Abstract
Background: Critically ill patients with COVID-19 are prone to develop severe acute kidney injury (AKI), defined as KDIGO (Kidney Disease Improving Global Outcomes) stages 2 or 3. However, data are limited in these patients. We aimed to report the incidence, risk factors, and prognostic impact of severe AKI in critically ill patients with COVID-19 admitted to the intensive care unit (ICU) for acute respiratory failure. Methods: A retrospective monocenter study including adult patients with laboratory-confirmed severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection admitted to the ICU for acute respiratory failure. The primary outcome was to identify the incidence and risk factors associated with severe AKI (KDIGO stages 2 or 3). Results: Overall, 110 COVID-19 patients were admitted. Among them, 77 (70%) required invasive mechanical ventilation (IMV), 66 (60%) received vasopressor support, and 9 (8.2%) needed extracorporeal membrane oxygenation (ECMO). Severe AKI occurred in 50 patients (45.4%). In multivariable logistic regression analysis, severe AKI was independently associated with age (odds ratio (OR) = 1.08 (95% CI (confidence interval): 1.03–1.14), p = 0.003), IMV (OR = 33.44 (95% CI: 2.20–507.77), p = 0.011), creatinine level on admission (OR = 1.04 (95% CI: 1.008–1.065), p = 0.012), and ECMO (OR = 11.42 (95% CI: 1.95–66.70), p = 0.007). Inflammatory (interleukin-6, C-reactive protein, and ferritin) or thrombotic (D-dimer and fibrinogen) markers were not associated with severe AKI after adjustment for potential confounders. Severe AKI was independently associated with hospital mortality (OR = 29.73 (95% CI: 4.10–215.77), p = 0.001) and longer hospital length of stay (subhazard ratio = 0.26 (95% CI: 0.14–0.51), p < 0.001). At the time of hospital discharge, 74.1% of patients with severe AKI who were discharged alive from the hospital recovered normal or baseline renal function. Conclusion: Severe AKI was common in critically ill patients with COVID-19 and was not associated with inflammatory or thrombotic markers. Severe AKI was an independent risk factor of hospital mortality and hospital length of stay, and it should be rapidly recognized during SARS-CoV-2 infection.
1. Introduction
Since late 2019, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) implicated in COVID-19 has infected millions of people all around the world, with hundreds of thousands of deaths [1]. The disease has resulted in a large number of hospitalizations, respiratory failure, and intensive care unit (ICU) admissions. The hospitals in most metropolitan areas have experienced a rapid surge in COVID-19 admissions, with significant mortality [2].
An alarming number of patients also developed acute kidney injury (AKI). Indeed, AKI in patients with COVID-19 infection is reported to range between 6.5% and 46% [2,3,4,5], with the highest ranges in the critically ill (23%–81%) [3,4,5,6,7,8,9,10,11,12]. Differences in the incidence of AKI have resulted from the various definitions of AKI used and the populations studied. Furthermore, AKI has been linked with a higher mortality worldwide [13].
The pathophysiology of AKI related to COVID-19 is incompletely elucidated. Several mechanisms have been suggested to be involved in COVID-19-associated AKI. SARS-CoV-2 can directly injure the tubular cells by binding to the angiotensin-converting enzyme 2 receptors expressed in high amounts in the kidneys’ proximal tubular cells and podocytes [14,15,16,17,18], thus leading to AKI. Severe COVID-19 is also known to cause the excessive release of inflammatory cytokines with high levels of interleukin 6 (IL-6) and maladaptive immune responses [19], thus leading to intrarenal inflammation, increased vascular permeability, and alterations of kidney microcirculation that result in renal hypoperfusion [17,18,20]. Furthermore, a high incidence of acute thrombotic events has been reported in COVID-19 patients [21,22,23]. The presence of fibrin thrombi in the kidney in autopsy findings of patients who died from COVID-19 [24] is in favor of abnormal coagulation that might induce renal microcirculatory dysfunction and AKI.
Data focusing on severe AKI (Kidney Disease Improving Global Outcomes (KDIGO) stages 2 or 3) in ICU are still scarce. Additionally, there have been no reports regarding AKI in patients with COVID-19 admitted to the ICU in the United Arab Emirates (United Arab Emirates). We decided to review our data to analyze the incidence of severe AKI, its predictors, and its association with mortality in critically ill COVID-19 patients in the ICU at Cleveland Clinic Abu Dhabi.
2. Methods
This retrospective study was approved by the institutional Ethics Committee of Cleveland Clinic Abu Dhabi on June 8th, 2020 (REC number: A-2020–055) and waived the need for informed consent due to the study’s retrospective nature.
All adult patients (age ≥ 18 years) admitted to our ICU between 1 March and 29 May 2020 with confirmed SARS-CoV-2 infection (virus detected by a real-time reverse-transcriptase–polymerase-chain-reaction assay of a nasopharyngeal sample) and acute respiratory failure requiring high-flow nasal oxygen therapy or mechanical ventilation were included in this study.
