Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI—Femoroacetabular Impingement: A Case–Control Study and Preliminary Report
Abstract
1. Introduction
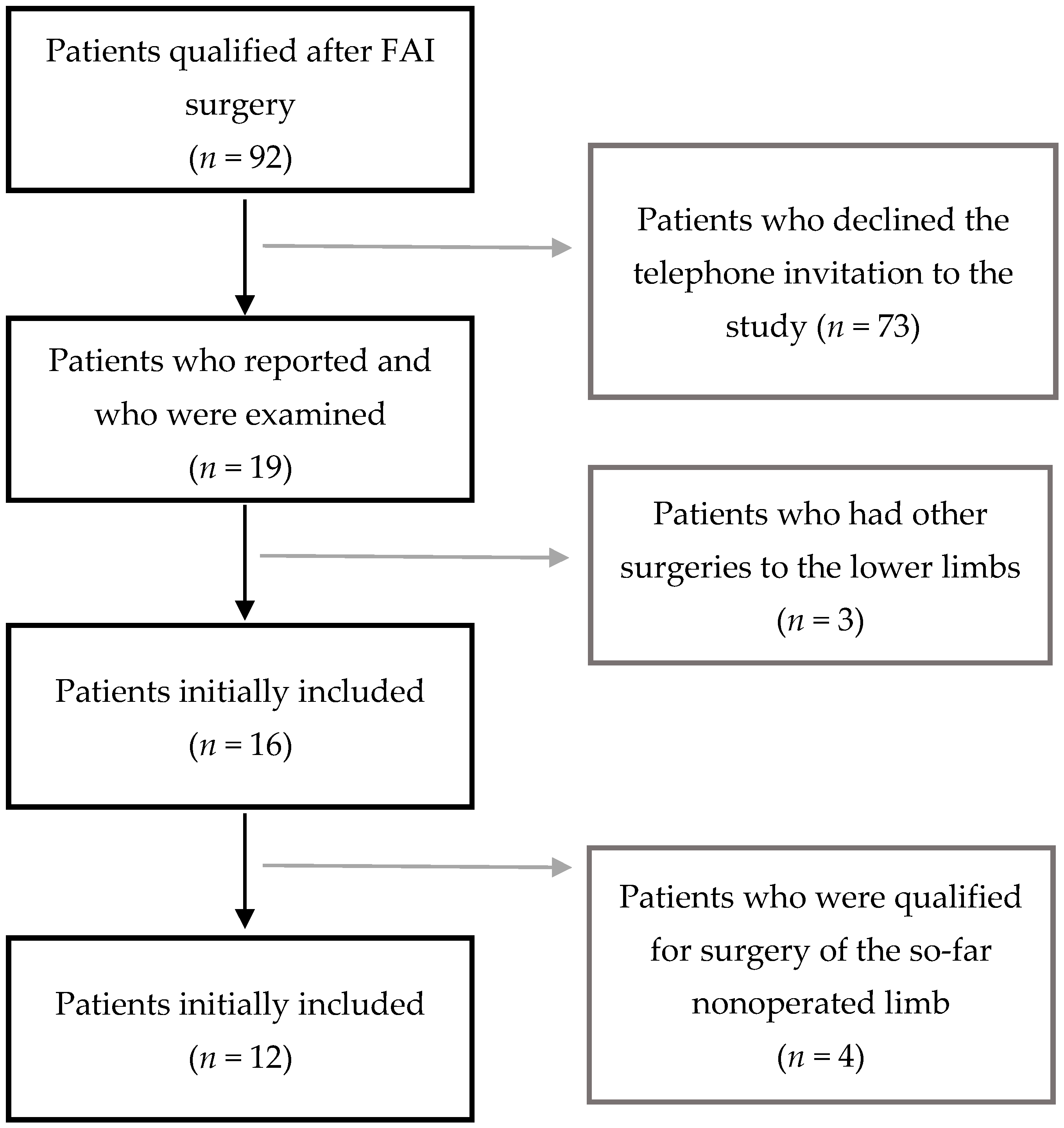
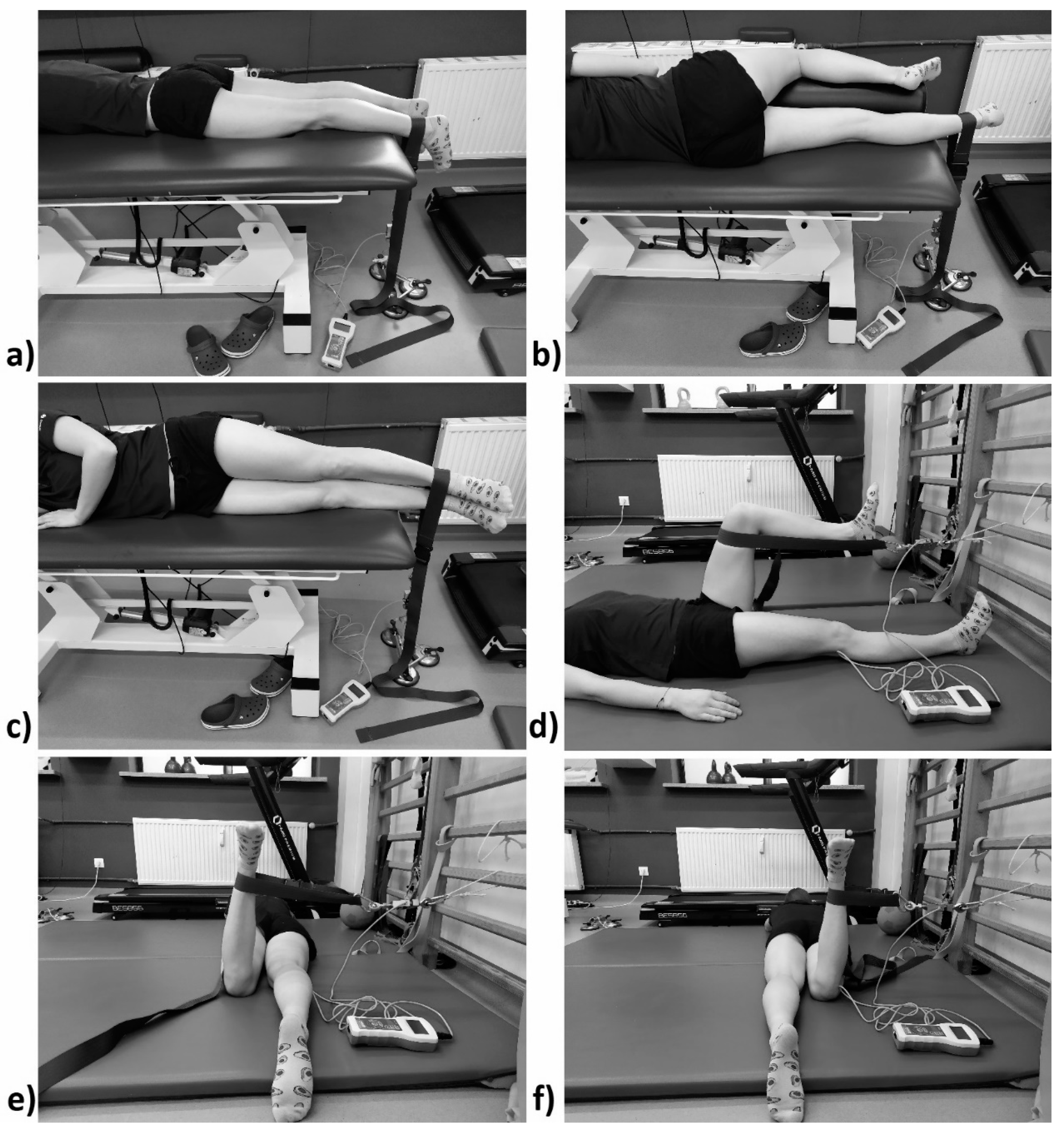
2. Materials and Methods
- The Short-Form Health Survey (SF-36) is used for the subjective assessment of patients’ quality of life. It comprises 36 statements. They are divided into 8 categories: physical functioning (PF), physical role functioning (RP), bodily pain (BP), general health perceptions (GH), emotional role functioning (RE), social role functioning (SF), mental health (MH), and vitality (VT). Question 2 on health transition (HT) within the past year was assessed separately. The categories were grouped into two components: physical component (PCS) and mental (MCS) mental component. The highest score for a question denoted the highest quality of life. The scores for each category were then calculated into points on a 0–100-point scale. The norm for the population was set at 50 points [12,13].
