Awake Bruxism—Single-Point Self-Report versus Ecological Momentary Assessment
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Tools
2.2.1. Single-Point Observation Self-Report of AB
- (i)
- Do you grind your teeth during the day (namely, do you move repeatedly your jaw from one side to another and/or forward and backwards with teeth contact)?—Self report grinding.
- (ii)
- Do you clench your teeth during the day (namely, do your lower teeth touch your upper teeth, even if lightly)?—Self-report teeth contact/clenching.
- (iii)
- Do you experience muscle bracing during the day (namely, are your jaw muscles strained, kept in a fixed position without teeth contact)?—Self-report bracing.
2.2.2. EMA with the Use of a Designated Smartphone Application
- (i)
- Relaxed jaw muscles: Condition of perceived relaxed state of jaw muscles, with jaws kept apart (BA (BruxApp)-relaxed).
- (ii)
- Muscle bracing (without tooth contact): Condition of jaw muscle stiffness or tension, as in tooth clenching but with the teeth apart (BA-bracing).
- (iii)
- Teeth contact: Condition of slight tooth contact, as if a 40 µ articulating paper is placed between the dental arches, and the subject is asked to keep it there by lightly touching the teeth together with the mouth closed (BA-teeth contact). The assumption was that participants (all dental students) were well familiar with the articulating paper procedure and that the example would help them to better discriminate between teeth contact and the condition teeth clenching (see below).
- (iv)
- Teeth clenching: All conditions where tooth contact is more marked than those listed above, and the jaw muscles are tensed (BA-clenching).
- (v)
- Teeth grinding: Condition in which the patient gnashes or grinds the opposing teeth, independent of the intensity and direction of antagonist tooth contact (BA-grinding).
2.3. Statistics
3. Results
3.1. Descriptive Results
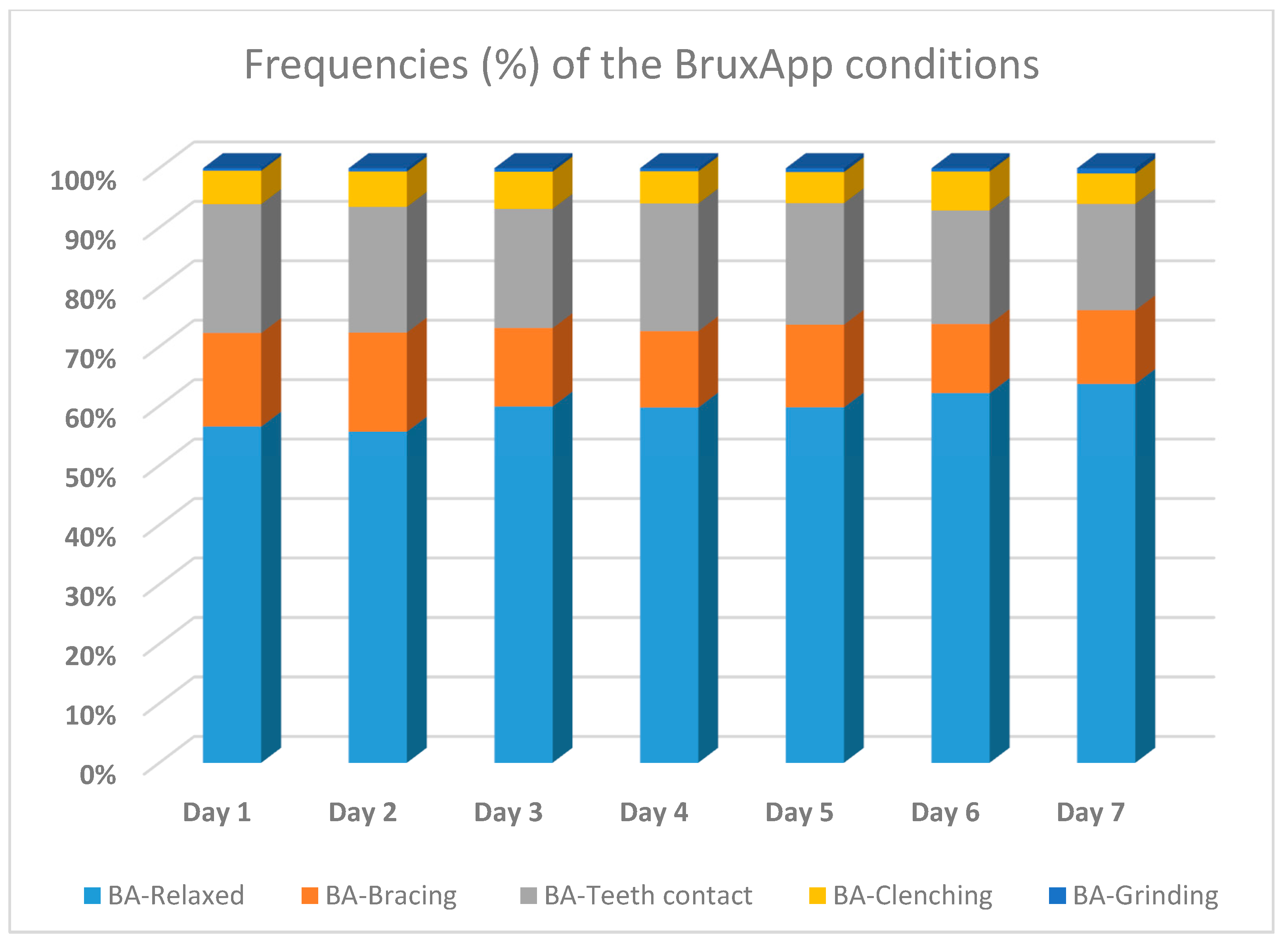
3.2. Frequencies of the BruxApp Behaviors
3.3. Correlations between Single-Point Self-Report AB and the BruxApp Conditions
3.4. Receiver Operating Characteristic (ROC) Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Colonna, A.; Bracci, A.; Lobbezoo, F. Bruxism: A summary of current knowledge on aetiology, assessment, and management. Oral Surg. 2019, 13, 305–452. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Visscher, C.M.; Ahlberg, J.; Manfredini, D. Bruxism and genetics: A review of the literature. J. Oral Rehabil. 2014, 41, 709–714. [Google Scholar] [CrossRef]
- Manfredini, D.; Lobbezoo, F. Role of psychosocial factors in the etiology of bruxism. J. Orofac. Pain 2009, 23, 153–166. [Google Scholar]
