Analysis of Personality Traits in Patients with Hodgkin Lymphoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Aims and Design of the Study
2.2. Sample and Procedure
2.3. Measures
2.3.1. Interview
2.3.2. NEO Five-Factor Inventory (NEO-FFI)
2.3.3. Personality Inventory for DSM-5 Brief Form (PID-5-BF)
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Patients
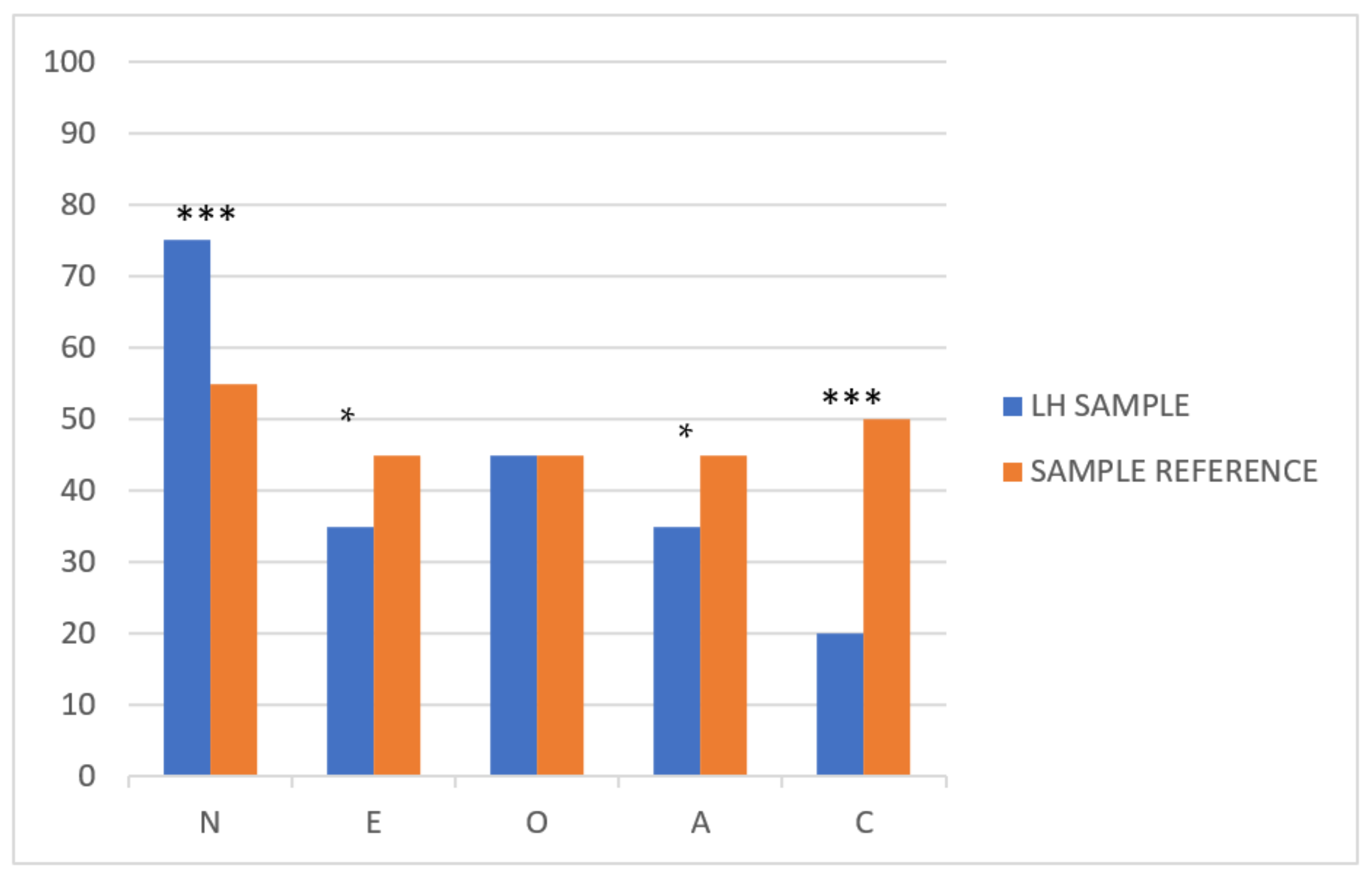
3.2. General Personality Traits
3.3. Maladaptive Personality Traits
3.4. Prevalence of Mental Disorders Others Related Psychological Aspect
3.5. Exploratory Analysis of the Relationship of Personality Traits and Clinical Characteristics of HL and Potential Biomarkers
4. Discussion
5. Conclusions
- To our knowledge, we present, for the first time, the presence of a differential profile of personality traits in HL when compared to the general population.