- The Harris Hip Score (HHS) is used to assess the functional state of the hip. It assesses the following: pain in the operated joints, range of motion, ability to move, ability to sit, and ability to put on shoes and socks. Each answer is adequately scored. The higher the score, the better the functional state. The maximum score is 100 points [14]. For the purposes of this study, results <70 were considered poor, results between 70 and 79 were considered fair, results between 80 and 89 were considered good, and results between 90 and 100 were considered excellent [15].
- We created a questionnaire on health and well-being for the purposes of this study. It supplements information that previous questionnaires lack. It contains inter alia questions on pain before and after surgery that is felt during daily life activities and during sports activities. Additionally, the subjects provided information on the frequency of sports activity, discomfort in the nonoperated limb, subjective improvement, and other orthopedic surgeries. All the questions were asked personally by the first author. Doubts or misunderstandings did not arise during the interview.
3. Results
3.1. Questionnaire Results
3.2. HHS Results
3.3. Quality of Life SF-36 Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin. Orthop. Relat. Res. 2003, 417, 112–120. [Google Scholar] [CrossRef]
- Kaczmarek, P. Obrazowanie w zakresie miednicy i stawów biodrowych. In Diagnostyka Obrazowa w Fizjoterapii i Rehabilitacji, 1st ed.; Sieroń, D., Ed.; PZWL Wydawnictwo Lekarskie: Warszawa, Poland, 2017; pp. 146–147. ISBN 978-83-200-5224-4. [Google Scholar]
- Leunig, M.; Azegami, S.; Kamath, A.; Ganz, R. Femoroacetabular Impingement: Definition, Etiology, and Pathophysiology. In Hip Arthroscopy and Hip Joint Preservation Surgery, 1st ed.; Nho, S., Leunig, M., Kelly, B., Bedi, A., Larson, C., Eds.; Springer: New York, NY, USA, 2014; pp. 1–10. ISBN 978-1-4614-7321-3. [Google Scholar]
- Larson, C.M.; Safran, M.R.; Brcka, D.A.; Vaughn, Z.D.; Giveans, M.R.; Stone, R.M. Predictors of Clinically Suspected Intra-articular Hip Symptoms and Prevalence of Hip Pathomorphologies Presenting to Sports Medicine and Hip Preservation Orthopaedic Surgeons. Arthroscopy 2018, 34, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Czubak, J.; Stępień, A. Obręcz biodrowa, staw biodrowy, udo. In Fizjoterapia w Ortopedii, 1st ed.; Białoszewski, D., Ed.; PZWL Wydawnictwo Lekarskie: Warszawa, Poland, 2014; pp. 254–257. ISBN 978-83-200-4802-5. [Google Scholar]
- Packer, J.D.; Safran, M.R. The etiology of primary femoroacetabular impingement: Genetics or acquired deformity? J. Hip Preserv. Surg. 2015, 2, 249–257. [Google Scholar] [CrossRef]
- Amanatullah, D.F.; Antkowiak, T.; Pillay, K.; Patel, J.; Refaat, M.; Toupadakis, C.A.; Jamali, A.A. Femoroacetabular impingement: Current concepts in diagnosis and treatment. Orthopedics 2015, 38, 185–199. [Google Scholar] [CrossRef]