- Manfredini, D.; Arreghini, A.; Lombardo, L.; Visentin, A.; Cerea, S.; Castroflorio, T.; Siciliani, G. Assessment of Anxiety and Coping Features in Bruxers: A Portable Electromyographic and Electrocardiographic Study. J. Oral Facial Pain Headache 2016, 30, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Winocur, E.; Uziel, N.; Lisha, T.; Goldsmith, C.; Eli, I. Self-reported Bruxism—Associations with perceived stress, motivation for control, dental anxiety and gagging. J. Oral Rehabil. 2010, 38, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.V.; Kumar, M.P.; Sravanthi, D.; Bin Mohsin, A.H.; Anuhya, V. Bruxism: A Literature Review. J. Int. Oral Health 2015, 6, 105–109. [Google Scholar]
- Raphael, K.G.; Sirois, D.A.; Janal, M.N.; Wigren, P.E.; Dubrovsky, B.; Nemelivsky, L.V.; Klausner, J.J.; Krieger, A.C.; Lavigne, G.J. Sleep bruxism and myofascial temporomandibular disorders: A laboratory-based polysomnographic investigation. J. Am. Dent. Assoc. 2012, 143, 1223–1231. [Google Scholar] [CrossRef]
- Maluly, M.; Andersen, M.L.; Dal-Fabbro, C.; Garbuio, S.; Bittencourt, L.; De Siqueira, J.T.T.; Tufik, S. Polysomnographic Study of the Prevalence of Sleep Bruxism in a Population Sample. J. Dent. Res. 2013, 92, S97–S103. [Google Scholar] [CrossRef]
- Koyano, K.; Tsukiyama, Y.; Ichiki, R.; Kuwata, T. Assessment of bruxism in the clinic. J. Oral Rehabil. 2008, 35, 495–508. [Google Scholar] [CrossRef]
- Pintado, M.R.; Anderson, G.C.; DeLong, R.; Douglas, W.H. Variation in tooth wear in young adults over a two-year period. J. Prosthet. Dent. 1997, 77, 313–320. [Google Scholar] [CrossRef]
- Abe, S.; Yamaguchi, T.; Rompre, P.H.; De Grandmont, P.; Chen, Y.J.; Lavigne, G.J. Tooth wear in young subjects: A dis-criminator between sleep bruxers and controls. Int. J. Prosthodont. 2009, 22, 342–350. [Google Scholar] [PubMed]
- Lavigne, G.; Rompre, P.; Montplaisir, J. Sleep Bruxism: Validity of Clinical Research Diagnostic Criteria in a Controlled Polysomnographic Study. J. Dent. Res. 1996, 75, 546–552. [Google Scholar] [CrossRef]
- Paesani, D.A.; Lobbezoo, F.; Gelos, C.; Guarda-Nardini, L.; Ahlberg, J.; Manfredini, D. Correlation between self-reported and clinically based diagnoses of bruxism in temporomandibular disorders patients. J. Oral Rehabil. 2013, 40, 803–809. [Google Scholar] [CrossRef]
- Takagi, I.; Sakurai, K. Investigation of the factors related to the formation of the buccal mucosa ridging. J. Oral Rehabil. 2003, 30, 565–572. [Google Scholar] [CrossRef]
- Yachida, W.; Arima, T.; Castrillon, E.E.; Baad-Hansen, L.; Ohata, N.; Svensson, P. Diagnostic validity of self-reported measures of sleep bruxism using an ambulatory single-channel EMG device. J. Prosthodont. Res. 2016, 60, 250–257. [Google Scholar] [CrossRef]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological Momentary Assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef] [PubMed]
- McKay, D.; Przeworski, A.; O’Neill, S. Emerging Technologies for Clinical Practice. In Computer-Assisted and Web-Based Innovations in Psychology, Special Education, and Health; Elsevier Academic Press: Amsterdam, The Netherlands, 2016; pp. 365–378. [Google Scholar] [CrossRef]