2.1. Definition of AKI
AKI was defined according to both urinary output and serum creatinine KDIGO criteria [25] as follows: stage 1: increase in serum creatinine by 26.5 µmol.L−1 within 48 h, a 1.5–1.9 times baseline value of serum creatinine, or urinary output < 0.5 mL.kg1.h−1 for 6–12 h within 7 days; stage 2: 2.0–2.9 times baseline value of serum creatinine or urinary output < 0.5 mL.kg−1.h−1 for ≥ 12 h within 7 days; stage 3: ≥ 3 times baseline value of serum creatinine or to ≥ 353.6 µmol.L−1, the initiation of renal replacement therapy (RRT), or urinary output < 0.3 mL.kg−1.h−1 for ≥24 h or anuria for ≥12 h within 7 days. Baseline creatinine was defined as the best value in the 3 preceding months, or, if unavailable, we used the serum creatinine on the day of hospital admission as the baseline serum creatinine.
2.2. Clinical and Laboratory Data
Data on baseline characteristics—including demographics, physiological variables, the presence of medical comorbidities; Sequential Organ Failure Assessment (SOFA) and Simplified Acute Physiology Score (SAPS) II scores; and laboratory values including oxygenation parameters, full blood count, coagulation parameters, and inflammatory markers (C-reactive protein, IL-6, and ferritin)—were collected on admission to the ICU. Data on the use of invasive mechanical ventilation, vasopressors, renal replacement therapy, extracorporeal membrane oxygenation, and other treatments were collected. Ventilatory variables including plateau pressure (Pplat), total positive end-expiratory pressure (PEEP), tidal volume, and driving pressure (Pplat-PEEP) were also captured. The time from symptoms onset to ICU admission was also calculated. Patients were categorized according to whether they developed AKI stages 2 and 3 or no AKI and AKI stage 1 during the ICU stay.
2.3. Outcome Measures
The primary outcome was to identify the incidence and risk factors associated with the occurrence of severe AKI (KDIGO stages 2 or 3).
Prespecified secondary outcomes were the associations between severe AKI and all-cause hospital mortality, ICU length of stay, hospital length of stay, and mechanical ventilation duration.
3. Statistical Analysis
The normality of data distribution was assessed using the Shapiro–Wilk test and visually checking each variable’s distribution (histogram). Data are expressed as mean ± SD when normally distributed or as median (interquartile range (IQR)) when non-normally distributed. Proportions were used as descriptive statistics for categorical variables. Comparisons of values between independent groups were performed by the 2-tailed Student t test or the Mann–Whitney U test, as appropriate. The analysis of the discrete data was performed by χ2 test or Fisher exact test when the numbers were small. There were missing data (missing at random) for IL-6 (3.6%), ferritin (1.8%), D-dimer (1%), and fibrinogen (8.2%) that were not imputed.
