Headache Is Associated with Low Systolic Blood Pressure and Psychosocial Problems in German Adolescents: Results from the Population-Based German KiGGS Study
Abstract
1. Introduction
2. Methods
2.1. Study Population and Data Collection
2.2. Clinical Assessments
2.3. Laboratory Measurements
2.4. Psychometric Assessment
2.5. Statistical Analysis
3. Results
3.1. Characterization of the Total Study Population
3.2. KINDL-R and SDQ as Predictors for Headache
3.3. Quality of Life and Distress Mediate the Effect of Blood Pressure on Headache
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kernick, D.; Reinhold, D. Children and adolescents with headache: What do they need? J. Headache Pain 2008, 9, 233–236. [Google Scholar] [CrossRef]
- Kelly, M.; Strelzik, J.; Langdon, R.; DiSabella, M. Pediatric headache: Overview. Curr. Opin. Pediatr. 2018, 30, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, E.; Aliprandi, A. Migraine and hypertension. Neurol. Sci. 2008, 29 (Suppl. 1), S37–S39. [Google Scholar] [CrossRef] [PubMed]
- Markush, R.E.; Karp, H.R.; Heyman, A.; O’Fallon, W.M. Epidemiologic study of migraine symptoms in young women. Neurology 1975, 25, 430–435. [Google Scholar] [CrossRef]
- Cirillo, M.; Stellato, D.; Lombardi, C.; De Santo, N.G.; Covelli, V. Headache and cardiovascular risk factors: Positive association with hypertension. Headache 1999, 39, 409–416. [Google Scholar] [CrossRef]
- Yang, W.C.; Wu, H.P. Clinical analysis of hypertension in children admitted to the emergency department. Pediatr. Neonatol. 2010, 51, 44–51. [Google Scholar] [CrossRef][Green Version]
- Yang, W.C.; Lin, M.J.; Chen, C.Y.; Wu, H.P. Clinical overview of hypertensive crisis in children. World J. Clin. Cases 2015, 3, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Waters, W.E. Headache and blood pressure in the community. Br. Med. J. 1971, 16, 142–143. [Google Scholar] [CrossRef][Green Version]
- Schéle, R.; Ahlborg, B.; Ekbom, K. Physical characteristics and allergic history in young men with migraine and other headaches. Headache 1978, 18, 80–86. [Google Scholar] [CrossRef]
- Ho, K.H.; Ong, B.K.C. Perceived headache associations in Singapore: Results of a randomized national survey. Headache 2001, 41, 164–170. [Google Scholar] [CrossRef]
- Hagen, K.; Stovner, L.J.; Vatten, L.; Holmen, J.; Zwart, J.A.; Bovim, G. Blood pressure and risk of headache: A prospective study of 22,685 adults in Norway. J. Neurol. Neurosurg. Psychiatry 2002, 72, 463–466. [Google Scholar]
- Tronvik, E.; Zwart, J.A.; Hagen, K.; Dyb, G.; Holmen, T.L.; Stovner, L.J. Association between blood pressure measures and recurrent headache in adolescents: Cross-sectional data from the HUNT-Youth study. J. Headache Pain 2011, 12, 347–357. [Google Scholar] [CrossRef][Green Version]
