Daily Sitting for Long Periods Increases the Odds for Subclinical Atheroma Plaques
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Subclinical Atherosclerosis Imaging
2.3. Physical Activity and Sedentary Assessment
2.4. Demographic, Clinical, and Biochemical Characteristics
2.5. Statistical Analysis
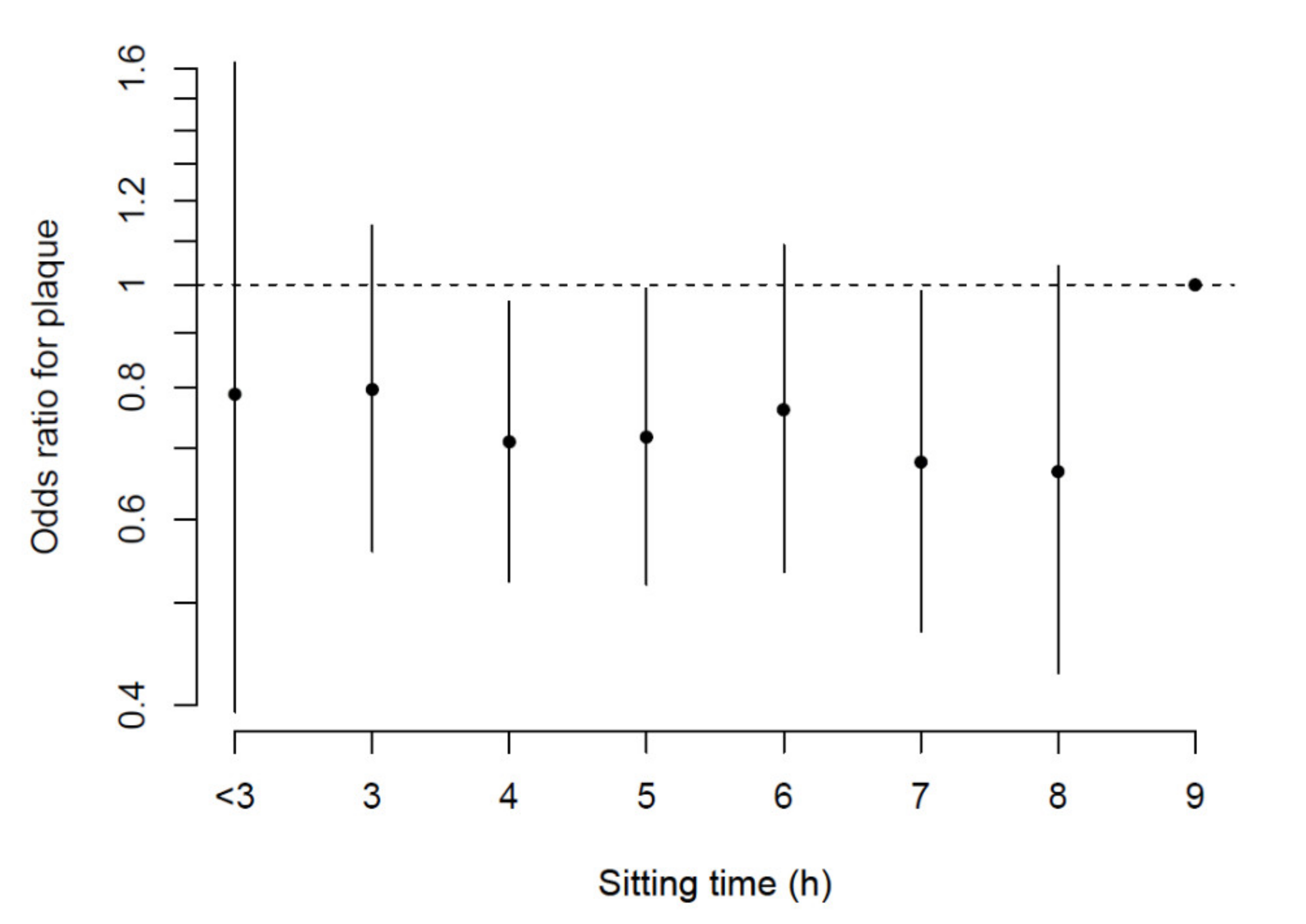
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Herrington, W.; Lacey, B.; Sherliker, P.; Armitage, J.; Lewington, S. Epidemiology of Atherosclerosis and the Potential to Reduce the Global Burden of Atherothrombotic Disease. Circ. Res. 2016, 118, 535–546. [Google Scholar] [CrossRef]
- Ford, E.S.; Caspersen, C.J. Sedentary behaviour and cardiovascular disease: A review of prospective studies. Int. J. Epidemiol. 2012, 41, 1338–1353. [Google Scholar] [CrossRef]
- Hamilton, M.T.; Hamilton, D.G.; Zderic, T.W. Role of Low Energy Expenditure and Sitting in Obesity, Metabolic Syndrome, Type 2 Diabetes, and Cardiovascular Disease. Diabetes 2007, 56, 2655–2667. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.T.; Healy, G.N.; Dunstan, D.W.; Theodore, W.; Owen, N. Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Curr. Cardiovasc. Risk Rep. 2008, 2, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.; Bauman, A.; Lee, I.-M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Impact of physical inactivity on the world´s major non-communicable diseases. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Fórnias, L.; De Rezende, M.; De Sá, T.H.; Mielke, G.I.; Yukari, J.; Viscondi, K.; PabloRey-López, J.; Garcia, L.M.T. All-Cause Mortality Attributable to Sitting Time: Analysis of 54 countries worldwide. Am. J. Prev. Med. 2016, 51, 253–263. [Google Scholar]
- Caruso, M.V.; Serra, R.; Perri, P.; Buffone, G.; Caliò, F.G.; De Franciscis, S.; Fragomeni, F. A computational evaluation of sedentary lifestyle effects on carotid hemodynamics and atherosclerotic events incidence. Acta Bioeng. Biomech. 2017, 19, 42–52. [Google Scholar] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; De Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef] [PubMed]
- Howard, B.J.; Balkau, B.; Thorp, A.; Magliano, D.J.; Shaw, J.; Owen, N.; Dunstan, D.W. Associations of overall sitting time and TV viewing time with fibrinogen and C reactive protein: The AusDiab study. Br. J. Sports Med. 2014, 49, 255–258. [Google Scholar] [CrossRef]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur. Hear. J. 2011, 32, 590–597. [Google Scholar] [CrossRef] [PubMed]
- León-Latre, M.; Moreno-Franco, B.; Andrés-Esteban, E.M.; Ledesma, M.; Laclaustra, M.; Alcalde, V.; Peñalvo, J.L.; Ordovás, J.M.; Casasnovas, J.A. Sedentary Lifestyle and Its Relation to Cardiovascular Risk Factors, Insulin Resistance and Inflammatory Profile. Rev. Esp. Cardiol. 2014, 67, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Lazaros, G.; Oikonomou, E.; Vogiatzi, G.; Christoforatou, E.; Tsalamandris, S.; Goliopoulou, A.; Tousouli, M.; Mystakidou, V.; Chasikidis, C.; Tousoulis, D. The impact of sedentary behavior patterns on carotid atherosclerotic burden: Implications from the Corinthia epidemiological study. Atherosclerosis 2019, 282, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Walker, T.J.; Heredia, N.I.; Lee, M.; Laing, S.T.; Fisher-Hoch, S.P.; McCormick, J.B.; Reininger, B.M. The combined effect of physical activity and sedentary behavior on subclinical atherosclerosis: A cross-sectional study among Mexican Americans. BMC Public Heal. 2019, 19, 1–11. [Google Scholar] [CrossRef]
