Abstract
Centralization of trauma centers leads to a higher hospital volume of severely injured patients (Injury Severity Score (ISS) > 15), but the effect of volume on outcome remains unclear. The aim of this study was to determine the association between hospital volume of severely injured patients and in-hospital mortality in Dutch Level-1 trauma centers. A retrospective observational cohort study was performed using the Dutch trauma registry. All severely injured adults (ISS > 15) admitted to a Level-1 trauma center between 2015 and 2018 were included. The effect of hospital volume on in-hospital mortality was analyzed with random effects logistic regression models with a random intercept for Level-1 trauma center, adjusted for important demographic and injury characteristics. A total of 11,917 severely injured patients from 13 Dutch Level-1 trauma centers was included in this study. Hospital volume varied from 120 to 410 severely injured patients per year. Observed mortality rates varied between 12% and 24% per center. After case-mix correction, no statistically significant differences between low- and high-volume centers were demonstrated (adjusted odds ratio 0.97 per 50 extra patients per year, 95% Confidence Interval 0.90–1.04, p = 0.44). The variation in hospital volume of the included Level-1 trauma centers was not associated with the outcome of severely injured patients. Our results suggest that well-organized trauma centers with a similar organization of care could potentially achieve comparable outcomes.
1. Introduction
Injury is the major cause of death in adults younger than 45 years of age []. The implementation of trauma systems and dedicated level I trauma centers in the United States and the Netherlands reduced mortality of severely injured patients, usually defined as patients with an Injury Severity Score (ISS) above 15, and improved functional outcome at discharge [,].
Implicit to the centralization of trauma care is the idea that increased volumes of severely injured patients lead to more experienced health care providers, which could result in improved patient outcomes. A recently published systematic review showed that higher hospital volume is associated with lower mortality in severely injured patients []. However, hospitals treating severely injured patients do not only differ in hospital volume. Other factors, such as variation in case mix, organization of care, facilities and geographic location could cause between-center differences. In 1999, an inclusive trauma system was implemented in the Netherlands, which divided hospitals between Level-1, Level-2 and Level-3 trauma centers []. Dutch Level-1 trauma centers are equipped to treat the most severely injured patients 24 h, 7 d per week, including neurotrauma patients, while Level-2 trauma centers are developed for patients with multiple and less severe injuries, and Level-3 trauma centers are developed to treat patients with isolated injuries. Thirteen Level-1 trauma centers cover the country with 17 million inhabitants. The number of severely injured patients treated by these trauma centers differs from approximately 100 to 450 per year [].
In the prehospital phase, Dutch emergency service providers try to discriminate between patients with severe injury and without severe injury. Each trauma region consists of at least one Level-1 trauma center and several Level-2/3 trauma centers. Severely injured patients, patients with a predicted ISS above 15, are transported to Level-1 trauma centers directly []. The triage protocol used is based on the Field Triage Decision Schema established by the American College of Surgeons Committee on Trauma []. The Dutch Helicopter Emergency Services (HEMS) are mostly activated for patients with severe neurotrauma or cardiac arrest.
Since some Level-1 trauma centers in other countries, like the United States, receive higher numbers of severely injured patients [], questions about the introduction of hospital volume cut-offs were raised in order to improve patient outcomes.
Therefore, the aim of this study was to determine whether there is an association between hospital volume of severely injured patients and in-hospital mortality in Dutch Level-1 trauma centers.
2. Materials and Methods
2.1. Study Population
A retrospective observational cohort study was performed using the Dutch Trauma Registry (LTR).
The LTR registers data from all Dutch trauma patients presenting at the Emergency Department (ED) within 48 h after injury, and who are directly admitted to the hospital, referred to another hospital or died at the ED []. Patients that died on arrival are not included in the LTR. LTR is a well-structured nationwide trauma registry that has broad inclusion criteria. This enables studies on the burden of injury, and the quality and efficiency of the trauma care system.
