Prognostic Impact of Perioperative CA19-9 Levels in Patients with Resected Perihilar Cholangiocarcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Preoperative Management
2.3. Surgical Procedures
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. Prognostic Value of Pre- and Postoperative CA19-9 Levels
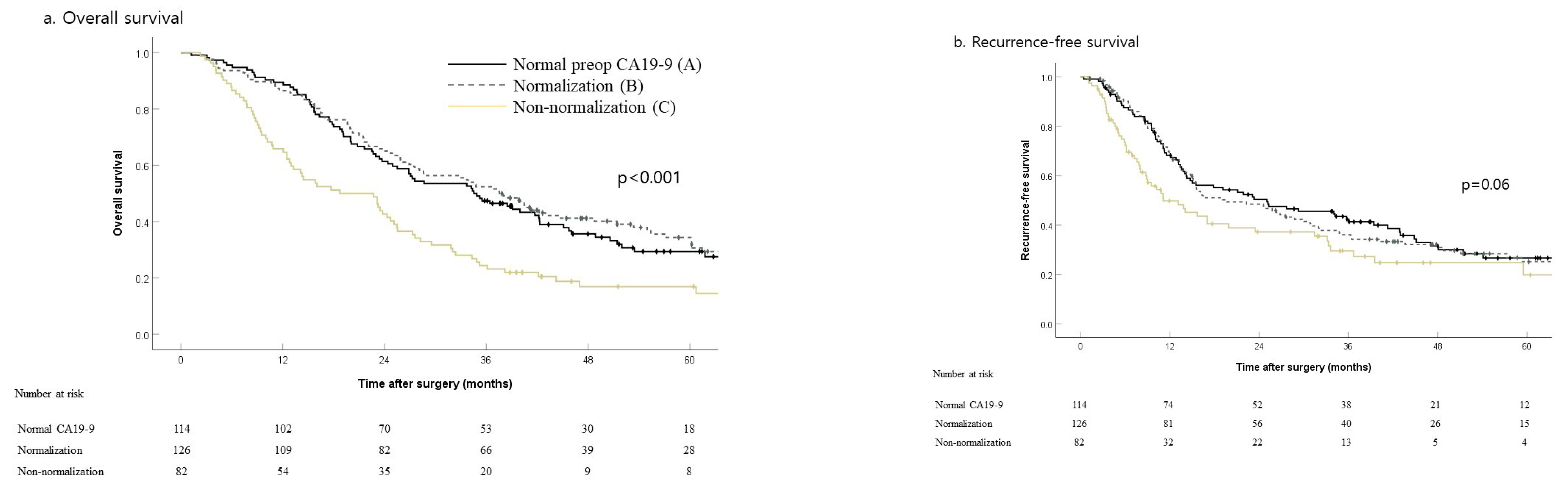
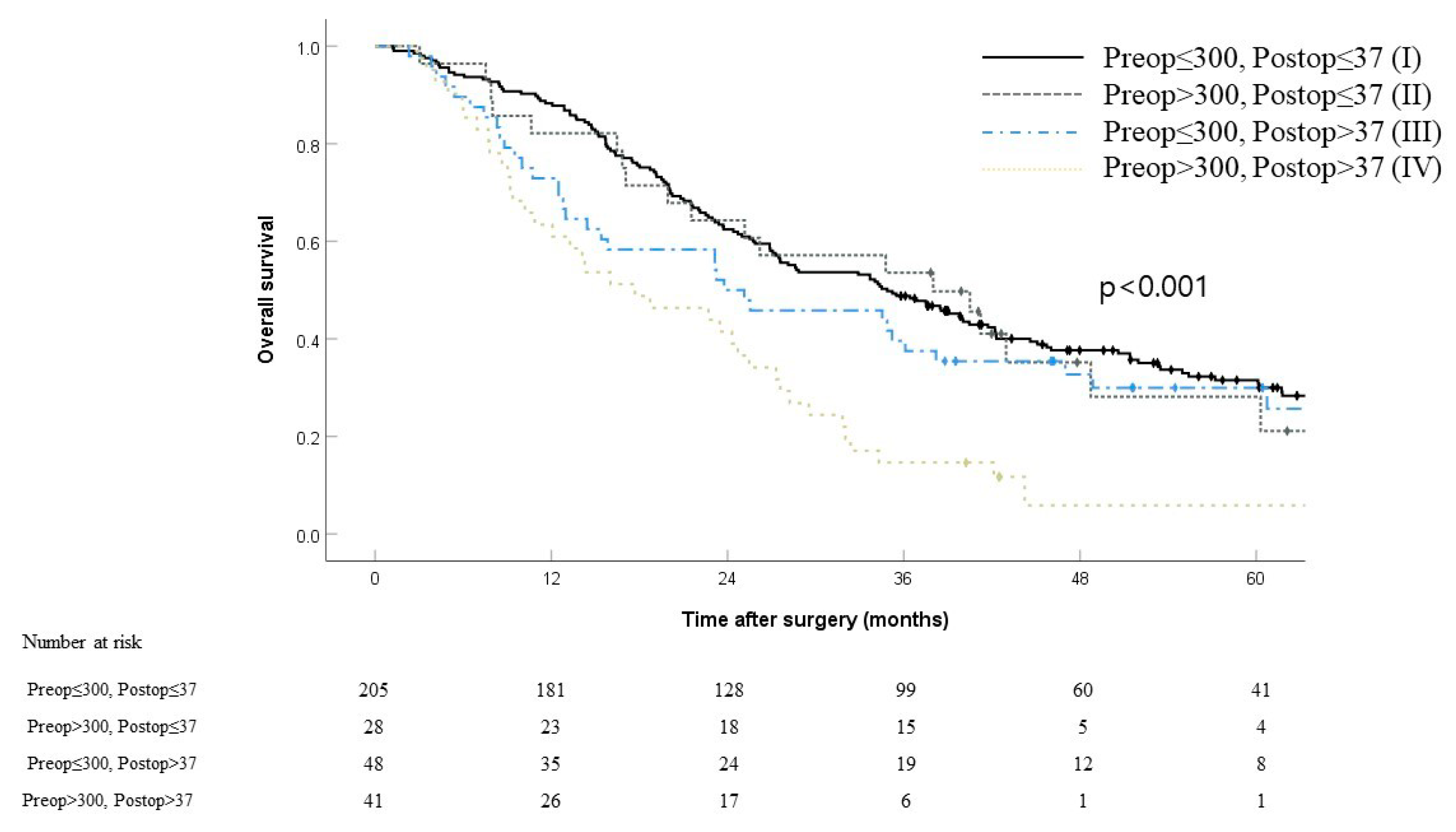
3.3. Outcomes According to Perioperative CA19-9 Status
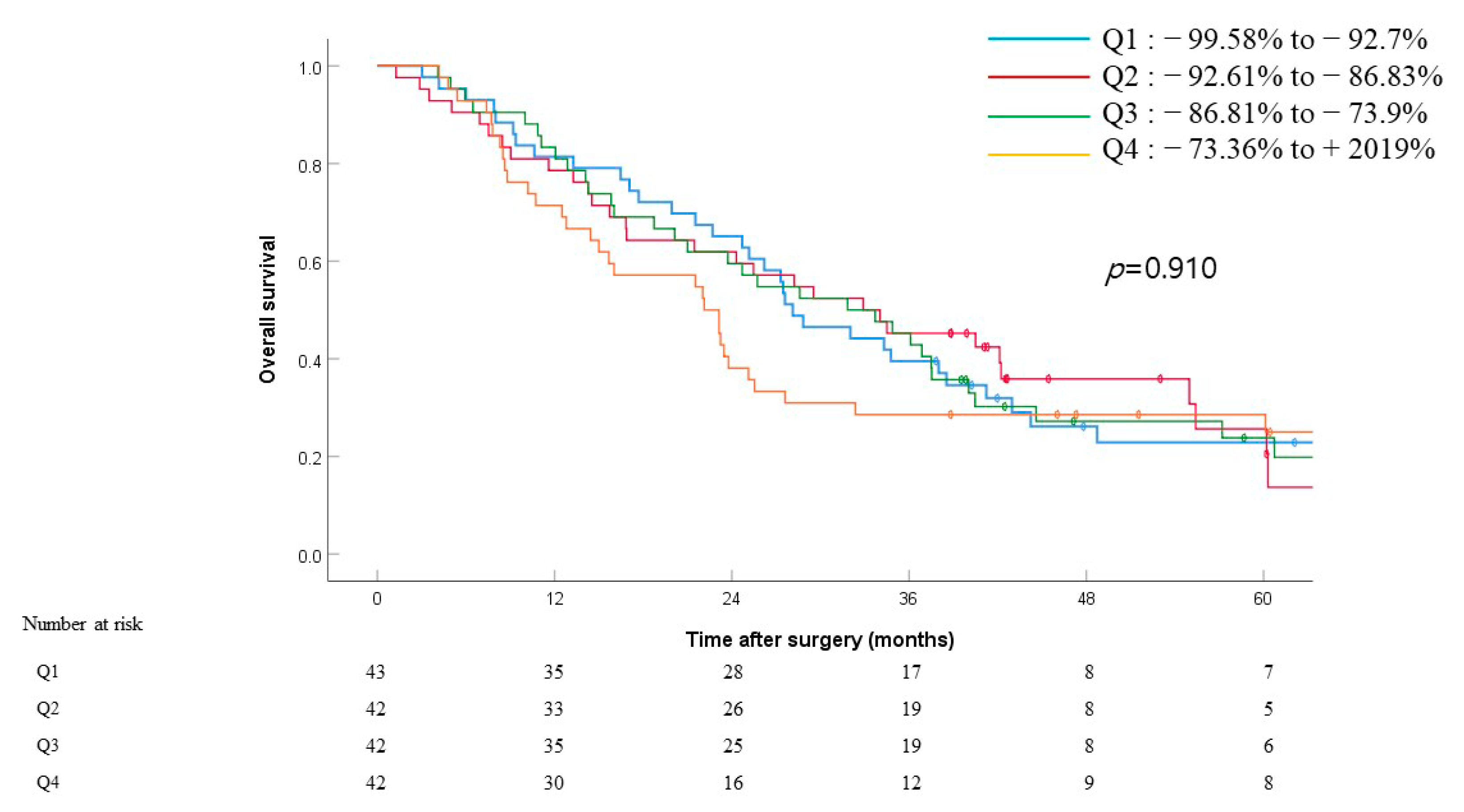
3.4. Effect of Changes in Perioperative CA19-9 Levels on Survival
3.5. Univariate and Multivariate OS Analyses for Clinicopathological Factors
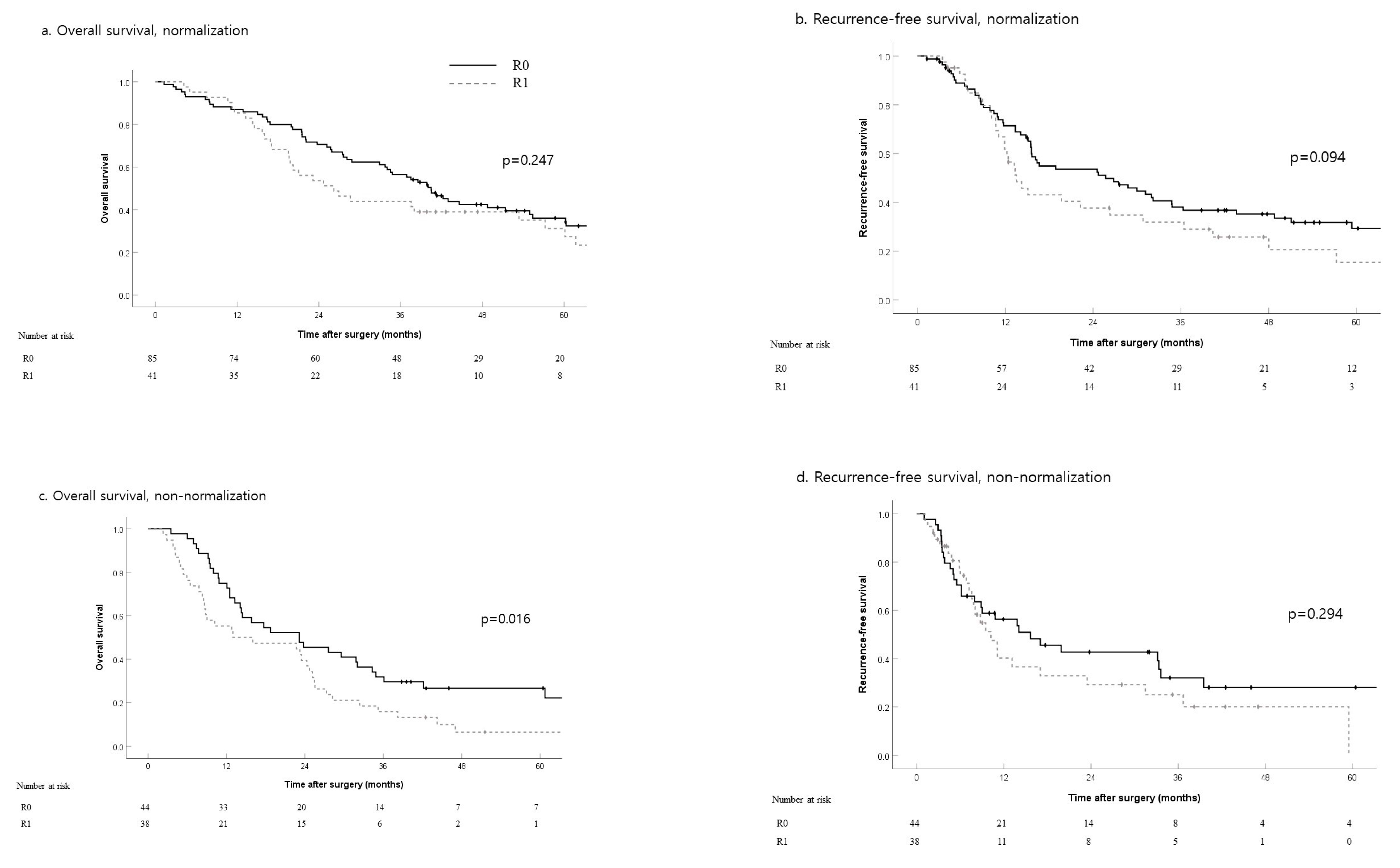
3.6. Outcomes According to Resection Margin in Patients with Elevated Preoperative CA19-9
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Groot Koerkamp, B.; Wiggers, J.K.; Allen, P.J.; Busch, O.R.; D’Angelica, M.I.; DeMatteo, R.P.; Fong, Y.; Gonen, M.; Gouma, D.J.; Kingham, T.P.; et al. American Joint Committee on Cancer staging for resected perihilar cholangiocarcinoma: A comparison of the 6th and 7th editions. HPB (Oxford) 2014, 16, 1074–1082. [Google Scholar] [CrossRef]
- Koprowski, H.; Steplewski, Z.; Mitchell, K.; Herlyn, M.; Herlyn, D.; Fuhrer, P. Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet. 1979, 5, 957–971. [Google Scholar] [CrossRef] [PubMed]
- Del Villano, B.C.; Brennan, S.; Brock, P.; Bucher, C.; Liu, V.; McClure, M.; Rake, B.; Space, S.; Westrick, B.; Schoemaker, H.; et al. Radioimmunometric assay for a monoclonal antibody-defined tumor marker, CA 19-9. Clin. Chem. 1983, 29, 549–552. [Google Scholar] [CrossRef]
- Humphris, J.L.; Chang, D.K.; Johns, A.L.; Scarlett, C.J.; Pajic, M.; Jones, M.D.; Colvin, E.K.; Nagrial, A.; Chin, V.T.; Chantrill, L.A.; et al. The prognostic and predictive value of serum CA19.9 in pancreatic cancer. Ann. Oncol. 2012, 23, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Kondo, N.; Murakami, Y.; Uemura, K.; Hayashidani, Y.; Sudo, T.; Hashimoto, Y.; Nakashima, A.; Sakabe, R.; Shigemoto, N.; Kato, Y.; et al. Prognostic impact of perioperative serum CA 19-9 levels in patients with resectable pancreatic cancer. Ann. Surg. Oncol. 