- Guidance; Ecological Momentary Assessment. Using an Ecological Momentary Assessment to Evaluate Your Digital Health Product. 2016-06-16 pdf. Available online: https://www.gov.uk/guidance/ecological-momentary-assessment (accessed on 31 March 2021).
- Bracci, A.; Djukic, G.; Favero, L.; Salmaso, L.; Guarda-Nardini, L.; Manfredini, D. Frequency of awake bruxism behav-iors in the natural environment. A seven-day, multiple-point observation of real time report in healthy young adults. J. Oral Rehabil. 2018, 45, 423–429. [Google Scholar] [CrossRef]
- Manfredini, D.; Bracci, A.; Djukic, G. BruxApp: The ecological momentary assessment of awake bruxism. Minerva Stomatol. 2016, 65, 252–255. [Google Scholar]
- Zani, A.; Lobbezoo, F.; Bracci, A.; Ahlberg, J.; Manfredini, D. Ecological Momentary Assessment and Intervention Prin-ciples for the Study of Awake Bruxism Behaviors, Part 1: General Principles and Preliminary Data on Healthy Young Italian Adults. Front Neurol. 2019, 10, 169. [Google Scholar] [CrossRef]
- Colonna, A.; Lombardo, L.; Siciliani, G.; Bracci, A.; Guarda-Nardini, L.; Djukic, G.; Manfredini, D. Smartphone-based appli-cation for EMA assessment of awake bruxism: Compliance evaluation in a sample of healthy young adults. Clin. Oral Investig. 2020, 24, 1395–1400. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Winocur, E.; Guarda-Nardini, L.; Paesani, D.; Lobbezoo, F. Epidemiology of Bruxism in Adults: A Systematic Review of the Literature. J. Orofac. Pain 2013, 27, 99–110. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Glaros, A.G.; Kato, T.; Koyano, K.; Lavigne, G.J.; De Leeuw, R.; Manfredini, D.; Svensson, P.; Winocur, E. Bruxism defined and graded: An international consensus. J. Oral Rehabil. 2013, 40, 2–4. [Google Scholar] [CrossRef]
- Perlman, A.E.; Lobbezoo, F.; Zar, A.; Rubin, P.F.; Van Selms, M.K.A.; Winocur, E. Self-Reported bruxism and associated factors in Israeli adolescents. J. Oral Rehabil. 2016, 43, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Van Selms, M.K.; Visscher, C.M.; Naeije, M.; Lobbezoo, F. Bruxism and associated factors among Dutch adolescents. Community Dent. Oral Epidemiol. 2012, 41, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Winocur, E.; Messer, T.; Eli, I.; Emodi-Perlman, A.; Kedem, R.; Reiter, S.; Friedman-Rubin, P. Awake and Sleep Bruxism Among Israeli Adolescents. Front. Neurol. 2019, 10, 443. [Google Scholar] [CrossRef] [PubMed]
- Wetselaar, P.; Vermaire, E.J.H.; Lobbezoo, F.; Schuller, A.A. The prevalence of awake bruxism and sleep bruxism in the Dutch adolescent population. J. Oral Rehabil. 2021, 48, 143–149. [Google Scholar] [CrossRef]
- IADR (International Association of Dental Research). Available online: https://www.iadr.org/Portals/69/docs/Groups/INfORM/Oral-Behavior-Checklist_2013-05-12.pdf (accessed on 26 February 2021).
