Cancer Patients’ Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER
Abstract
1. Introduction
2. Methods
2.1. Objectives
2.2. Study Design, Settings, and Participants
2.3. Outcome Measures and Analysis
2.4. Study Registration and Ethical Approval
3. Results
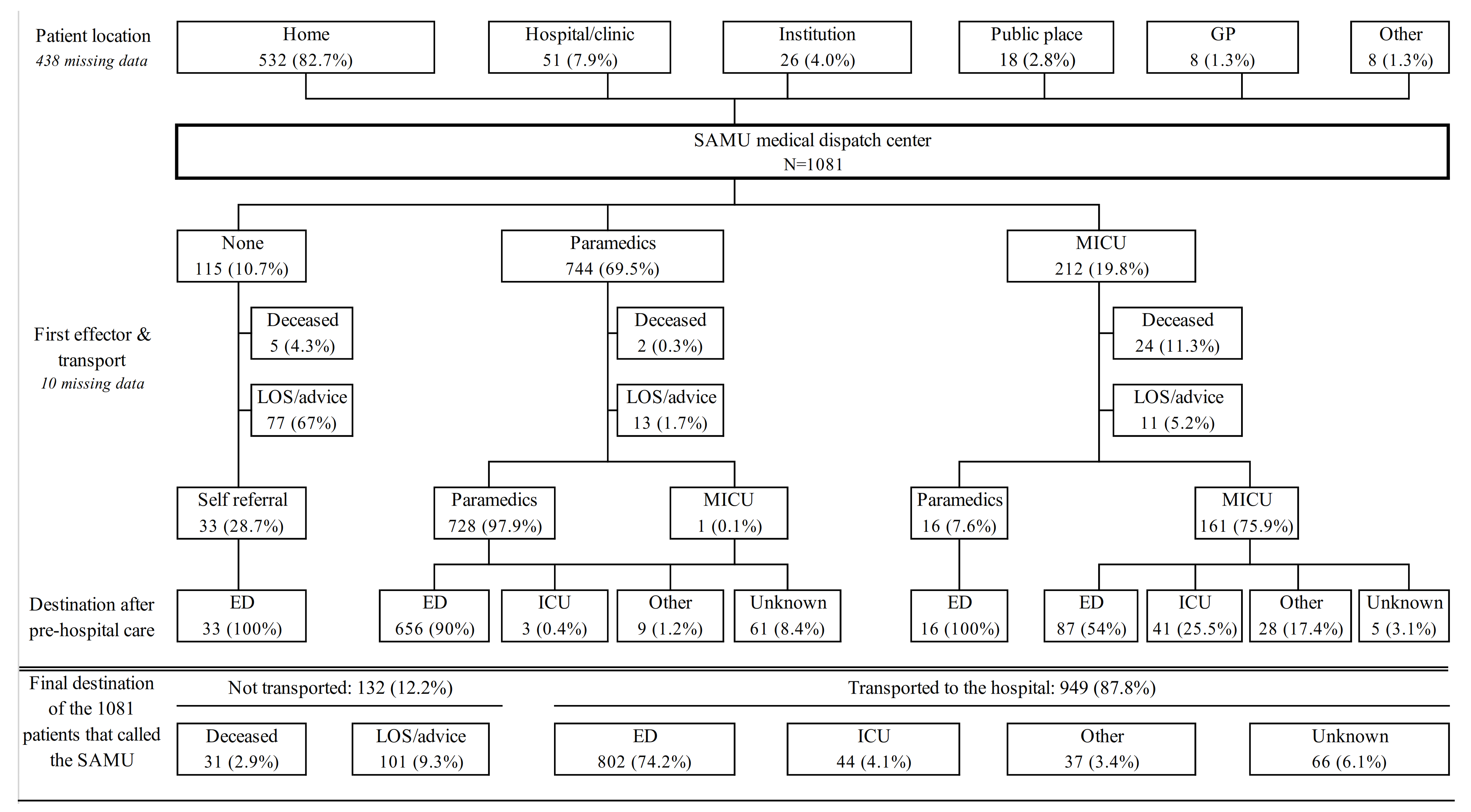
3.1. General Characteristics, Trajectories, and Reasons for Seeking Emergency Care
3.2. Care Delivered by MICUs
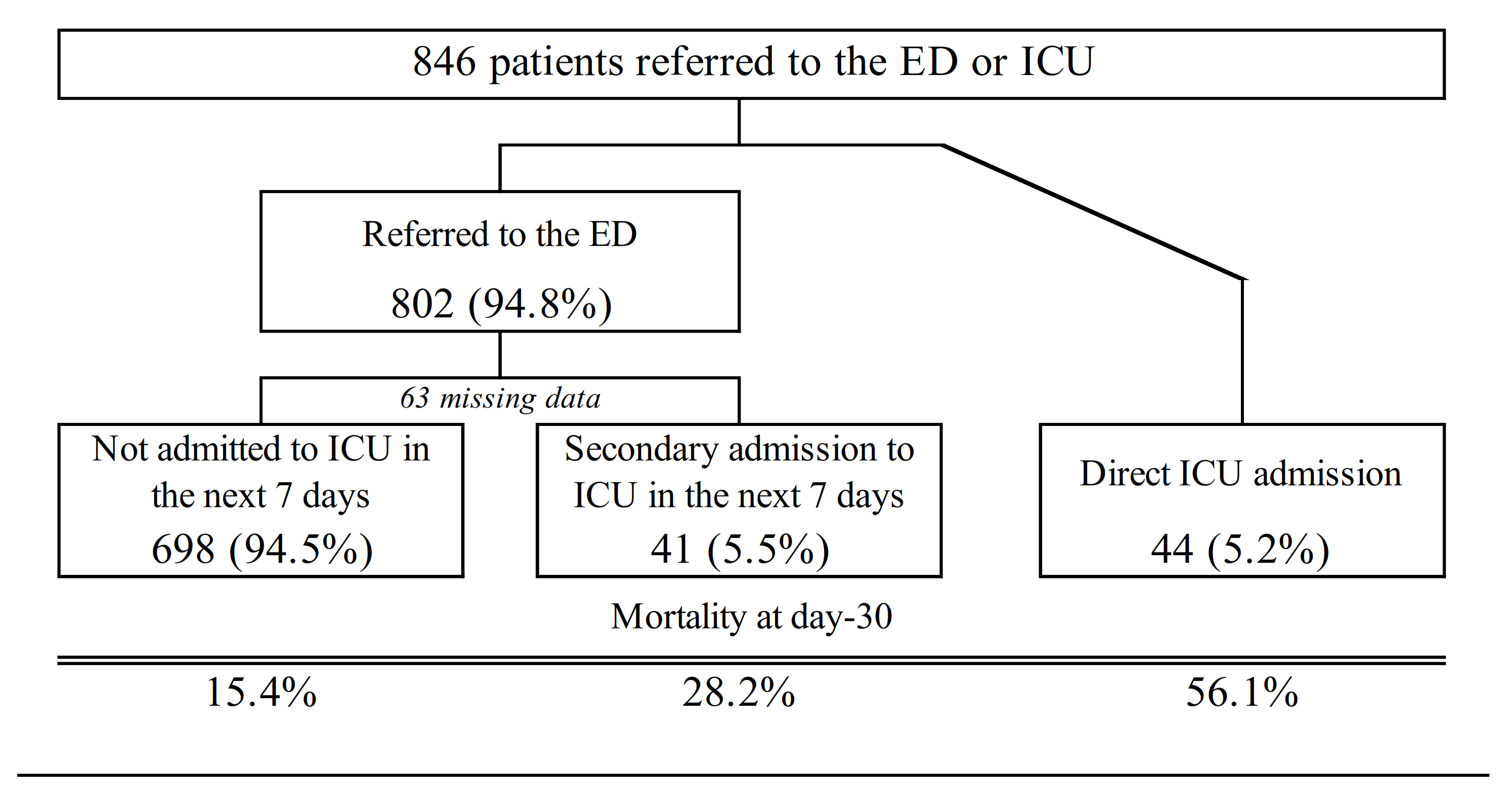
3.3. Patients’ Outcomes
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Defossez, G.; Le Guyader-Peyrou, S.; Uhry, Z.; Grosclaude, P.; Colonna, M.; Dantony, E.; Delafosse, P.; Molinié, F.; Woronoff, A.S.; Bouvier, A.M.; et al. Estimations nationales de l’incidence et de la mortalité par cancer en France métropolitaine entre 1990 et 2018. In Etude À Partir Des Registres Des Cancers Du Réseau Francim. Résultats Préliminaires. Synthèse; Saint-Maurice: Santé Publique, France, 2019. [Google Scholar]
- Shapiro, C.L. Cancer Survivorship. N. Engl. J. Med. 2018, 379, 2438–2450. [Google Scholar] [CrossRef]
- Howlader, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.; et al. SEER Cancer Statistics Review, 1975–2016; Based on November 2018 SEER Data Submission, Posted to the SEER Web Site, April 2019; National Cancer Institute: Bethesda, MD, USA. Available online: https://seer.cancer.gov/csr/1975_2016/ (accessed on 9 April 2020).
- Peyrony, O.; Shapiro, N.I. The 10 signs telling me that my cancer patient in the emergency department is at high risk of becoming critically ill. Intensive Care Med. 2018, 44, 2315–2318. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Grudzen, C.; Kyriacou, D.N.; Obermeyer, Z.; Quest, T.; Rivera, D.; Stone, S.; Wright, J.; Shelburne, N. The Emergency Care of Patients With Cancer: Setting the Research Agenda. Ann. Emerg. Med. 2016, 68, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Greene, J. CONCERN for Cancer: New National Institutes of Health Network to Focus on Cancer Patients in the Emergency Department. Ann. Emerg. Med. 2015, 66, A13–A15. [Google Scholar] [CrossRef] [PubMed]