- Parsons, T.J.; Sartini, C.; Ellins, E.A.; Halcox, J.P.; Smith, K.E.; Ash, S.; Lennon, L.T.; Wannamethee, S.G.; Lee, I.-M.; Whincup, P.H.; et al. Objectively measured physical activity, sedentary time and subclinical vascular disease: Cross-sectional study in older British men. Prev. Med. 2016, 89, 194–199. [Google Scholar] [CrossRef]
- Casasnovas, J.A.; Alcalde, V.; Civeira, F.; Guallar, E.; Ibañez, B.; Jimenez Borreguero, J.; Laclaustra, M.; León, M.; Peñalvo, J.L.; Ordovás, J.M.; et al. Aragon workers’ health study—Design and cohort description. BMC Cardiovasc. Disord. 2012, 12, 1–11. [Google Scholar] [CrossRef]
- Muntendam, P.; McCall, C.; Sanz, J.; Falk, E.; Fuster, V. The BioImage Study: Novel approaches to risk assessment in the primary prevention of atherosclerotic cardiovascular disease—study design and objectives. Am. Hear. J. 2010, 160, 49–57. [Google Scholar] [CrossRef]
- Junyent, M.; Gilabert, R.; Zambón, D.; Pocoví, M.; Mallén, M.; Cofán, M.; Núñez, I.; Civeira, F.; Tejedor, D.; Ros, E. Femoral Atherosclerosis in Heterozygous Familial Hypercholesterolemia. Arter. Thromb. Vasc. Biol. 2008, 28, 580–586. [Google Scholar] [CrossRef]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: A meta-analysis. Atherosclerosis 2012, 220, 128–133. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; López-Fontana, C.; Varo, J.J.; Sánchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Heal. Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef]
- Chasan-Taber, S.; Rimm, E.B.; Stampfer, M.J.; Spiegelman, D.; Colditz, G.A.; Giovannucci, E.; Ascherio, A.; Willett, W.C. Reproducibility and Validity of a Self-Administered Physical Avtivity Questionnaire for Male Health Professionals. Epidemiology 1996, 7, 81–86. [Google Scholar] [CrossRef]
- Wolf, A.M.; Hunter, D.J.; Colditz, G.; Manson, J.; Stampfer, M.J.; Corsano, K.; Rosner, B.; Kriska, A.; Willett, W.C. Reproducibility and Validity of a Self-Administered Physical Activity Questionnaire. Int. J. Epidemiol. 1994, 23, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-locke, C.; Greer, J.L.; Vezina, J.; Whitt-glover, M.C.; Leon, A.S. Compendium of Physical Activities: A Second Update of Codes and MET Values. Med Sci Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, Without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.A.; Palaniappan, L.P.; Artinian, N.T.; Carnethon, M.R.; Criqui, M.H.; Daniels, S.R.; Fonarow, G.C.; Fortmann, S.P.; Franklin, B.A.; Galloway, J.M.; et al. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 Update: A scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation 2013, 127, 1730–1753. [Google Scholar] [CrossRef] [PubMed]