For this analysis, all severely injured adult patients (ISS > 15 and age > 18 years) admitted to a Level-1 trauma center between 2015 and 2018 were included. The AIS codebook 2005 update 08 was used to calculate ISS scores [,]. Incoming transfers from foreign hospitals were excluded from the analysis but did count as case load. The primary outcome was in-hospital mortality.
2.2. Statistical Analysis
First, hospital volume was calculated for each Level-1 trauma center as the number of severely injured patients admitted to a Level-1 trauma center per three years (2015–2017). To assess the volume-outcome relationship, observed mortality rates were plotted against hospital volume for all Level-1 trauma centers. To describe patient characteristics, hospital volume was divided in low- versus high-volume centers with a cut-off of 180 severely injured patients per year. The value of 180 patients per year was chosen based on the median number of patients per year. For the analysis part, missing data were imputed using multiple imputation, assuming missingness at random. All variables, except for the outcome variable, in-hospital mortality, which had no missing values, were imputed. Continuous variables were standardized using Z-score standardization before imputation. There were five imputed datasets created which were pooled using Rubin’s Rules (Table A1 and Figure A1). A complete case analysis was done to validate our results (Appendix B).
Subsequently, multivariable random effects logistic regression models were used to analyze the effect of hospital volume on outcome (in-hospital mortality). Hospital volume was tested for nonlinearity using splines and a likelihood ratio test. Both the unadjusted and adjusted models contained hospital volume and a random intercept for centers to adjust for between-center differences. The adjusted models were based on clinically relevant parameters and included age, sex, ISS, systolic blood pressure at ED, respiratory rate at ED, GCS at ED, prehospital intubation, ASA, penetrating injury and Abbreviated Injury Score (AIS) for head injury []. Age was modelled with a spline function, and an interaction term was added for the relationship between the effect of age and the effect of sex []. Sensitivity analyses were performed in subgroups of patients with ISS > 24, AIS Head < 4 and AIS Head > 3. All random effects logistic regression models were evaluated for multicollinearity by assessing the correlation between the included variables. A cut-off value of −0.8 or 0.8 was used as measure of severe multicollinearity.
Statistical analyses were performed in R statistical software 3.5.1 (R Foundation for Statistical Computation, Vienna, Austria). Random effect models were fitted with Adaptive Gaussian Quadrature with 15 points using the lme4 package. Multiple imputation was done using the mice package in R. The significance level used in this study was 0.05. Our study was done in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) guidelines [].
3. Results
3.1. Patient Characteristics
A total of 11,917 severely injured patients were included in this study. These patients were admitted to 13 Level-1 trauma centers, with mean volumes varying from 120 to 410 severely injured patients per year. For the description of patients’ characteristics, hospital volume was divided in low- (<180 patients per year, N = 3532) and high- (≥180 patients per year, N = 8385) volume centers.
Patients admitted to high-volume centers were younger (median 53, IQR 30–69 versus median 58 IQR 35–74 for lower volume centers), more frequently intubated (31.6% versus 15.6%, Table 1), in shock (6.9% versus 4.6% for low volume centers) and comatose (33.7% versus 24.3% for low volume centers). When looking at the outcome characteristics, patients admitted to high-volume centers had a longer ICU length of stay when admitted to ICU (median 4, IQR 2–9 versus median 3, IQR 2–7 for low volume centers, Table 2). Additionally, in-hospital mortality was slightly higher in high-volume centers (19.8% versus 16.4% for low volume centers, Table 2).

Table 1.
Baseline characteristics divided by low and high hospital volume.

Table 2.
Outcome characteristics divided by low and high hospital volume (ISS > 15).
3.2. Volume-Outcome Relationship: In-Hospital Mortality
The funnel plot of volume and mortality shows small unadjusted differences (Figure 1).
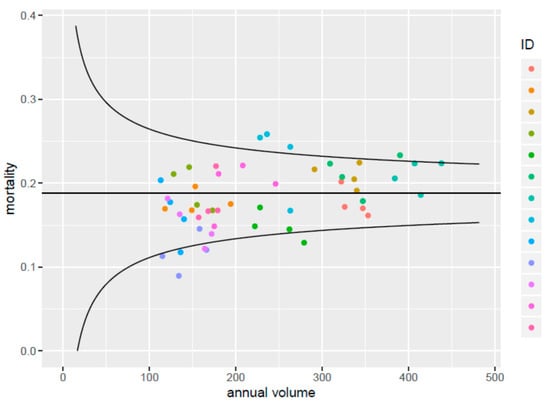
Figure 1.