- Rivera, D.R.; Gallicchio, L.; Brown, J.; Liu, B.; Kyriacou, D.N.; Shelburne, N. Trends in Adult Cancer–Related Emergency Department Utilization: An Analysis of Data From the Nationwide Emergency Department Sample. JAMA Oncol. 2017, 3, e172450. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.; Donnelly, J.P.; Moore, J.X.; Meneses, K.; Williams, G.; Wang, H.E. National characteristics of Emergency Department visits by patients with cancer in the United States. Am. J. Emerg. Med. 2018, 36, 2038–2043. [Google Scholar] [CrossRef] [PubMed]
- Van Der Meer, D.M.; Weiland, T.J.; Philip, J.; Jelinek, G.A.; Boughey, M.; Knott, J.; Marck, C.H.; Weil, J.L.; Lane, H.P.; Dowling, A.J.; et al. Presentation patterns and outcomes of patients with cancer accessing care in emergency departments in Victoria, Australia. Support. Care Cancer 2016, 24, 1251–1260. [Google Scholar] [CrossRef]
- Mayer, D.K.; Travers, D.; Wyss, A.; Leak, A.; Waller, A. Why Do Patients with Cancer Visit Emergency Departments? Results of a 2008 Population Study in North Carolina. J. Clin. Oncol. 2011, 29, 2683–2688. [Google Scholar] [CrossRef]
- VanDyk, A.D.; Harrison, M.B.; Macartney, G.; Ross-White, A.; Stacey, D. Emergency department visits for symptoms experienced by oncology patients: A systematic review. Support. Care Cancer 2012, 20, 1589–1599. [Google Scholar] [CrossRef]
- Peyrony, O.; Fontaine, J.-P.; Beaune, S.; Khoury, A.; Truchot, J.; Balen, F.; Vally, R.; Schmitt, J.; Ben Hammouda, K.; Roussel, M.; et al. EPICANCER—Cancer Patients Presenting to the Emergency Departments in France: A Prospective Nationwide Study. J. Clin. Med. 2020, 9, 1505. [Google Scholar] [CrossRef] [PubMed]
- Wiese, C.H.R.; Bartels, U.E.; Marczynska, K.; Ruppert, D.; Graf, B.M.; Hanekop, G.G. Quality of out-of-hospital palliative emergency care depends on the expertise of the emergency medical team—A prospective multi-centre analysis. Support. Care Cancer 2009, 17, 1499–1506. [Google Scholar] [CrossRef]
