Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients
Abstract
1. Introduction
2. Methods
Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Drug Classes of OAC/PAI
3.3. Trauma Mechanism
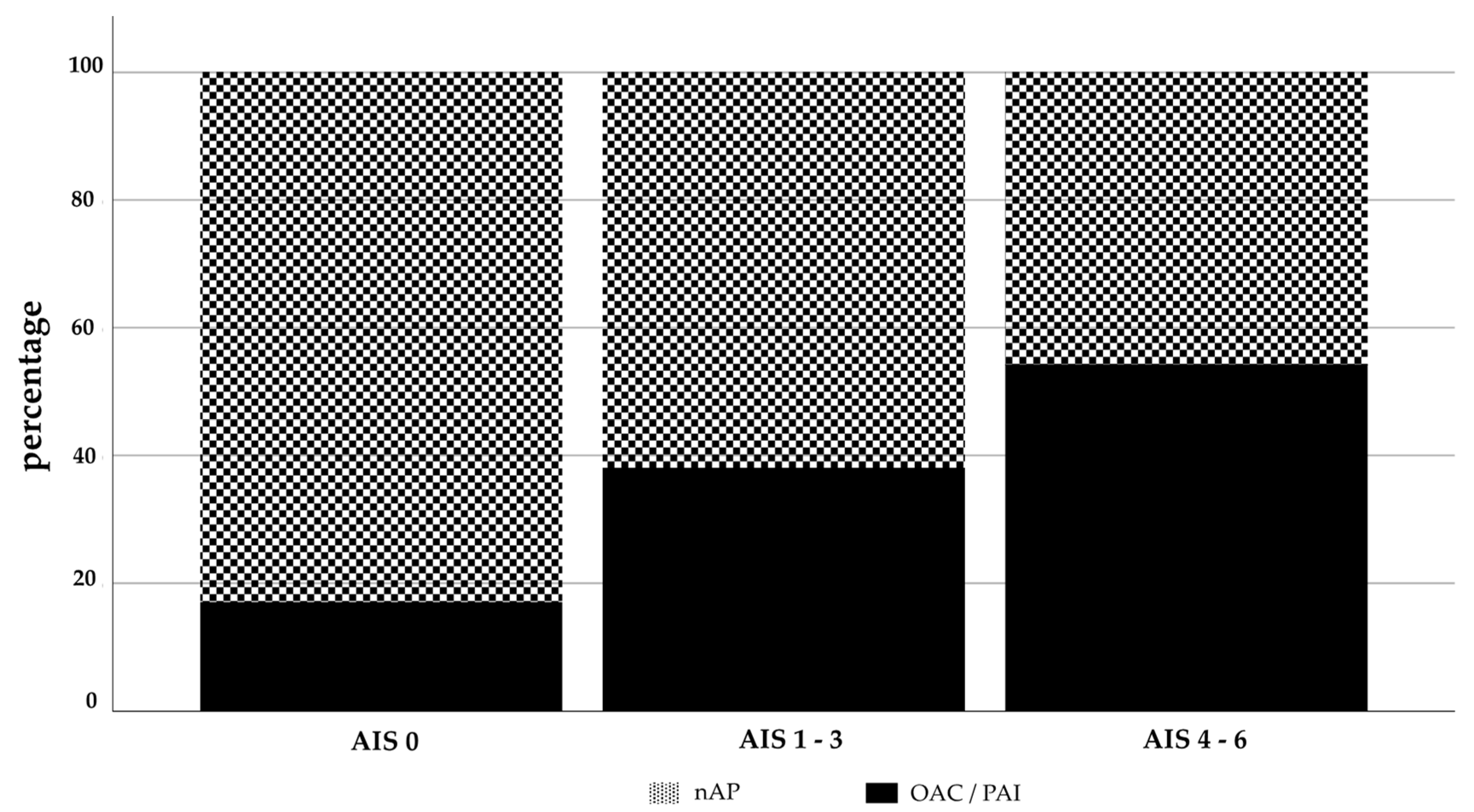
3.4. Effect of OAC/PAI On Head Injuries
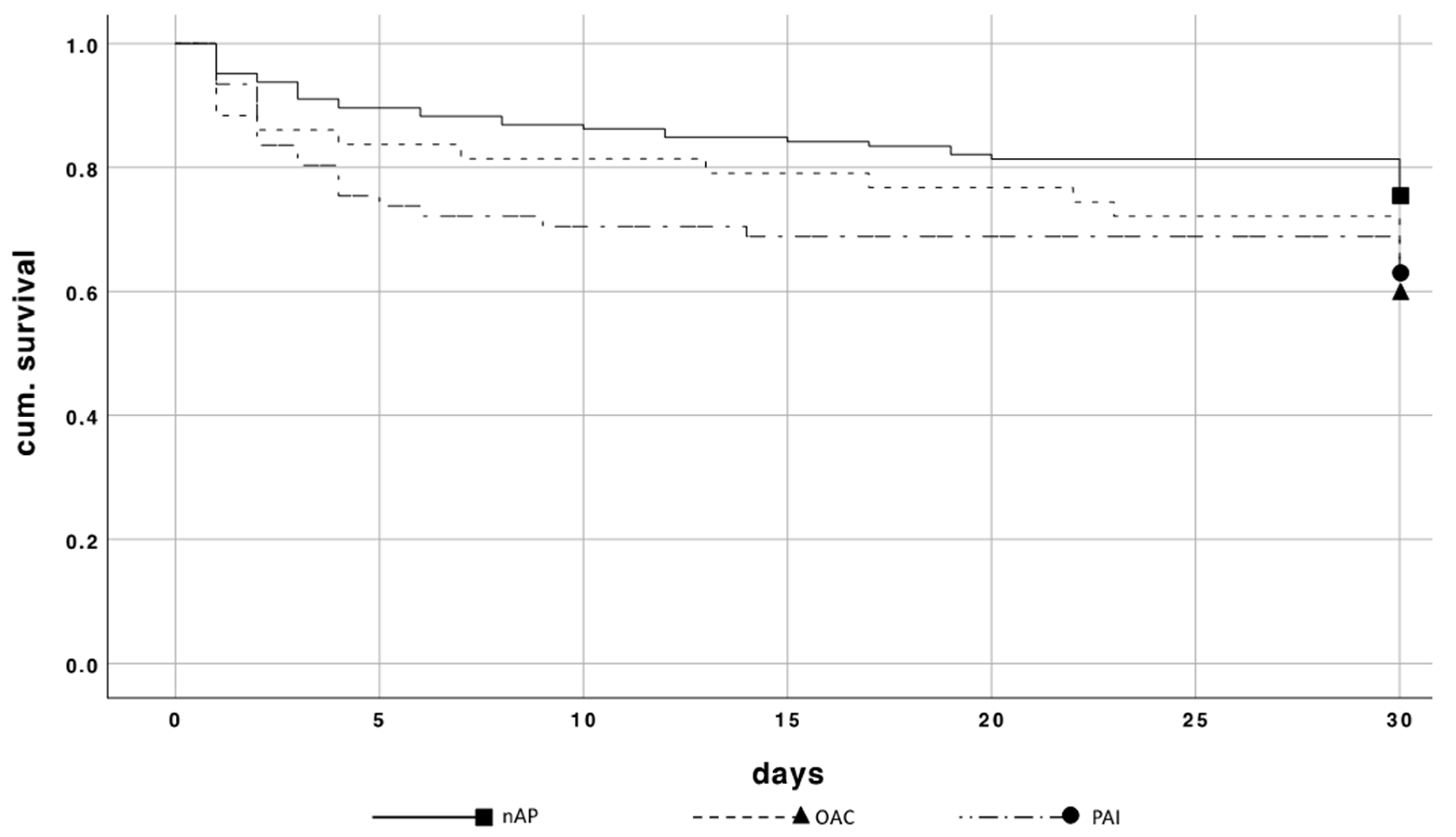
3.5. 30-Day Mortality Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sammy, I.; Lecky, F.; Sutton, A.; Leaviss, J.; O’Cathain, A. Factors Affecting Mortality in Older Trauma Patients-a Systematic Review and Meta-Analysis. Injury 2016, 47, 1170–1183. [Google Scholar] [CrossRef]
- Spering, C.; Lefering, R.; Bouillon, B.; Lehmann, W.; von Eckardstein, K.; Dresing, K.; Sehmisch, S. It Is Time for a Change in the Management of Elderly Severely Injured Patients! An Analysis of 126,015 Patients from the Traumaregister Dgu((R)). Eur. J. Trauma Emerg. Surg. 2020, 46, 487–497. [Google Scholar] [CrossRef]
- Popp, D.; Frankewycz, B.; Lang, S.; Ernstberger, A.; Alt, V.; Worlicek, M.; Kerschbaum, M. Are There Any Red Flag Injuries in Severely Injured Patients in Older Age? J. Clin. Med. 2021, 10, 185. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, K.J.; Jeyaretna, D.S.; Enki, D.G.; Whitfield, P.C. Head Injury in the Elderly: What Are the Outcomes of Neurosurgical Care? World Neurosurg. 2016, 94, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Fawzy, A.M.; Olshansky, B.; Lip, G.Y.H. Frailty and Multi-Morbidities Should Not Govern Oral Anticoagulation Therapy Prescribing for Patients with Atrial Fibrillation. Am. Heart J. 2019, 208, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, C.; Todd, O.; Clegg, A.; Gale, C.P.; Hall, M. Management of Atrial Fibrillation for Older People with Frailty: A Systematic Review and Meta-Analysis. Age Ageing 2019, 48, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Boltz, M.M.; Podany, A.B.; Hollenbeak, C.S.; Armen, S.B. Injuries and Outcomes Associated with Traumatic Falls in the Elderly Population on Oral Anticoagulant Therapy. Injury 2015, 46, 1765–1771. [Google Scholar] [CrossRef] [PubMed]
- Feeney, M.J.; Neulander, M.; DiFiori, M.; Kis, L.; Shapiro, D.S.; Jayaraman, V.; Marshall, W.T., 3rd; Montgomery, S.C. Direct Oral Anticoagulants Compared with Warfarin in Patients with Severe Blunt Trauma. Injury 2017, 48, 47–50. [Google Scholar] [CrossRef]