Independent risk factors of AKI stages 2 and 3 were assessed using multivariable logistic regression analysis. Variables associated with AKI stages 2 and 3 (p < 0.1) in univariate analysis were included in the model. To respect the rule of 5–9 events per variable in logistic regression [26], we selected the model with less than 10 events per variable that had the lower Akaike information criteria (AIC) and Bayesian information criteria (BIC) values. The potential problem of co-linearity was evaluated using Spearman or Pearson correlation coefficient before running the analysis. The goodness of fit of the model was assessed using Hosmer–Lemeshow test.
Logistic regression analysis was also used to assess whether severe AKI (stages 2 or 3) was independently associated with hospital mortality. As sensitivity analyses, we evaluated if severe AKI was associated with hospital mortality in different models with less than 10 events per variable [26] by keeping age, severity score, and comorbidity variables in each model. Cox proportional hazards regression analysis was also used to assess whether severe AKI was independently associated with time-to-hospital death. Variables associated with hospital mortality (p < 0.1) in univariate analysis were included in the Cox model. The proportional hazards assumption was checked based on the scaled Schoenfeld residuals.
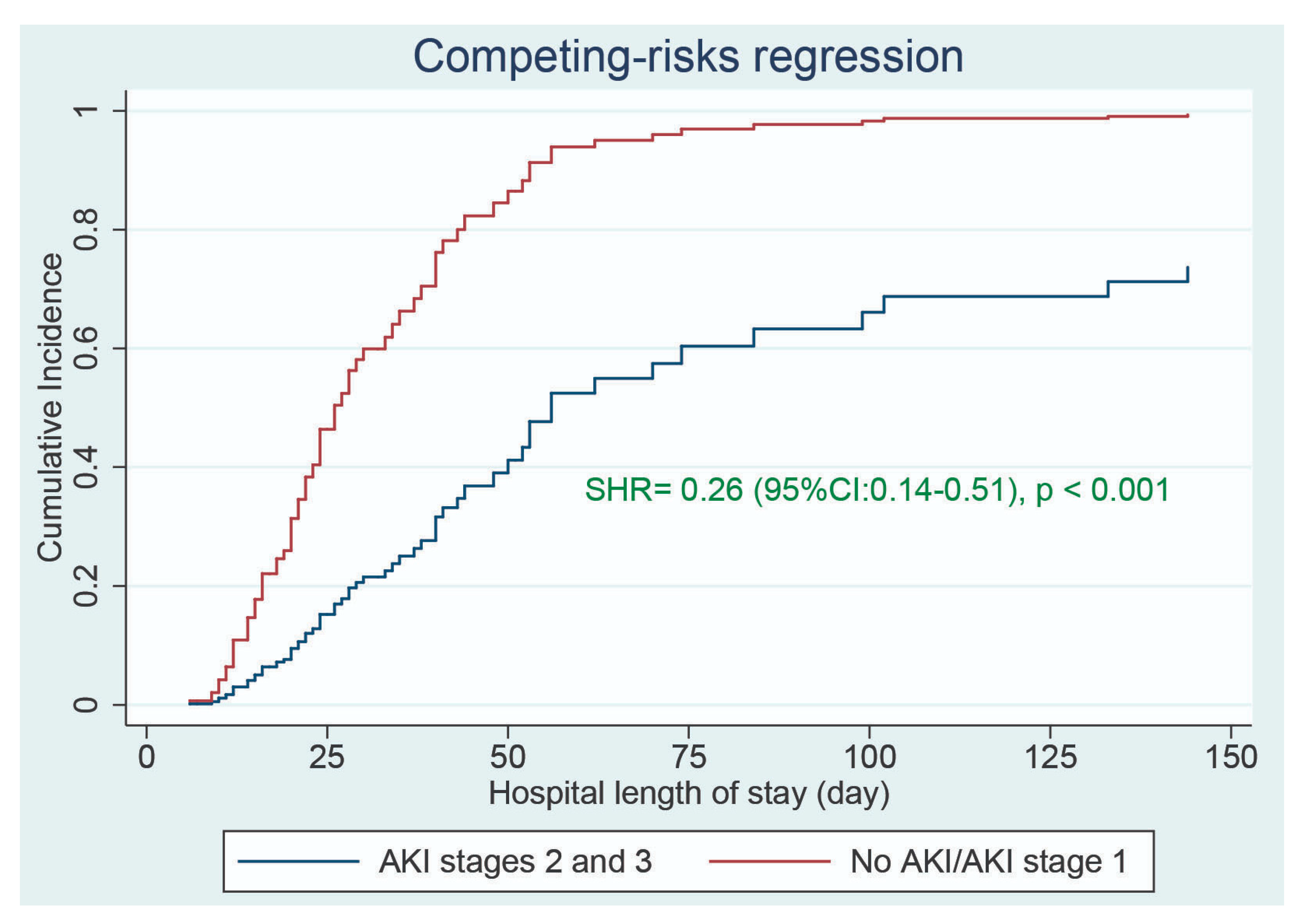
The association between severe AKI (stages 2 or 3) and hospital length of stay was evaluated using the competing-risks regression proportional sub hazards analysis based on the method of Fine and Gray. Death before hospital discharge was considered the competing event, and time-to-event analysis was right-censored at hospital discharge. Adjusted competing-risks regression models were fitted to identify whether severe AKI was independently associated with time-to-hospital discharge.
A value of p < 0.05 was considered statistically significant, and all reported p values are two-sided. Robust standard errors were used to calculate the 95% confidence intervals (CIs) for odds ratios (ORs), hazards ratios (HRs), and subhazard ratios (SHRs). Statistical analyses were performed using Stata/SE 14.2 software for Windows (Stata Corp LLC., College Station, TX, USA).
4. Results
4.1. Study Population
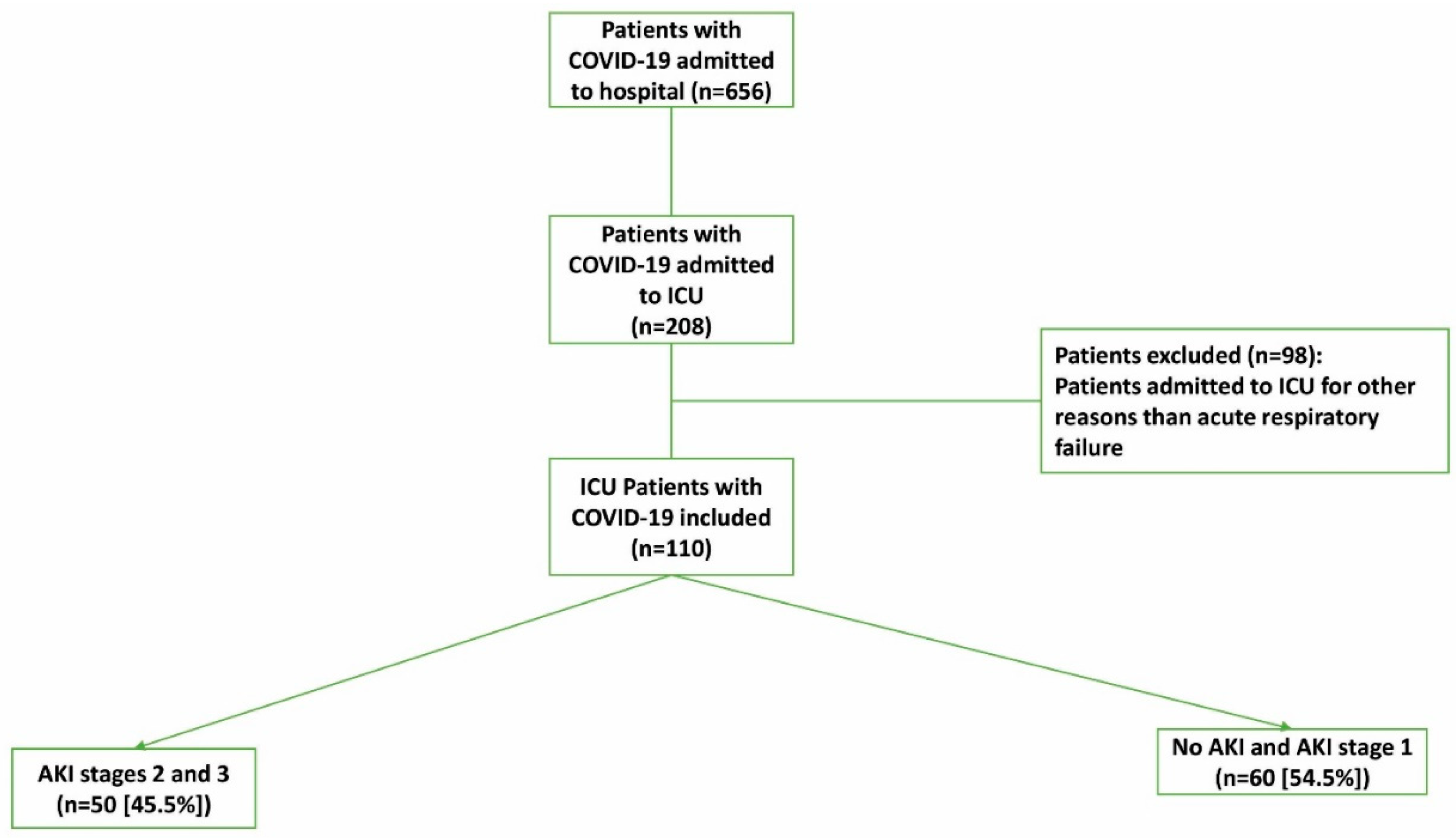
From 1 March to 29 May 2020, 110 adult patients with acute respiratory failure caused by COVID-19 infection were admitted to the ICU and included in this study (Figure 1). The main characteristics of the cohort are summarized in Table 1. The median age among all patients was 50 years (IQR: 41–59 years), and 98 (89.1%) were men. Among the patients, 65 (59.1%) had at least one comorbidity, 77 (70.0%) received invasive mechanical ventilation, and 66 (60.0%) required vasopressor support. The median time from symptoms onset to ICU admission was 5 days (IQR: 3–7 days).