Funnel plot showing unadjusted differences in mortality rates between trauma centers, with hospital volume of severely injured patients on the x-axis. All centers are plotted for each year separately.
There was a nonsignificant association between higher hospital volume and higher in-hospital mortality according to the unadjusted random effects model (OR 1.04 per 50 extra patients, 95% CI 0.99–1.09, p = 0.10, Table 3). After adjustment, there was no association between hospital volume and in-hospital mortality (OR 0.97 per 50 extra patients, 95%CI 0.90–1.04, p = 0.44). The correlation between the included variables varied between −0.76 and 0.77. The complete case analysis showed similar results (OR: 1.03 per 50 extra patients, 95% CI 0.94–1.12, p = 0.54). Sensitivity analyses showed no significant effect of hospital volume on in-hospital mortality (Table 3).

Table 3.
Effect of hospital volume on in-hospital mortality.
4. Discussion
This study aimed to evaluate whether there was an association between hospital volume and in-hospital mortality among severely injured patients in Dutch Level-1 trauma centers. Patients admitted to the seven largest centers were younger and more severely injured compared to patients admitted to centers with smaller hospital volume. Overall, there was a small variation in hospital volume from 120 to 410 patients per year. After adjusting for differences in case mix, we did not find a relationship between hospital volume and in-hospital mortality of severely injured patients.
Compared to other countries, the variation in hospital volume in the Netherlands was small []. Level-1 trauma centers in the United States treat at least 240 severely injured patients per year with volumes up to 1500 severely injured patients [,], while the largest Dutch trauma centers treat approximately 400 severely injured patients per year []. This could be one of the reasons for not being able to demonstrate a significant volume-outcome relationship in our study. The Netherlands have a relatively large amount of Level-1 trauma centers compared to the number of inhabitants and surface. This creates comparable transfer times and transportation times across the country. Additionally, there are still differences in case mix among Level-1 trauma centers in the Netherlands. Patients in larger centers are more severely injured, and this is visible in the difference between unadjusted and adjusted ORs. The odds ratio goes from above one to below one after adjustment. This implies that there might be a volume-outcome relationship, but differences in case mix make it difficult to show this relationship. Additionally, Dutch trauma centers are well organized in a similar manner, which reduces the impact of volume on outcomes []. Dutch Level-1 trauma centers have to fulfill several criteria in order to become certified, for example, availability of several medical specialties 24/7, a minimum number of ICU beds, damage control surgery facilities and the availability of a CT-scan at the ED.
Centralization of care is suggested to improve cost-effectivity and patient outcomes [,]. Most evidence for the benefit of regionalization in terms of hospital volume is found in elective surgical procedures [,,]. It seems likely that severely injured patients could benefit from centralization, because severely injured patients often require complex care, and having experience in treating those patients could improve patient outcomes. Specifically, in trauma care, the 24/7 availability of experienced medical staff in treating unstable patients and availability of specific specialties like neurosurgery is likely to improve outcomes of severely injured patients. On the other hand, the implementation of comprehensive trauma systems by regionalizing and standardizing complex trauma care in Level-1 facilities is likely to be more effective in improving outcomes after trauma than hospital volume itself []. In the Netherlands, maturation of the trauma system resulted in improved patient outcomes []. This was also shown in the United Kingdom, where a recent publication shows that the development of Major Trauma Networks without volume requirements increases the odds of survival for patients reaching the hospital alive []. Since Dutch Level-1 trauma centers need to meet various high standards, facilities and criterions, there might be little inter-hospital variation in both trauma care for outcomes and outcomes for trauma care of severely injured patients []. This centralization of trauma care in the Netherlands already led to a mortality reduction of 50%, and major improvements in efficiency were found [].