- Wiese, C.H.R.; Bartels, U.E.; Zausig, Y.A.; Pfirstinger, J.; Graf, B.M.; Hanekop, G.G. Prehospital emergency treatment of palliative care patients with cardiac arrest: A retrolective investigation. Support. Care Cancer 2010, 18, 1287–1292. [Google Scholar] [CrossRef]
- Chen, B.; Kanaan, C.; Jaiyesimi, I.; Ezekwudo, D.; Swor, R. Clinical Characteristics of Patients with Cancer Presenting to the Emergency Department and Their Use of Emergency Medical Service Transport. Prehospital Emerg. Care 2020, 25, 1–9. [Google Scholar] [CrossRef]
- Purcell, M.G.; El Majzoub, I. The Oncologic Emergency Medicine Fellowship. Emerg. Med. Clin. N. Am. 2018, 36, 637–643. [Google Scholar] [CrossRef]
- Legramante, J.M.; Pellicori, S.; Magrini, A.; Frittelli, T.; Formica, V.; Roselli, M. Cancer Patients in the Emergency Department: A “Nightmare” that Might Become a Virtuous Clinical Pathway. Anticancer. Res. 2018, 38, 6387–6391. [Google Scholar] [CrossRef]
- Brooks, G.A.; Chen, E.J.; Murakami, M.A.; Giannakis, M.; Baugh, C.W.; Schrag, D. An ED pilot intervention to facilitate outpatient acute care for cancer patients. Am. J. Emerg. Med. 2016, 34, 1934–1938. [Google Scholar] [CrossRef]
- Azoulay, E.; Mokart, D.; Pène, F.; Lambert, J.; Kouatchet, A.; Mayaux, J.; Vincent, F.; Nyunga, M.; Bruneel, F.; Laisne, L.-M.; et al. Outcomes of Critically Ill Patients With Hematologic Malignancies: Prospective Multicenter Data From France and Belgium—A Groupe de Recherche Respiratoire en Réanimation Onco-Hématologique Study. J. Clin. Oncol. 2013, 31, 2810–2818. [Google Scholar] [CrossRef] [PubMed]
- Azoulay, E.; Pène, F.; Darmon, M.; Lengliné, E.; Benoit, D.; Soares, M.; Vincent, F.; Bruneel, F.; Perez, P.; Lemiale, V.; et al. Groupe de Recherche Respiratoire en Réanimation Onco-Hématologique (Grrr-OH). Managing critically Ill hematology patients: Time to think differently. Blood Rev. 2015, 29, 359–367. [Google Scholar] [CrossRef]
- Soares, M.; Bozza, F.A.; Azevedo, L.C.; Silva, U.V.; Corrêa, T.D.; Colombari, F.; Torelly, A.P.; Varaschin, P.; Viana, W.N.; Knibel, M.F.; et al. Effects of Organizational Characteristics on Outcomes and Resource Use in Patients with Cancer Admitted to Intensive Care Units. J. Clin. Oncol. 2016, 34, 3315–3324. [Google Scholar] [CrossRef]