Figure 1.
Flow chart of COVID-19 patients admitted to the intensive care unit (ICU). AKI: acute kidney injury.

Table 1.
Comparisons of baseline characteristics, laboratory data, and treatments during ICU stay between severe AKI (stage 2 and 3) and AKI stage 1 and no-AKI groups.
Fifty patients (45.4%) developed severe AKI (stage 2 or 3), and 60 (54.5%) had no AKI (46.4%) or AKI stage 1 (8.2%); see Table 1. The median time from ICU admission to AKI occurrence was 0 days (IQR: 0–7 days). Among patients who developed severe AKI (stages 2 or 3), 27 (54%) required renal replacement therapy. The median time from ICU admission to renal replacement therapy was 2 days (IQR: 0–9 days).
Patients in the severe AKI group were older and had a higher rate of comorbidities, higher severity scores, and lower a mean arterial pressure on ICU admission than the other group (Table 1). Regarding laboratory data on ICU admission, only leucocyte, D-dimer, and creatinine levels were significantly higher in the severe AKI group than in the other group (Table 1). IL-6, C-reactive protein, ferritin, and fibrinogen levels did not significantly differ between the two groups (Table 1). Urine output and fluid balance were not significantly different between the two groups. The treatments received in the ICU (invasive mechanical ventilation, vasopressors, diuretics, and extracorporeal membrane oxygenation) were significantly higher in the severe AKI group (Table 1). The other treatments did not differ significantly between the two groups.
4.2. Primary Outcome
In univariate analysis (without adjustment), age, comorbidities (diabetes mellitus, hypertension, and chronic kidney disease), severity scores (SOFA and SAPS II), mean arterial pressure, leucocyte count, D-dimer, creatinine on admission, vasopressor use, invasive mechanical ventilation, and extracorporeal membrane oxygenation were found to be associated (p < 0.1) with severe AKI (Table 1). In the multivariable logistic regression analysis, after including the variables mentioned above, age, creatinine level on ICU admission, the use of invasive mechanical ventilation, and extracorporeal membrane oxygenation were independently associated with the development of severe AKI stages (Supplementary Table S1). Instead of SAPS II, SOFA score was included in the model because of the collinearity between the two variables (r = 0.73, p < 0.001). However, including SAPS II instead of the SOFA score resulted in the same findings (results not shown). Table 2 shows the logistic regression model with the lowest AKI and BIC values, including less than nine events per variable. The same variables (age, admission creatinine, invasive mechanical ventilation, and extracorporeal membrane oxygenation) were found as risk factors for severe AKI development.

Table 2.
Factors associated with severe AKI (stages 2 and 3) in multivariable logistic regression analysis.