4.1. Strengths and Limitations
This study has several strengths. First, we used data from the national trauma registry, which includes a detailed data collection of all admitted trauma patients in Dutch hospitals, registered by trained data managers []. We were also able to include patients who died due to declared intention. Some variables had a larger number of missing data, for example, respiration rate, for which we used multiple imputation as a rigorous method to handle missing data. Information about transfer and transportation times was not usable for the analysis due to the high amount of missing data. Therefore, these factors cannot be excluded as a potential confounding factor. Second, we assessed hospital volume on a continuous scale, which is statistically more efficient and leads to a more in-depth assessment of the volume-outcome relationship than categorization into low volume and high volume []. However, there were small differences in hospital volume between centers which could introduce a lack of power. The number of included hospitals was small because the Netherlands has only 13 Level 1 trauma centers. This could reduce the global generalizability of our results. Additionally, the possibility of Level II error does exist, although we believe that our sample size and number of included hospitals is large enough. Third, random effects logistic regression models were used instead of conservative logistic regression models. This made it possible to further adjust for random variation between Level-1 trauma centers. We saw that the effect of volume changed substantially after adjusting for case mix, so there were differences in case mix among Level-1 trauma centers. However, we cannot exclude the risk of residual confounding, since it remains difficult to adjust for differences between Level-1 trauma centers fully. In particular, not all detailed information about potential confounders like frailty (medication or cognitive performance) was available. Additionally, we were not able to look at the effect of surgeon volume on in-hospital mortality. The caseload and experience per surgeon could be important for the outcome of the patient, but previous studies showed inconsistent results [,,,]. Future studies could focus on the impact of surgeon volume, transfer status and centralization on outcome. Another limitation of our study is the lack of a good definition of the severely injured patient. The universally used injury severity measure in trauma registries and research is ISS, where ISS > 15 is defined as severely injured. However, questions about the accuracy of ISS were raised. First, an equal Abbreviated Injury Scale (AIS) in different body regions is assumed to be equal in injury severity [,]. Second, ISS does not account for multiple injuries in the same body region [,]. Therefore, it is possible that patients with equal ISS scores do not have the same injury severity, and some Level-1 trauma centers might receive more severely injured patients with equal ISS scores. Future studies should look at the proposed Berlin definition of polytrauma, which captures not only injury severity but also physiological components []. Lastly, we were only able to look at in-hospital mortality as an outcome, while other outcome measures like quality of life are more important for the patients surviving trauma.
4.2. Implications
Our study shows that Level-1 trauma centers with a similar organization of care could potentially achieve similar results. Our findings can be extrapolated to other trauma systems and are comparable to findings from the United Kingdom []. Further research should include quality of life as a patient outcome, since severely injured patients suffer from long-term impairments []. Mortality in severely injured patients shows a decrease over the years, but high-volume centers might achieve better outcomes in quality of life. Additionally, it is important to include the workflow and treatment costs of Level-1 trauma centers. When Level-1 trauma centers become more cost-effective when they treat high volumes of severely injured patients, this could be a reason to introduce national volume cut-offs. With increasing health care costs, it is important to take cost-effectiveness into account when assessing the effect of centralization on trauma care.
5. Conclusions
The variation in hospital volume of the included Level-1 trauma centers was not associated with outcomes of severely injured patients. Our results suggest that well-organized trauma centers with a similar organization of care could potentially achieve comparable outcomes.
Author Contributions
Conceptualization, C.A.S., E.V., J.C.v.D., S.C.E.S., S.P., H.F.L. and D.d.H.; Data curation, E.v.Z.; Formal analysis, C.A.S., E.v.Z. and H.F.L.; Methodology, C.A.S., E.V., E.v.Z. and H.F.L.; Supervision, H.F.L. and D.d.H.; Writing—original draft, C.A.S., E.V., J.C.v.D., S.C.E.S., S.P. and D.d.H.; Writing—review & editing, E.V. Review and editing: LTR Research Group. Resources, data curation: LTR Research Group. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Erasmus MC (protocol code MEC-2017-170 and date of approval 06 April 2017).