- Berendes, A.; Meyer, T.; Hulpke-Wette, M.; Herrmann-Lingen, C. Association of elevated blood pressure with low distress and good quality of life: Results from the nationwide representative German Health Interview and Examination Survey for Children and Adolescents. Psychosom. Med. 2013, 75, 422–428. [Google Scholar] [CrossRef]
- Kurth, B.M.; Kamtsiuris, P.; Hölling, H.; Schlaud, M.; Dölle, R.; Ellert, U.; Kahl, H.; Knopf, H.; Lange, M.; Mensink, G.B.M.; et al. The challenge of comprehensively mapping children’s health in a nation-wide health survey: Design of the German KiGGS-Study. BMC Public Health 2008, 8, 196. [Google Scholar] [CrossRef] [PubMed]
- Kamtsiuris, P.; Lange, M.; Schaffrath Rosario, A. The German Health Interview and Examination Survey for Children and Adolescents (KiGGS): Sample design, response and nonresponse analysis. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Hölling, H.; Kurth, B.M.; Rothenberger, A.; Becker, A.; Schlack, R. Assessing psychopathological problems of children and adolescents from 3 to 17 years in a nationwide representative sample: Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Eur. Child Adolesc. Psychiatry 2008, 17, S34–S41. [Google Scholar] [CrossRef]
- Rattay, P.; von der Lippe, E.; Mauz, E.; Richter, F.; Hölling, H.; Lange, C.; Lampert, T. Heath and health risk behaviour of adolescents - Differences according to family structure. Results of the German KiGGS cohort study. PLoS ONE 2018, 13, e0192968. [Google Scholar] [CrossRef]
- Krause, L.; Mauz, E. Headache, abdominal pain, and back pain in children and adolescents in Thuringia: Representative results of a regional module study in KiGGS wave 1. Schmerz 2018, 32, 105–114. [Google Scholar] [CrossRef]
- Neuhauser, H.; Thamm, M. Blood pressure measurement in the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Methodology and initial results. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Thierfelder, W.; Dortschy, R.; Hintzpeter, B.; Kahl, H.; Scheidt-Nave, C. Biochemical measures in the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 757–770. [Google Scholar] [CrossRef]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child. Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.; Ford, T.; Simmons, H.; Gatward, R.; Meltzer, H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br. J. Psychiatry 2000, 177, 534–539. [Google Scholar] [CrossRef]
- Janitza, S.; Klipker, K.; Hölling, H. Age-specific norms and validation of the German SDQ parent version based on a nationally representative sample (KiGGS). Eur. Child Adolesc. Psychiatry 2020, 29, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Ellert, U.; Erhart, M. Health-related quality of life of children and adolescents in Germany. Norm data from the German Health Interview and Examination Survey (KiGGS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Ellert, U.; Ravens-Sieberer, U.; Erhart, M.; Kurth, B.M. Determinants of agreement between self-reported and parent-assessed quality of life for children in Germany - results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Heath Qual. Life Outcomes 2011, 9, 102. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