4.3. Secondary Outcomes
Overall, 27 patients (24.5%) died in the hospital. Among them, 23 patients (46%) were in the severe AKI group, and only 4 (6.7%) were in the other group (p < 0.001). In univariate analysis, age, comorbidities (hypertension), SAPS II, leucocyte count, platelet count, ferritin, PaO2/FiO2 ratio, lactate levels, severe AKI, vasopressor use, invasive mechanical ventilation, extracorporeal membrane oxygenation, and hydroxychloroquine were found to be associated (p < 0.1) with hospital mortality (Table 3). In the multivariable logistic regression analysis, after adjusting for the above confounder variables, severe AKI was found to be independently associated with a higher hospital mortality (OR = 29.7 (95% CI: 4.10–215.8), p = 0.001); see Table 4. After a sensitivity analysis, we found that severe AKI was still independently associated with hospital mortality in the different models that included less than 10 events per variable (Supplementary File, Tables S3–S12). We did not adjust p-values for multiple comparisons because they were considered to be exploratory analyses. Severe AKI was also associated with time-to-hospital death in univariate analysis (HR = 4.25 (95% CI: 1.47–12.30), p = 0.008). However, after adjusting for confounding variables, severe AKI was no longer associated with time-to-hospital death (HR = 4.00 (95% CI: 0.80–20.00), p = 0.09); see Table 5.

Table 3.
Comparisons of baseline characteristics, laboratory data, and treatments during ICU stay between survival and death groups.

Table 4.
Factors associated with hospital mortality (multivariable logistic regression analysis).

Table 5.
Factors associated with hospital mortality (multivariable Cox regression analysis).
Hospital length of stay (31 days (IQR: 19–51 days) vs. 19 days (IQR: 12–28 days), p = 0.002), ICU length of stay (21 days (IQR: 4–35 days) vs. 9 days (IQR: 6–17 days), p < 0.001), and duration of mechanical ventilation (21 days (IQR: 10–37 days) vs. 11 days (IQR: 8–15 days), p = 0.002) were significantly longer in the severe AKI group than in the other group. In the multivariable competing-risks regression analysis, after adjusting for confounding variables, severe AKI was independently associated with a longer hospital length of stay (SHR = 0.26 (95% CI: 0.14–0.51), p < 0.001); see Figure 2 and Supplementary Table S13.
Figure 2.
Comparisons of cumulative incidence function of hospital discharge between patients who had severe AKI (KDIGO stages 2 and 3) and those who did not. SHR: subhazard ratio.
Among the 50 patients with severe AKI, 27 (54%) were discharged alive from the hospital. At hospital discharge, 20 of 27 (74.1%) recovered normal or baseline renal function.
5. Discussion
In this study of critically ill patients with COVID-19 and acute respiratory failure, the incidence of severe AKI was 45.4%. Age, creatinine level on admission, invasive mechanical ventilation, and extracorporeal membrane oxygenation were associated with severe AKI development. Furthermore, severe AKI was associated with a higher hospital mortality rate and a longer hospital length of stay.
The reported incidence of overall AKI using KDIGO definition in critically ill patients admitted to the ICU ranged from 50% to 81% [3,4,8,10,11]. In a retrospective study of 100 COVID-19 patients admitted to the ICU, Joseph et al. found a 37% incidence of severe AKI (stages 2 and 3) [8]. Other studies showed severe AKI incidence ranging from 40.6% to 57.4% in COVID-19 ICU patients [3,4,10,11]. We found a 45.5% incidence of severe AKI. The differences in the reported incidence rates of severe AKI might be explained by differences in severity of COVID-19 patients and the different methods/definitions used to estimate missing baseline creatinine, which can lead to disparities in the incidence of AKI of up to 15% [27]. Additionally, our incidence rate of patients requiring renal replacement therapy was higher (24.5%) than that reported in the studies of Joseph et al., Doher et al., and Fominskiy et al. (13%, 16.9%, and 17.7%, respectively) [8,10,11], but it was in line with other reports ranging between 20.4% and 31% [3,4,12,28].
The risk factors of developing AKI vary between studies [3,4,8,10]. Hirsch et al. found that older age, the presence of comorbidities (hypertension, diabetes, and cardiovascular disease), and the need for invasive mechanical ventilation and vasopressor medications were independently associated with AKI in a large population of patients hospitalized with COVID-19 (n = 5449) in metropolitan New York [4]. In a retrospective study of patients admitted to the hospital with COVID-19, Chan et al. observed that chronic kidney disease, male gender, and admission potassium were independent predictors of severe AKI (stage 3) [3]. In ICU patients with COVID-19, only chronic kidney disease and modified SOFA score on admission were independently associated with AKI occurrence [8]. In critically ill patients with COVID-19 admitted to the ICU, the use of diuretics, invasive mechanical ventilation, and creatinine level on admission were independently associated with AKI [10]. In our study, the use of invasive mechanical ventilation, age, creatinine level on admission, and extracorporeal membrane oxygenation were associated with the development of severe AKI (stages 2 and 3). The most common predictors of AKI across all those studies were older age, comorbidities (specifically hypertension and chronic kidney disease), and the need for invasive mechanical ventilation.
COVID-19 has been characterized by elevated cytokine levels (cytokine storm) and a hyperinflammatory state induced by SARS-CoV-2 infection [18,29]. High levels of IL-6 were found to be associated with the development of severe COVID-19 infection and mortality [30,31]. It can be assumed that IL-6 may contribute to AKI in COVID-19 patients by inducing endothelial and tubular dysfunction. Indeed, the harmful effect of IL-6 has been shown in different models of AKI, including ischemic and sepsis-induced AKI [31,32,33]. In our study, IL-6, C-reactive protein, and ferritin were not independently associated with severe AKI (Table 2). Our findings were in line with those of Joseph et al., who found no association between IL-6, ferritin, and AKI development [8]. The invoked “cytokine storm” induced by COVID-19 infection has been recently challenged. It has been shown that even if blood IL-6 levels were elevated in patients with COVID-19, they were lower than the values typically reported in acute respiratory distress syndrome [34]. These findings question the premise of whether the degree of inflammation in COVID-19 infection is more extensive than the systemic inflammatory response seen in other infection-associated critical illness.