2010, 17, 2321–2329. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, S.; Passot, G.; Aloia, T.A.; Chun, Y.S.; Javle, M.; Lee, J.E.; Vauthey, J.N.; Conrad, C. Prognostic value of carbohydrate antigen 19-9 in patients undergoing resection of biliary tract cancer. Br. J. Surg. 2017, 104, 267–277. [Google Scholar] [CrossRef]
- Kondo, N.; Murakami, Y.; Uemura, K.; Sudo, T.; Hashimoto, Y.; Sasaki, H.; Sueda, T. Elevated perioperative serum CA 19-9 levels are independent predictors of poor survival in patients with resectable cholangiocarcinoma. J. Surg. Oncol. 2014, 110, 422–429. [Google Scholar] [CrossRef]
- Cai, W.K.; Lin, J.J.; He, G.H.; Wang, H.; Lu, J.H.; Yang, G.S. Preoperative serum CA19-9 levels is an independent prognostic factor in patients with resected hilar cholangiocarcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 7890–7898. [Google Scholar]
- Chaiteerakij, R.; Harmsen, W.S.; Marrero, C.R.; Aboelsoud, M.M.; Ndzengue, A.; Kaiya, J.; Therneau, T.M.; Sanchez, W.; Gores, G.J.; Roberts, L.R. A new clinically based staging system for perihilar cholangiocarcinoma. Am. J. Gastroenterol. 2014, 109, 1881–1890. [Google Scholar] [CrossRef]
- Juntermanns, B.; Radunz, S.; Heuer, M.; Hertel, S.; Reis, H.; Neuhaus, J.P.; Vernadakis, S.; Trarbach, T.; Paul, A.; Kaiser, G.M. Tumor markers as a diagnostic key for hilar cholangiocarcinoma. Eur. J. Med. Res. 2010, 15, 357–361. [Google Scholar] [CrossRef]
- Ramacciato, G.; Nigri, G.; Bellagamba, R.; Petrucciani, N.; Ravaioli, M.; Cescon, M.; Del Gaudio, M.; Ercolani, G.; Di Benedetto, F.; Cautero, N.; et al. Univariate and multivariate analysis of prognostic factors in the surgical treatment of hilar cholangiocarcinoma. Am. Surg. 2010, 76, 1260–1268. [Google Scholar] [CrossRef] [PubMed]