- Ottaviani, C.; Fagioli, S.; Mattei, E.; Censi, F.; Edwards, L.; Macaluso, E.; Bozzali, M.; Critchley, H.D.; Calcagnini, G. Brain-heart pathways to blood pressure-related hypoalgesia. Psychosom. Med. 2018, 80, 845–852. [Google Scholar] [CrossRef]
- Guasti, L.; Zanotta, D.; Mainardi, L.T.; Petrozzino, M.R.; Grimoldi, P.; Garganico, D.; Diolisi, A.; Gaudio, G.; Klersy, C.; Grandi, A.M.; et al. Hypertension-related hypoalgesia, autonomic function and spontaneous baroreflex sensitivity. Auton. Neurosci. 2002, 99, 127–133. [Google Scholar] [CrossRef]
- Ghione, S. Hypertension-associated hypalgesia. Evidence in experimental animals and humans, pathophysiological mechanisms, and potential clinical consequences. Hypertension 1996, 28, 494–504. [Google Scholar] [CrossRef]
- Hildrum, B.; Mykletun, A.; Stordal, E.; Bjelland, I.; Dahl, A.A.; Holmen, J. Association of low blood pressure with anxiety and depression: The Nord-Trøndelag Health Study. J. Epidemiol. Community Health 2007, 61, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Joung, K.I.; Cho, S.I. Association of low blood pressure with suicidal ideation: A cross-sectional study of 10,708 adults with normal or low blood pressure in Korea. BMC Public Health 2018, 18, 200. [Google Scholar] [CrossRef] [PubMed]
- Pilgrim, J.A.; Stansfeld, S.; Marmot, M. Low blood pressure, low mood? BMJ 1992, 304, 75–78. [Google Scholar] [CrossRef]
- Meyer, T.; Becker, A.; Sundermann, J.; Rothenberger, A.; Herrmann-Lingen, C. Attention deficit-hyperactivity disorder is associated with reduced blood pressure and serum vitamin D levels: Results from the nationwide German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Eur. Child Adolesc. Psychiatry 2017, 26, 165–175. [Google Scholar] [CrossRef]
- Gallai, V.; Sarchielli, P.; Coata, G.; Firenze, C.; Morucci, P.; Abbritti, G. Serum and salivary magnesium levels in migraine. Results in a group of juvenile patients. Headache 1992, 32, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Soriani, S.; Arnaldi, C.; De Carlo, L.; Arcudi, D.; Mazzotta, D.; Battistella, P.A.; Sartori, S.; Abbasciano, V. Serum and red blood cell magnesium levels in juvenile migraine patients. Headache 1995, 35, 14–16. [Google Scholar] [CrossRef]
- Allais, G.; Gabellari, I.C.; Airola, G.; Borgogno, P.; Schiapparelli, P.; Benedetto, C. Headache induced by the use of combined oral contraceptives. Neurol. Sci. 2009, 30 (Suppl. 1), S15–S17. [Google Scholar] [CrossRef]
- Sacco, S.; Merki-Feld, G.S.; Ægidius, K.L.; Bitzer, J.; Canonico, M.; Gantenbein, A.R.; Kurth, T.; Lampl, C.; Lidegaard, Ø.; MacGregor, E.A.; et al. Effect of exogenous estrogens and progestogens on the course of migraine during reproductive age: A consensus statement by the European Headache Federation (EHF) and the European Society of Contraception and Reproductive Health (ESCRH). J. Headache Pain 2018, 19, 76. [Google Scholar] [CrossRef]