- Patients with HL showed significantly higher scores of neuroticism and lower conscientiousness, extraversion, and openness.
- Considering maladaptive personality traits, HL patients showed higher levels of detachment and psychoticism.
- All of these translated into the fact that HL patients show a higher prevalence (more than double) of mental illnesses and suicidal ideation or attempts (more than triple) than the general population.
- An exploratory analysis of biomarkers associated with HL personality traits showed that higher scores of neuroticism correlated with higher levels of ESR and RDW, which suggests a potential link between neuroticism and pro-inflammatory activity in HL. Further studies should confirm this observation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eysenck, H.J. Cancer, personality and stress: Prediction and prevention. Adv. Behav. Res. Ther. 1994, 16, 167–215. [Google Scholar] [CrossRef]
- Dahl, A.A. Link between personality and cancer. Future Oncol. 2010, 6, 691–707. [Google Scholar] [CrossRef]
- Herzberg, P.Y.; Lee, S.J.; Heussner, P.; Mumm, F.H.A.; Hilgendorf, I.; Von Harsdorf, S.; Hemmati, P.; Rieger, K.; Greinix, H.T.; Freund, M.; et al. Personality influences quality-of-life assessments in adult patients after allogeneic hematopoietic SCT: Results from a joint evaluation of the prospective German Multicenter Validation Trial and the Fred Hutchinson Cancer Research Center. Bone Marrow Transpl. 2013, 48, 127–134. [Google Scholar] [CrossRef] [PubMed][Green Version]
- İzci, F.; Sarsanov, D.; Erdogan, Z.İ.; Ilgun, A.S.; Celebi, E.; Alco, G.; Kocaman, N.; Ordu, Ç.; Öztürk, A.; Duymaz, T.; et al. Impact of Personality Traits, Anxiety, Depression and Hopelessness Levels on Quality of Life in the Patients with Breast Cancer. Eur. J. Breast Health 2018, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, M.A.; Dawson, A.A.; Walker, L.G. Eysenck Personality Inventory L-scores in patients wtih Hodgkin’s disease and non-Hodgkin’s lymphoma. Psychooncology 1995, 4, 39–45. [Google Scholar] [CrossRef]
- Arts, L.P.J.; Oerlemans, S.; Schoormans, D.; Sanders, A.L.T.M.; Stevens, W.B.C.; Posthuma, E.F.M.; Tick, L.W.; van de Poll-Franse, L.V. Psychological distress among patients with lymphoma: The association with personality and coping strategies. J. Psychosoc. Oncol. Res. Pract. 2021, 3, e041. [Google Scholar]
- McCrae, R.R.; Sutin, A.R. A Five-Factor Theory Perspective on Causal Analysis. Physiol. Behav. 2018, 32, 151–166. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T.J. The Five Factor Theory of personality. Handbook of Personality: Theory and Research; John, O.P., Robbins, R.W., Pervin, L.A., Eds.; The Guilford Press: New York, NY, USA, 2008; pp. 159–181. [Google Scholar]
- Trull, T.J.; Widiger, T.A. Assessment of the five-factor model of personality. J. Personal. Assess. 1997, 68, 228–250. [Google Scholar]
- McCrae, R.R.; John, O.P. An introduction to the five-factor model and its applications. J. Personal. 1992, 60, 175–215. Available online: http://psych.colorado.edu/~carey/Courses/PSYC5112/Readings/psnBig5_Mccrae03.pdf%5Cnpapers2://publication/uuid/93B1ABF6-B622-4726-B2E8-826C2746478D (accessed on 27 December 2020). [CrossRef] [PubMed]
- Pérez-García, A.; Bermudez Moreno, J. Introducción al estudio de la personalidad: Unidades de análisis. In Psicología de la Personalidad; Herder: Freiburg im Breisgau, Germany, 2011; pp. 25–68. [Google Scholar]
- Costa, P.T.; McCrae, R.R.; Löckenhoff, C.E. Personality Across the Life Span. Annu. Rev. Psychol. 2019, 70, 423–448. [Google Scholar] [CrossRef]