- Sano, T.; Shimada, K.; Sakamoto, Y.; Ojima, H.; Esaki, M.; Kosuge, T. Prognosis of perihilar cholangiocarcinoma: Hilar bile duct cancer versus intrahepatic cholangiocarcinoma involving the hepatic hilus. Ann. Surg. Oncol. 2008, 15, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Ebata, T.; Kosuge, T.; Hirano, S.; Unno, M.; Yamamoto, M.; Miyazaki, M.; Kokudo, N.; Miyagawa, S.; Takada, T.; Nagino, M. Proposal to modify the International Union Against Cancer staging system for perihilar cholangiocarcinomas. Br. J. Surg. 2014, 101, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.K.; Hu, H.J.; Shrestha, A.; Ma, W.J.; Yang, Q.; Liu, F.; Cheng, N.S.; Li, F.Y. Can preoperative and postoperative CA19-9 levels predict survival and early recurrence in patients with resectable hilar cholangiocarcinoma? Oncotarget 2017, 8, 45335–45344. [Google Scholar] [CrossRef][Green Version]
- Koo, T.R.; Eom, K.Y.; Kim, I.A.; Cho, J.Y.; Yoon, Y.S.; Hwang, D.W.; Han, H.S.; Kim, J.S. Patterns of failure and prognostic factors in resected extrahepatic bile duct cancer: Implication for adjuvant radiotherapy. Radiat. Oncol. J. 2014, 32, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.J.; Lee, K.J.; Bang, S.; Park, S.W.; Kim, K.S.; Lee, W.J.; Song, S.Y.; Chung, J.B.; Park, J.Y. Preoperative serum CA 19-9 level as a predictive factor for recurrence after curative resection in biliary tract cancer. Ann. Surg. Oncol. 2011, 18, 1651–1656. [Google Scholar] [CrossRef]
- Hatzaras, I.; Schmidt, C.; Muscarella, P.; Melvin, W.S.; Ellison, E.C.; Bloomston, M. Elevated CA 19-9 portends poor prognosis in patients undergoing resection of biliary malignancies. HPB (Oxford) 2010, 12, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.C.; Garcia, M., Jr.; Hoffman, J.P.; Regine, W.F.; Abrams, R.A.; Safran, H.; Konski, A.; Benson, A.B., 3rd; MacDonald, J.; Willett, C.G. Postresection CA 19-9 predicts overall survival in patients with pancreatic cancer treated with adjuvant chemoradiation: A prospective validation by RTOG 9704. J. Clin. Oncol. 2008, 26, 5918–5922. [Google Scholar] [CrossRef]