- Raphael, K.G.; Janal, M.N.; Sirois, D.A.; Dubrovsky, B.; Klausner, J.J.; Krieger, A.C.; Lavigne, G.J. Validity of self-reported sleep bruxism among myofascial temporomandibular disorder patients and controls. J. Oral Rehabil. 2015, 42, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, M.; Kanemura, K.; Tanabe, N.; Gohdo, Y.; Watanabe, A.; Iizuka, T.; Sato, M.; Ishibashi, K. Determination of day-time clenching events in subjects with and without self-reported clenching. J. Oral Rehabil. 2013, 40, 731–736. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Mikami, S.; Maeda, M.; Saito, T.; Nakajima, T.; Yachida, W.; Gotouda, A. Portable and wearable electro-myographic devices for the assessment of sleep bruxism and awake bruxism: A literature review. Cranio 2020. [Google Scholar] [CrossRef]
- Itani, O.; Kaneita, Y.; Ikeda, M.; Kondo, S.; Yamamoto, R.; Osaki, Y.; Kanda, H.; Suzuki, K.; Higuchi, S.; Ohida, T. Disorders of arousal and sleep-related bruxism among Japanese adolescents: A nationwide representative survey. Sleep Med. 2013, 14, 532–541. [Google Scholar] [CrossRef]
- Carra, M.C.; Huynh, N.; Morton, P.; Rompré, P.H.; Papadakis, A.; Remise, C.; Lavigne, G.J. Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population. Eur. J. Oral Sci. 2011, 119, 386–394. [Google Scholar] [CrossRef]
- Soares, L.G.; Costa, I.R.; Júnior, J.D.S.B.; Cerqueira, W.S.B.; De Oliveira, E.S.; De Oliveira, D.W.D.; Gonçalves, P.F.; Glória, J.C.R.; Tavano, K.T.A.; Flecha, O.D. Prevalence of bruxism in undergraduate students. Cranio 2017, 35, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Prado, I.M.; Abreu, L.G.; Silveira, K.S.; Auad, S.M.; Paiva, S.M.; Manfredini, D.; Serra-Negra, J.M. Study of Associated Factors With Probable Sleep Bruxism Among Adolescents. J. Clin. Sleep Med. 2018, 14, 1369–1376. [Google Scholar] [CrossRef]
- Sousa, H.C.S.; Lima, M.D.M.; Dantas Neta, N.B.; Tobias, R.Q.; Moura, M.S.; Moura, L.F.A.D. Prevalence and associated fac-tors to sleep bruxism in adolescents from Teresina. Piauí. Rev Bras Epidemiol. 2018, 21, e180002. [Google Scholar] [PubMed]
- Emodi-Perlman, A.; Eli, I.; Smardz, J.; Uziel, N.; Wieckiewicz, G.; Gilon, E.; Grychowska, N.; Wieckiewicz, M. Temporo-mandibular Disorders and Bruxism Outbreak as a Possible Factor of Orofacial Pain Worsening during the COVID-19 Pan-demic-Concomitant Research in Two Countries. J. Clin. Med. 2020, 12, 3250. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Ahlberg, J.; Wetselaar, P.; Svensson, P.; Lobbezoo, F. The bruxism construct: From cut-off points to a con-tinuum spectrum. J. Oral Rehabil. 2019, 46, 991–997. [Google Scholar] [CrossRef]
- Schiffman, S. Ecological momentary assessment (EMA) in studies of substance use. Psychol. Assess. 2009, 21, 486–497. [Google Scholar] [CrossRef]
- Stone, A.A.; Shiffman, S. Ecological Momentary Assessment (EMA) in behavioral medicine. Ann. Behav. Med. 1999, 16, 199–202. [Google Scholar] [CrossRef]
- Hufford, M. Special methodological challenges and opportunities in ecological momentary assessment. In The Science of Real- time Data Capture: Self-Reports in Health Research; Stone, A., Schiffman, S., Atienzae, A., Nebeling, L., Eds.; Oxford University Press: New York, NY, USA, 2007; pp. 54–75. [Google Scholar]