- Terracciano, A.; Costa, P.T.; McCrae, R.R. Personality Plasticity After Age 30. Personal. Soc. Psychol. Bull. 2006, 32, 999–1009. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf (accessed on 6 July 2020). [CrossRef] [PubMed]
- Caspi, A.; Roberts, B.W.; Shiner, R.L. Personality Development: Stability and Change. Annu. Rev. Psychol. 2005, 56, 453–484. [Google Scholar] [CrossRef]
- Ruiz, J.; Gutiérrez, F.; Peri, J.M.; Aluja, A.; Baillés, E.; Gutiérrez-Zotes, A.; Vall, G.; Villamón, S.E.; De Alba, A.M.; Rodríguez, M.; et al. Mean-level change in pathological personality dimensions over 4 decades in clinical and community samples: A cross-sectional study. Personal Disord. Theory Res. Treat. 2020, 11, 409–417. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Grov, E.K.; Foss, S.D.; Bremnes, R.M.; Dahl, O.; Klepp, O.; Wist, E.; Dahl, A. The personality trait of neuroticism is strongly associated with long-term morbidity in testicular cancer survivors. Acta Oncol. 2009, 48, 842–849. [Google Scholar] [CrossRef]
- Neeme, M.; Aavik, A.; Aavik, T.; Punab, M. Personality and Utilization of Prostate Cancer Testing: Evidence for the Influence of Neuroticism and Conscientiousness. SAGE Open 2015, 5, 2158244015593324. [Google Scholar] [CrossRef]
- Cardenal, V.; Cerezo, M.V.; Martínez, J.; Ortiz-Tallo, M.; José Blanca, M. Personality, emotions and coping styles: Predictive value for the evolution of cancer patients. Span. J. Psychol. 2012, 15, 756–767. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22774449 (accessed on 20 December 2020). [CrossRef]
- Herraez, I.; Bento, L.; Del Campo, R.; Sas, A.; Ramos, R.; Ibarra, J.; Mestre, F.; Alemany, R.; Bargay, J.; Sampol, A.; et al. Prognostic role of the red blood cell distribution width (RDW)in Hodgkin lymphoma. Cancers 2020, 12, 3262. [Google Scholar] [CrossRef]
- Cordero, P.A.; Pamos, A.; Seisdedos, C.N.; Avia AM, D.; Costa, P.T.; McCrae, R.R. Inventario de personalidad Neo Revisado (NEO PI-R), Inventario Neo Reducido de Cinco Factores (NEO-FFI): Manual Professional; TEA Editor: Madrid, Spain, 2008. [Google Scholar]
- Krueger, R.F.; Derringer, J.; Markon, K.E.; Watson, D.; Skodol, A.E. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol. Med. 2012, 42, 1879–1890. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, F.; Aluja, A.; Peri, J.M.; Calvo, N.; Ferrer, M.; Baillés, E.; Gutiérrez-Zotes, J.A.; Gárriz, M.; Caseras, X.; Markon, K.E.; et al. Psychometric Properties of the Spanish PID-5 in a Clinical and a Community Sample. Assessment 2017, 24, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Henares Montiel, J.; Ruiz-Pérez, I.; Sordo, L. Mental health in Spain and differences by sex, and by autonomous communities. Gac. Sanit. 2020, 34, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Villagrasa, B.; Olaya, B.; Lopez-Anton, R.; de la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of anxiety disorder among older adults in Spain: A meta-analysis. J Affect. Disord. 2019, 246, 408–417. [Google Scholar] [CrossRef]
- Haro, J.M.; Palacín, C.; Vilagut, G.; Martínez, M.; Bernal, M.; Luque, I.; Luque, I.; Codony, M.; Dolz, M.; Alonso, J. Prevalencia de los trastornos mentales y factores asociados: Resultados del estudio ESEMeD-España. Med. Clin. 2006, 126, 445–451. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social; Instituto Nacional de Estadística. Encuesta Nacional de Salud 2017. Available online: http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176783&menu=resultados&secc=1254736195650&idp=1254735573175 (accessed on 12 May 2020).