- Ferrone, C.R.; Finkelstein, D.M.; Thayer, S.P.; Muzikansky, A.; Fernandez-delCastillo, C.; Warshaw, A.L. Perioperative CA19-9 levels can predict stage and survival in patients with resectable pancreatic adenocarcinoma. J. Clin. Oncol. 2006, 24, 2897–2902. [Google Scholar] [CrossRef] [PubMed]
- Ruzzenente, A.; Bagante, F.; Ardito, F.; Campagnaro, T.; Scoleri, I.; Conci, S.; Iacono, C.; Giuliante, F.; Guglielmi, A. Comparison of the 7th and 8th editions of the American Joint Committee on Cancer Staging Systems for perihilar cholangiocarcinoma. Surgery 2018, 164, 244–250. [Google Scholar] [CrossRef]
- Yoo, T.; Park, S.J.; Han, S.S.; Kim, S.H.; Lee, S.D.; Kim, T.H.; Lee, S.A.; Woo, S.M.; Lee, W.J.; Hong, E.K. Proximal Resection Margins: More Prognostic than Distal Resection Margins in Patients Undergoing Hilar Cholangiocarcinoma Resection. Cancer Res. Treat. 2018, 50, 1106–1113. [Google Scholar] [CrossRef]
- Hartwig, W.; Strobel, O.; Hinz, U.; Fritz, S.; Hackert, T.; Roth, C.; Buchler, M.W.; Werner, J. CA19-9 in potentially resectable pancreatic cancer: Perspective to adjust surgical and perioperative therapy. Ann. Surg. Oncol. 2013, 20, 2188–2196. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Kim, H.S.; Song, K.S.; Noh, S.H.; Kim, H.G.; Paik, Y.K.; Kim, H.O. Altered expression of Lewis antigen on tissue and erythrocytes in gastric cancer patients. Yonsei Med. J. 2002, 43, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Tempero, M.A.; Uchida, E.; Takasaki, H.; Burnett, D.A.; Steplewski, Z.; Pour, P.M. Relationship of carbohydrate antigen 19-9 and Lewis antigens in pancreatic cancer. Cancer Res. 1987, 47, 5501–5503. [Google Scholar]
- Regine, W.F.; Winter, K.A.; Abrams, R.A.; Safran, H.; Hoffman, J.P.; Konski, A.; Benson, A.B.; Macdonald, J.S.; Kudrimoti, M.R.; Fromm, M.L.; et al. Fluorouracil vs. gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: A randomized controlled trial. JAMA 2008, 299, 1019–1026. [Google Scholar] [CrossRef]
- Hidalgo, M. Pancreatic cancer. N. Engl. J. Med. 2010, 362, 1605–1617. [Google Scholar] [CrossRef]
