Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
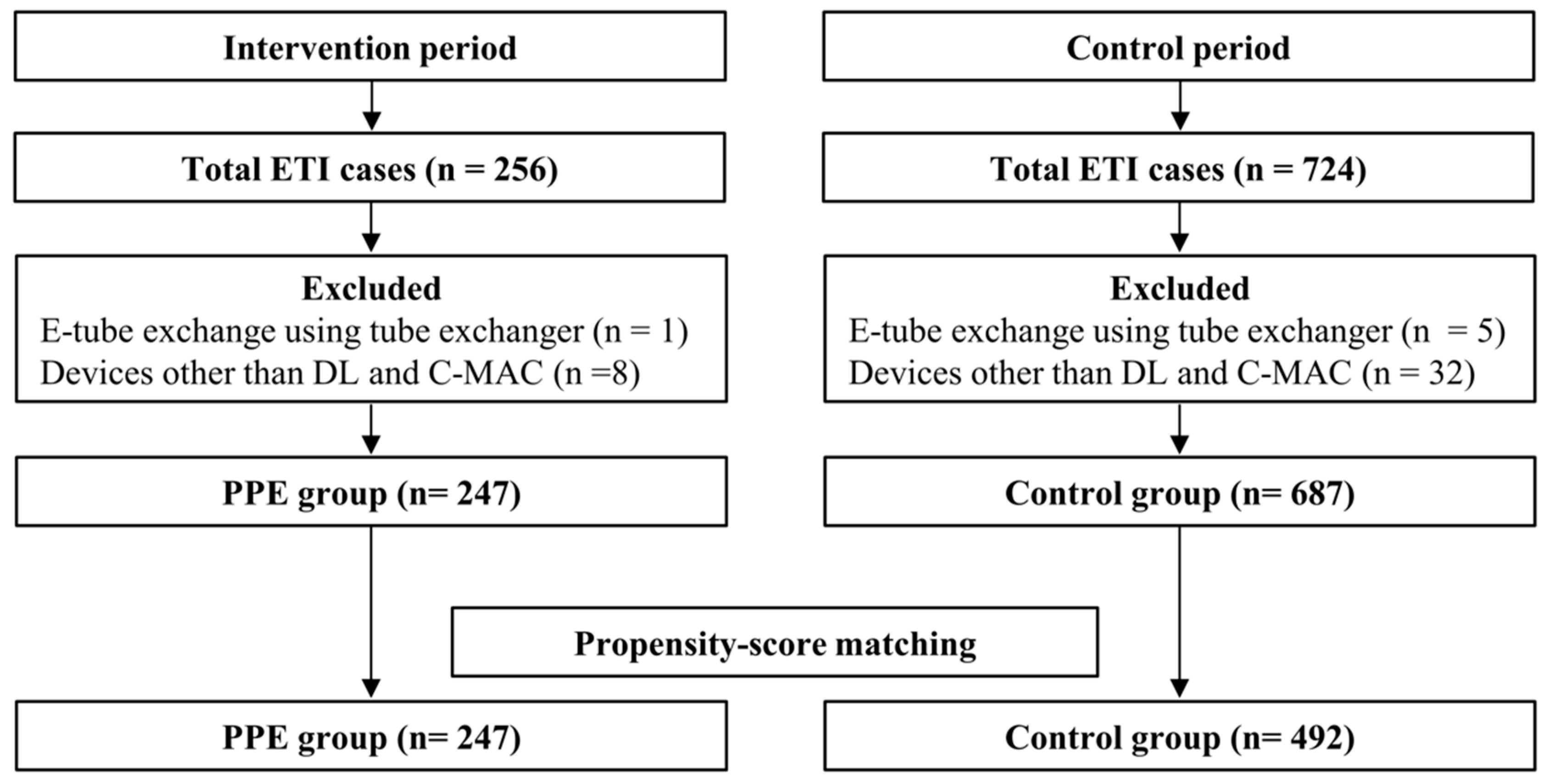
2.2. Study Population
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Characteristics of Study Subjects
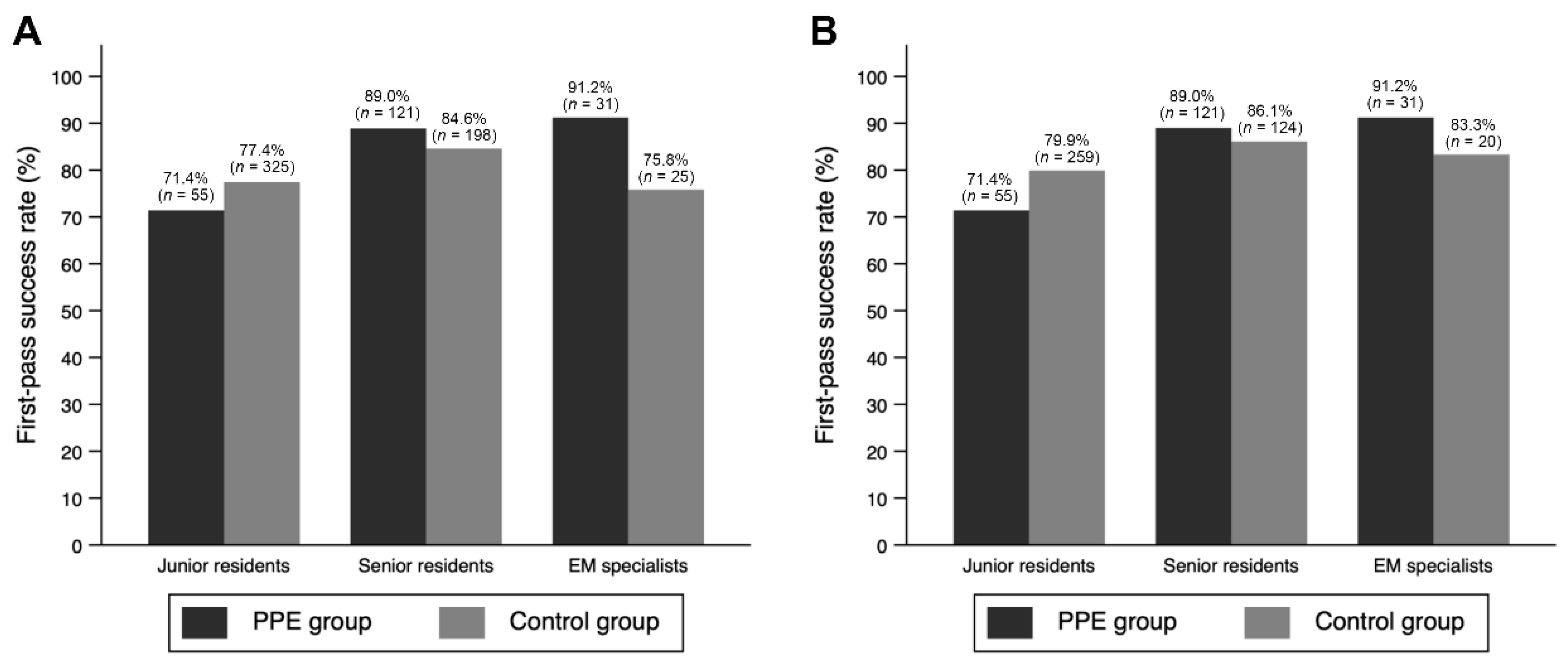
3.2. Main Results
3.3. Subgroup Analysis of Cases Wherein C-MAC VL Was Used
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/table (accessed on 31 December 2020).
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.; Deibert, D.; Wyatt, G.; Durand-Moreau, Q.; Adisesh, A.; Khunti, K.; Khunti, S.; Smith, S.; Chan, X.H.S.; Ross, L.; et al. Classification of aerosol-generating procedures: A rapid systematic review. BMJ Open Respir. Res. 2020, 7. [Google Scholar] [CrossRef]
- Tran, K.; Cimon, K.; Severn, M.; Pessoa-Silva, C.L.; Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS ONE 2012, 7, e35797. [Google Scholar] [CrossRef]
- Tizaoui, K.; Zidi, I.; Lee, K.H.; Ghayda, R.A.; Hong, S.H.; Li, H.; Smith, L.; Koyanagi, A.; Jacob, L.; Kronbichler, A.; et al. Update of the current knowledge on genetics, evolution, immunopathogenesis, and transmission for coronavirus disease 19 (COVID-19). Int. J. Biol. Sci. 2020, 16, 2906–2923. [Google Scholar] [CrossRef]
- El-Boghdadly, K.; Wong, D.J.N.; Owen, R.; Neuman, M.D.; Pocock, S.; Carlisle, J.B.; Johnstone, C.; Andruszkiewicz, P.; Baker, P.A.; Biccard, B.M.; et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: A prospective international multicentre cohort study. Anaesthesia 2020, 75, 1437–1447. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Flaishon, R.; Sotman, A.; Ben-Abraham, R.; Rudick, V.; Varssano, D.; Weinbroum, A.A. Antichemical protective gear prolongs time to successful airway management: A randomized, crossover study in humans. Anesthesiology 2004, 100, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Scott Taylor, R.; Pitzer, M.; Goldman, G.; Czysz, A.; Simunich, T.; Ashurst, J. Comparison of intubation devices in level C personal protective equipment: A cadaveric study. Am. J. Emerg. Med. 2018, 36, 922–925. [Google Scholar] [CrossRef]
- Wong, E.; Ho, K.K. The effect of severe acute respiratory syndrome (SARS) on emergency airway management. Resuscitation 2006, 70, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, J.; Arlidge, J.; Dudley, D.; Sicinski, M.; Ahmad, I. The impact of respiratory protective equipment on difficult airway management: A randomised, crossover, simulation study. Anaesthesia 2020, 75, 1301–1306. [Google Scholar] [CrossRef]