- Borcoman, E.; Dupont, A.; Mariotte, E.; Doucet, L.; Joseph, A.; Chermak, A.; Valade, S.; Resche-Rigon, M.; Azoulay, E.; Lemiale, V. One-year survival in patients with solid tumours discharged alive from the intensive care unit after unplanned admission: A retrospective study. J. Crit. Care 2020, 57, 36–41. [Google Scholar] [CrossRef]
- Darmon, M.; Bourmaud, A.; Georges, Q.; Soares, M.; Jeon, K.; Oeyen, S.; Rhee, C.K.; Gruber, P.; Ostermann, M.; Hill, Q.A.; et al. Changes in critically ill cancer patients’ short-term outcome over the last decades: Results of systematic review with meta-analysis on individual data. Intensive Care Med. 2019, 45, 977–987. [Google Scholar] [CrossRef]
- Peyrony, O.; Chevret, S.; Meert, A.-P.; Perez, P.; Kouatchet, A.; Pène, F.; Mokart, D.; Lemiale, V.; Demoule, A.; Nyunga, M.; et al. Direct admission to the intensive care unit from the emergency department and mortality in critically ill hematology patients. Ann. Intensive Care 2019, 9, 110. [Google Scholar] [CrossRef] [PubMed]
- Lengliné, E.; Raffoux, E.; Lemiale, V.; Darmon, M.; Canet, E.; Boissel, N.; Schlemmer, B.; Dombret, H.; Azoulay, E. Intensive care unit management of patients with newly diagnosed acute myeloid leukemia with no organ failure. Leuk. Lymphoma 2012, 53, 1352–1359. [Google Scholar] [CrossRef]
- Thiéry, G.; Azoulay, É.; Darmon, M.; Ciroldi, M.; De Miranda, S.; Lévy, V.; Fieux, F.; Moreau, D.; Le Gall, J.R.; Schlemmer, B. Outcome of Cancer Patients Considered for Intensive Care Unit Admission: A Hospital-Wide Prospective Study. J. Clin. Oncol. 2005, 23, 4406–4413. [Google Scholar] [CrossRef]
| Missing Data | |||
|---|---|---|---|
| N | 1081 | ||
| Age (years), Median (IQR) | 72 | (62–82) | 23 |
| Female Gender, n (%) | 470 | (43.8) | 9 |
| Night Shift (18 h–8 h), n (%) | 412 | (38.3) | 5 |
| Cancer Type, n (%) | 13 | ||
| Hematologic Malignancy | 153 | (14.3) | |
| Solid Malignancy | 915 | (85.7) | |
| Malignancy Status, n (%) | 308 | ||