- Orntoft, T.F.; Vestergaard, E.M.; Holmes, E.; Jakobsen, J.S.; Grunnet, N.; Mortensen, M.; Johnson, P.; Bross, P.; Gregersen, N.; Skorstengaard, K.; et al. Influence of Lewis alpha1-3/4-L-fucosyltransferase (FUT3) gene mutations on enzyme activity, erythrocyte phenotyping, and circulating tumor marker sialyl-Lewis a levels. J. Biol. Chem. 1996, 271, 32260–32268. [Google Scholar] [CrossRef] [PubMed]
- Lamerz, R. Role of tumour markers, cytogenetics. Ann. Oncol. 1999, 10 (Suppl. 4), 145–149. [Google Scholar] [CrossRef]
- Vestergaard, E.M.; Hein, H.O.; Meyer, H.; Grunnet, N.; Jorgensen, J.; Wolf, H.; Orntoft, T.F. Reference values and biological variation for tumor marker CA 19-9 in serum for different Lewis and secretor genotypes and evaluation of secretor and Lewis genotyping in a Caucasian population. Clin. Chem. 1999, 45, 54–61. [Google Scholar]
| Normal CA19-9 (A, n = 114) | Normalization (B, n = 126) | Non-Normalization (C, n = 82) | p-Value | |||
|---|---|---|---|---|---|---|
| A vs. B | A vs. C | B vs. C | ||||
| Age (years) | 64.2 ± 9.0 | 63.1 ± 9.6 | 63.6 ± 8.0 | 0.364 | 0.617 | 0.714 |
| Sex ratio (male:female) | 76:38 | 89:37 | 52:30 | 0.508 | 0.637 | 0.276 |
| BMI (kg/m2) | 23.6 ± 3.0 | 23.0 ± 2.7 | 22.8 ± 2.6 | 0.129 | 0.068 | 0.595 |
| Jaundice at presentation | 47 (41.2%) | 80 (63.5%) | 54 (65.9%) | 0.001 | 0.001 | 0.728 |
| Albumin (g/dL) | 3.4 ± 0.4 | 3.3 ± 0.5 | 3.3 ± 0.4 | 0.088 | 0.026 | 0.541 |
| Total bilirubin (mg/dL) | 1.5 ± 1.2 | 1.9 ± 1.4 | 2.1 ± 1.5 | 0.053 | 0.011 | 0.364 |
| Preoperative biliary drainage | 0.025 | 0.124 | 0.723 | |||
| None | 25 (21.9%) | 18 (14.3%) | 11 (13.4%) | |||
| Percutaneous transhepatic drainage | 54 (47.4%) | 80 (63.5%) | 47 (57.3%) | |||
| Endoscopic drainage | 31 (27.2%) | 20 (15.9%) | 17 (20.7%) | |||
| Both | 4 (3.5%) | 8 (6.3%) | 7 (8.5%) | |||
| Preoperative cholangitis | 20 (17.5%) | 24 (19.0%) | 23 (28.0%) | 0.764 | 0.080 | 0.129 |
| Preoperative CA19-9 (U/mL) | 16.3 ± 9.9 | 245.4 ± 441.9 | 1420.3 ± 3860.6 | <0.001 | 0.001 | 0.007 |
| Portal vein embolization | 2 (1.8%) | 2 (1.6%) | 4 (4.9%) | 1.000 | 0.239 | 0.215 |
| Liver resection type | 0.130 | 0.040 | 0.136 | |||