- Wang, C.C.; Chaou, C.H.; Tseng, C.Y.; Lin, C.C. The effect of personal protective equipment on emergency airway management by emergency physicians: A mannequin study. Eur. J. Emerg. Med. 2016, 23, 124–129. [Google Scholar] [CrossRef]
- Shin, D.H.; Choi, P.C.; Na, J.U.; Cho, J.H.; Han, S.K. Utility of the Pentax-AWS in performing tracheal intubation while wearing chemical, biological, radiation and nuclear personal protective equipment: A randomised crossover trial using a manikin. Emerg. Med. J. 2013, 30, 527–531. [Google Scholar] [CrossRef]
- Greenland, K.B.; Tsui, D.; Goodyear, P.; Irwin, M.G. Personal protection equipment for biological hazards: Does it affect tracheal intubation performance? Resuscitation 2007, 74, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Yousif, S.; Machan, J.T.; Alaska, Y.; Suner, S. Airway Management in Disaster Response: A Manikin Study Comparing Direct and Video Laryngoscopy for Endotracheal Intubation by Prehospital Providers in Level C Personal Protective Equipment. Prehosp. Disaster Med. 2017, 32, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Hwang, S.Y.; Park, J.H.; Yoon, H.; Cha, W.C.; Jo, I.J.; Sim, M.S.; Song, K.J.; Woo, H.J.; Jeong, S.G.; Shin, T.G.; et al. Quality Improvement Program Outcomes for Endotracheal Intubation in the Emergency Department. J. Patient Saf. 2018, 14, e83–e88. [Google Scholar] [CrossRef]
- Caputo, K.M.; Byrick, R.; Chapman, M.G.; Orser, B.J.; Orser, B.A. Intubation of SARS patients: Infection and perspectives of healthcare workers. Can. J. Anaesth. 2006, 53, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Abualenain, J.T.; Al-Alawi, M.M. Simulation-based training in Ebola Personal Protective Equipment for healthcare workers: Experience from King Abdulaziz University Hospital in Saudi Arabia. J. Infect. Public Health 2018, 11, 796–800. [Google Scholar] [CrossRef]
- Aljahany, M.; Alassaf, W.; Alibrahim, A.A.; Kentab, O.; Alotaibi, A.; Alresseeni, A.; Algarni, A.; Algaeed, H.A.; Aljaber, M.I.; Alruwaili, B.; et al. Use of In Situ Simulation to Improve Emergency Department Readiness for the COVID-19 Pandemic. Prehosp. Disaster Med. 2021, 36, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Lo, H.Y.; Lin, S.C.; Chaou, C.H.; Chang, Y.C.; Ng, C.J.; Chen, S.Y. What is the impact of the COVID-19 pandemic on emergency medicine residency training: An observational study. BMC Med. Educ. 2020, 20, 348. [Google Scholar] [CrossRef]
