Rescue Operations Lead to Increased Cardiovascular Stress in HEMS Crew Members: A Prospective Pilot Study of a German HEMS Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Design and Procedure
2.3. Long-Term Blood Pressure and Long-Term Electrocardiography Measurements
2.4. Cardiac Events
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Medical History
3.3. Operating Characteristics
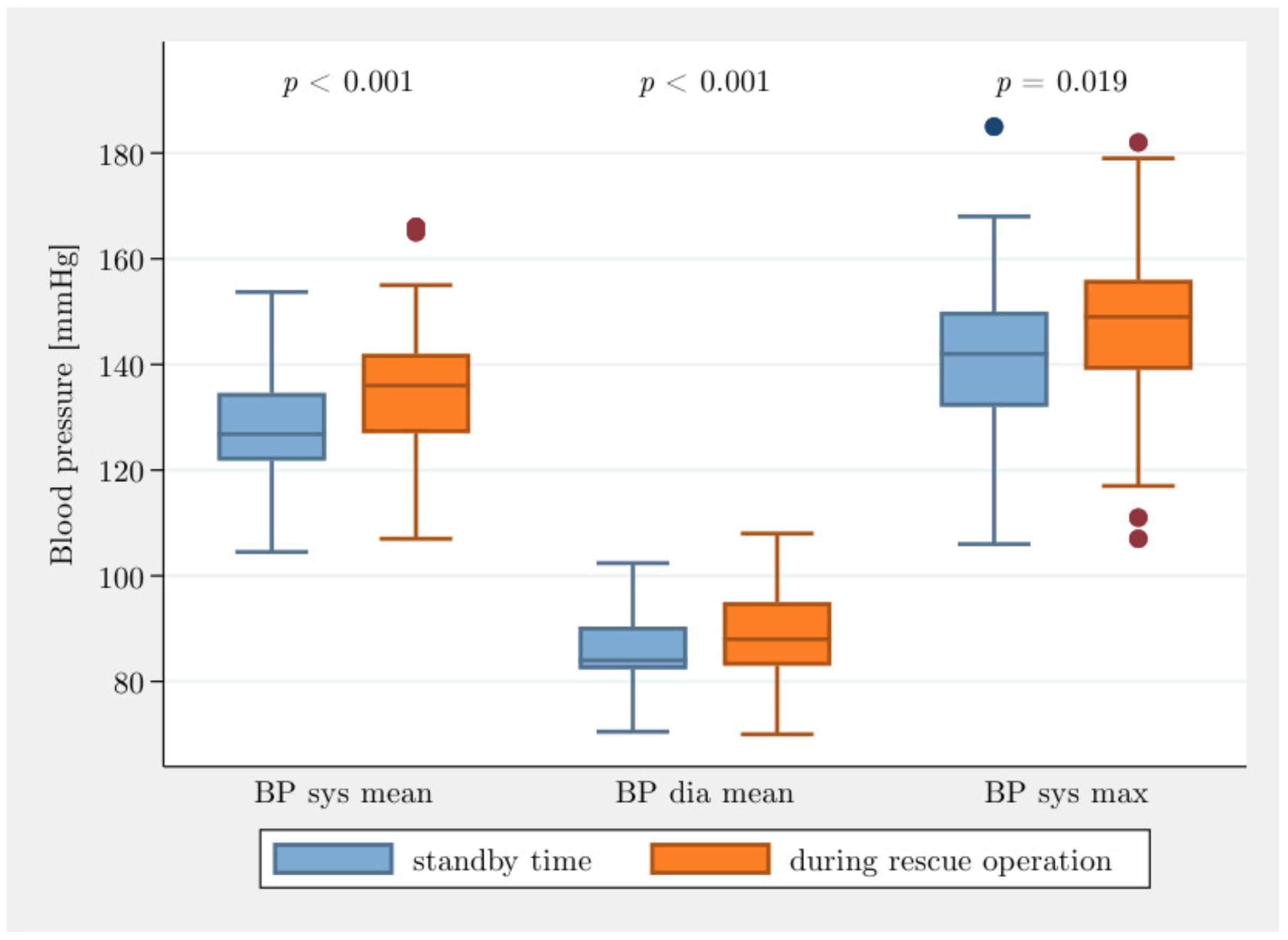
3.4. Blood Pressure
3.5. Holter (24 h) ECG
3.6. Cardiac Event Rates
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| ECG | Electrocardiography |
| ESC | European Society of Cardiology |
| HEMS | Helicopter emergency medical service |
| HR | Heart rate |
| HR max | Maximum heart rate |
| HR mean | Average heart rate |
| HR min | Minimal heart rate |
| BP | Blood pressure |
| BP dia max | Diastolic maximum blood pressure |
| BP dia mean | Diastolic average blood pressure |
| BP dia min | Diastolic minimum blood pressure |
| BP sys max | Systolic maximum blood pressure |
| BP sys mean | Systolic average blood pressure |
| BP sys min | Systolic minimum blood pressure |
| SVES | Supraventricular extrasystole |
| VES | Ventricular extrasystole |
References
- Hinkelbein, J.; Schwalbe, M.; Neuhaus, C.; Wetsch, W.A.; Genzwürker, H.V. Incidents, accidents and fatalities in 40 years of German helicopter emergency medical system operations. Eur. J. Anaesthesiol. 2011, 28, 766–773. [Google Scholar] [CrossRef]
- Leischik, R.; Foshag, P.; Strauß, M.; Littwitz, H.; Garg, P.; Dworrak, B.; Horlitz, M. Aerobic Capacity, Physical Activity and Metabolic Risk Factors in Firefighters Compared with Police Officers and Sedentary Clerks. PLoS ONE 2015, 10, e0133113. [Google Scholar]
- Yang, J.; Teehan, D.; Farioli, A.; Baur, D.M.; Smith, D.; Kales, S.N. Sudden cardiac death among firefighters ≤45 years of age in the United States. Am. J. Cardiol. 2013, 112, 1962–1967. [Google Scholar] [CrossRef]
- Thomas, S.H.; Arthur, A.O. Helicopter EMS: Research Endpoints and Potential Benefits. Emerg. Med. Int. 2011, 2012, 698562. [Google Scholar] [CrossRef][Green Version]
- Braun, J. Stellenwert der Luftrettung in der präklinischen Notfallversorgung in Deutschland. Notfall Rettungsmedizin. 2008, 11, 234. [Google Scholar] [CrossRef]
- Petrowski, K.; Herhaus, B.; Schöniger, C.; Frank, M.; Pyrc, J. Stress load of emergency service: Effects on the CAR and HRV of HEMS emergency physicians on different working days (N = 20). Nt. Arch. Occup. Environ. Health 2018, 92, 155–164. [Google Scholar] [CrossRef]
