Adult Gambling Problems and Histories of Mental Health and Substance Use: Findings from a Prospective Multi-Wave Australian Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Problem Gambling Severity
2.2.2. Mental Health Symptoms
2.2.3. Substance Use Behaviours
2.2.4. Mental Health Symptom and Substance Use Behaviour Histories
2.2.5. Potential Confounders
2.3. Statistical Analysis
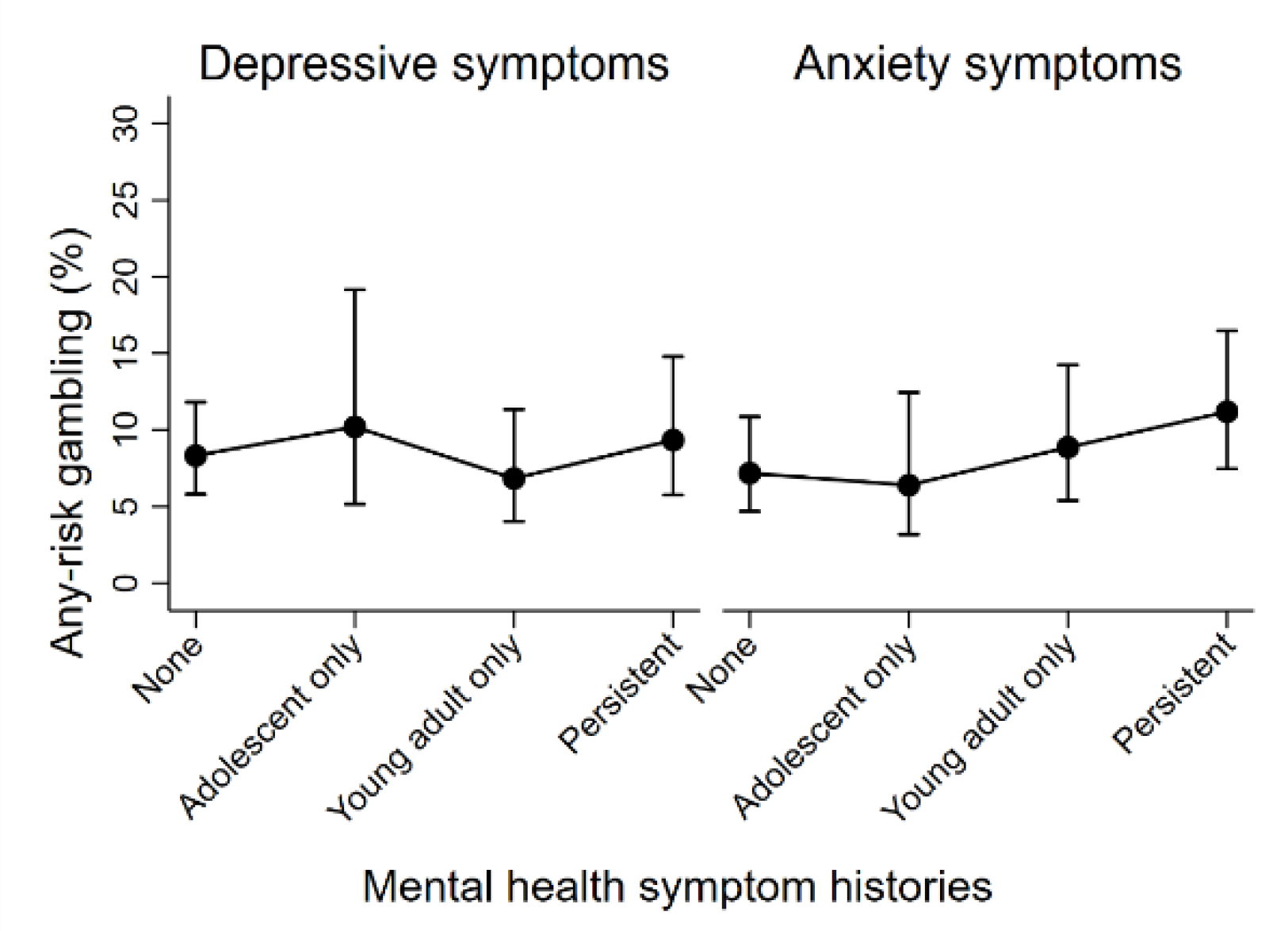
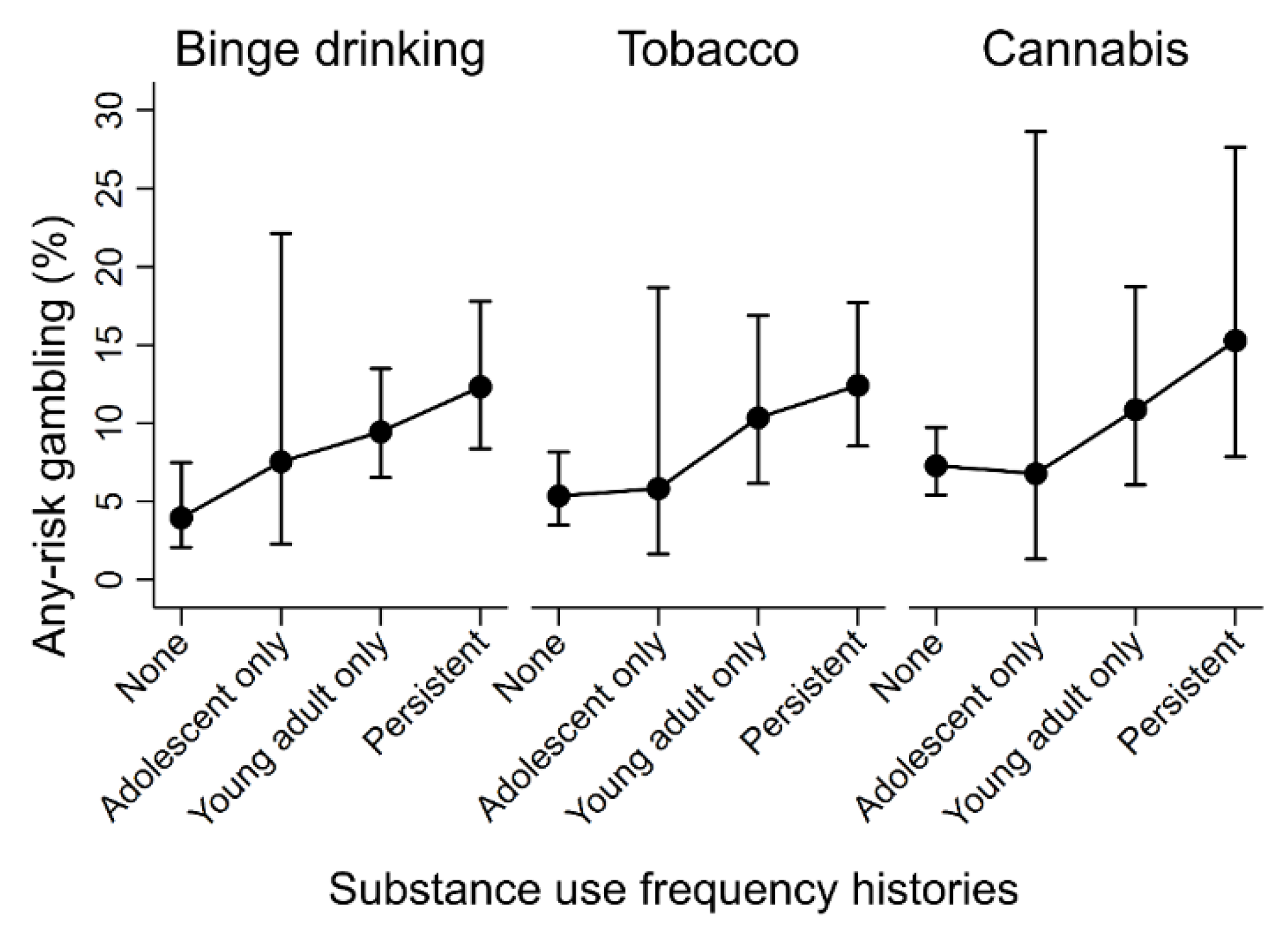
3. Results
4. Discussion
4.1. Substance Use Behaviours
4.2. Mental Health Symptoms
4.3. Sex Differences
4.4. Study Limitations
4.5. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Ferris, J.; Wynne, H. The Canadian Problem Gambling Index: Final Report; Canadian Centre on Substance Abuse: Ottawa, ON, Canada, 2001. [Google Scholar]
- Dowling, N.A.; Youssef, G.J.; Jackson, A.C.; Pennay, D.W.; Francis, K.L.; Pennay, A.; Lubman, D.I. National estimates of Australian gambling prevalence: Findings from a dual-frame omnibus survey. Addiction 2016, 111, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Gainsbury, S.M.; Russell, A.; Hing, N.; Wood, R.; Lubman, D.I.; Blaszczynski, A. The prevalence and determinants of problem gambling in Australia: Assessing the impact of interactive gambling and new technologies. Psychol. Addict. Behav. 2014, 28, 769. [Google Scholar] [CrossRef] [PubMed]
- Browne, M.; Greer, N.; Rawat, V.; Rockloff, M. A population-level metric for gambling-related harm. Int. Gambl. Stud. 2017, 17, 163–175. [Google Scholar] [CrossRef]
- Langham, E.; Thorne, H.; Browne, M.; Donaldson, P.; Rose, J.; Rockloff, M. Understanding gambling related harm: A proposed definition, conceptual framework, and taxonomy of harms. BMC Public Health 2016, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N.A.; Cowlishaw, S.; Jackson, A.C.; Merkouris, S.S.; Francis, K.L.; Christensen, D.R. Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Aust. N. Z. J. Psychiatry 2015, 49, 519–539. [Google Scholar] [CrossRef]