- Cook, T.M.; El-Boghdadly, K.; McGuire, B.; McNarry, A.F.; Patel, A.; Higgs, A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020, 75, 785–799. [Google Scholar] [CrossRef] [PubMed]
- Pek, J.H.; Low, J.W.M.; Lau, T.P.; Gan, H.N.; Phua, D.H. Emergency medicine residency training during COVID-19. Singapore Med. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- April, M.D.; Arana, A.; Schauer, S.G.; Davis, W.T.; Oliver, J.J.; Fantegrossi, A.; Summers, S.M.; Maddry, J.K.; Walls, R.M.; Brown, C.A., 3rd. Ketamine Versus Etomidate and Peri-intubation Hypotension: A National Emergency Airway Registry Study. Acad. Emerg. Med. 2020, 27, 1106–1115. [Google Scholar] [CrossRef]
- Mohr, N.M.; Pape, S.G.; Runde, D.; Kaji, A.H.; Walls, R.M.; Brown, C.A., 3rd. Etomidate Use Is Associated With Less Hypotension Than Ketamine for Emergency Department Sepsis Intubations: A NEAR Cohort Study. Acad. Emerg. Med. 2020, 27, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
| Before Matching | After Matching * | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 934) | PPE Group (n = 247) | Control Group (n = 687) | p-Value | Total (n = 739) | PPE Group (n = 247) | Control Group (n = 492) | p-Value | |
| Patient age (years) | 65.6 (15.3) | 66.3 (14.5) | 65.4 (15.6) | 0.452 | 65.6 (15.4) | 66.3 (14.5) | 65.3 (15.8) | 0.414 |
| Patient sex (male) | 578 (61.9) | 149 (60.3) | 429 (62.4) | 0.608 | 460 (62.2) | 149 (60.3) | 311 (63.2) | 0.463 |
| Patient BMI (kg/m2) | 22.9 (4.0) | 22.6 (3.9) | 23.1 (4.0) | 0.123 | 22.9 (4.1) | 22.6 (3.9) | 23.10 (4.2) | 0.080 |
| Patient BMI grade * | 0.422 | 0.466 | ||||||
| Normal (18.5–24.9) | 594 (63.6) | 159 (64.4) | 435 (63.3) | 475 (64.3) | 159 (64.4) | 316 (64.2) | ||
| Under (<18.5) | 105 (11.2) | 31 (12.6) | 74 (10.8) | 83 (11.2) | 31 (12.6) | 52 (10.6) | ||
| Over (25.0–29.9) | 195 (20.9) | 44 (17.8) | 151 (22.0) | 146 (19.8) | 44 (17.8) | 102 (20.7) | ||
| Obesity (≥30.0) | 40 (4.3) | 13 (5.3) | 27 (3.9) | 35 (4.7) | 13 (5.3) | 22 (4.5) | ||
| Vital signs and SpO2† | ||||||||