- Benzer, A.; Niebergall, H.; Posch, G.; Flora, G. Characteristics of the heart rate of emergency physicians in emergency helicopters. Anasthesiol. Intensivmed. Notf. Schmerzther. 1991, 26, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Carchietti, E.; Valent, F.; Cecchi, A.; Rammer, R. Influence of Stressors on HEMS Crewmembers in Flight. Air Med. J. 2011, 30, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome-a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [PubMed]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Meng, L.; Tsiaousis, G.; He, J.; Tse, G.; Antoniadis, A.P.; Korantzopoulos, P.; Letsas, K.P.; Baranchuk, A.; Qi, W.; Zhang, Z.; et al. Excessive Supraventricular Ectopic Activity and Adverse Cardiovascular Outcomes: A Systematic Review and Meta-analysis. Curr. Atheroscler. Rep. 2020, 22, 14. [Google Scholar] [CrossRef]
- Samel, A.; Vejvoda, M.; Maass, H. Sleep deficit and stress hormones in helicopter pilots on 7-day duty for emergency medical services. Aviat. Space Environ. Med. 2004, 75, 935–940. [Google Scholar]
- Strauß, M.; Karutz, H.; Foshag, P.; Spelsberg, N.; Dworrak, B.; Horlitz, M.; Leischik, R. Fit for rescue? Notfall + Rett. 2016, 19, 364–372. [Google Scholar] [CrossRef]
- Neuhauser, H.; Kuhnert, R.; Born, S. 12-Monats-Prävalenz von Bluthochdruck in Deutschland. J. Health Monit. 2017, 2, 57–63. [Google Scholar] [CrossRef]
- Soteriades, E.S.; Hauser, R.; Kawachi, I.; Liarokapis, D.; Christiani, D.C.; Kales, S.N. Obesity and cardiovascular disease risk factors in firefighters: A prospective cohort study. Obes. Res. 2005, 13, 1756–1763. [Google Scholar] [CrossRef] [PubMed]
- Geibe, J.R.; Holder, J.; Peeples, L.; Kinney, A.M.; Burress, J.W.; Kales, S.N. Predictors of on-duty coronary events in male firefighters in the United States. Am. J. Cardiol. 2008, 101, 585–589. [Google Scholar] [CrossRef]
- Kales, S.N.; Soteriades, E.S.; Christoudias, S.G.; Christiani, D.C. Firefighters and on-duty deaths from coronary heart disease: A case control study. Environ. Health 2003, 2, 14. [Google Scholar] [CrossRef]
- Kannel, W.B. Hypertension as a risk factor for cardiac events—Epidemiologic results of long-term studies. J. Cardiovasc. Pharmacol. 1993, 21 (Suppl. 2), S27–S37. [Google Scholar] [CrossRef]
- Reklaitiene, R.; Tamosiunas, A.; Virvičiūte, D.; Baceviciene, M.; Luksiene, D. Trends in prevalence, awareness, treatment, and control of hypertension, and the risk of mortality among middle-aged Lithuanian urban population in 1983–2009. BMC Cardiovasc. Disord. 2012, 12, 68. [Google Scholar] [CrossRef]
- Kales, S.N.; Tsismenakis, A.J.; Zhang, C.; Soteriades, E.S. Blood pressure in firefighters, police officers, and other emergency responders. Am. J. Hypertens. 2009, 22, 11–20. [Google Scholar] [CrossRef]