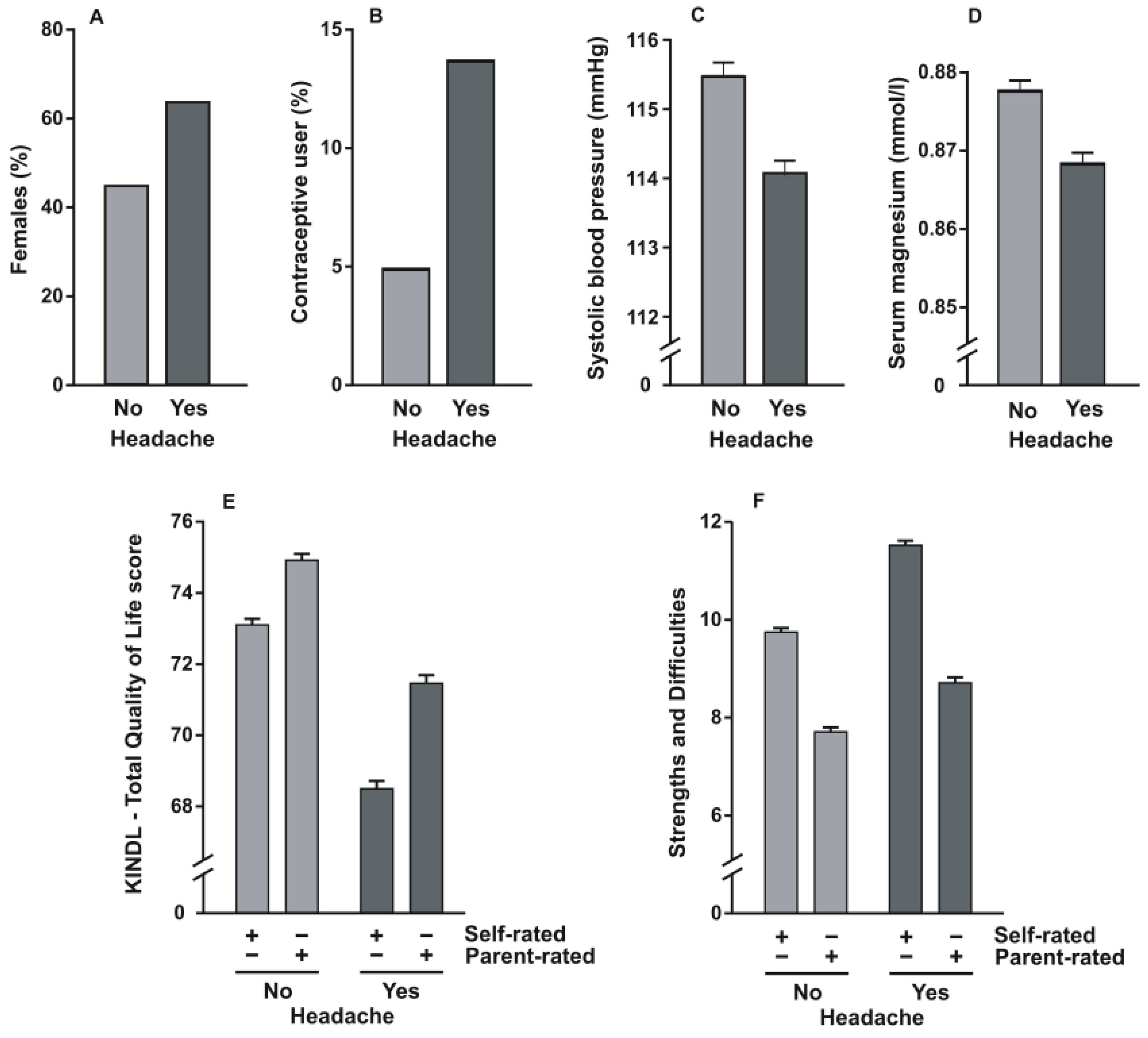
| Total Study Cohort (n = 5221) | Cohort with Headache (n = 2238) | Cohort without Headache (n = 2983) | p Value | |
|---|---|---|---|---|
| Age | 14.9 ± 2.0 | 15.0 ± 1.9 | 14.7 ± 2.0 | <0.001 |
| Sex (males, %) | 47.1 | 36.3 | 55.1 | <0.001 |
| Migrants (%) | 17.4 | 17.3 | 17.5 | 0.794 |
| Body mass index (kg/m2) | 21.3 ± 4.1 | 21.7 ± 4.4 | 21.0 ± 3.8 | <0.001 |
| Contraceptive use (%) | 8.7 | 13.7 | 4.9 | <0.001 |
| Socioeconomic status (%) | Low: 27.3 Middle: 47.8 High: 25.0 | Low: 26.0 Middle: 49.0 High: 25.1 | Low: 28.3 Middle: 47.0 High: 24.8 | 0.157 |
| Systolic blood pressure (mmHg) | 114.9 ± 10.7 | 114.0 ± 10.2 | 115.5 ± 11.0 | <0.001 |
| Magnesium (mmol/L) | 0.87 ± 0.07 | 0.86 ± 0.06 | 0.87 ± 0.07 | <0.001 |
| Self-rated KINDL | 70.8 ± 10.1 | 68.5 ± 10.5 | 73.1 ± 9.7 | <0.001 |
| Parent-rated KINDL | 73.1 ± 10.2 | 71.5 ± 10.5 | 75.0 ± 9.9 | <0.001 |
| Self-rated SDQ score | 10.7 ± 4.4 | 11.5 ± 4.6 | 9.8 ± 4.4 | <0.001 |
| Parent-rated SDQ score | 8.2 ± 5.1 | 8.7 ± 5.3 | 7.7 ± 5.0 | <0.001 |
| Model 1: self-rated KINDL (R2 = 0.088; p < 0.001) | Model 2: parent-rated KINDL (R2 = 0.077; p < 0.001) | |||||
| Variable | Exp(B) | 95% CI | P value | Exp(B) | 95% CI | P value |
| Sex | 0.619 | 0.546–0.702 | <0.001 | 0.569 | 0.502–0.646 | <0.001 |
| Age | 1.027 | 0.993–1.063 | 0.125 | 1.040 | 1.005–1.076 | 0.025 |
| Body mass index (kg/m2) | 1.032 | 1.016–1.048 | <0.001 | 1.034 | 1.018–1.051 | <0.001 |
| Contraceptive user (%) | 2.083 | 1.650–2.629 | <0.001 | 2.000 | 1.588–2.520 | <0.001 |
| Blood pressure (mmHg) | 0.985 | 0.979–0.991 | <0.001 | 0.985 | 0.979–0.991 | <0.001 |
| Magnesium (mmol/L) | 0.410 | 0.176–0.956 | 0.039 | 0.376 | 0.162–0.873 | 0.023 |
| Self-/parent-rated KINDL | 0.961 | 0.955–0.967 | <0.001 | 0.969 | 0.963–0.975 | <0.001 |
| Model 3: self-rated SDQ (R2 = 0.081; p < 0.001) | Model 4: parent-rated SDQ (R2 = 0.067; p < 0.001) | |||||
| Variable | Exp(B) | 95% CI | P value | Exp(B) | 95% CI | P value |
| Sex | 0.584 | 0.516–0.660 | <0.001 | 0.524 | 0.462–0.595 | <0.001 |
| Age | 1.057 | 1.022–1.093 | 0.001 | 1.065 | 1.029–1.102 | <0.001 |
| Body mass index (kg/m2) | 1.030 | 1.014–1.047 | <0.001 | 1.031 | 1.015–1.048 | <0.001 |
| Contraceptive user (%) | 1.965 | 1.563–2.470 | <0.001 | 1.960 | 1.559–2.463 | <0.001 |
| Blood pressure (mmHg) | 0.987 | 0.981–0.993 | <0.001 | 0.986 | 0.980–0.992 | <0.001 |
| Magnesium (mmol/L) | 0.515 | 0.223–1.187 | 0.119 | 0.464 | 0.201–1.072 | 0.072 |
| Self-/parent-rated SDQ | 1.081 | 1.067–1.095 | <0.001 | 1.048 | 1.036–1.061 | <0.001 |
| Model 1: self-rated KINDL (R2 = 0.0454; p < 0.001) | Model 2: parent-rated KINDL (R2 = 0.0119; p < 0.001) | |||||
| Variable | Coeff. | 95% CI | P value | Coeff. | 95% CI | P value |
| Age | 0.0381 | 0.0019–0.0743 | 0.0393 | 0.0515 | 0.0151–0.0879 | 0.0055 |
| Body mass index (kg/m2) | 0.0241 | 0.0069–0.0413 | 0.0060 | 0.0279 | 0.0105–0.0452 | 0.0016 |