- Smith, A.T.; Wrenn, K.D.; Barrett, T.W.; Jones, I.D.; Rohde, J.P.; Slovis, C.M.; Russ, S.; Self, W.H. Delayed Intracranial Hemorrhage after Head Trauma in Patients on Direct-Acting Oral Anticoagulants. Am. J. Emerg. Med. 2017, 35, 377.e1–377.e2. [Google Scholar] [CrossRef]
- Hwang, P.; Ong, A.W.; Muller, A.; McNicholas, A.; Martin, A.; Sigal, A.; Fernandez, F.B. Geriatric Patients on Antithrombotic Agents Who Fall: Does Trauma Team Activation Improve Outcomes? Am. Surg. 2019, 85, 721–724. [Google Scholar] [CrossRef]
- Scantling, D.; Kucejko, R.; Williamson, J.; Galvez, A.; Teichman, A.; Gruner, R.; Serniak, N.; McCracken, B. Worsening Head Bleeds in Elderly Blunt Head Trauma Patients Taking Antithrombotics: Delayed Ct Head Fails to Change Management. Injury 2019, 50, 54–60. [Google Scholar] [CrossRef]
- Frink, M.; Lechler, P.; Debus, F.; Ruchholtz, S. Multiple Trauma and Emergency Room Management. Dtsch. Aerzteblatt Online 2017, 114, 497–503. [Google Scholar] [CrossRef]
- Rauf, R.; Von Matthey, F.; Croenlein, M.; Zyskowski, M.; Van Griensven, M.; Biberthaler, P.; Lefering, R.; Huber-Wagner, S.; Dgu, T.S.N.O. Changes in the Temporal Distribution of in-Hospital Mortality in Severely Injured Patients-an Analysis of the Traumaregister Dgu. PLoS ONE 2019, 14, e0212095. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.; Karim, S.; Bowman, S.M.; Recicar, J.; Bledsoe, G.H.; Maxson, R.T. Impact of a Statewide Trauma System on the Triage, Transfer, and Inpatient Mortality of Injured Patients. J. Trauma Acute Care Surg. 2018, 84, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Tennant, C.; Muwanga, C. Polytrauma in the Elderly: Predictors of the Cause and Time of Death. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 26–27. [Google Scholar] [CrossRef] [PubMed]
- Gather, A.; Grutzner, P.A.; Munzberg, M. [Polytrauma in Old Age-Knowledge from the Traumaregister Dgu(R)]. Chirurg 2019, 90, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Labib, N.; Nouh, T.; Winocour, S.; Deckelbaum, D.; Banici, L.; Fata, P.; Razek, T.; Khwaja, K. Severely Injured Geriatric Population: Morbidity, Mortality, and Risk Factors. J. Trauma 2011, 71, 1908–1914. [Google Scholar] [CrossRef] [PubMed]