| Systolic BP (mmHg) | 132.45 (43.0) | 123.3 (39.0) | 135.90 (43.9) | 0.001 | 131.6 (43.8) | 123.3 (39.0) | 135.9 (45.5) | 0.001 |
| Diastolic BP (mmHg) | 73.9 (26.3) | 71.9 (25.4) | 74.67 (26.6) | 0.242 | 73.7 (26.7) | 71.9 (25.4) | 74.6 (27.3) | 0.257 |
| Heart rate (per minute) | 109.2 (26.8) | 109.7 (25.2) | 109.02 (27.4) | 0.789 | 108.4 (26.9) | 109.7 (25.2) | 107.7 (27.7) | 0.424 |
| Respiratory rate (per minute) | 26.1 (9.0) | 26.8 (9.8) | 25.88 (8.6) | 0.254 | 26.2 (9.0) | 26.8 (9.8) | 25.8 (8.5) | 0.255 |
| SpO2 (%) | 92.9 (11.0) | 93.5 (7.9) | 92.68 (11.9) | 0.434 | 93.0 (10.0) | 93.5 (7.9) | 92.8 (11.0) | 0.443 |
| Difficult laryngoscopy * | 267 (28.6) | 73 (29.6) | 194 (28.2) | 0.756 | 213 (28.8) | 73 (29.6) | 140 (28.5) | 0.757 |
| ETI indication † | ||||||||
| Cardiac arrest | 308 (33.0) | 74 (30.0) | 234 (34.1) | 0.418 | 237 (32.1) | 74 (30.0) | 163 (33.1) | 0.702 |
| Altered mental status | 173 (18.5) | 44 (17.8) | 129 (18.8) | 136 (18.4) | 44 (17.8) | 92 (18.7) | ||
| Respiratory distress | 297 (31.8) | 79 (32.0) | 218 (31.7) | 234 (31.7) | 79 (32.0) | 155 (31.5) | ||
| Shock | 77 (8.2) | 23 (9.3) | 54 (7.9) | 64 (8.7) | 23 (9.3) | 41 (8.3) | ||
| Others | 79 (8.5) | 27 (10.9) | 52 (7.6) | 68 (9.2) | 27 (10.9) | 41 (8.3) | ||
| Method of ETI * | 0.191 | 0.237 | ||||||
| Crash approach | 336 (36.0) | 82 (33.2) | 254 (37.0) | 253 (34.2) | 82 (33.2) | 171 (34.8) | ||
| RSI | 512 (54.8) | 135 (54.7) | 377 (54.9) | 411 (55.6) | 135 (54.7) | 276 (56.1) | ||
| Sedative only | 85 (9.1) | 30 (12.1) | 55 (8.0) | 75 (10.1) | 30 (12.1) | 45 (9.1) | ||
| No medication | 1 (0.1) | 0 (0.0) | 1 (0.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| First attempt | ||||||||
| Specialty of the intubator | 0.218 | 0.245 | ||||||
| EM | 871 (93.3) | 235 (95.1) | 636 (92.6) | 692 (93.6) | 235 (95.1) | 457 (92.9) | ||
| Non-EM | 63 (6.7) | 12 (4.9) | 51 (7.4) | 47 (6.4) | 12 (4.9) | 35 (7.1) | ||
| Level of the intubator ‡ | <0.001 | <0.001 | ||||||
| Junior resident | 497 (53.2) | 77 (31.2) | 420 (61.1) | 401 (54.3) | 77 (31.2) | 324 (65.9) | ||
| Senior resident | 370 (39.6) | 136 (55.1) | 234 (34.1) | 280 (37.9) | 136 (55.1) | 144 (29.3) | ||
| EM specialist | 67 (7.2) | 34 (13.8) | 33 (4.8) | 58 (7.8) | 34 (13.8) | 24 (4.9) | ||
| Device * | <0.001 | 0.547 | ||||||
| DL | 307 (32.9) | 44 (17.8) | 263 (38.3) | 133 (18.0) | 44 (17.8) | 89 (18.1) | ||
