Developmental anomalies | 6355 (0.2) |
| 20 | Developmental anomalies | 7858 (0.2) | Visual system disease | 246 (0.0) | Perinatal disorders | 2399 (0.1) |
| 21 | External causes | 343 (0.0) | External causes | 132 (0.0) | External causes | 211 (0.0) |
| 22 | Special purposes | 145 (0.0) | Special purposes | 24 (0.0) | Special purposes | 121 (0.0) |
| Rank | Total (n = 3,539,945) | ICU (n = 589,434) | GW (n = 2,950,511) | |||
|---|---|---|---|---|---|---|
| Code | Frequency (%) | Code | Frequency (%) | Code | Frequency (%) | |
| 1 | Pneumonia | 158,554 (4.5) | Hemorrhagic stroke | 51,982 (8.8) | Pneumonia | 127,374 (4.3) |
| 2 | Acute appendicitis | 95,558 (2.7) | AMI | 49,156 (8.3) | Acute appendicitis | 93,978 (3.2) |
| 3 | Cerebral infarct | 92,835 (2.6) | Pneumonia | 31,180 (5.3) | Rectal cancer complication | 81,405 (2.8) |
| 4 | AKI | 86,441 (2.4) | Cerebral infarct | 28,475 (4.8) | Cerebral infarct | 69,191 (2.3) |
| 5 | Rectal cancer complications | 84,716 (2.4) | Sepsis | 12,448 (2.1) | AKI | 65,760 (2.2) |
| 6 | Urinary tract infection | 44,178 (1.2) | Heart failure | 10,477 (1.8) | Urinary tract infection | 37,558 (1.3) |
| 7 | AMI | 43,346 (1.2) | AKI | 9236 (1.6) | Femur neck fracture | 34,465 (1.2) |
| 8 | Seizure | 37,413 (1.1) | Ischemic heart disease | 8091 (1.4) | Enterocolitis | 27,266 (0.9) |
| 9 | Femur neck fracture | 35,461 (1.0) | Cardiac arrest | 7831 (1.3) | HCC complication | 21,195 (0.7) |
| 10 | Hemorrhagic stroke | 33,500 (0.9) | Urinary tract infection | 6620 (1.1) | Concussion | 21,000 (0.7) |
| 11 | Enterocolitis | 28,729 (0.8) | CKD | 5127 (0.9) | Acute cholecystitis | 20,888 (0.7) |
| 12 | HCC complications | 24,339 (0.7) | Gastrointestinal hemorrhage | 4890 (0.8) | Fever, unspecified | 20,368 (0.7) |
| 13 | Heart failure | 24,051 (0.7) | Ischemic heart disease | 4568 (0.8) | Acute pancreatitis | 18,956 (0.6) |
| 14 | CKD | 23,140 (0.7) | Gastric ulcer | 3552 (0.6) | Acute cholangitis | 18,529 (0.6) |
| 15 | Concussion | 22,247 (0.6) | Pulmonary embolism | 3519 (0.6) | Neck sprain | 18,403 (0.6) |
| 16 | Acute cholecystitis | 21,880 (0.6) | Rectal cancer terminal complication | 3311 (0.6) | CKD | 18,013 (0.6) |
| 17 | Fever, unspecified | 21,255 (0.6) | Seizure | 3221 (0.5) | Seizure | 17,904 (0.6) |
| 18 | Acute cholangitis | 20,110 (0.6) | HCC complication | 3144 (0.5) | Dizziness | 16,801 (0.6) |
| 19 | Acute pancreatitis | 19,992 (0.6) | Alcoholic liver cirrhosis | 2563 (0.4) | Heart failure | 16,272 (0.6) |
| 20 | Sepsis | 19,628 (0.6) | Pulmonary edema | 2173 (0.4) | Lung cancer complications | 15,201 (0.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-s.; Seo, D.W.; Kim, Y.-J.; Hong, S.I.; Kang, H.; Kim, S.J.; Han, K.S.; Lee, S.W.; Moon, S.; Kim, W.Y. Emergency Department as the Entry Point to Inpatient Care: A Nationwide, Population-Based Study in South Korea, 2016–2018. J. Clin. Med. 2021, 10, 1747. https://doi.org/10.3390/jcm10081747
Kim J-s, Seo DW, Kim Y-J, Hong SI, Kang H, Kim SJ, Han KS, Lee SW, Moon S, Kim WY. Emergency Department as the Entry Point to Inpatient Care: A Nationwide, Population-Based Study in South Korea, 2016–2018. Journal of Clinical Medicine. 2021; 10(8):1747. https://doi.org/10.3390/jcm10081747
Chicago/Turabian StyleKim, June-sung, Dong Woo Seo, Youn-Jung Kim, Seok In Hong, Hyunggoo Kang, Su Jin Kim, Kap Su Han, Sung Woo Lee, Sungwoo Moon, and Won Young Kim. 2021. "Emergency Department as the Entry Point to Inpatient Care: A Nationwide, Population-Based Study in South Korea, 2016–2018" Journal of Clinical Medicine 10, no. 8: 1747. https://doi.org/10.3390/jcm10081747
APA StyleKim, J.-s., Seo, D. W., Kim, Y.-J., Hong, S. I., Kang, H., Kim, S. J., Han, K. S., Lee, S. W., Moon, S., & Kim, W. Y. (2021). Emergency Department as the Entry Point to Inpatient Care: A Nationwide, Population-Based Study in South Korea, 2016–2018. Journal of Clinical Medicine, 10(8), 1747. https://doi.org/10.3390/jcm10081747