- Lorains, F.K.; Cowlishaw, S.; Thomas, S.A. Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction 2011, 106, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Cowlishaw, S.; Hakes, J.K.; Dowling, N.A. Gambling problems in treatment for affective disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J. Affect. Disord. 2016, 202, 110–114. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kennedy, S.H.; Welsh, B.R.; Fulton, K.; Soczynska, J.K.; McIntyre, R.S.; O’Donovan, C.; Milev, R.; le Melledo, J.-M.; Bisserbe, J.-C.; Zimmerman, M.; et al. Frequency and correlates of gambling problems in outpatients with major depressive disorder and bipolar disorder. Can. J. Psychiatry 2010, 55, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Manning, V.; Dowling, N.A.; Lee, S.; Rodda, S.; Garfield, J.B.B.; Volberg, R.; Kulkarni, J.; Lubman, D.I. Problem gambling and substance use in patients attending community mental health services. J. Behav. Addict. 2017. submitted. [Google Scholar] [CrossRef] [PubMed]
- Quilty, L.C.; Watson, C.; Robinson, J.J.; Toneatto, T.; Bagby, R.M. The prevalence and course of pathological gambling in the mood disorders. J. Gambl. Stud. 2011, 27, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Cowlishaw, S.; Merkouris, S.; Chapman, A.; Radermacher, H. Pathological and problem gambling in substance use treatment: A systematic review and meta-analysis. J. Subst. Abuse Treat. 2014, 46, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Nehlin, C.; Gronbladh, L.; Fredriksson, A.; Jansson, L. Alcohol and drug use, smoking, and gambling among psychiatric outpatients: A 1-year prevalence study. Subst. Abuse 2013, 34, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Ariyabuddhiphongs, V. Adolescent gambling: A narrative review of behavior and its predictors. Int. J. Ment. Health Addict. 2013, 11, 97–109. [Google Scholar] [CrossRef]
- Blinn-Pike, L.; Worthy, S.L.; Jonkman, J.N. Adolescent gambling: A review of an emerging field of research. J. Adolesc. Health 2010, 47, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Dickson, L.M.; Derevensky, J.L.; Gupta, R. The prevention of gambling problems in youth: A conceptual framework. J. Gambl. Stud. 2002, 18, 97–159. [Google Scholar] [CrossRef] [PubMed]
- Hardoon, K.; Derevensky, J.L. Child and adolescent gambling behavior: Current knowledge. Clin. Child Psychol. Psychiatry 2002, 7, 263–281. [Google Scholar] [CrossRef]