| C-MAC VL | 627 (67.1) | 203 (82.2) | 424 (61.7) | 606 (82.0) | 203 (82.2) | 403 (81.9) | ||
| Sedatives | 0.082 | 0.021 | ||||||
| Ketamine | 144 (15.4) | 51 (20.6) | 93 (13.5) | 115 (15.6) | 51 (20.6) | 64 (13.0) | ||
| Etomidate | 414 (44.3) | 100 (40.5) | 314 (45.7) | 335 (45.3) | 100 (40.5) | 235 (47.8) | ||
| Midazolam | 20 (2.1) | 7 (2.8) | 13 (1.9) | 18 (2.4) | 7 (2.8) | 11 (2.2) | ||
| Others | 26 (2.8) | 7 (2.8) | 19 (2.8) | 24 (3.2) | 7 (2.8) | 17 (3.5) | ||
| No sedatives | 330 (35.3) | 82 (33.2) | 248 (36.1) | 247 (33.4) | 82 (33.2) | 165 (33.5) | ||
| NMBAs | 0.775 | 0.708 | ||||||
| Succinylcholine | 230 (24.6) | 65 (26.3) | 165 (24.0) | 189 (25.6) | 65 (26.3) | 124 (25.2) | ||
| Rocuronium | 270 (28.9) | 66 (26.7) | 204 (29.7) | 212 (28.7) | 66 (26.7) | 146 (29.7) | ||
| Others § | 18 (1.9) | 4 (1.6) | 14 (2.0) | 14 (1.9) | 4 (1.6) | 10 (2.0) | ||
| No NMBAs | 416 (44.5) | 112 (45.3) | 304 (44.3) | 324 (43.8) | 112 (45.3) | 212 (43.1) | ||
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (n = 934) | PPE Group (n = 247) | Control Group (n = 687) | p-Value | Total (n = 739) | PPE Group (n = 247) | Control Group (n = 492) | p-Value | |
| Primary outcome | ||||||||
| First-pass success rate | 755 (80.8) | 207 (83.8) | 548 (79.8) | 0.168 | 610 (82.5) | 207 (83.8) | 403 (81.9) | 0.522 |
| Secondary outcomes | ||||||||
| Multiple attempts (≥3) | 52 (5.6) | 11 (4.5) | 41 (6.0) | 0.375 | 35 (4.7) | 11 (4.5) | 24 (4.9) | 0.798 |
| Glottic view | ||||||||
| C-L grade III or IV (%) | 98 (10.5) | 19 (7.7) | 79 (11.5) | 0.100 | 67 (9.1) | 19 (7.7) | 48 (9.8) | 0.354 |
| Complications | ||||||||
| Overall complications * | 144 (15.4) | 47 (19.0) | 97 (14.1) | 0.068 | 120 (16.2) | 47 (19.0) | 73 (14.8) | 0.146 |
| EI | 34 (3.6) | 5 (2.0) | 29 (4.2) | 0.122 | 22 (3.0) | 5 (2.0) | 17 (3.5) | 0.286 |
| Unrecognized EI † | 1 (0.1) | 0 (0.0) | 1 (0.1) | 0.961 | 0 (0.0) | 0 (0.0) | 0 (0.0) | - |
| Dental injury | 15 (1.6) | 2 (0.8) | 13 (1.9) | 0.260 | 13 (1.8) | 2 (0.8) | 11 (2.2) | 0.182 |
| Post-intubation hypotension | 52 (5.6) | 29 (11.7) | 23 (3.3) | <0.001 | 47 (6.4) | 29 (11.7) | 18 (3.7) | <0.001 |
| Post-intubation hypoxemia | 31 (3.3) | 8 (3.2) | 23 (3.3) | 0.935 | 24 (3.2) | 8 (3.2) | 16 (3.3) | 0.992 |
| Vomiting | 2 (0.2) | 0 (0.0) | 2 (0.3) | 0.685 | 2 (0.3) | 0 (0.0) | 2 (0.4) | 0.512 ‡ |