| RH and ERH | 77 (67.5%) | 73 (57.9%) | 55 (67.1%) | |||
| RTS | 2 (1.8%) | 6 (4.8%) | 5 (6.1%) | |||
| LH and ELH | 32 (28.1%) | 37 (29.4%) | 14 (17.1%) | |||
| LTS | 3 (2.6%) | 10 (7.9%) | 6 (7.3%) | |||
| CBS | 0 | 0 | 2 (0.6%) | |||
| Portal vein resection | 12 (10.5%) | 22 (17.5%) | 16 (19.5%) | 0.124 | 0.076 | 0.708 |
| R1 resection | 42 (36.8%) | 41 (32.5%) | 38 (46.3%) | 0.484 | 0.182 | 0.045 |
| Intraoperative transfusion | 38 (33.3%) | 47 (37.3%) | 31 (37.8%) | 0.521 | 0.518 | 0.942 |
| Operative time(min) | 357.9 ± 75.0 | 362.5 ± 69.4 | 380.5 ± 78.8 | 0.625 | 0.043 | 0.084 |
| Bismuth type | 0.507 | 0.149 | 0.800 | |||
| I | 5 (4.4%) | 5 (4.0%) | 2 (2.4%) | |||
| II | 22 (19.3%) | 18 (14.3%) | 8 (9.8%) | |||
| IIIa | 50 (43.9%) | 57 (45.2%) | 37 (45.1%) | |||
| IIIb | 22 (19.3%) | 20 (15.9%) | 15 (18.3%) | |||
| IV | 15 (13.2%) | 26 (20.6%) | 20 (24.4%) | |||
| TNM stage (AJCC 8th) | 0.226 | <0.001 | 0.063 | |||
| I | 19 (16.7%) | 10 (7.9%) | 4 (4.9%) | |||
| II | 48 (42.1%) | 48 (38.1%) | 18 (22.0%) | |||
| IIIA | 10 (8.8%) | 14 (11.1%) | 7 (8.5%) | |||
| IIIB | 3 (2.6%) | 6 (4.8%) | 6 (7.3%) | |||
| IIIC | 28 (24.6%) | 36 (28.6%) | 29 (35.4%) | |||
| IVA | 6 (5.3%) | 9 (7.1%) | 14 (17.1%) | |||
| IVB | 0 | 3 (2.4%) | 4 (4.9%) | |||
| Hospital stay (days) | 20.7 ± 12.6 | 20.0 ± 12.2 | 23.9 ± 15.2 | 0.659 | 0.104 | 0.050 |
| 90-day mortality | 1 (0.9%) | 0 | 1 (1.2%) | 0.475 | 1.000 | 0.394 |
| Postoperative CA19-9 (U/mL) | 14.7 ± 17.2 | 20.0 ± 9.3 | 186.1 ± 349.2 | 0.003 | <0.001 | <0.001 |
| Overall survival (months) | 36.5 ± 24.3 | 39.7 ± 26.7 | 25.9 ± 23.2 | 0.334 | 0.003 | 0.000 |
| Recurrence-free survival (months) | 28.0 ± 23.9 | 28.6 ± 26.6 | 18.6 ± 22.1 | 0.862 | 0.006 | 0.004 |
| Adjuvant chemotherapy | 44 (38.6%) | 52 (41.3%) | 33 (40.2%) | 0.673 | 0.816 | 0.883 |
| Adjuvant radiotherapy | 25 (21.9%) | 23 (18.3%) | 19 (23.2%) | 0.477 | 0.837 | 0.388 |
| Tumor size (cm) | 2.9 ± 1.5 | 3.3 ± 1.5 | 3.5 ± 1.9 | 0.054 | 0.015 | 0.451 |
| LN metastasis | 33 (28.9%) | 48 (38.1%) | 47 (57.3%) | 0.134 | <0.001 | 0.007 |