- Miret, M.; Caballero, F.F.; Huerta-Ramírez, R.; Moneta, M.V.; Olaya, B.; Chatterji, S.; Haro, J.M.; Ayuso-Mateos, J.L. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J. Affect. Disord. 2014, 163, 1–9. [Google Scholar] [CrossRef]
- Gabilondo, A.; Alonso, J.; Pinto-Meza, A.; Vilagut, G.; Fernández, A.; Serrano-Blanco, A.; Almansa, J.; Codony, M.; Haro, J.M. Prevalencia y factores de riesgo de las ideas, planes e intentos de suicidio en la población general española. Resultados del estudio ESEMeD. Med. Clin. 2007, 129, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Hagger-Johnson, G.; Sabia, S.; Nabi, H.; Brunner, E.; Kivimäki, M.; Singh-Manoux, A. Low Conscientiousness and Risk of All-Cause, Cardiovascular and Cancer Mortality over 17 Years: Whitehall II Cohort Study. J. Psychosom. Res. 2012, 73, 98–103. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf (accessed on 20 December 2020). [CrossRef]
- Bogg, T.; Roberts, B.W. The Case for Conscientiousness: Evidence and Implications for a Personality Trait Marker of Health and Longevity. Ann. Behav. Med. 2013, 45, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Nakaya, N.; Hansen, P.E.; Schapiro, I.R.; Eplov, L.F.; Saito-Nakaya, K.; Uchitomi, Y.; Johansen, C. Personality traits and cancer survival: A Danish cohort study. Br. J. Cancer. 2006, 95, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Lahey, B.B. Public Health Significance of Neuroticism. Am. Psychol. 2009, 64, 241–256. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.; Cooper, B.; Paul, S.; Hammer, M.; Conley, Y.P.; Levine, J.D.; Miaskowski, C.; Dunn, L.B. Association of Personality Profiles with Depressive, Anxiety, and Cancer-related Symptoms in Patients Undergoing Chemotherapy. Personal. Individ. Differ. 2017, 117, 130–138. [Google Scholar] [CrossRef]
- Langford, D.J.; Morgan, S.; Cooper, B.; Paul, S.; Kober, K.; Wright, F.; Hammer, M.J.; Conley, Y.P.; Levine, J.D.; Miaskowski, C.; et al. Association of personality profiles with coping and adjustment to cancer among patients undergoing chemotherapy. Psycho Oncology 2020, 29, 1060–1067. [Google Scholar] [CrossRef]
- Rochefort, C.; Hoerger, M.; Turiano, N.A.; Duberstein, P. Big Five personality and health in adults with and without cancer. J. Health Psychol. 2019, 24, 1494–1504. [Google Scholar] [CrossRef]
- Joyner, C.; Loprinzi, P.D. Longitudinal Effects of Personality on Physical Activity Among College Students: Examining Executive Function as a Potential Moderator. Psychol. Rep. 2018, 121, 344–355. [Google Scholar] [CrossRef]