Informed Consent Statement
Patient consent was waived due to the observational nature of our study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Participants of LTR Research Group
- F.W. Bloemers, MD, PhD, Trauma Surgery, Department of Surgery, VU University Medical Center, Amsterdam, The Netherlands
- H.J. ten Duis, PhD, University of Groningen, the Netherlands
- M.J.R. Edwards, MD, PhD, Department of Trauma surgery, Radboud University Medical Center, Nijmegen, The Netherlands
- M.A.C. de Jongh, PhD, Brabant Trauma Registry, Network Emergency Care Brabant, Tilburg, the Netherlands
- L.P.H. Leenen, MD, PhD, Department of Trauma surgery, University Medical Center Utrecht, Utrecht, The Netherlands
- P.A. Leenhouts, MD, Department of Surgery, Academic Medical Center, Amsterdam, The Netherlands
- M. Poeze, MD, PhD, Department of Surgery, Maastricht University Medical Center, Maastricht, The Netherlands
- I.B. Schipper, MD, PhD, Department of Trauma surgery, Leiden University Medical Center, Leiden, The Netherlands
- W.R. Spanjersberg, MD, Department of Trauma Surgery, Isala Klinieken, Zwolle, The Netherlands
- L.M. Sturms, PhD, Dutch Network Emergency Care, Utrecht, The Netherlands
- R.J. de Wit, MD, Department of Trauma Surgery, Medisch Spectrum Twente, Enschede, The Netherlands
- K.W. Wendt, MD, PhD, Department of Trauma Surgery, University Medical Center Groningen, University of Groningen
- S. van Zutphen, MD, Department of Surgery Elisabeth Tweesteden Ziekenhuis, Tilburg, The Netherlands
Appendix B

Table A1.
Baseline characteristics of multiple imputed dataset 1 divided by low and high hospital volume.
Table A1.
Baseline characteristics of multiple imputed dataset 1 divided by low and high hospital volume.
| Low Volume <180 Patients/Year (n = 3532) | High Volume ≥180 Patients/Year (n = 8385) | |
|---|---|---|
| Number of Level-1 trauma centers | 6 | 7 |
| Mean hospital volume per year | 147 | 299 |
| Age | 58 (35–74) | 53 (30–69) |
| Male | 2322 (65.7%) | 5783 (69.0%) |
| Penetrating injury | 130 (3.7%) | 288 (3.4%) |
| ISS | 22 (17–26) | 22 (17–29) |
| ISS > 24 | 1444 (40.9%) | 3869 (46.1%) |
| ASA comorbidities 1-A normal healthy patient 2-A patient with mild systemic disease 3-A patient with severe systemic disease 4-A patient with severe systemic disease that is a constant threat to life | 1714 (48.5%) 1403 (39.7%) 410 (11.6%) 5 (0.1%) | 4126 (49.2%) 3037 (36.2%) 1118 (13.3%) 104 (1.2%) |
| Prehospital intubation | 536 (15.2%) | 2545 (30.4%) |
| GCS at arrival Emergency Department (ED) | 14 (7–15) | 13 (3–15) |
| GCS < 8 | 924 (26.2%) | 2810 (33.5%) |
| Respiration rate at arrival ED | 16 (14–20) | 18 (14–20) |
| Systolic blood pressure at arrival ED | 134 (119–159) | 129 (113–150) |
| Systolic Blood Pressure < 90 | 169 (4.8%) | 575 (6.9%) |
| Cardiac arrest | 179 (5.1%) | 582 (6.9%) |
| AIS head > 3 | 1515 (42.9%) | 3622 (43.2%) |
Continuous: median (IQR), categorical: N (%), Injury Severity Score (ISS), Abbreviated Injury Scale (AIS), Glasgow Coma Score (GCS), respiratory rate (RR), systolic blood pressure (SBP), physical status classification system (ASA).