A hypercoagulable state and a high incidence of acute thrombotic events have been frequently reported in patients with COVID-19 [21,22,23,35]. The presence of thrombi in glomerular loops suggested that coagulation dysregulation can participate in AKI development [24]. However, the absence of association between D-dimer, fibrinogen levels, and AKI in our study and previous reports [8] does not support the evidence of a role of hypercoagulability in COVID-19-induced AKI. Until now, there has been no evidence suggesting that the pathophysiological mechanisms of AKI in COVID-19 are different from sepsis-associated AKI [36]. Indeed, acute tubular necrosis was the predominant pathologic finding in autopsies and kidney biopsies of patients with COVID 19 [37,38]. Until more is known about the pathophysiology of COVID-related AKI, the treatment will continue to be supportive, including careful fluid and hemodynamic management, the avoidance of potentially nephrotoxic agents, and the individualized application of renal replacement therapy [36,39].
Similar to our results, Chan et al. [3] found that AKI was independently associated with death in ICU patients with COVID-19 (adjusted OR = 11.4 (95% CI: 7.2–18)). Additionally, in 201 critically ill COVID-19 patients, another study showed that AKI was significantly related to hospital mortality [10]. On the contrary, Forest et al. [26] did not observe a significant association between renal replacement therapy and death (adjusted OR = 2.3 (95% CI: 0.98–5.5)) in 330 critically ill COVID-19 patients admitted to the ICU. Contrary to previous reports [8,10], we did not find an independent association between severe AKI and an instantaneous risk of death (HR = 4.00 (95% CI: 0.80- 20.00); see Table 5)—only with the likelihood of death over the hospital stay (Table 4). Fominskiy et al. did not also find a relationship between AKI and instantaneous risk of death (adjusted HR = 1.32 (95% CI: 0.48–3.63)) in 96 mechanically ventilated patients with COVID-19 [11]. In line with our results, Doher et al. [10] found that AKI was independently associated with longer hospital length of stay (adjusted SHR = 0.31 (95% CI: 0.22–0.44)). Therefore, across most of these studies, AKI in COVID-19 patients seems to be associated with adverse outcomes, and its awareness must be highlighted.
We observed a higher rate of AKI recovery (74.1%) than those reported by Chan et al. [3] and Pei et al. [40] (which were 65% and 45.7%, respectively) in hospitalized COVID-19 patients, even though our population was sicker than those in the two studies. This might have been because our patients were younger (median age: 50 years) compared to the studies of Chan et al. [3] (median age: 64 years) and Pei et al. [40] (mean age: 63 years). Differences in management might also account for the different rates of renal recovery between studies.
Our study had certain strengths. To the best of our knowledge, this is the first report on AKI in critically ill patients from United Arab Emirates. We focused on severe AKI (stages 2 and 3) in critically ill COVID-19 patients with acute respiratory failure, of which a large proportion was managed with invasive mechanical ventilation (70%) and vasopressors (60%). This contrasts with many other published studies that looked at all comers without a specific emphasis on critically ill patients. Indeed, data on severe AKI in these patients are scarce. Additionally, we had a complete follow-up on all our patients. All patients were discharged from the hospital or died before the conception of the study. Furthermore, we reported data on renal recovery in these patients.
Our study had some limitations. First, it was a retrospective study with the potential for selection bias. However, we included a large number of confounders, and after careful adjustment, we were able to determine the potential risk factors of severe AKI and to demonstrate that severe AKI was an independent predictor of hospital mortality. Nevertheless, our data did not include the use of nephrotoxin agents such as aminoglycosides, which are well known as potential risk factors of AKI development. Second, it was a single-center study performed in a specific region of the world, so the results might not be generalized to other centers. Third, in many cases (60%), we did not have a baseline creatinine value, and using the admission value may have overestimated the incidence of AKI. However, most of our patients were young, and only 5.4% had chronic kidney disease. Thus, we think that the baseline creatinine value was normal in the majority of our patients, and the high creatinine levels observed in some patients on hospital admission truly reflected the presence of AKI.
6. Conclusions
In critically ill patients with COVID-19 and acute respiratory failure, we found that the occurrence of severe AKI was common and not associated with inflammatory (IL-6, ferritin, and C-reactive protein) or thromboembolism (D-dimer and fibrinogen) markers. Severe AKI was an independent risk factor of hospital mortality and hospital length of stay, and it should be recognized rapidly during SARS-CoV-2 infection. Prospective studies are needed to confirm our results.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/10/6/1217/s1, Table S1: Factors associated with severe AKI (stages 2 and 3) in multivariable logistic regression analysis. Table S2: Factors associated with AKI stages 2 and 3 (multivariable logistic regression analysis). Table S3: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S4: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S5: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S6: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S7: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S8: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S9: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S10: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S11: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S12: Factors associated with hospital mortality (multivariable logistic regression analysis). Table S13: Factors associated with hospital length of stay in multivariable competing-risks regression analysis.