- Raento, M.; Oulasvirta, A.; Eagle, N. Smartphones: An emerging tool for social scientist. Sociol. Methods Res. 2009, 37, 426–454. [Google Scholar] [CrossRef]
- Runyan, J.D.; Steenbergh, T.A.; Bainbridge, C.; Daugherty, D.A.; Oke, L.; Fry, B.N. A Smartphone Ecological Momentary Assessment/Intervention “App” for Collecting Real-Time Data and Promoting Self-Awareness. PLoS ONE 2013, 8, e71325. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Ahlberg, J.; Aarab, G.; Bracci, A.; Durham, J.; Ettlin, D.; Gallo, L.M.; Koutris, M.; Wetselaar, P.; Svensson, P.; et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB)—Overview and general remarks of a multidimensional bruxism evaluation system. J. Oral Rehabil. 2020, 47, 549–556. [Google Scholar] [CrossRef] [PubMed]
| BruxApp | BA-Relaxed | BA-Bracing | BA-Teeth Contact | BA-Clenching | BA-Grinding | BA-AB |
|---|---|---|---|---|---|---|
| Pearson’s Correlation | −0.297 | 0.220 | 0.148 | 0.225 | 0.111 | 0.320 |
| Sig. (2-tailed) | 0.002 | 0.023 | 0.130 | 0.021 | 0.259 | 0.001 |
| Number | 106 | 106 | 106 | 106 | 106 | 106 |
| Test Result Variable(s) | ROC-AUC | Std. Error | Asymptotic Sig. * | Asymptotic 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| BA-AB | 0.665 | 0.058 | 0.006 | 0.551 | 0.779 |
| BA-bracing | 0.674 | 0.054 | 0.003 | 0.568 | 0.780 |
| BA-teeth contact | 0.556 | 0.059 | 0.349 | 0.439 | 0.672 |
| BA-clenching | 0.604 | 0.060 | 0.081 | 0.485 | 0.722 |
| BA-grinding | 0.505 | 0.060 | 0.936 | 0.387 | 0.623 |
| BA-Relaxed ** | 0.657 | 0.062 | 0.008 | 0.535 | 0.779 |
| Present Study | Zani et al. * [22] | Bracci et al. [20] | |
|---|---|---|---|
| BA-relaxed | 59.7 | 62 | 71 |
| BA-clenching | 5.7 | 3 | 3.7 |
| BA-teeth contact | 20.2 | 20 | 14 |
| BA-grinding | 0.6 | 1 | 0.1 |
| BA-bracing | 13.7 | 14 | 10 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Emodi-Perlman, A.; Manfredini, D.; Shalev, T.; Yevdayev, I.; Frideman-Rubin, P.; Bracci, A.; Arnias-Winocur, O.; Eli, I. Awake Bruxism—Single-Point Self-Report versus Ecological Momentary Assessment. J. Clin. Med. 2021, 10, 1699. https://doi.org/10.3390/jcm10081699
Emodi-Perlman A, Manfredini D, Shalev T, Yevdayev I, Frideman-Rubin P, Bracci A, Arnias-Winocur O, Eli I. Awake Bruxism—Single-Point Self-Report versus Ecological Momentary Assessment. Journal of Clinical Medicine. 2021; 10(8):1699. https://doi.org/10.3390/jcm10081699
Chicago/Turabian StyleEmodi-Perlman, Alona, Daniele Manfredini, Tamar Shalev, Ilanit Yevdayev, Pessia Frideman-Rubin, Alessandro Bracci, Orit Arnias-Winocur, and Ilana Eli. 2021. "Awake Bruxism—Single-Point Self-Report versus Ecological Momentary Assessment" Journal of Clinical Medicine 10, no. 8: 1699. https://doi.org/10.3390/jcm10081699
APA StyleEmodi-Perlman, A., Manfredini, D., Shalev, T., Yevdayev, I., Frideman-Rubin, P., Bracci, A., Arnias-Winocur, O., & Eli, I. (2021). Awake Bruxism—Single-Point Self-Report versus Ecological Momentary Assessment. Journal of Clinical Medicine, 10(8), 1699. https://doi.org/10.3390/jcm10081699