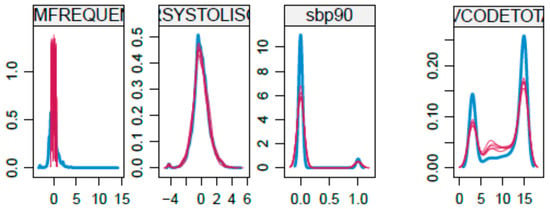
Figure A1.
Density plots of continous variables with missing values of multiple imputed datasets.
References
- Polinder, S.; Haagsma, J.A.; Toet, H.; van Beeck, E.F. Epidemiological burden of minor, major and fatal trauma in a national injury pyramid. Br. J. Surg. 2012, 99 (Suppl. S1), 114–121. [Google Scholar] [CrossRef]
- Celso, B.; Tepas, J.; Langland-Orban, B.; Pracht, E.; Papa, L.; Lottenberg, L.; Flint, L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma 2006, 60, 371–378. [Google Scholar] [CrossRef]
- Lansink, K.W.; Gunning, A.C.; Spijkers, A.T.; Leenen, L.P. Evaluation of trauma care in a mature level I trauma center in the Netherlands: Outcomes in a Dutch mature level I trauma center. World J. Surg. 2013, 37, 2353–2359. [Google Scholar] [CrossRef] [PubMed]
- Sewalt, C.A.; Wiegers, E.J.A.; Venema, E.; Lecky, F.E.; Schuit, S.C.E.; Den Hartog, D.; Lingsma, H.F. The volume-outcome relationship in severely injured patients: A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2018, 85, 810–819. [Google Scholar] [CrossRef] [PubMed]
- Lansink, K.W.; Leenen, L.P. History, development and future of trauma care for multiple injured patients in the Netherlands. Eur. J. Trauma Emerg. Surg. 2013, 39, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, E.J.; Leenen, L. Landelijke Traumaregistratie 2013–2017: Rapportage Nederland; LNAZ: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Van Rein, E.A.J.; Sadiqi, S.; Lansink, K.W.W.; Lichtveld, R.A.; van Vliet, R.; Oner, F.C.; Leenen, L.P.H.; van Heijl, M. The role of emergency medical service providers in the decision-making process of prehospital trauma triage. Eur. J. Trauma Emerg. Surg. 2020, 46, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Dijkink, S.; Krijnen, P.; Hage, A.; Van der Wilden, G.M.; Kasotakis, G.; Hartog, D.D.; Salim, A.; Goslings, J.C.; Bloemers, F.W.; Rhemrev, S.J.; et al. Differences in Characteristics and Outcome of Patients with Penetrating Injuries in the USA and the Netherlands: A Multi-institutional Comparison. World J. Surg. 2018, 42, 3608–3615. [Google Scholar] [CrossRef]
- Driessen, M.L.S.; Sturms, L.M.; Bloemers, F.W.; Ten Duis, H.J.; Edwards, M.J.R.; den Hartog, D.; de Jongh, M.A.C.; Leenhouts, P.A.; Poeze, M.; Schipper, I.B.; et al. The Dutch nationwide trauma registry: The value of capturing all acute trauma admissions. Injury 2020, 51, 2553–2559. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Schluter, P.J. The Trauma and Injury Severity Score (TRISS) revised. Injury 2011, 42, 90–96. [Google Scholar] [CrossRef]
- Bouamra, O.; Jacques, R.; Edwards, A.; Yates, D.W.; Lawrence, T.; Jenks, T.; Woodford, M.; Lecky, F. Prediction modelling for trauma using comorbidity and ‘true’ 30-day outcome. Emerg. Med. J. 2015, 32, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef]
- Eastman, A.B. Resources for optimal care of the injured patient—1993. Bull. Am. Coll. Surg. 1994, 79, 21–27. [Google Scholar]
- Calland, J.F.; Stukenborg, G.J. Trauma centre patient volume and inpatient mortality risk reconsidered. Injury 2016, 47, 1072–1077. [Google Scholar] [CrossRef]
- Gordon, T.A.; Burleyson, G.P.; Tielsch, J.M.; Cameron, J.L. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann. Surg. 1995, 221, 43–49. [Google Scholar] [CrossRef]