- Hill, P.L.; Turiano, N.A.; Hurd, M.D.; Mroczek, D.K.; Roberts, B. Conscientiousness and Longevity: An Examination of Possible Mediators. Health Psychol. 2011, 30, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Terracciano, A.; Löckenhoff, C.E.; Zonderman, A.B.; Ferruci, L.; Costa, P.J. Personality predictors of longevity: Activity, Emotional Stability, and Conscientiousness. Psychosom. Med. 2008, 70, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Gleason, M.E.J.; Weinstein, Y.; Balsis, S.; Oltmanns, T.F. The enduring impact of maladaptive personality traits on relationship quality and health in later life. J. Personal. 2014, 82, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Griffin, S.A.; Samuel, D.B. Capturing the DSM-5 Alternative Personality Disorder Model Traits in the Five-Factor Model’s Nomological Net. J. Personal. 2017, 85, 220–231. [Google Scholar] [CrossRef]
- Watson, D.; Stasik, S.M.; Ro, E.; Clark, L.A. Integrating Normal and Pathological Personality: Relating the DSM-5 Trait-Dimensional Model to General Traits of Personality. Assessment 2013, 20, 312–326. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Lepine, J.P. Overview of key data from the European Study of the Epidemiology of Mental Disorders (ESE- MeD). J. Clin. Psychiatry 2007, 68, 3–9. [Google Scholar]
- Fundación Española para la Prevención del Suicidio. Observatorio del Suicidio en España 2017. 2019, Volume 2018, pp. 1–8. Available online: https://www.fsme.es/observatorio-del-suicidio-2018/ (accessed on 10 June 2020).
- Friedman, S.; Henry-Amar, M.; Cosset, J.M.; Carde, P.; Hayat, M.; Dupouy, N.; Tubiana, M. Evolution of erythrocyte sedimentation rate as predictor of early relapse in posttherapy early-stage Hodgkin’s disease. J. Clin. Oncol. 1988, 6, 596–602. [Google Scholar] [CrossRef]
- Semba, R.D.; Patel, K.V.; Ferrucci, L.; Sun, K.; Roy, C.N.; Guralnik, J.M.; Fried, L.P. Serum antioxidants and inflammation predict red cell distribution width in older women: The Women’s Health and Aging Study I. Clin. Nutr. 2010, 29, 600–604. [Google Scholar] [CrossRef]
- Lippi, G.; Tagher, G.; Montagnana, M.; Salvagno, G.L.; Zopinni, G.; Guidi, G.C. Relation Between Red Blood Cell Distribution Width and Inflammatory Biomarkers in a Large Cohort of Unselected Outpatients. Arch. Pathol. Lab. Med. 2009, 133, 628–632. [Google Scholar] [CrossRef]
- Sutin, A.R.; Terracciano, A.; Deiana, B.; Naitza, S.; Ferrucci, L.; Uda, M.; Schlessinger, D.; Costa, P.T., Jr. High Neuroticism and Low Conscientiousness Are Associated with Interleukin-6. Psychol. Med. 2010, 40, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, M.; Kumano-Go, T.; Suganuma, N.; Adachi, H.; Yamamura, S.; Morishima, H.; Shigedo, Y.; Mikami, A.; Takeda, M.; Sugita, Y. Anxiety, neuroticism and oxidative stress: Cross-sectional study in non-smoking college students. Psychiatry Clin. Neurosci. 2010, 64, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.; Ajdacic-Gross, V.; Strippoli, M.-P.; Gholam-Rezaee, M.; Glaus, J.; Vandeleur, C.; Castelao, E.; Vollenweider, P.; Preisig, M.; von Känel, R. Associations of Personality Traits with chronic low-grade inflammation in a swiss community sample. Front. Psychiatry 2019, 10, 819. [Google Scholar] [CrossRef] [PubMed]