- Johnstone, M.T.; Mittleman, M.; Tofler, G.; Muller, J.E. The pathophysiology of the onset of morning cardiovascular events. Am. J. Hypertens. 1996, 9, 22s–28s. [Google Scholar] [CrossRef][Green Version]
- Adams, S.L.; Roxe, D.M.; Weiss, J.; Zhang, F.; Rosenthal, J.E. Ambulatory blood pressure and Holter monitoring of emergency physicians before, during, and after a night shift. Acad. Emerg. Med. 1998, 5, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Hennigan, J.K.; Wortham, A.W. Analysis of workday stresses on industrial managers using heart rate as a criterion. Ergonomics 1975, 18, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 2007, 25, 1105–1187. [Google Scholar] [CrossRef]
- Ho, J.E.; Larson, M.G.; Ghorbani, A.; Cheng, S.; Coglianese, E.E.; Vasan, R.S.; Wang, T.J. Long-term cardiovascular risks associated with an elevated heart rate: The Framingham Heart Study. J. Am. Heart Assoc. 2014, 3, e000668. [Google Scholar] [CrossRef]
- Lohman, E.B., 3rd; Petrofsky, J.S.; Maloney-Hinds, C.; Betts-Schwab, H.; Thorpe, D. The effect of whole body vibration on lower extremity skin blood flow in normal subjects. Med. Sci. Monit. 2007, 13, CR71–CR76. [Google Scholar]
- Bjerregaard, P. Premature beats in healthy subjects 40–79 years of age. Eur. Heart J. 1982, 3, 493–503. [Google Scholar] [CrossRef]
- Perez-Silva, A.; Luis Merino, J. Frequent ventricular extrasystoles: Significance, prognosis and treatment. ESC Coun. Cardiol. Pract. 2011, 9, 17. [Google Scholar]
- Gaita, F.; Giustetto, C.; Di Donna, P.; Richiardi, E.; Libero, L.; Brusin, M.C.; Molinari, G.; Trevi, G. Long-term follow-up of right ventricular monomorphic extrasystoles. J. Am. Coll. Cardiol. 2001, 38, 364–370. [Google Scholar] [CrossRef]
- Kennedy, H.L.; Whitlock, J.A.; Sprague, M.K.; Kennedy, L.J.; Buckingham, T.A.; Goldberg, R.J. Long-Term Follow-up of Asymptomatic Healthy Subjects with Frequent and Complex Ventricular Ectopy. N. Engl. J. Med. 1985, 312, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, H.L.; Underhill, S.J. Frequent or complex ventricular ectopy in apparently healthy subjects: A clinical study of 25 cases. Am. J. Cardiol. 1976, 38, 141–148. [Google Scholar] [CrossRef]
- Barutçu, A.; Gazi, E.; Temiz, A.; Bekler, A.; Altun, B.; Kırılmaz, B.; Kucuk, U. Assessment of left-atrial strain parameters in patients with frequent ventricular ectopic beats without structural heart disease. Int. J. Cardiovasc. Imaging 2014, 30, 1027–1036. [Google Scholar] [CrossRef]