Author Contributions
J.M., M.G. and N.A. designed the study. J.M., M.B., B.D.O., K.A., A.N., H.E., Y.V., D.M., K.S., A.B., B.A., S.S., J.D., A.W., A.T. and F.H. collected data. J.M. conducted statistical analyses. M.G., N.A., N.R. and J.M. participated in manuscript writing and reviewing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Cleveland Clinic Abu Dhabi (protocol code A-2020-055, on 8 June 2020).
Informed Consent Statement
Patient consent was waived due to the retrospective design of the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the Ethics Committee restrictions.
Conflicts of Interest
The authors declare that they have no competing interests related to the subject of the study. The authors have disclosed that they do not have any potential conflicts of interest.
Glossary
| ICU | intensive care unit |
| AKI | acute kidney injury |
| KDIGO | Kidney Disease Improving Global Outcomes |
| COVID | corona virus infectious disease |
| SARS-CoV-2 | severe acute respiratory syndrome corona virus 2 |
| RRT | renal replacement therapy |
| IL-6 | interleukin-6 |
| OR | odds ratio |
| IQR | interquartile range |
| SHR | sub hazard ratio |
| aptt | activated partial thromboplastin time |
| INR | international normalized ratio |
| SOFA | Sequential Organ Failure assessment |
| SAPS | Simplified Acute Physiology Score |
References
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fung, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef]
- Chan, L.; Chaudhary, K.; Saha, A.; Chauhan, K.; Vaid, A.; Zhao, S.; Paranjpe, I.; Richter, F.; Nadkarni, G.N.; Lala, A.; et al. Mount Sinai COVID Informatics Center (MSCIC). AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 2021, 32, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J.S.; Ng, J.H.; Ross, D.W.; Sharma, P.; Shah, H.H.; Barnett, R.L.; Hazzan, A.D.; Fishbane, S.; Jhaveri, K.D.; Abate, M.; et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020, 98, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Zhao, Y.; Yang, L. Acute kidney injury in COVID-19: The Chinese experience. Semin. Nephrol. 2020, 40, 430–442. [Google Scholar] [CrossRef]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef]
- Chen, Y.-T.; Shao, S.-C.; Chen, Y.-C.; Hsu, C.-K.; Hung, M.-J.; Wu, I.-W. Incidence of acute kidney injury in COVID-19 infection: A systematic review and me-ta-analysis. Crit. Care 2020, 24, 346. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.; Zafrani, L.; Mabrouki, A.; Azoulay, E.; Darmon, M. Acute kidney injury in patients with SARS-CoV-2 infection. Ann Intensive Care 2020, 10, 117. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Zhang, L.; Hu, Y.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Doher, M.P.; De Carvalho, F.R.T.; Scherer, P.F.; Matsui, T.N.; Ammirati, A.L.; Da Silva, B.C.; Barbeiro, B.G.; Carneiro, F.D.; Corrêa, T.D.; Ferraz, L.J.R.; et al. Acute kidney injury and renal replacement therapy in critically Ill COVID-19 patients: Risk factors and outcomes: A single-center experience in Brazil. Blood Purif. 2020, 18, 1–11. [Google Scholar] [CrossRef]
- Fominskiy, E.V.; Scandroglio, A.M.; Monti, G.; Calabrò, M.G.; Landoni, G.; Dell’Acqua, A.; Beretta, L.; Moizo, E.; Ravizza, A.; Monaco, F.; et al. Prevalence, characteristics, risk factors, and outcomes of invasively ventilated COVID-19 patients with acute kidney injury and renal replacement therapy. Blood Purif. 2021, 50, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hayek, S.S.; Wang, W.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J.; et al. Factors associated with death in critically Ill patients with coronavirus disease 2019 in the US. JAMA Intern. Med. 2020, 180, 1–12. [Google Scholar] [CrossRef]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Ye, M.; Wysocki, J.; William, J.; Soler, M.J.; Cokic, I.; Batlle, D. Glomerular localization and expression of angiotensin-converting enzyme 2 and angiotensin-converting enzyme: Implications for albuminuria in diabetes. J. Am. Soc. Nephrol. 2006, 17, 3067–3075. [Google Scholar] [CrossRef]
- Pan, X.W.; Xu, D.; Zhang, H.; Zhou, W.; Wang, L.-H.; Cui, X.G. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: A study based on single-cell transcriptome analysis. Intensive Care Med. 2020, 46, 1114–1116. [Google Scholar] [CrossRef]
- Hassanein, M.; Radhakrishnan, Y.; Sedor, J.; Vachharajani, T.; Vachharajani, V.T.; Augustine, J.; Demirjian, S.; Thomas, G. COVID-19 and the kidney. Clevel. Clin. J. Med. 2020, 87, 619–631. [Google Scholar] [CrossRef]
- Gabarre, P.; Dumas, G.; Dupont, T.; Darmon, M.; Azoulay, E.; Zafrani, L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020, 46, 1339–1348. [Google Scholar] [CrossRef] [PubMed]
- Batlle, D.; Soler, M.J.; Sparks, M.A.; Hiremath, S.; South, A.M.; Welling, P.A.; Swaminathan, S. Acute kidney injury in COVID-19: Emerging evidence of a distinct pathophysiology. J. Am. Soc. Nephrol. 2020, 31, 1380–1383. [Google Scholar] [CrossRef]
- Soy, M.; Keser, G.; Atagündüz, P.; Tabak, F.; Atagündüz, I.; Kayhan, S. Cytokine storm in COVID-19: Pathogenesis and overview of anti-inflammatory agents used in treatment. Clin. Rheumatol. 2020, 39, 2085–2094. [Google Scholar] [CrossRef]
- Zarbock, A.; Gomez, H.; Kellum, J.A. Sepsis-induced acute kidney injury revisited: Pathophysiology, prevention and future therapies. Curr. Opin. Crit. Care 2014, 20, 588–595. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Gandet, F.F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Keptain, F.H.J.; van paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Incidence of thrombotic compli-cations in critically ill ICU patients with COVID-19. Thromb. Res. 2020, 191, 145–147. [Google Scholar] [CrossRef]
- Atallah, B.; Sadik, Z.G.; Salem, N.; El Nekidy, W.S.; Almahmeed, W.; Park, W.M.; Cherfan, A.; Hamed, F.; Mallat, J. The impact of protocol-based high-intensity pharmacological thromboprophylaxis on thrombotic events in critically ill COVID-19 patients. Anaesthesia 2021, 76, 327–335. [Google Scholar] [CrossRef]
- Su, H.; Yang, M.; Wan, C.; Yi, L.-X.; Tang, F.; Zhu, H.-Y.; Yi, F.; Yang, H.-C.; Fogo, A.B.; Nie, X.; et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020, 98, 219–227. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO): Acute Kidney Injury (AKI). Available online: https://kdigo.org/guidelines/acute-kidney-injury/ (accessed on 22 January 2021).