- Messerlian, C.; Gillespie, M.; Derevensky, J.L. Beyond drugs and alcohol: Including gambling in a high-risk behavioural framework. J. Paediatr. Child Health 2007, 12, 199–204. [Google Scholar] [CrossRef][Green Version]
- Shead, N.W.; Derevensky, J.L.; Gupta, R. Risk and protective factors associated with youth problem gambling. Int. J. Adolesc. Med. Health 2010, 22, 39–58. [Google Scholar]
- Dowling, N.A.; Merkouris, S.S.; Greenwood, C.J.; Oldenhof, E.; Toumbourou, J.W.; Youssef, G.J. Early risk and protective factors for problem gambling: A systematic review and meta-analysis of longitudinal studies. Clin. Psychol. Rev. 2017, 51, 109–124. [Google Scholar] [CrossRef] [PubMed]
- Fraser, M. Risk and Resilience in Childhood; National Association of Social Workers: Washington, DC, USA, 2004. [Google Scholar]
- Blanco, C.; Hasin, D.S.; Petry, N.; Stinson, F.S.; Grant, B.F. Sex differences in subclinical and DSM-IV pathological gambling: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2006, 36, 943–953. [Google Scholar] [CrossRef]
- Desai, R.A.; Potenza, M.N. Gender differences in the associations between past-year gambling problems and psychiatric disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2008, 43, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Díez, D.; Aragay, N.; Soms, M.; Prat, G.; Casas, M. Male and female pathological gamblers: Bet in a different way and show different mental disorders. Span. J. Psychol. 2014, 17, E101. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N.A.; Oldenhof, E. Gender Differences in Risk and Protective Factors for Problem Gambling. In Problem Gambling in Women: An International Perspective; Prever, H.B.-J.F., Ed.; Taylor and Francis: London, UK, 2017. [Google Scholar]
- Echeburúa, E.; González-Ortega, I.; de Corral, P.; Polo-López, R. Clinical gender differences among adult pathological gamblers seeking treatment. J. Gambl. Stud. 2011, 27, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Pilver, C.E.; Libby, D.J.; Hoff, R.A.; Potenza, M.N. Problem gambling severity and the incidence of Axis I psychopathology among older adults in the general population. J. Psychiatr. Res. 2013, 47, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Fröberg, F.; Hallqvist, J.; Tengström, A. Psychosocial health and gambling problems among men and women aged 16–24 years in the Swedish National Public Health Survey. Eur. J. Public Health 2013, 23, 427–433. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yücel, M.; Whittle, S.; Youssef, G.J.; Kashyap, H.; Simmons, J.G.; Schwartz, O.; Lubman, D.I.; Allen, N.B. The influence of sex, temperament, risk-taking and mental health on the emergence of gambling: A longitudinal study of young people. Int. Gambl. Stud. 2015, 15, 108–123. [Google Scholar] [CrossRef]
- Blanco, C.; Hanania, J.; Petry, N.M.; Wall, M.M.; Wang, S.; Jin, C.J.; Kendler, K.S. Towards a comprehensive developmental model of pathological gambling. Addiction 2015, 110, 1340–1351. [Google Scholar] [CrossRef] [PubMed]
- Rodda, S.N.; Dowling, N.A.; Thomas, A.C.; Bagot, K.L.; Lubman, D.I. Treatment for family members of people experiencing gambling problems: Family members want both gambler-focused and family-focused options. Int. J. Ment. Health Addict. 2019, 18, 1318–1334. [Google Scholar] [CrossRef]
- Hing, N.; Russell, A.; Tolchard, B.; Nower, L. Risk factors for gambling problems: An analysis by gender. J. Gambl. Stud. 2016, 32, 511–534. [Google Scholar] [CrossRef] [PubMed]
- Vassallo, S.; Sanson, A. The Australian Temperament Project: The First 30 Years; Melbourne, Australian Institue of Family Studies: Melbourne, Australia, 2013.
- Dellis, A.; Sharp, C.; Hofmeyr, A.; Schwardmann, P.M.; Spurrett, D.; Rousseau, J.; Ross, D. Criterion-related and construct validity of the Problem Gambling Severity Index in a sample of South African gamblers. South Afr. J. Psychol. 2014, 44, 243–257. [Google Scholar] [CrossRef]
- Merkouris, S.S.; Greenwood, C.; Manning, V.; Oakes, J.; Rodda, S.; Lubman, D.; Dowling, N.A. Enhancing the utility of the problem gambling severity index in clinical settings: Identifying refined categories within the problem gambling category. Addict. Behav. 2020, 103, 106257. [Google Scholar] [CrossRef]
- Neal, P.; Delfabbro, P.; O’Neil, M. Problem Gambling and Harm: Toward a National Definition; Office of Gaming and Racing: Melbourne, Australia, 2005.