- Batey, M.; Hecht, J.; Callahan, C.; Wahl, W. Direct Oral Anticoagulants Do Not Worsen Traumatic Brain Injury after Low-Level Falls in the Elderly. Surgery 2018, 164, 814–819. [Google Scholar] [CrossRef]
- Spaniolas, K.; Cheng, J.D.; Gestring, M.L.; Sangosanya, A.; Stassen, N.A.; Bankey, P.E. Ground Level Falls Are Associated with Significant Mortality in Elderly Patients. J. Trauma 2010, 69, 821–825. [Google Scholar] [CrossRef]
- Hukkelhoven, C.W.P.M.; Steyerberg, E.W.; Rampen, A.J.J.; Farace, E.; Habbema, J.D.F.; Marshall, L.F.; Murray, G.D.; Maas, A.I.R. Patient Age and Outcome Following Severe Traumatic Brain Injury: An Analysis of 5600 Patients. J. Neurosurg. 2003, 99, 666–673. [Google Scholar] [CrossRef]
- Moyer, A.J.; Shah, J.; Nowakowski, K.; Martin, A.; McNicholas, A.; Muller, A.; Fernandez, F.B.; Ong, A.W. Does Antithrombotic Drug Use Mandate Trauma Team Activation in Awake Geriatric Patients with Intracranial Hemorrhage? Am. Surg. 2018, 84, 1180–1184. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Macedonio, S.; Gerosa, S.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Lucifero, A.G.; et al. Trauma Coagulopathy and Its Outcomes. Medicina (Kaunas) 2020, 56, 205. [Google Scholar] [CrossRef]
- Beedham, W.; Peck, G.; E Richardson, S.; Tsang, K.; Fertleman, M.; Shipway, D.J. Head Injury in the Elderly—An Overview for the Physician. Clin. Med. (Lond.) 2019, 19, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G. Frailty as a Predictor of Future Falls among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015, 16, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- de Wit, K.; Merali, Z.; Kagoma, Y.K.; Mercier, E. Incidence of Intracranial Bleeding in Seniors Presenting to the Emergency Department after a Fall: A Systematic Review. Injury 2020, 51, 157–163. [Google Scholar] [CrossRef]