| Agitation | 6 (0.6) | 4 (1.6) | 2 (0.3) | 0.047 | 6 (0.8) | 4 (1.6) | 2 (0.4) | 0.109 |
| Cardiac arrest | 21 (2.2) | 5 (2.0) | 16 (2.3) | 0.782 | 20 (2.7) | 5 (2.0) | 15 (3.0) | 0.421 |
| 24 h Mortality | 5 (0.5) | 1 (0.4) | 4 (0.6) | 0.745 | 5 (0.7) | 1 (0.4) | 4 (0.8) | 0.531 |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| First-pass success | |||
| Wearing of PPE | 0.90 | 0.57–1.40 | 0.629 |
| Level of the intubator * | |||
| Junior resident | Reference | ||
| Senior resident | 2.00 | 1.27–3.16 | 0.003 |
| EM specialist | 2.11 | 0.86–5.17 | 0.103 |
| Multiple attempts | |||
| Wearing of PPE | 0.90 | 0.39–2.07 | 0.795 |
| Level of the intubator * | |||
| Junior resident | Reference | ||
| Senior resident | 1.01 | 0.48–2.15 | 0.978 |
| EM specialist | 1.15 | 0.28–4.66 | 0.850 |
| Glottic view (C-L grade III or IV) | |||
| Wearing of PPE | 0.78 | 0.43–1.40 | 0.404 |
| Level of the intubator * | |||
| Junior resident | Reference | ||
| Senior resident | 0.96 | 0.56–1.65 | 0.878 |
| EM specialist | 0.99 | 0.35–2.77 | 0.984 |
| Overall complications† | |||
| Wearing of PPE | 1.36 | 0.87–2.13 | 0.173 |
| Level of the intubator * | |||
| Junior resident | Reference | ||
| Senior resident | 0.89 | 0.57–1.41 | 0.894 |
| EM specialist | 1.21 | 0.60–2.45 | 1.214 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.; Shin, T.G.; Park, J.E.; Lee, G.T.; Kim, Y.M.; Lee, S.A.; Kim, S.; Hwang, N.Y.; Hwang, S.Y. Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis. J. Clin. Med. 2021, 10, 1060. https://doi.org/10.3390/jcm10051060
Choi J, Shin TG, Park JE, Lee GT, Kim YM, Lee SA, Kim S, Hwang NY, Hwang SY. Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis. Journal of Clinical Medicine. 2021; 10(5):1060. https://doi.org/10.3390/jcm10051060
Chicago/Turabian StyleChoi, Jeonghyun, Tae Gun Shin, Jong Eun Park, Gun Tak Lee, Young Min Kim, Soo Ah Lee, Seonwoo Kim, Na Young Hwang, and Sung Yeon Hwang. 2021. "Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis" Journal of Clinical Medicine 10, no. 5: 1060. https://doi.org/10.3390/jcm10051060
APA StyleChoi, J., Shin, T. G., Park, J. E., Lee, G. T., Kim, Y. M., Lee, S. A., Kim, S., Hwang, N. Y., & Hwang, S. Y. (2021). Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis. Journal of Clinical Medicine, 10(5), 1060. https://doi.org/10.3390/jcm10051060