| Complete or Partial Remission | 417 | (53.9) | |
| Uncontrolled | 356 | (46.1) | |
| Metastatic Malignancy, n (%) | 301 | (51.5) | 497 |
| Time since Malignancy Diagnosis, n (%) | 198 | ||
| <6 months | 169 | (19.1) | |
| 6 months to 5 years | 528 | (59.8) | |
| >5 years | 186 | (21.1) | |
| Nursing Services, n (%) | 92 | ||
| None | 552 | (55.8) | |
| Home nursing service | 338 | (34.2) | |
| Nursing home care | 42 | (4.2) | |
| Institution | 57 | (5.8) | |
| Patient Alone at Home, n (%) | 155 | (27.0) | 506 |
| Poor Performance Status (>2), n (%) | 234 | (28.7) | 267 |
| Missing Data | |||
|---|---|---|---|
| N | 1081 | ||
| Reason, n (%) | 2 | ||
| Dyspnea | 218 | (20.2) | |
| Neurological Disorder | 166 | (15.4) | |
| Fatigue | 141 | (13.1) | |
| Trauma | 129 | (12.0) | |
| Gastro-intestinal | 123 | (11.4) | |
| Thoracic Pain | 90 | (8.3) | |
| Fever | 75 | (7.0) | |
| Bleeding | 74 | (6.9) | |
| Dizziness/Instability | 74 | (6.9) | |
| Pain | 47 | (4.4) | |
| Cardiac Arrest | 27 | (2.5) | |
| Agitation | 21 | (1.9) | |
| Metabolic Disorder | 15 | (1.4) | |
| Cytopenia | 14 | (1.3) | |
| Rash | 12 | (1.1) | |
| Shock | 11 | (1.0) | |
| Arrythmia | 11 | (1.0) | |
| Urologic Disorder | 11 | (1.0) | |
| Medical Device Complication | 4 | (0.4) | |
| Other | 38 | (3.5) | |
| Reason Related to Malignancy, n (%) | 557 | (54.7) | 63 |
| MICU Dispatched | OR | 95% CI | p | Missing Data | |||||
|---|---|---|---|---|---|---|---|---|---|
| No | Yes | ||||||||
| N | 462 | 213 | |||||||
| Age (years), Median (IQR) | 71 | (62–82) | 72 | (64–80) | 1.01 | 0.99 | 1.02 | 0.4 | 15 |
| Male Gender, n (%) | 248 | (54.1) | 129 | (60.8) | 1.32 | 0.95 | 1.84 | 0.1 | 5 |
| Solid Malignancy, n (%) | 399 | (87.9) | 173 | (82.8) | 0.66 | 0.42 | 1.05 | 0.08 | 12 |
| Uncontrolled Malignancy, n (%) | 142 | (46.6) | 72 | (49.0) | 1.10 | 0.74 | 1.63 | 0.6 | 223 |
| Metastatic Malignancy, n (%) | 125 | (55.3) | 54 | (51.9) | 0.87 | 0.55 | 1.39 | 0.6 | 345 |
| Time since Malignancy Diagnosis, n (%) | 161 | ||||||||
| <6 months | 62 | (18.6) | 41 | (22.8) | 1.00 | ||||
