Quality of Life in Presbyopes with Low and High Myopia Using Single-Vision and Progressive-Lens Correction
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Examinations
2.3. Questionnaires
2.4. Statistical Analysis
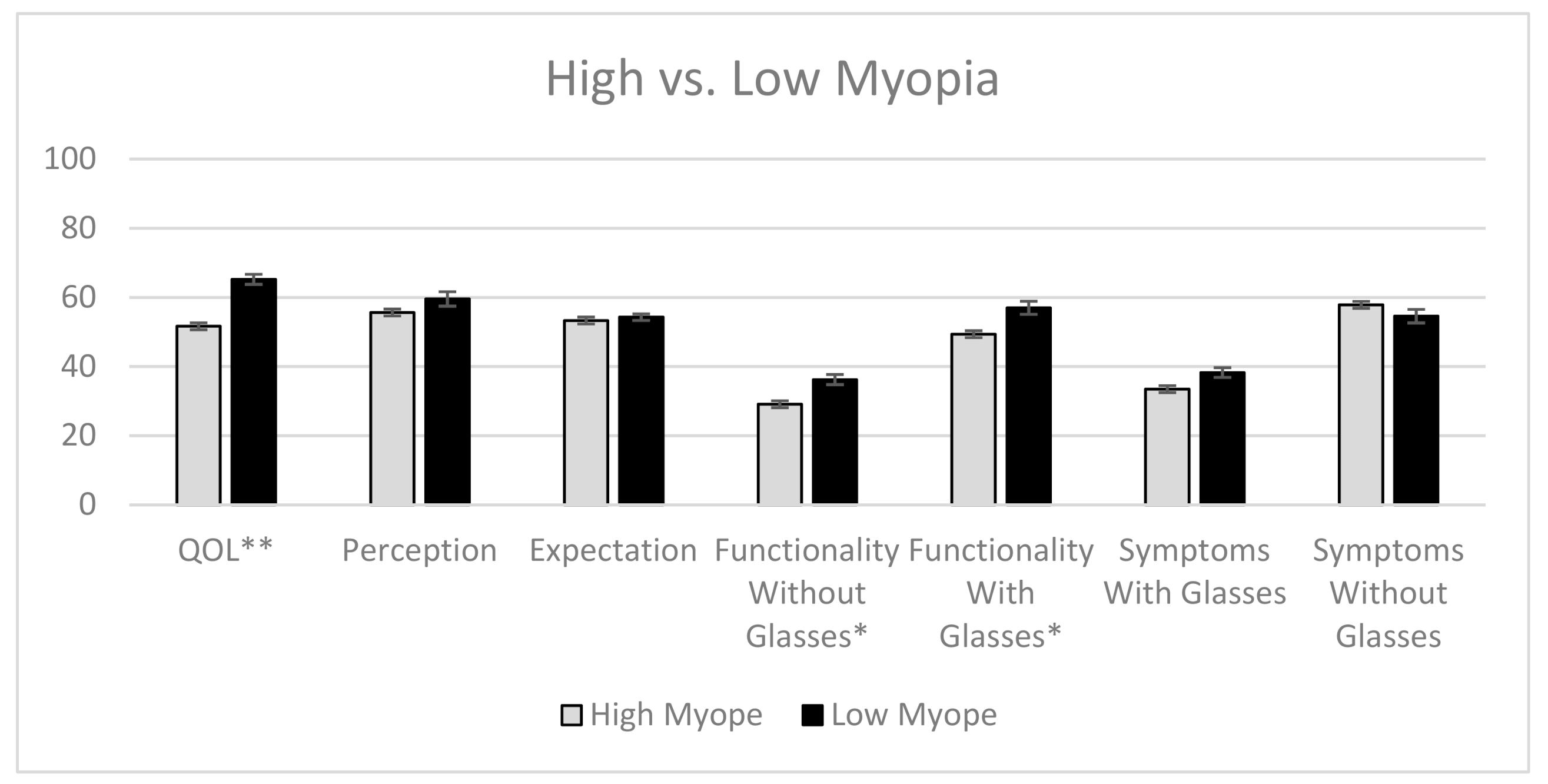
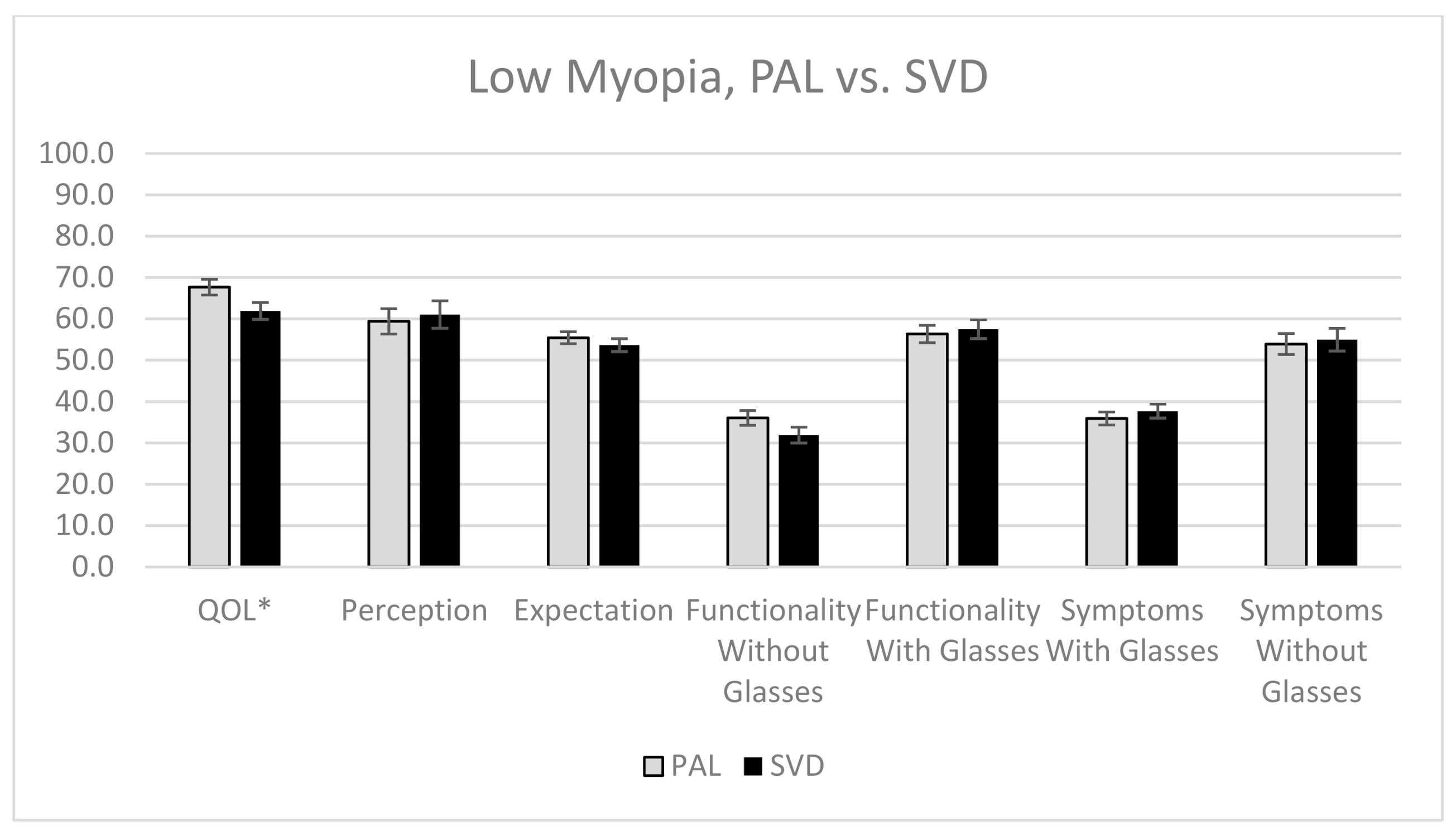
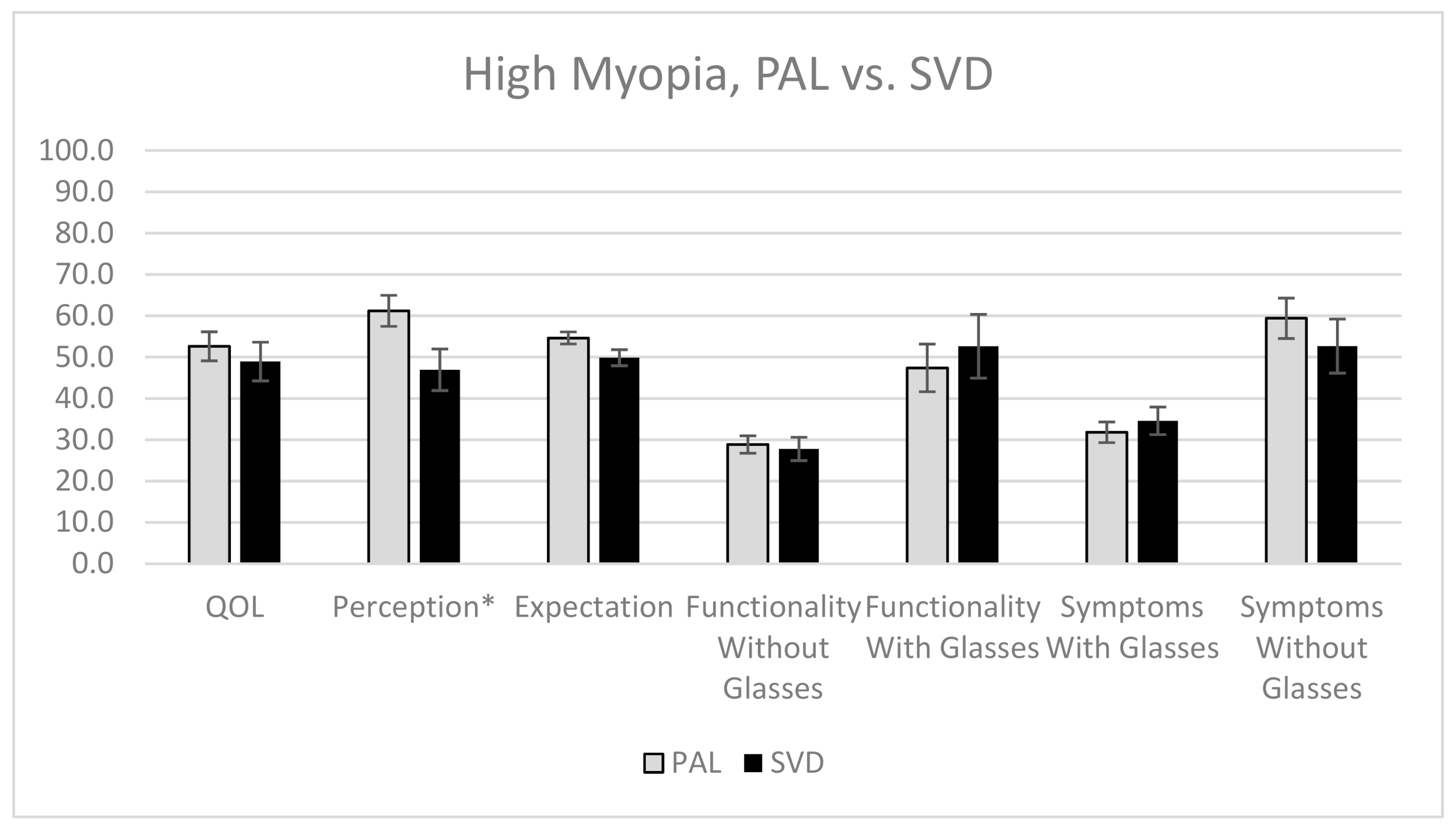
3. Results
4. Discussion
4.1. Significant Findings
4.2. Strengths and Limitations of the Study
4.3. Suggestions for Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Population Prospects—Population Division. United Nations. 2020. Available online: https://population.un.org/wpp/ (accessed on 15 January 2020).