- Niwano, S.; Wakisaka, Y.; Niwano, H.; Fukaya, H.; Kurokawa, S.; Kiryu, M.; Hatakeyama, Y.; Izumi, T. Prognostic significance of frequent premature ventricular contractions originating from the ventricular outflow tract in patients with normal left ventricular function. Heart 2009, 95, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Barutcu, A.; Bekler, A.; Temiz, A.; Kirilmaz, B.; Gazi, E.; Altun, B.; Ozdemir, S.; Aksu, F.U. Assessment of the effects of frequent ventricular extrasystoles on the left ventricle using speckle tracking echocardiography in apparently normal hearts. Anatol. J. Cardiol. 2015, 16, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Froelicher, V.F.; Thomas, M.M.; Pillow, C.; Lancaster, M.C. Epidemiologic study of asymptomatic men screened by maximal treadmill testing for latent coronary artery disease. Am. J. Cardiol. 1974, 34, 770–776. [Google Scholar] [CrossRef]
- Goldbarg, A.N.; Moran, J.F.; Childers, R.W.; Ricketts, H.T. Results and correlations of multistage exercise tests in a group of clinically normal business executives. Am. Heart J. 1970, 79, 194–200. [Google Scholar] [CrossRef]
- McHenry, P.L.; Morris, S.N.; Kavalier, M.; Jordan, J.W. Comparative study of exercise-induced ventricular arrhythmias in normal subjects and patients with documented coronary artery disease. Am. J. Cardiol. 1976, 37, 609–616. [Google Scholar] [CrossRef]
- Maurer, M.S.; Shefrin, E.A.; Fleg, J.L. Prevalence and prognostic significance of exercise-induced supraventricular tachycardia in apparently healthy volunteers. Am. J. Cardiol. 1995, 75, 788–792. [Google Scholar] [CrossRef]
- Morshedi-Meibodi, A.; Evans, J.; Levy, D.; Larson, M.; Vasan, R. Clinical correlates and prognostic significance of exercise-induced ventricular premature beats in the community. The Framingham Heart Study. ACC Curr. J. Rev. 2004, 13, 47. [Google Scholar] [CrossRef]
- Ouven, X.; Zureik, M.; Desnos, M.; Courbon, D.; Ducimetière, P. Long-Term Outcome in Asymptomatic Men with Exercise-Induced Premature Ventricular Depolarizations. N. Engl. J. Med. 2000, 343, 826–833. [Google Scholar]
- Smith, D.L.; Horn, G.P.; Fernhall, B.; Kesler, R.M.; Fent, K.W.; Kerber, S.; Rowland, T.W. Electrocardiographic Responses Following Live-Fire Firefighting Drills. J. Occup. Environ. Med. 2019, 61, 1030–1035. [Google Scholar] [CrossRef] [PubMed]
- Carey, M.G.; Thevenin, B.J. High-resolution 12-lead electrocardiograms of on-duty professional firefighters: A pilot feasibility study. J. Cardiovasc. Nurs. 2009, 24, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Al-Zaiti, S.S.; Carey, M.G. The Prevalence of Clinical and Electrocardiographic Risk Factors of Cardiovascular Death Among On-duty Professional Firefighters. J. Cardiovasc. Nurs. 2015, 30, 440–446. [Google Scholar] [CrossRef]