- Zhang, P.; Li, Y.; Huang, J.; Zhang, H.; Wang, X.; Dong, L.; Yan, Z.; She, L. Chronic Subdural Haematoma in Antithrombotic Cohorts: Characteristics, Surgical Outcomes, and Recurrence. Br. J. Neurosurg. 2020, 34, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Inohara, T.; Xian, Y.; Liang, L.; Matsouaka, R.A.; Saver, J.L.; Smith, E.E.; Schwamm, L.H.; Reeves, M.J.; Hernandez, A.F.; Bhatt, D.L.; et al. Association of Intracerebral Hemorrhage among Patients Taking Non-Vitamin K Antagonist vs. Vitamin K Antagonist Oral Anticoagulants with in-Hospital Mortality. JAMA 2018, 319, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.S.; Marsh, E.B.; Ali, H.; Nyquist, P.A.; Hanley, D.F.; Ziai, W.C. Comparison of Traumatic Intracranial Hemorrhage Expansion and Outcomes among Patients on Direct Oral Anticoagulants Versus Vitamin K Antagonists. Neurocritical Care 2020, 32, 407–418. [Google Scholar] [CrossRef]
- Lowe, J.A.; Pearson, J.; Leslie, M.; Griffin, R. Ten-Year Incidence of High-Energy Geriatric Trauma at a Level 1 Trauma Center. J. Orthop. Trauma 2018, 32, 129–133. [Google Scholar] [CrossRef]



| OAC/PAI | nAP | p-Value | |
|---|---|---|---|
| Number (n) | 109 | 145 | |
| Male % (n) | 66.1 (72) | 61.4 (89) | 0.444 |
| Age (years ± SD) | 78.3 ± 6.9 | 74.9 ± 7.1 | 0.000 * |
| ISS (Ø ± SD) | 29.0 ± 15.4 | 29.1 ± 14.2 | 0.971 |
| Head AIS ≥ 3% (n) | 81.7 (89) | 63.4 (92) | 0.003 * |
| Average AIS Head | 3.7 ± 1.6 | 2.8 ± 1.9 | 0.000 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerschbaum, M.; Lang, S.; Henssler, L.; Ernstberger, A.; Alt, V.; Pfeifer, C.; Worlicek, M.; Popp, D. Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients. J. Clin. Med. 2021, 10, 1649. https://doi.org/10.3390/jcm10081649
Kerschbaum M, Lang S, Henssler L, Ernstberger A, Alt V, Pfeifer C, Worlicek M, Popp D. Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients. Journal of Clinical Medicine. 2021; 10(8):1649. https://doi.org/10.3390/jcm10081649
Chicago/Turabian StyleKerschbaum, Maximilian, Siegmund Lang, Leopold Henssler, Antonio Ernstberger, Volker Alt, Christian Pfeifer, Michael Worlicek, and Daniel Popp. 2021. "Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients" Journal of Clinical Medicine 10, no. 8: 1649. https://doi.org/10.3390/jcm10081649
APA StyleKerschbaum, M., Lang, S., Henssler, L., Ernstberger, A., Alt, V., Pfeifer, C., Worlicek, M., & Popp, D. (2021). Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients. Journal of Clinical Medicine, 10(8), 1649. https://doi.org/10.3390/jcm10081649