- Pollack, M.M.; Alexander, S.R.; Clarke, N.; Ruttimann, U.E.; Tesselaar, H.M.; Bachulis, A.C. Improved outcomes from tertiary center pediatric intensive care: A statewide comparison of tertiary and nontertiary care facilities. Crit. Care Med. 1991, 19, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Cramer, L.D.; Hoskins, W.J.; Brennan, M.F. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998, 280, 1747–1751. [Google Scholar] [CrossRef]
- Birkmeyer, J.D.; Finlayson, S.R.; Tosteson, A.N.; Sharp, S.M.; Warshaw, A.L.; Fisher, E.S. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery 1999, 125, 250–256. [Google Scholar] [CrossRef]
- Ellison, L.M.; Heaney, J.A.; Birkmeyer, J.D. The effect of hospital volume on mortality and resource use after radical prostatectomy. J. Urol. 2000, 163, 867–869. [Google Scholar] [CrossRef]
- Moran, C.G.; Lecky, F.; Bouamra, O.; Lawrence, T.; Edwards, A.; Woodford, M.; Willett, K.; Coats, T.J. Changing the system-major trauma patients and their outcomes in the NHS (England) 2008–2017. EClinicalMedicine 2018, 2, 13–21. [Google Scholar] [CrossRef]
- Altman, D.G.; Royston, P. The cost of dichotomising continuous variables. BMJ 2006, 332, 1080. [Google Scholar] [CrossRef]
- Konvolinka, C.W.; Copes, W.S.; Sacco, W.J. Institution and per-surgeon volume versus survival outcome in Pennsylvania’s trauma centers. Am. J. Surg. 1995, 170, 333–340. [Google Scholar] [CrossRef]
- Margulies, D.R.; Cryer, H.G.; McArthur, D.L.; Lee, S.S.; Bongard, F.S.; Fleming, A.W. Patient volume per surgeon does not predict survival in adult level I trauma centers. J. Trauma 2001, 50, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Sava, J.; Kennedy, S.; Jordan, M.; Wang, D. Does volume matter? The effect of trauma surgeons’ caseload on mortality. J. Trauma 2003, 54, 829–833. [Google Scholar] [CrossRef]
- Chawda, M.N.; Hildebrand, F.; Pape, H.C.; Giannoudis, P.V. Predicting outcome after multiple trauma: Which scoring system? Injury 2004, 35, 347–358. [Google Scholar] [CrossRef]
- Koksal, O.; Ozdemir, F.; Bulut, M.; Aydin, S.; Almacioglu, M.L.; Ozguc, H. Comparison of trauma scoring systems for predicting mortality in firearm injuries. Turk. J. Trauma Emerg. Surg. 2009, 15, 559–564. [Google Scholar]
- Tamim, H.; Al Hazzouri, A.Z.; Mahfoud, Z.; Atoui, M.; El-Chemaly, S. The injury severity score or the new injury severity score for predicting mortality, intensive care unit admission and length of hospital stay: Experience from a university hospital in a developing country. Injury 2008, 39, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Pape, H.C.; Lefering, R.; Butcher, N.; Peitzman, A.; Leenen, L.; Marzi, I.; Lichte, P.; Josten, C.; Bouillon, B.; Schmucker, U.; et al. The definition of polytrauma revisited: An international consensus process and proposal of the new ‘Berlin definition’. J. Trauma Acute Care Surg. 2014, 77, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Sewalt, C.A.; Wiegers, E.J.A.; Lecky, F.E.; den Hartog, D.; Schuit, S.C.E.; Venema, E.; Lingsma, H.F. The volume-outcome relationship among severely injured patients admitted to English major trauma centres: A registry study. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 18. [Google Scholar] [CrossRef] [PubMed]
- Kaske, S.; Lefering, R.; Trentzsch, H.; Driessen, A.; Bouillon, B.; Maegele, M.; Probst, C. Quality of life two years after severe trauma: A single-centre evaluation. Injury 2014, 45 (Suppl. S3), S100–S105. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).