- Holden, B.A.; Fricke, T.R.; Ho, S.M.; Wong, R.; Schlenther, G.; Cronje, S.; Burnett, A.; Papas, E.; Naidoo, K.S.; Frick, K.D. Global vision impairment due to uncorrected presbyopia. Arch. Ophthalmol. 2008, 126, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.; Fricke, T. Global Prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Fricke, T.R.; Tahhan, N.; Resnikoff, S.; Papas, E.; Burnett, A.; Ho, S.M.; Naduvilath, T.; Naidoo, K.S. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmology 2018, 125, 1492–1499. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Congdon, N. Quality of life and near vision impairment due to functional presbyopia among rural Chinese adults. Investig. Opthal. Vis. Sci. 2011, 52, 4118–4123. [Google Scholar] [CrossRef]
- Muhammad, N.; Alhassan, M. Visual function and vision-related quality of life in a presbyopic adult population of Northwestern Nigeria. Niger Med. J. 2015, 56, 317–322. [Google Scholar] [CrossRef]
- McDonnell, P.J.; Lee, P.; Spritzer, K.; Lindblad, A.S.; Hays, R.D. Associations of presbyopia with vision-targeted health-related quality of life. Arch. Ophthalmol. 2003, 121, 1577–1581. [Google Scholar] [CrossRef]
- Kumaran, S.; Balasubramaniam, S. Refractive error and vision-related quality of life in South Indian children. Optom. Vis. Sci. 2015, 92, 272–278. [Google Scholar] [CrossRef]
- Rose, K.; Harper, R.; Tromans, C.; Waterman, C.; Goldberg, D.; Haggerty, C.; Tullo, A. Quality of life in myopia. Br. J. Ophthalmol. 2000, 84, 1031–1034. [Google Scholar] [CrossRef]
- Black, N. Patient reported outcome measures could help transform healthcare. Br. Med. J. 2013, 346, f167. [Google Scholar] [CrossRef]
- Elliott, D.; Pesudovs, K. Vision-related quality of life. Optom. Vis. Sci. 2007, 84, 656–658. [Google Scholar] [CrossRef]
- Vitale, S. The Refractive Status and Vision Profile A Questionnaire to Measure Vision-Related Quality of Life in Persons with Refractive Error. Ophthalmology 2000, 107, 1529–1539. [Google Scholar] [CrossRef]
- Nichols, J.J. Reliability and Validity of Refractive Error–Specific Quality-of-Life Instruments. Arch. Ophthalmol. 2003, 121, 1289. [Google Scholar] [CrossRef]
- Khadka, J.; McAlinden, C.; Pesudovs, K. Quality Assessment of Ophthalmic Questionnaires. Optom. Vis. Sci. 2013, 90, 720–744. [Google Scholar] [CrossRef]
- Wu, X.Y.; Ohinmaa, A.; Johnson, J.A.; Veugelers, P.J. Assessment of Children’s Own Health Status Using Visual Analogue Scale and Descriptive System of the EQ-5D-Y: Linkage between Two Systems. Qual. Life Res. 2013, 23, 393–402. [Google Scholar] [CrossRef]
- Andrich, D. A rating formulation for ordered response categories. Psychometrika 1978, 43, 561–573. [Google Scholar] [CrossRef]
- Linacre, J.M. Winsteps Rasch Measurement Computer Program; Winsteps: Chicago, IL, USA, 2006. [Google Scholar]
- Lamoureux, E.L.; Wang, J.; Aung, T.; Saw, S.M.; Wong, T.Y. Myopia and quality of life: The Singapore Malay Eye Study (SiMES). Investig. Ophthalmol. Vis. Sci. 2008, 49, 4469. [Google Scholar]