- National Cholesterol Education Program (US); Expert Panel on Detection; Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Sillesen, H.; Sartori, S.; Sandholt, B.; Baber, U.; Mehran, R.; Fuster, V. Carotid plaque thickness and carotid plaque burden predict future cardiovascular events in asymptomatic adult Americans. Eur. Hear. J. Cardiovasc. Imaging 2018, 19, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting Time, Physical Activity, and Risk of Mortality in Adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.; Bauman, A.; Lee, I.-M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br. J. Sports Med. 2019, 53, 886–894. [Google Scholar] [CrossRef]
- Blasco-Colmenares, E.; Moreno-Franco, B.; Latre, M.L.; Mur-Vispe, E.; Pocovi, M.; Jarauta, E.; Civeira, F.; Laclaustra, M.; Casasnovas, J.A.; Guallar, E. Sleep duration and subclinical atherosclerosis: The Aragon Workers’ Health Study. Atherosclerosis 2018, 274, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Laclaustra, M.; Casasnovas, J.A.; Fernández-Ortiz, A.; Fuster, V.; León-Latre, M.; Jiménez-Borreguero, L.J.; Pocovi, M.; Hurtado-Roca, Y.; Ordovas, J.M.; Jarauta, E.; et al. Femoral and carotid subclinical atherosclerosis association with risk factors and coronary calcium: The AWHS study. J. Am. Coll. Cardiol. 2016, 67, 1263–1274. [Google Scholar] [CrossRef] [PubMed]
- Vanderlaan, P.A.; Reardon, C.A.; Getz, G.S. Site Specificity of Atherosclerosis. Site-Selective Responses to Atherosclerotic Modulators. Arter. Thromb. Vasc. Biol. 2004, 24, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Gemignani, T.; Azevedo, R.C.; Higa, C.M.; Coelho, O.R.; Matos-Souza, J.R.; Nadruz, W. Increased popliteal circumferential wall tension induced by orthostatic body posture is associated with local atherosclerotic plaques. Atherosclerosis 2012, 224, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Papaharilaou, Y.; Aristokleous, N.; Seimenis, I. Effect of head posture on the healthy human carotid bifurcation hemodynamics. Med. Biol. Eng. Comput. 2013, 51, 207–218. [Google Scholar] [CrossRef]
- Gemignani, T.; Matos-souza, J.R.; Coelho, O.R.; Franchini, K.G.; Nadruz, W. Postural changes may influence popliteal atherosclerosis by modifying local circumferential wall tension. Hypertens. Res. 2008, 31, 2059–2064. [Google Scholar] [CrossRef]
- Owen, N.; Healy, N.; Matthews, C.E.; Dunstan, D.W. Too Much Sitting: The Population Health Science of Sedentary Behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.; Altenburg, T.M.; Chinapaw, M.J. On Behalf of Sbrn Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.T.; Hamilton, D.G.; Zderic, T.W. Exercise Physiology versus Inactivity Physiology: An Essential Concept for Understanding Lipoprotein Lipase Regulation. Exerc. Sport Sci. Rev. 2004, 32, 161–166. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall | <9 h/day | ≥9 h/day | p-Value |
|---|---|---|---|---|
| n | 2082 | 1554 | 528 | |
| Age, years | 50.9 (3.9) | 50.8 (3.9) | 51.0 (3.9) | 0.353 |
| BMI, kg/m2 | 27.6 (3.3) | 27.5 (3.2) | 28.0 (3.4) | 0.007 |
| Waist circumference, cm | 97.3 (8.9) | 96.9 (8.8) | 98.4 (8.8) | 0.001 |