| 6 months to 5 years | 196 | (58.7) | 105 | (58.3) | 0.81 | 0.51 | 1.29 | 0.4 | |
| >5 years | 76 | (22.8) | 34 | (18.9) | 0.68 | 0.38 | 1.19 | 0.2 | |
| Home Nursing Services, n (%) | 183 | (44.4) | 75 | (39.3) | 0.81 | 0.57 | 1.15 | 0.2 | 72 |
| Patient Alone at Home, n (%) | 53 | (24.0) | 29 | (28.4) | 1.26 | 0.74 | 2.13 | 0.4 | 352 |
| Poor Performance Status (>2), n (%) | 86 | (27.8) | 48 | (29.4) | 1.08 | 0.71 | 1.64 | 0.7 | 203 |
| Reason for Seeking Emergency Care, n (%) | 2 | ||||||||
| Cardiac Arrest | 7 | (1.5) | 20 | (9.4) | 6.71 | 2.92 | 17.33 | <0.0001 | |
| Dyspnea | 70 | (15.2) | 74 | (34.7) | 2.97 | 2.03 | 4.34 | <0.0001 | |
| Neurological Disorder | 57 | (12.4) | 47 | (22.1) | 2.00 | 1.3 | 3.06 | 0.001 | |
| Thoracic Pain | 37 | (8.0) | 32 | (15.0) | 2.02 | 1.22 | 3.35 | 0.006 | |
| Trauma | 57 | (12.4) | 4 | (1.9) | 0.14 | 0.04 | 0.33 | 0.0001 | |
| Fatigue | 58 | (12.6) | 5 | (2.3) | 0.17 | 0.06 | 0.38 | 0.0002 | |
| Fever | 38 | (8.3) | 5 | (2.3) | 0.27 | 0.09 | 0.63 | 0.006 | |
| Digestive Disorder | 60 | (13.0) | 10 | (4.7) | 0.33 | 0.16 | 0.63 | 0.002 | |
| Reason Related to Malignancy, n (%) | 248 | (58.5) | 115 | (56.4) | 0.92 | 0.65 | 1.29 | 0.6 | 47 |
| Critically Ill, n (%) | 29 | (6.4) | 115 | (54.2) | 17.42 | 11.1 | 28.1 | <0.0001 | 8 |
| Cardiac Arrest | 7 | (1.6) | 21 | (12.4) | 8.64 | 3.77 | 22.3 | <0.0001 | 73 |
| Shock | 1 | (0.2) | 41 | (24.6) | 138.62 | 29.7 | >100 | <0.0001 | 81 |
| Respiratory Failure | 12 | (2.7) | 65 | (35.1) | 19.23 | 10.41 | 38.48 | <0.0001 | 52 |
| Altered Mental Status | 7 | (1.6) | 30 | (17.2) | 12.68 | 5.76 | 31.97 | <0.0001 | 68 |
| Missing Data | |||
|---|---|---|---|
| N | 115 | ||
| Critically Ill, n (%) | 49 | (42.6) | 0 |
| Respiratory Failure | 30 | (26.1) | 0 |
| Shock | 28 | (24.6) | 1 |
| Altered Mental Status | 14 | (12.2) | 0 |
| Cardiac Arrest | 13 | (11.3) | 0 |
| Investigation, n (%) | 0 | ||
| Ultrasound | 4 | (3.5) | |
| Blood Sample | 12 | (10.4) | |
| ECG | 51 | (44.3) | |
| Venous Access, n (%) | 0 | ||
| Peripheral | 78 | (67.8) | |
| Central | 4 | (3.5) | |