| Perineural invasion | 88 (77.2%) | 110 (87.3%) | 71 (86.6%) | 0.040 | 0.097 | 0.881 |
| Lympho-vascular invasion | 55 (48.2%) | 57 (45.2%) | 48 (58.5%) | 0.641 | 0.155 | 0.061 |
| Recurrence | 75 | 84 | 53 | 0.901 | 0.048 | 0.070 |
| Locoregional | 30 (26.3%) | 32 (25.4%) | 9 (11.0%) | |||
| Systemic | 29 (25.4%) | 37 (29.4%) | 30 (36.6%) | |||
| Both | 16 (14.0%) | 15 (11.9%) | 14 (17.1%) | |||
| CA19-9 Cut-off Value (U/mL) | Preoperative CA19-9 | Postoperative CA19-9 | ||||
|---|---|---|---|---|---|---|
| Patient Number (n) | Median Survival (Months) | p-Value | Patient Number (n) | Median Survival (Months) | p-Value | |
| ≤37 | 114 | 34.53 | 0.300 | 233 | 35.23 | 0.000 |
| >37 | 208 | 27.47 | 89 | 23.13 | ||
| ≤100 | 190 | 33.70 | 0.138 | 288 | 34.37 | 0.000 |
| >100 | 132 | 27.30 | 34 | 10.87 | ||
| ≤200 | 229 | 33.70 | 0.027 | 307 | 33.70 | 0.000 |
| >200 | 93 | 26.20 | 15 | 8.50 | ||
| ≤300 | 253 | 34.37 | 0.001 | 309 | 32.90 | 0.000 |
| >300 | 69 | 24.3 | 13 | 8.50 | ||
| ≤400 | 270 | 33.70 | 0.003 | 315 | 29.53 | 0.003 |
| >400 | 52 | 24.30 | 7 | 12.07 | ||
| ≤1000 | 297 | 32.90 | 0.007 | 318 | 28.83 | 0.001 |
| >1000 | 25 | 24.70 | 4 | 5.40 | ||
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age (years) | 1.01 | 0.99–1.02 | 0.390 | |||
| Albumin (g/dL) | 0.92 | 0.70–1.20 | 0.528 | |||
| Total bilirubin (mg/dL) | 1.07 | 0.98–1.17 | 0.111 | |||
| Prothrombin time (min) | 1.39 | 0.38–5.00 | 0.618 | |||
| Quartile of ΔCA19-9 | 0.425 | |||||
| Q1 | Ref. | |||||
| Q2 | 0.90 | 0.58–1.40 | 0.636 | |||
| Q3 | 0.88 | 0.57–1.37 | 0.578 | |||
| Q4 | 1.23 | 0.80–1.88 | 0.350 | |||
| Preop CA19-9 >300 U/mL | 1.62 | 1.20–2.19 | 0.001 | |||
| Postop CA19-9 >37 U/mL | 1.64 | 1.25–2.16 | <0.001 | 1.94 | 1.36–2.77 | <0.001 |
| CA19-9 status | <0.001 | |||||
| Normal CA19-9 | Ref. | |||||
| Normalization | 0.90 | 0.67–1.22 | 0.512 | |||
| Non-normalization | 1.75 | 1.27–2.40 | 0.001 | |||
| Liver resection type | 0.312 | |||||
| RH or ERH | Ref. | |||||
| LH or ELH | 0.90 | 0.67–1.21 | 0.478 | |||