| Systolic blood pressure, mmHg | 125.4 (13.9) | 125.4 (14.0) | 125.4 (13.7) | 0.941 |
| Diastolic blood pressure, mmHg | 82.4 (9.4) | 82.4 (9.5) | 82.4 (9.2) | 0.899 |
| Total cholesterol, mg/dL | 220.1 (36.4) | 220.9 (36.5) | 217.7 (36.1) | 0.084 |
| HDL-c, mg/dL | 53.0 (11.4) | 53.2 (11.3) | 52.6 (11.5) | 0.299 |
| Non-HDL-c, mg/dL | 167.1 (35.2) | 167.7 (35.2) | 165.1 (35.3) | 0.146 |
| LDL-c, mg/dL | 137.9 (31.4) | 138.8 (31.2) | 135.4 (31.8) | 0.034 |
| Triglycerides, mg/dL | 150.1 (97.1) | 148.8 (97.1) | 153.9 (97.1) | 0.303 |
| Glucose, mg/dL | 97.7 (17.5) | 97.4 (16.5) | 98.8 (20.1) | 0.092 |
| Hypertension, % | 37.5 (781) | 37.3 (580) | 38.1 (201) | 0.760 |
| Dyslipidemia, % | 49.2 (1025) | 48.8 (758) | 50.6 (267) | 0.477 |
| Diabetes, % | 5.6 (117) | 5.1 (79) | 7.2 (38) | 0.076 |
| Ever smokers, % | 77.1 (1606) | 76.9 (1195) | 77.8 (411) | 0.655 |
| Different Models in the Analyzed Territories | Sitting Time | p-Value | |
|---|---|---|---|
| <9 h/day | ≥9 h/day | ||
| Number with carotid plaque/Total | 550/1554 | 214/528 | |
| Age-adjusted | 1.00 (ref) | 1.23 (0.99, 1.51) | 0.051 |
| Multivariable-adjusted 1 | 1.00 (ref) | 1.24 (1.00, 1.53) | 0.047 |
| Multivariable-adjusted 2 | 1.00 (ref) | 1.25 (1.01, 1.55) | 0.037 |
| Number with femoral plaque/Total | 868/1554 | 313/528 | |
| Age-adjusted | 1.00 (ref) | 1.13 (0.92, 1.39) | 0.231 |
| Multivariable-adjusted 1 | 1.00 (ref) | 1.14 (0.92, 1.42) | 0.237 |
| Multivariable-adjusted 2 | 1.00 (ref) | 1.16 (0.93, 1.45) | 0.175 |
| Number with plaque in any territory/Total | 1020/1554 | 380/528 | |
| Age-adjusted | 1.00 (ref) | 1.33 (1.07, 1.67) | 0.010 |
| Multivariable-adjusted 1 | 1.00 (ref) | 1.35 (1.07, 1.71) | 0.010 |
| Multivariable-adjusted 2 | 1.00 (ref) | 1.38 (1.09, 1.74) | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez-Lasierra, J.L.; Laclaustra, M.; Guallar-Castillón, P.; Casasnovas, J.A.; Casajús, J.A.; Jarauta, E.; Gonzalez-Agüero, A.; Moreno-Franco, B. Daily Sitting for Long Periods Increases the Odds for Subclinical Atheroma Plaques. J. Clin. Med. 2021, 10, 1229. https://doi.org/10.3390/jcm10061229
Perez-Lasierra JL, Laclaustra M, Guallar-Castillón P, Casasnovas JA, Casajús JA, Jarauta E, Gonzalez-Agüero A, Moreno-Franco B. Daily Sitting for Long Periods Increases the Odds for Subclinical Atheroma Plaques. Journal of Clinical Medicine. 2021; 10(6):1229. https://doi.org/10.3390/jcm10061229
Chicago/Turabian StylePerez-Lasierra, Jose Luis, Martin Laclaustra, Pilar Guallar-Castillón, Jose Antonio Casasnovas, Jose Antonio Casajús, Estibaliz Jarauta, Alejandro Gonzalez-Agüero, and Belen Moreno-Franco. 2021. "Daily Sitting for Long Periods Increases the Odds for Subclinical Atheroma Plaques" Journal of Clinical Medicine 10, no. 6: 1229. https://doi.org/10.3390/jcm10061229
APA StylePerez-Lasierra, J. L., Laclaustra, M., Guallar-Castillón, P., Casasnovas, J. A., Casajús, J. A., Jarauta, E., Gonzalez-Agüero, A., & Moreno-Franco, B. (2021). Daily Sitting for Long Periods Increases the Odds for Subclinical Atheroma Plaques. Journal of Clinical Medicine, 10(6), 1229. https://doi.org/10.3390/jcm10061229