| Long Term Central Catheter | 2 | (1.7) | |
| Intra-Osseous | 1 | (0.9) | |
| Oxygen Therapy, n (%) | 56 | (48.7) | 0 |
| Nasal | 49 | (42.6) | |
| Mechanical Ventilation | 13 | (11.3) | |
| Nasal High Flow Oxygen | 8 | (7.0) | |
| Existing Tracheostomy Use | 1 | (5.6) | |
| Treatment, n (%) | 0 | ||
| Fluid Challenge | 24 | (20.9) | |
| Catecholamines | 13 | (11.3) | |
| Analgesia (Not Morphine) | 6 | (5.2) | |
| Morphine | 10 | (8.7) | |
| Cardiopulmonary Resuscitation | 8 | (7.0) | |
| Sedation | 7 | (6.1) | |
| Antibiotics | 2 | (1.7) | |
| Other | 11 | (9.6) | |
| Length of Intervention (min), Median (IQR) | 60 | (42–82) | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peyrony, O.; Fontaine, J.-P.; Trabattoni, E.; Nakad, L.; Charreyre, S.; Picaud, A.; Bosc, J.; Viglino, D.; Jacquin, L.; Laribi, S.; et al. Cancer Patients’ Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER. J. Clin. Med. 2021, 10, 1145. https://doi.org/10.3390/jcm10051145
Peyrony O, Fontaine J-P, Trabattoni E, Nakad L, Charreyre S, Picaud A, Bosc J, Viglino D, Jacquin L, Laribi S, et al. Cancer Patients’ Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER. Journal of Clinical Medicine. 2021; 10(5):1145. https://doi.org/10.3390/jcm10051145
Chicago/Turabian StylePeyrony, Olivier, Jean-Paul Fontaine, Eloïse Trabattoni, Lionel Nakad, Sylvain Charreyre, Adrien Picaud, Juliane Bosc, Damien Viglino, Laurent Jacquin, Saïd Laribi, and et al. 2021. "Cancer Patients’ Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER" Journal of Clinical Medicine 10, no. 5: 1145. https://doi.org/10.3390/jcm10051145
APA StylePeyrony, O., Fontaine, J.-P., Trabattoni, E., Nakad, L., Charreyre, S., Picaud, A., Bosc, J., Viglino, D., Jacquin, L., Laribi, S., Pereira, L., Thiriez, S., Paquet, A.-L., Tanneau, A., Azoulay, E., Chevret, S., & Initiatives de Recherche aux Urgences (IRU-SFMU) Research Group. (2021). Cancer Patients’ Prehospital Emergency Care: Post Hoc Analysis from the French Prospective Multicenter Study EPICANCER. Journal of Clinical Medicine, 10(5), 1145. https://doi.org/10.3390/jcm10051145