- Williams, R.J.; Volberg, R.A. The classification accuracy of four problem gambling assessment instruments in population research. Int. Gambl. Stud. 2014, 14, 15–28. [Google Scholar] [CrossRef]
- Angold, A.; Costello, E.J.; Messer, S.; Pickles, A.; Winder, F. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int. J. Methods Psychiatr. Res. 1995, 5, 237–249. [Google Scholar]
- Turner, N.; Joinson, C.; Peters, T.J.; Wiles, N.; Lewis, G. Validity of the Short Mood and Feelings Questionnaire in late adolescence. Psychol. Assess. 2014, 26, 752. [Google Scholar] [CrossRef] [PubMed]
- Thapar, A.; McGuffin, P. Validity of the shortened Mood and Feelings Questionnaire in a community sample of children and adolescents: A preliminary research note. Psychiatry Res. 1998, 81, 259–268. [Google Scholar] [CrossRef]
- Rutter, M.; Tizard, J.; Whitmore, K. Education, Health and Behaviour; Longman: London, UK, 1970. [Google Scholar]
- Reynolds, C.R.; Richmond, B.O. What I think and feel: A revised measure of children’s manifest anxiety. J. Abnorm. Child Psychol. 1997, 25, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176. [Google Scholar] [CrossRef]
- Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation of Australia: Sydney, Australia, 1995.
- Moffitt, T.E.; Silva, P.A. Self-reported delinquency: Results from an instrument for new zealand. Aust. N. Z. J. Criminol. 1988, 21, 227–240. [Google Scholar] [CrossRef]
- StataCorp. Stata: Release 15. Statistical Software; StataCorp LP: College Station, TX, USA, 2017. [Google Scholar]
- Lee, K.J.; Carlin, J.B. Multiple imputation for missing data: Fully conditional specification versus multivariate normal imputation. Am. J. Epidemiol. 2010, 171, 624–632. [Google Scholar] [CrossRef] [PubMed]
- Bernaards, C.A.; Belin, T.R.; Schafer, J.L. Robustness of a multivariate normal approximation for imputation of incomplete binary data. Stat. Med. 2007, 26, 1368–1382. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley Series in Probability and Statistics; Wiley: Hoboken, NJ, USA, 1987. [Google Scholar]
- Chen, H.; Cohen, P.; Chen, S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun. Stat. Simul. Comput. 2010, 39, 860–864. [Google Scholar] [CrossRef]
- Baron, E.; Dickerson, M. Alcohol consumption and self-control of gambling behaviour. J. Gambl. Stud. 1999, 15, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Cooney, N.L.; Litt, M.D.; Morse, P.A.; Bauer, L.O.; Gaupp, L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J. Abnorm. Psychol. 1997, 106, 243. [Google Scholar] [CrossRef] [PubMed]
- Cronce, J.M.; Corbin, W.R. Effects of alcohol and initial gambling outcomes on within-session gambling behavior. Exp. Clin. Psychopharmacol. 2010, 18, 145. [Google Scholar] [CrossRef] [PubMed]
- Giacopassi, D.; Stitt, B.G.; Vandiver, M. An analysis of the relationship of alcohol to casino gambling among college students. J. Gambl. Stud. 1998, 14, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Kyngdon, A.; Dickerson, M. An experimental study of the effect of prior alcohol consumption on a simulated gambling activity. Addiction 1999, 94, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Blaszczynski, A.; Nower, L. A pathways model of problem and pathological gambling. Addiction 2002, 97, 487–499. [Google Scholar] [CrossRef] [PubMed]