- Parmač Kovačić, M.; Galić, Z.; Jerneić, Ž. Social desirability scales as indicators of self-enhancement and impression management. J. Personal. Assess. 2014, 96, 532–543. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, S.; Bagby, M.M.; Kushner, S.C.; Burchett, D. The impact of underreporting and overreporting on the validity of the personality inventory for DSM-5 (PID-5): A simulation analog design investigation. Psychol. Assess. 2017, 29, 473–478. [Google Scholar] [CrossRef]
- Keeley, J.W.; Webb, C.; Peterson, D.; Roussin, L.; Flanagan, E.H. Development of a Response Inconsistency Scale for the Personality Inventory for DSM–5. J. Personal. Assess. 2016, 98, 351–359. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.D. Measuring personality constructs: The advantages and disadvantages of self-reports, informant reports and behavioural assessments. Enquire 2008, 1, 1–19. [Google Scholar]
| Clinical Characteristics | n (%) |
|---|---|
| Median age (range) (years) | 37 (14–76) |
| Age > 45 years | 35 (37%) |
| Age > 60 years | 12 (13%) |
| Sex (Male/Female) | 49 (52%)/46 (48%) |
Medical center:
| 60 (63%) 20 (21%) 15 (16%) |
AA stage:
| 55 (59%) 38 (41%) |
| B-symptoms: | 33 (36%) |
| Bulky disease: | 20 (22%) |
| ECOG PS >1: | 7 (8%) |
| GHSG ≥1 (Early HL): | 23 (59%) |
| IPS > 3 (Advanced HL): | 8 (24%) |
Frontline Chemotherapy:
| 89 (94%) 2 (2%) 1 (1%) 2 (2%) |
| Radiotherapy: | 29 (31%) |
Response:
| 81 (85%) 5 (5%) 9 (9%) |
| Median follow-up (range) (months) | 72 (5–415) |
| 6 years-EFS (95%CI) | 79% (74–84) |
| Progression | 17 (18%) |
| Exitus | 1 (10%) |
| n (%) | |
|---|---|
| Civil Status | |
| Single | 46 (48.4) |
| Married | 38 (40) |
| Separated/Divorced | 8 (8.4) |
| Widowed | 3 (3.2) |
| Educational level | |
| Uneducated | 2 (2.1) |
| Primary | 18 (18.9) |
| Secondary | 31 (32.6) |
| High School | 42 (44.2) |
| Substance abuse | |
| No habits of abuse | 52 (54.7) |
| Tobacco | 13 (13.7) |
| Alcohol | 7 (7.4) |
| Cannabis | 5 (5.3) |
| Several substances | 18 (18.9) |
| Vital stressor | |
| No vital stressor | 28 (29.5) |
| Mild | 3 (3.2) |
| Moderate | 10 (10.5) |
| Intense | 53 (55.8) |
| NEO-FFI | α | Reference Population * | HL Sample | t ** | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean Difference | CI (95%) | p | ||
| Neuroticism | 0.852 | 15.35 | 7.40 | 20.61 | 9.31 | 5.26 | (3.30; 7.23) | 0.000 |
| Extraversion | 0.829 | 32.59 | 6.35 | 30.36 | 7.94 | −2.22 | (−3.93, −0.52) | 0.011 |
| Openness | 0.774 | 28.64 | 6.56 | 28.64 | 7.69 | 0.006 | (−1.68, 1.69) | 0.994 |
| Agreeableness | 0.676 | 32.79 | 5.67 | 31.36 | 6.35 | −1.42 | (−2.77, −0.067) | 0.040 |
| Conscientiousness | 0.798 | 36.01 | 6.02 | 32.21 | 7.35 | −3.79 | (−5.33, −2.25) | 0.000 |
| PID-5-BF | α | Reference Population * | HL Sample | Z ** | ||||
|---|---|---|---|---|---|---|---|---|
| M | SD | Med | M | SD | Med | p | ||
| Negative affectivity | 0.720 | 0.940 | 0.431 | 0.906 | 1.384 | 0.704 | 1.40 | 0.000 |