| LTS | 1.11 | 0.64–1.92 | 0.708 | |||
| RTS | 1.21 | 0.66–2.24 | 0.539 | |||
| CBS | 3.78 | 0.93–15.33 | 0.063 | |||
| Portal vein resection | 1.52 | 1.09–2.12 | 0.014 | |||
| Intraoperative transfusion | 1.51 | 1.17–1.96 | 0.002 | 1.74 | 1.22–2.48 | 0.002 |
| R1 resection | 1.02 | 0.90–1.15 | 0.756 | |||
| Size (cm) | 1.07 | 0.99–1.15 | 0.089 | |||
| Poorly differentiated | 1.27 | 0.86–1.87 | 0.226 | |||
| Portal vein invasion | 1.88 | 1.35–2.61 | <0.001 | |||
| Lymphovascular invasion | 1.71 | 1.33–2.21 | <0.001 | |||
| Perineural invasion | 1.43 | 1.01–2.04 | 0.046 | |||
| LN metastasis | 2.02 | 1.56–2.60 | <0.001 | 2.07 | 1.45–2.97 | <0.001 |
| T stage (T3,4 vs. T1,2) | 1.83 | 1.40–2.40 | <0.001 | 1.67 | 1.16–2.41 | 0.006 |
| Adjuvant chemotherapy | 1.36 | 1.06–1.76 | 0.016 | |||
| Adjuvant radiotherapy | 1.42 | 1.06–1.90 | 0.019 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.W.; Lee, J.H.; Park, Y.; Kwon, J.; Lee, W.; Song, K.B.; Hwang, D.W.; Kim, S.C. Prognostic Impact of Perioperative CA19-9 Levels in Patients with Resected Perihilar Cholangiocarcinoma. J. Clin. Med. 2021, 10, 1345. https://doi.org/10.3390/jcm10071345
Lee JW, Lee JH, Park Y, Kwon J, Lee W, Song KB, Hwang DW, Kim SC. Prognostic Impact of Perioperative CA19-9 Levels in Patients with Resected Perihilar Cholangiocarcinoma. Journal of Clinical Medicine. 2021; 10(7):1345. https://doi.org/10.3390/jcm10071345
Chicago/Turabian StyleLee, Jong Woo, Jae Hoon Lee, Yejong Park, Jaewoo Kwon, Woohyung Lee, Ki Byung Song, Dae Wook Hwang, and Song Cheol Kim. 2021. "Prognostic Impact of Perioperative CA19-9 Levels in Patients with Resected Perihilar Cholangiocarcinoma" Journal of Clinical Medicine 10, no. 7: 1345. https://doi.org/10.3390/jcm10071345
APA StyleLee, J. W., Lee, J. H., Park, Y., Kwon, J., Lee, W., Song, K. B., Hwang, D. W., & Kim, S. C. (2021). Prognostic Impact of Perioperative CA19-9 Levels in Patients with Resected Perihilar Cholangiocarcinoma. Journal of Clinical Medicine, 10(7), 1345. https://doi.org/10.3390/jcm10071345