- Merkouris, S.S.; Thomas, A.C.; Shandley, K.A.; Rodda, S.N.; Oldenhof, E.; Dowling, N.A. An update on gender differences in the characteristics associated with problem gambling: A systematic review. Curr. Addict. Rep. 2016, 3, 254–267. [Google Scholar] [CrossRef]
- Granero, R.; Penelo, E.; Martínez-Giménez, R.; Álvarez-Moya, E.; Gómez-Peña, M.; Aymamí, M.N.; Bueno, B.; Fernández-Aranda, F.; Jiménez-Murcia, S. Sex differences among treatment-seeking adult pathologic gamblers. Compr. Psychiatry 2009, 50, 173–180. [Google Scholar] [CrossRef] [PubMed]
- LaPlante, D.A.; Nelson, S.E.; LaBrie, R.A.; Shaffer, H.J. Men & women playing games: Gender and the gambling preferences of Iowa gambling treatment program participants. J. Gambl. Stud. 2006, 22, 65. [Google Scholar] [PubMed]
- Nelson, S.E.; LaPlante, D.A.; LaBrie, R.A.; Shaffer, H.J. The proxy effect: Gender and gambling problem trajectories of Iowa gambling treatment program participants. J. Gambl. Stud. 2006, 22, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355. [Google Scholar] [CrossRef] [PubMed]
- Kuentzel, J.G.; Henderson, M.J.; Melville, C.L. The impact of social desirability biases on self-report among college student and problem gamblers. J. Gambl. Stud. 2008, 24, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Salam, R.A.; Arshad, A.; Finkelstein, Y.; Bhutta, Z.A. Interventions for adolescent substance abuse: An overview of systematic reviews. J. Adolesc. Health 2016, 59, S61–S75. [Google Scholar] [CrossRef] [PubMed]
- Tanner-Smith, E.E.; Lipsey, M.W. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. J. Subst. Abus. Treat. 2015, 51, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N.A.; Merkouris, S.S.; Dias, S.; Rodda, S.N.; Manning, V.; Youssef, G.J.; Lubman, D.I.; Volberg, R.A. The diagnostic accuracy of brief screening instruments for problem gambling: A systematic review and meta-analysis. Clin. Psychol. Rev. 2019, 74, 101784. [Google Scholar] [CrossRef] [PubMed]
| Problem Gambling Severity | |||
| n | % | 95% CI | |
| Any-Risk Gambling | 137 | 10.26 | (8.24, 12.28) |
| Mental Health and Substance Use Histories | |||
| n | % | 95% CI | |
| Depressive symptoms | |||
| None | 565 | 42.4 | (39.34, 45.47) |
| Adolescence only | 135 | 10.09 | (8.17, 12.01) |
| Young adulthood only | 307 | 23.01 | (20.15, 25.86) |
| Persistent | 327 | 24.5 | (21.88, 27.12) |
| Anxiety symptoms | |||
| None | 483 | 36.24 | (33.15, 39.33) |
| Adolescence only | 222 | 16.66 | (14.35, 18.97) |
| Young adulthood only | 293 | 22.01 | (19.18, 24.85) |
| Persistent | 334 | 25.08 | (22.44, 27.73) |
| Binge drinking | |||
| None | 394 | 29.55 | (26.81, 32.3) |
| Adolescence only | 60 | 4.48 | (3.07, 5.89) |
| Young adulthood only | 536 | 40.18 | (37.16, 43.2) |
| Persistent | 344 | 25.79 | (23.04, 28.53) |
| Tobacco | |||
| None | 607 | 45.57 | (42.52, 48.62) |
| Adolescence only | 74 | 5.58 | (4.04, 7.12) |
| Young adulthood only | 223 | 16.74 | (13.94, 19.54) |
| Persistent | 428 | 32.11 | (29.3, 34.91) |
| Cannabis | |||
| None | 977 | 73.3 | (70.45, 76.15) |
| Adolescence only | 43 | 3.25 | (2.05, 4.45) |
| Young adulthood only | 210 | 15.73 | (13.16, 18.3) |
| Persistent | 103 | 7.72 | (6.09, 9.34) |
| Potential confounding factors | |||
| n | % | 95% CI | |