| Contraceptive user (%) | 0.7392 | 0.4819–0.9964 | <0.001 | 0.7176 | 0.4615–0.9738 | <0.001 |
| Blood pressure (mmHg) | −0.0145 | −0.0213 to –0076 | <0.001 | −0.0159 | −0.0227 to –0.0090 | <0.001 |
| Magnesium (mmol/L) | −0.8217 | −1.7165–0.0732 | 0.0719 | −0.9651 | −1.8606 to –0.0697 | 0.0346 |
| Quality of life (KINDL-R) | −0.0393 | −0.0457 to –0.0328 | <0.001 | −0.0299 | −0.0362 to –0.0236 | <0.001 |
| Indirect effect | E = −0.0034, 95% CI = −0.0213 to −0.0076 | E = −0.0022, 95% CI = −0.0033 to −0.0012 | ||||
| Model 3: self-rated SDQ (R2 = 0.0414; p < 0.001) | Model 4: parent-rated SDQ (R2 = 0.0578; p < 0.001) | |||||
| Variable | Coeff. | 95% CI | P value | Coeff. | 95% CI | P value |
| Age | 0.0645 | 0.0288–0.1003 | <0.001 | 0.0708 | 0.0345–0.1072 | <0.001 |
| Body mass index (kg/m2) | 0.0239 | 0.0067–0.0411 | 0.0064 | 0.0255 | 0.0082–0.0427 | 0.0038 |
| Contraceptive user (%) | 0.7138 | 0.4600–0.9676 | <0.001 | 0.7090 | 0.4549–0.9631 | <0.001 |
| Blood pressure (mmHg) | −0.0127 | −0.0195 to –0.0059 | <0.001 | −0.0148 | −0.0216 to –0.0080 | <0.001 |
| Magnesium (mmol/L) | −0.5696 | −1.4566–0.3174 | 0.2082 | −0.7343 | −1.6217–0.1531 | 0.1048 |
| Distress (SDQ) | 0.0797 | 0.0656–0.0938 | <0.001 | 0.0446 | 0.0322–0.0569 | <0.001 |
| Indirect effect | E = −0.0047, 95% CI = −0.0062 to −0.0033 | E = −0.0028, 95% CI = −0.0039 to −0.0017 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Córdova, M.A.C.; Stausberg, D.; Wang, B.; Becker, A.; Rothenberger, A.; Herrmann-Lingen, C.; Meyer, T.; Staab, J. Headache Is Associated with Low Systolic Blood Pressure and Psychosocial Problems in German Adolescents: Results from the Population-Based German KiGGS Study. J. Clin. Med. 2021, 10, 1492. https://doi.org/10.3390/jcm10071492
Córdova MAC, Stausberg D, Wang B, Becker A, Rothenberger A, Herrmann-Lingen C, Meyer T, Staab J. Headache Is Associated with Low Systolic Blood Pressure and Psychosocial Problems in German Adolescents: Results from the Population-Based German KiGGS Study. Journal of Clinical Medicine. 2021; 10(7):1492. https://doi.org/10.3390/jcm10071492
Chicago/Turabian StyleCórdova, Melissa A. Centeno, Daniela Stausberg, Biyao Wang, Andreas Becker, Aribert Rothenberger, Christoph Herrmann-Lingen, Thomas Meyer, and Julia Staab. 2021. "Headache Is Associated with Low Systolic Blood Pressure and Psychosocial Problems in German Adolescents: Results from the Population-Based German KiGGS Study" Journal of Clinical Medicine 10, no. 7: 1492. https://doi.org/10.3390/jcm10071492
APA StyleCórdova, M. A. C., Stausberg, D., Wang, B., Becker, A., Rothenberger, A., Herrmann-Lingen, C., Meyer, T., & Staab, J. (2021). Headache Is Associated with Low Systolic Blood Pressure and Psychosocial Problems in German Adolescents: Results from the Population-Based German KiGGS Study. Journal of Clinical Medicine, 10(7), 1492. https://doi.org/10.3390/jcm10071492