- Farioli, A.; Yang, J.; Teehan, D.; Baur, D.M.; Smith, D.L.; Kales, S.N. Duty-related risk of sudden cardiac death among young US firefighters. Occup. Med. 2014, 64, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Kales, S.N.; Soteriades, E.S.; Christophi, C.A.; Christiani, D.C. Emergency Duties and Deaths from Heart Disease among Firefighters in the United States. N. Engl. J. Med. 2007, 356, 1207–1215. [Google Scholar] [CrossRef]

| All Participants | Emergency Physicians | Paramedics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Median | n | Mean | SD | Median | n | Mean | SD | Median | |
| Age (years) | 21 | 40.6 | 7.7 | 38.0 | 11 | 37.0 | 3.0 | 36.0 | 10 | 44.6 | 9.35 | 44.0 |
| Height (m) | 21 | 1.83 | 0.08 | 1.83 | 11 | 1.82 | 0.09 | 1.82 | 10 | 1.83 | 0.07 | 1.83 |
| Weight (kg) | 21 | 83.0 | 9.9 | 84.0 | 11 | 81.9 | 10.4 | 82.5 | 10 | 84.2 | 9.7 | 84.2 |
| BMI | 21 | 24.8 | 2.1 | 25.1 | 11 | 24.6 | 2.6 | 24.9 | 10 | 24.9 | 1.5 | 25.2 |
| Waist circumference (cm) | 21 | 89.4 | 7.1 | 90.0 | 11 | 88.1 | 8.4 | 90.0 | 10 | 90.9 | 5.4 | 90.5 |
| Professional experience (years) | 21 | 7.0 | 7.9 | 4.0 | 11 | 2.9 | 2.4 | 3.0 | 10 | 11.4 | 9.4 | 8.0 |
| 10-year risk (%) (ESC score) | 21 | 0.6 | 1.3 | 0 | 11 | 0.3 | 0.5 | 0 | 10 | 1 | 1.7 | 0.5 |
| Description | Linear Regression ** | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Min–Max | Estimated Mean (95% CI) | p-Value | ||
| BP sys mean * | standby time | 127.6 | 11.4 | 126.8 | 104.5–153.7 | 128.0 (123.6; 132.4) | |
| n = 45 | rescue operation | 135.0 | 13.6 | 136.0 | 107.0–166.0 | 135.6 (130.1; 141.1) | |
| difference | 7.4 | 9.0 | 7.2 | −16.0 to 31.0 | 7.4 (5.1; 9.7) | <0.001 | |
| BP dia mean * | standby time | 85.3 | 7.3 | 84.0 | 70.5–102.4 | 85.2 (82.4; 88.0) | |
| n = 45 | rescue operation | 88.7 | 9.1 | 88.0 | 70.0–108.0 | 89.1 (85.5; 92.9) | |
| difference | 3.4 | 6.0 | 3.5 | −12.0 to 20.0 | 3.6 (1.8; 5.5) | <0.001 | |
| BP sys min * | standby time | 114.7 | 12.6 | 114.0 | 84.0–143.0 | 114.6 (109.7; 119.4) | |
| n = 41 | emergency operation | 124.7 | 13.0 | 125.0 | 102.0–152.0 | 125.2 (119.5; 103.8) | |
| difference | 10.0 | 8.9 | 9.0 | −8.0 to 28.0 | 10.1 (7.0; 13.3) | <0.001 | |
| BP dia min * | standby time | 76.4 | 8.7 | 77.0 | 50.0–94.0 | 76.4 (73.0; 79.8) | |
| n = 41 | rescue operation | 82.8 | 9.5 | 84.0 | 63.0–104.0 | 83.1 (78.8; 87.5) | |
| difference | 6.4 | 7.0 | 7.0 | −7.0 to 24.0 | 6.7 (3.8; 9.5) | <0.001 | |
| BP sys max * | standby time | 141.8 | 15.5 | 142.0 | 106.0–185.0 | 142.4 (136.5; 148.4) | |
| n = 41 | rescue operation | 147.4 | 17.3 | 149.0 | 107.0–182.0 | 147.7 (141.9; 153.5) | |