- Vittinghoff, E.; McCulloch, C.E. Relaxing the rule of ten events per variable in logistic and cox regression. Am. J. Epidemiol. 2006, 165, 710–718. [Google Scholar] [CrossRef]
- Wiersema, R.; Jukarainen, S.; Eck, R.J.; Kaufmann, T.; Koeze, J.; Keus, F.; Pettilä, V.; Van Der Horst, I.C.C.; Vaara, S.T. Different applications of the KDIGO criteria for AKI lead to different incidences in critically ill patients: A post hoc analysis from the prospective observational SICS-II study. Crit. Care 2020, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Forest, S.J.; Michler, R.E.; Skendelas, J.P.; DeRose, J.J.; Friedmann, P.; Parides, M.K.; Forest, S.K.; Chauhan, D.; Goldstein, D.J. De novo renal failure and clinical out-comes of patients with critical coronavirus disease 2019. Crit. Care Med. 2021, 49, e161–e169. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Liu, F.; Li, L.; Xu, M.; Wu, J.; Luo, D.; Zhu, Y.; Li, B.; Song, X.; Zhou, X. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in pa-tients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Su, H.; Lei, C.-T.; Zhang, C. Interleukin-6 signaling pathway and its role in kidney disease: An update. Front. Immunol. 2017, 8, 405. [Google Scholar] [CrossRef] [PubMed]
- Nechemia-Arbely, Y.; Barkan, D.; Pizov, G.; Shriki, A.; Rose-John, S.; Galun, E.; Axelrod, J.H. IL-6/IL-6R axis plays a critical Role in acute kidney injury. J. Am. Soc. Nephrol. 2008, 19, 1106–1115. [Google Scholar] [CrossRef]
- Sinha, P.; Matthay, M.A.; Calfee, C.S. Is a "cytokine storm" relevant to COVID-19? JAMA Intern. Med. 2020, 180, 1152–1154. [Google Scholar] [CrossRef] [PubMed]
- Salem, N.; Atallah, B.; El Nekidy, W.S.; Sadik, Z.G.; Park, W.M.; Mallat, J. Thromboelastography findings in critically ill COVID-19 patients. J. Thromb. Thrombolysis 2020, 1–5. [Google Scholar] [CrossRef]
- Kellum, J.A.; Nadim, M.K.; Forni, L.G. Sepsis-associated acute kidney injury: Is COVID-19 different? Kidney Int. 2020, 98, 1370–1372. [Google Scholar] [CrossRef]
- Sharma, P.; Uppal, N.N.; Wanchoo, R.; Shah, H.H.; Yang, Y.; Parikh, R.; Khanin, Y.; Madireddy, V.; Larsen, C.P.; Jhaveri, K.D.; et al. COVID-19–associated kidney injury: A case series of kidney biopsy findings. J. Am. Soc. Nephrol. 2020, 31, 1948–1958. [Google Scholar] [CrossRef]
- Ng, H.J.; Sise, E.M.; Jhaveri, K.D.; Bijol, V.; Sparks, M.A.; Izzedine, H. Pathophysiology and pathology of acute kidney injury in patients with COVID-19. Adv. Chronic Kidney Dis. 2020, 27, 365–376. [Google Scholar] [CrossRef]
- Kellum, J.A.; van Till, J.W.O.; Mulligan, G. Targeting acute kidney injury in COVID-19. Nephrol. Dial. Transplant. 2020, 35, 1652–1662. [Google Scholar] [CrossRef]
- Pei, G.; Zhang, Z.; Peng, J.; Liu, L.; Zhang, C.; Yu, C.; Ma, Z.; Huang, Y.; Liu, W.; Yao, Y.; et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J. Am. Soc. Nephrol. 2020, 31, 1157–1165. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).