| Detachment | 0.710 | 0.626 | 0.432 | 0.562 | 0.758 | 0.620 | 0.70 | 0.006 |
| Psychoticism | 0.681 | 0.392 | 0.407 | 0.250 | 0.821 | 0.608 | 0.80 | 0.000 |
| Antagonism | 0.603 | 0.497 | 0.419 | 0.400 | 0.302 | 0.372 | 0.20 | 0.002 |
| Disinhibition | 0.752 | 0.742 | 0.465 | 0.687 | 0.780 | 0.638 | 0.60 | 0.224 |
| Current Series | Other Series | |||||
|---|---|---|---|---|---|---|
| Global | Male | Female | Global | Male | Female | |
| Mental disorders (%) | 39 (41%) | 18 (37%) | 21 (46%) | 15.4% [24] | 9.7% [24]. | 20.2% [24]. |
Mood disorders:
| 33 (35%) 26 (28%) 20 (21%) | 8 (16%) 7 (14%) | 19 (41%) 12 (26%) | 6.7% [25] 6.7%) [26] | 4.3% [25] 4% [27] | 9.1% [25] 9% [27] |
| Suicidal ideation | 14 (15%) | 6 (12%) | 8 (17%) | 4% [28] | - | - |
| Suicidal attempts | 6 (6%) | 4 (8%) | 2 (4%) | 1.48% [29] | - | - |
| Characteristics/Biomarkers | High Neuroticism (>27). n (%) | p | Very Low Conscientiousness (<26). n (%) | p |
|---|---|---|---|---|
Age:
| 13 (23%) 5 (15%) | 0.42 | 13 (22%) 3 (9%) | 0.12 |
Sex:
| 4 (9%) 14 (32%) | 0.009 | 7 (15%) 9 (20%) | 0.52 |
AA stage:
| 10 (19%) 7 (20%) | 1 | 10 (19%) 5 (14%) | 0.58 |
B-symptoms:
| 7 (22%) 9 (17%) | 0.58 | 8 (26%) 7 (13%) | 0.12 |
Bulky mass:
| 6 (30%) 10 (16%) | 0.15 | 3 (15%) 12 (19%) | 0.7 |
IPS:
| 8 (14%) 3 (30%) | 0.23 | 7 (13%) 3 (30%) | 0.16 |
ESR:
| 3 (9%) 11 (26%) | 0.046 | 6 (17%) 7 (17%) | 0.96 |
RCP:
| 2 (9%) 10 (23%) | 0.2 | 5 (23%) 6 (14%) | 0.37 |
RDW:
| 2 (7%) 9 (29%) | 0.023 | 4 (13%) 7 (23%) | 0.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roso-Bas, F.; Alonso-Llobregat, M.D.; Bento, L.; Sanchez-Gonzalez, B.; Herraez, I.; Garcia-Dilla, P.; Vallespir, C.; Rado, F.; Rodriguez, R.; Garcia-Pallarols, F.; et al. Analysis of Personality Traits in Patients with Hodgkin Lymphoma. J. Clin. Med. 2021, 10, 1631. https://doi.org/10.3390/jcm10081631
Roso-Bas F, Alonso-Llobregat MD, Bento L, Sanchez-Gonzalez B, Herraez I, Garcia-Dilla P, Vallespir C, Rado F, Rodriguez R, Garcia-Pallarols F, et al. Analysis of Personality Traits in Patients with Hodgkin Lymphoma. Journal of Clinical Medicine. 2021; 10(8):1631. https://doi.org/10.3390/jcm10081631
Chicago/Turabian StyleRoso-Bas, Fatima, Maria Dolores Alonso-Llobregat, Leyre Bento, Blanca Sanchez-Gonzalez, Ines Herraez, Pilar Garcia-Dilla, Catalina Vallespir, Francesca Rado, Raquel Rodriguez, Francesc Garcia-Pallarols, and et al. 2021. "Analysis of Personality Traits in Patients with Hodgkin Lymphoma" Journal of Clinical Medicine 10, no. 8: 1631. https://doi.org/10.3390/jcm10081631
APA StyleRoso-Bas, F., Alonso-Llobregat, M. D., Bento, L., Sanchez-Gonzalez, B., Herraez, I., Garcia-Dilla, P., Vallespir, C., Rado, F., Rodriguez, R., Garcia-Pallarols, F., Aguirre, I., Bargay, J., Sampol, A., Salar, A., & Gutierrez, A. (2021). Analysis of Personality Traits in Patients with Hodgkin Lymphoma. Journal of Clinical Medicine, 10(8), 1631. https://doi.org/10.3390/jcm10081631