| difference | 5.6 | 16.5 | 6.0 | −42.0 to 48.0 | 5.6 (0.9; 10.3) | 0.019 | |
| BP dia min * | standby time | 95.7 | 10.5 | 94.0 | 78.0–124.0 | 95.8 (91.9; 99.7) | |
| n = 41 | rescue operation | 95.6 | 11.2 | 95.0 | 70.0–117.0 | 96.0 (91.6; 100.4) | |
| difference | −0.1 | 11.4 | 2.0 | −45.0 to 25.0 | 0.0 (−3.9; 3.9) | 1.000 | |
| Description: | Linear Regression ** | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Min–Max | Estimated Mean (95% CI) | p-Value | ||
| HR mean * | standby time | 78.1 | 13.2 | 78.8 | 56.4–115.0 | 76.3 (71.3; 81.6) | |
| n = 48 | rescue operation | 91.1 | 14.8 | 92.0 | 60.0–126.0 | 89.5 (83.8; 95.1) | |
| difference | 13.0 | 9.4 | 12.3 | −11.0 to 37.5 | 13.0 (10.8; 15.3) | <0.001 | |
| HR min * | standby time | 67.9 | 12.7 | 68.0 | 44.0–100.0 | 67.3 (61.9; 72.6) | |
| n = 44 | rescue operation | 75.1 | 14.1 | 74.0 | 49.0–111.0 | 74.6 (69.2; 80.0) | |
| difference | 7.2 | 9.1 | 6.0 | −9.0 to 33.0 | 7.2 (5.1; 9.4) | <0.001 | |
| HR max * | standby time | 90.0 | 15.4 | 89.5 | 56.0–128.0 | 89.8 (84.5; 95.1) | |
| n = 44 | rescue operation | 123.7 | 21.0 | 127.0 | 83.0–165.0 | 122.9 (115.1; 130.8) | |
| difference | 33.7 | 20.5 | 36.0 | −18 to 70.0 | 33.5 (26.2; 40.8) | <0.001 | |
| Time (Hours) | Cardiac Events | Event Rate Per Hour | 95% CI * | p-Value ** | |
|---|---|---|---|---|---|
| Standby time | 227.8 | 2514 | 11.0 | 10.6–11.5 | |
| Rescue operation | 46.0 | 770 | 16.7 | 15.6–18.0 | 0.020 |
| Total | 273.8 | 3284 | 12.0 | 11.6–12.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strauss, M.; Dahmen, J.; Hutter, S.; Brade, M.; Leischik, R. Rescue Operations Lead to Increased Cardiovascular Stress in HEMS Crew Members: A Prospective Pilot Study of a German HEMS Cohort. J. Clin. Med. 2021, 10, 1602. https://doi.org/10.3390/jcm10081602
Strauss M, Dahmen J, Hutter S, Brade M, Leischik R. Rescue Operations Lead to Increased Cardiovascular Stress in HEMS Crew Members: A Prospective Pilot Study of a German HEMS Cohort. Journal of Clinical Medicine. 2021; 10(8):1602. https://doi.org/10.3390/jcm10081602
Chicago/Turabian StyleStrauss, Markus, Janosch Dahmen, Sophia Hutter, Marko Brade, and Roman Leischik. 2021. "Rescue Operations Lead to Increased Cardiovascular Stress in HEMS Crew Members: A Prospective Pilot Study of a German HEMS Cohort" Journal of Clinical Medicine 10, no. 8: 1602. https://doi.org/10.3390/jcm10081602
APA StyleStrauss, M., Dahmen, J., Hutter, S., Brade, M., & Leischik, R. (2021). Rescue Operations Lead to Increased Cardiovascular Stress in HEMS Crew Members: A Prospective Pilot Study of a German HEMS Cohort. Journal of Clinical Medicine, 10(8), 1602. https://doi.org/10.3390/jcm10081602