| Parent non-Australian birth | 360 | 26.98 | (24.59, 29.37) |
| Parent separation/divorce | 213 | 15.95 | (13.98, 17.91) |
| Parent low education (<year 12) | 342 | 25.69 | (23.37, 28.01) |
| Women | 721 | 54.07 | (51.42, 56.71) |
| Adolescent anti-social behaviour | 608 | 45.64 | (42.95, 48.32) |
| Behaviour problems | 267 | 20.04 | (17.74, 22.35) |
| Early (<13 years) gambling | 100 | 7.47 | (5.52, 9.41) |
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Depressive symptoms | ||||||
| None | 1.00 | 1.00 | ||||
| Adolescence only | 1.13 | (0.52, 2.46) | 0.759 | 1.25 | (0.56, 2.80) | 0.583 |
| Young adulthood only | 1.06 | (0.56, 2.01) | 0.860 | 0.81 | (0.42, 1.56) | 0.524 |
| Persistent | 1.19 | (0.67, 2.10) | 0.560 | 1.13 | (0.61, 2.09) | 0.685 |
| Anxiety symptoms | ||||||
| None | 1.00 | 1.00 | ||||
| Adolescence only | 0.75 | (0.33, 1.72) | 0.501 | 0.88 | (0.37, 2.08) | 0.775 |
| Young adulthood only | 1.57 | (0.85, 2.91) | 0.148 | 1.26 | (0.67, 2.38) | 0.478 |
| Persistent | 1.49 | (0.81, 2.72) | 0.196 | 1.63 | (0.86, 3.08) | 0.132 |
| Binge drinking | ||||||
| None | 1.00 | 1.00 | ||||
| Adolescence only | 1.98 | (0.48, 8.20) | 0.343 | 1.98 | (0.47, 8.37) | 0.351 |
| Young adulthood only | 3.35 | (1.62, 6.94) | 0.001 | 2.54 | (1.17, 5.50) | 0.019 |
| Persistent | 5.09 | (2.46, 10.53) | 0.000 | 3.42 | (1.54, 7.59) | 0.003 |
| Tobacco | ||||||
| None | 1.00 | 1.00 | ||||
| Adolescence only | 0.98 | (0.24, 3.93) | 0.978 | 1.09 | (0.27, 4.49) | 0.903 |
| Young adulthood only | 2.31 | (1.18, 4.51) | 0.014 | 2.04 | (1.03, 4.05) | 0.042 |
| Persistent | 2.71 | (1.54, 4.77) | 0.001 | 2.50 | (1.34, 4.66) | 0.004 |
| Cannabis | ||||||
| None | 1.00 | 1.00 | ||||
| Adolescence only | 1.09 | (0.20, 6.03) | 0.924 | 0.93 | (0.16, 5.36) | 0.931 |
| Young adulthood only | 2.00 | (1.04, 3.86) | 0.038 | 1.55 | (0.77, 3.14) | 0.221 |
| Persistent | 3.19 | (1.53, 6.61) | 0.002 | 2.30 | (1.01, 5.20) | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merkouris, S.S.; Greenwood, C.J.; Youssef, G.J.; Letcher, P.; Vassallo, S.; Dowling, N.A.; Olsson, C.A. Adult Gambling Problems and Histories of Mental Health and Substance Use: Findings from a Prospective Multi-Wave Australian Cohort Study. J. Clin. Med. 2021, 10, 1406. https://doi.org/10.3390/jcm10071406
Merkouris SS, Greenwood CJ, Youssef GJ, Letcher P, Vassallo S, Dowling NA, Olsson CA. Adult Gambling Problems and Histories of Mental Health and Substance Use: Findings from a Prospective Multi-Wave Australian Cohort Study. Journal of Clinical Medicine. 2021; 10(7):1406. https://doi.org/10.3390/jcm10071406
Chicago/Turabian StyleMerkouris, Stephanie S., Christopher J. Greenwood, George J. Youssef, Primrose Letcher, Suzanne Vassallo, Nicki A. Dowling, and Craig A. Olsson. 2021. "Adult Gambling Problems and Histories of Mental Health and Substance Use: Findings from a Prospective Multi-Wave Australian Cohort Study" Journal of Clinical Medicine 10, no. 7: 1406. https://doi.org/10.3390/jcm10071406
APA StyleMerkouris, S. S., Greenwood, C. J., Youssef, G. J., Letcher, P., Vassallo, S., Dowling, N. A., & Olsson, C. A. (2021). Adult Gambling Problems and Histories of Mental Health and Substance Use: Findings from a Prospective Multi-Wave Australian Cohort Study. Journal of Clinical Medicine, 10(7), 1406. https://doi.org/10.3390/jcm10071406