- Collins, J.W.; Carney, L.G. Visual performance in high myopia. Curr. Eye Res. 1990, 9, 217–223. [Google Scholar] [CrossRef]
- Cheng, X.U.; Bradley, A.; Hong, X.; Thibos, L.N. Relationship between refractive error and monochromatic aberrations of the eye. Optom. Vis. Sci. 2003, 80, 43–49. [Google Scholar] [CrossRef]
- Paquin, M.P.; Hamam, H.; Simonet, P. Objective measurement of optical aberrations in myopic eyes. Optom. Vis. Sci. 2002, 79, 285–291. [Google Scholar] [CrossRef]
- Atchison, D.A.; Pritchard, N.; Schmid, K.L. Peripheral refraction along the horizontal and vertical visual fields in myopia. Vis. Res. 2006, 46, 1450–1458. [Google Scholar] [CrossRef]
- Chen, P.C.; Woung, L.C.; Yang, C.F. Modulation transfer function and critical flicker frequency in high-myopia patients. J. Formos Med. Assoc. 2000, 99, 45–48. [Google Scholar] [PubMed]
- Kawabata, H.; Adachi-Usami, E. Multifocal electroretinogram in myopia. Investig. Ophthalmol. Vis. Sci. 1997, 38, 2844–2851. [Google Scholar]
- Westall, C.A.; Dhaliwal, H.S.; Panton, C.M.; Sigesmun, D.; Levin, A.V.; Nischal, K.K.; Héon, E. Values of electroretinogram responses according to axial length. Doc Ophthalmol. 2001, 102, 115–130. [Google Scholar] [CrossRef] [PubMed]
- Mashige, K. Night vision and glare vision thresholds and recovery time in myopic and hyperopic eyes. Afr. Vis. Eye Health 2010, 69, a136. [Google Scholar] [CrossRef]
- Jaworski, A.; Gentle, A.; Zele, A.J.; Vingrys, A.J.; McBrien, N.A. Altered visual sensitivity in axial high myopia: A local postreceptoral phenomenon? Investig. Ophthalmol. Vis. Sci. 2006, 47, 3695–3702. [Google Scholar] [CrossRef]
- Kandel, H.; Khadka, J.; Goggin, M.; Pesudovs, K. Impact of refractive error on quality of life: A qualitative study. Clin. Exp. Ophthalmol. 2017, 45, 677–688. [Google Scholar] [CrossRef]
- Smith, T.S.; Katz, J.; Khatry, S.; Le Clerk, S.; Patel, I.; Hyon, B.; Tielsch, J. The impact of uncorrected presbyopia on performance in tasks of daily living and vision-related quality of life in rural Nepal. Investig. Ophthalmol. Vis. Sci. 2009, 50, 3966. [Google Scholar]
- Sivardeen, A.; McAlinden, C.; Wolffsohn, J.S. Presbyopic correction use and its impact on quality of vision symptoms. J. Optom. 2020, 13, 29–34. [Google Scholar] [CrossRef]
- Chu, B.S.; Wood, J.M.; Collins, M.J. Effect of presbyopic vision corrections on perceptions of driving difficulty. Eye Contact Lens 2009, 35, 133–143. [Google Scholar] [CrossRef]
- Chu, B.S.; Wood, J.M.; Collins, M.J. The effect of presbyopic vision corrections on nighttime driving performance. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4861–4866. [Google Scholar] [CrossRef]
- Pesudovs, K.; Garamendi, E.; Elliott, D.B. The contact lens impact on quality of life (CLIQ) questionnaire: Development and validation. Investig. Ophthalmol. Vis. Sci. 2006, 47, 2789–2796. [Google Scholar] [CrossRef]
- Kandel, H.; Khadka, J.; Lundström, M.; Goggin, M.; Pesudovs, K. Questionnaires for Measuring Refractive Surgery Outcomes. J. Refract Surg. 2017, 33, 416–424. [Google Scholar] [CrossRef]
- Kandel, H.; Khadka, J.; Goggin, M.; Pesudovs, K. Patient-reported Outcomes for Assessment of Quality of Life in Refractive Error: A Systematic Review. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2017, 94, 1102–1119. [Google Scholar] [CrossRef]
- Garamendi, E.; Pesudovs, K.; Stevens, M.J.; Elliott, D.B. The Refractive Status and Vision Profile: Evaluation of psychometric properties and comparison of Rasch and summated Likert-scaling. Vis. Res. 2006, 46, 1375–1383. [Google Scholar] [CrossRef]
| Questions | Scale |
|---|---|
Perception
|
|
Expectation
|
|
Functionality (With and without correction)
|
|
Visual Symptoms (With and without correction)
| |
| The current state of healthYour own health state today | 0 (worst imaginable health state) to 100 (best imaginable health state) using a visual analogue scale |
| Low Myopia (n = 108) | High Myopia (n = 41) | p-Value | |
|---|---|---|---|
| Mean age (years) | 51.8 ± 6.6 | 52.8 ± 7.7 | 0.43 |
| Gender, n (%) | |||
| Female | 70 (64.8%) | 19 (46.3%) | 0.04 * |
| Male | 38 (35.2%) | 22 (53.7%) | |
| Mean spherical equivalent, diopters | −3.1 ± 1.7 | −5.6 ± 2.4 | <0.001 * |
| Type of glasses, n (%) | |||
| PAL | 55 (50.9%) | 25 (61.0%) | 0.40 |
| SVD | 47 (43.5%) | 14 (34.1%) | 0.50 |
| Others | 6 (5.6%) | 2 (4.9%) | - |
| Mean distance visual acuity, LogMAR | −0.09 ± 0.09 | −0.04 ± 0.09 | 0.003 * |
| Mean near visual acuity, LogMAR | 0.25 ± 0.20 | 0.25 ± 0.14 | 0.57 |
| Mean log contrast sensitivity | 1.94 ± 0.02 | 1.94 ± 0.03 | 0.22 |
| Current health (VAS) | 77.48 ± 1.50 | 73.07 ± 2.42 | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, A.; Lim, S.Y.; Wong, Y.L.; Yeo, A.; Rajeev, N.; Drobe, B. Quality of Life in Presbyopes with Low and High Myopia Using Single-Vision and Progressive-Lens Correction. J. Clin. Med. 2021, 10, 1589. https://doi.org/10.3390/jcm10081589
Yang A, Lim SY, Wong YL, Yeo A, Rajeev N, Drobe B. Quality of Life in Presbyopes with Low and High Myopia Using Single-Vision and Progressive-Lens Correction. Journal of Clinical Medicine. 2021; 10(8):1589. https://doi.org/10.3390/jcm10081589
Chicago/Turabian StyleYang, Adeline, Si Ying Lim, Yee Ling Wong, Anna Yeo, Narayanan Rajeev, and Björn Drobe. 2021. "Quality of Life in Presbyopes with Low and High Myopia Using Single-Vision and Progressive-Lens Correction" Journal of Clinical Medicine 10, no. 8: 1589. https://doi.org/10.3390/jcm10081589
APA StyleYang, A., Lim, S. Y., Wong, Y. L., Yeo, A., Rajeev, N., & Drobe, B. (2021). Quality of Life in Presbyopes with Low and High Myopia Using Single-Vision and Progressive-Lens Correction. Journal of Clinical Medicine, 10(8), 1589. https://doi.org/10.3390/jcm10081589