- Grantham, W.J.; Philippon, M.J. Etiology and Pathomechanics of Femoroacetabular Impingement. Curr. Rev. Musculoskelet. Med. 2019, 12, 253–259. [Google Scholar] [CrossRef]
- Lerch, T.D.; Boschung, A.; Todorski, I.; Steppacher, S.D.; Schmaranzer, F.; Zheng, G.; Ryan, M.K.; Siebenrock, K.A.; Tannast, M. Femoroacetabular Impingement Patients with Decreased Femoral Version Have Different Impingement Locations and Intra- and Extraarticular Anterior Subspine FAI on 3D-CT-Based Impingement Simulation: Implications for Hip Arthroscopy. Am. J. Sports Med. 2019, 47, 3120–3132. [Google Scholar] [CrossRef]
- Lerch, T.D.; Siegfried, M.; Schmaranzer, F.; Leibold, C.S.; Zurmühle, C.A.; Hanke, M.S.; Ryan, M.K.; Steppacher, S.D.; Siebenrock, K.A.; Tannast, M. Location of Intra- and Extra-articular Hip Impingement Is Different in Patients with Pincer-Type and Mixed-Type Femoroacetabular Impingement Due to Acetabular Retroversion or Protrusio Acetabuli on 3D CT-Based Impingement Simulation. Am. J. Sports Med. 2020, 48, 661–672. [Google Scholar] [CrossRef]
- Zembaty, A. (Ed.) Szczegółowa metodyka badań i normy wybranych zakresów ruchów w stawie biodrowym. In Kinezyterapia, 1st ed.; Kasper: Kraków, Poland, 2002; Volume 1, pp. 425–427. ISBN 83-910437-4-6. [Google Scholar]
- McDowell, I. The Short-Form-36 health survey. In Measuring Health: A Guide to Rating Scales and Questionnaires; Oxford University Press: New York, NY, USA, 2006; ISBN 9780195165678. [Google Scholar]
- Turska, W.; Skowron, A. Metodyka oceny jakości życia. Farm. Pol. Czas. 2009, 65, 572–580. [Google Scholar]
- Kościelna, P.; Pogorzała, A.M. Badanie funkcjonalne stawu biodrowego w przypadku zmian zwyrodnieniowych. In Innowacyjność i Tradycja w Fizjoterapii; Borowicz, A.M., Ed.; Wyższa Szkoła Edukacji i Terapii w Poznaniu: Poznań, Poland, 2017; pp. 51–70. ISBN 978-83-941936-5-2. [Google Scholar]
- Kalairajah, Y.; Azurza, K.; Hulme, C.; Molloy, S.; Drabu, K.J. Health outcome measures in the evaluation of total hip arthroplasties—A comparison between the Harris hip score and the Oxford hip score. J. Arthroplast. 2005, 20, 1037–1041. [Google Scholar] [CrossRef]
- Botser, I.B.; Smith, T.W.J.; Nasser, R.; Domb, B.G. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: A comparison of clinical outcomes. Arthroscopy 2011, 27, 270–278. [Google Scholar] [CrossRef]
- Matsuda, D.K.; Carlisle, J.C.; Arthurs, S.C.; Wierks, C.H.; Philippon, M.J. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 2011, 27, 252–269. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Rebolledo, B.J.; McCormick, F.; Rosas, S.; Harris, J.D.; Kelly, B.T. Arthroscopic Versus Open Treatment of Femoroacetabular Impingement: A Systematic Review of Medium- to Long-Term Outcomes. Am. J. Sports Med. 2016, 44, 1062–1068. [Google Scholar] [CrossRef] [PubMed]
- Maupin, J.J.; Steinmetz, G.; Thakral, R. Management of femoroacetabular impingement syndrome: Current insights. Orthop. Res. Rev. 2019, 11, 99–108. [Google Scholar] [CrossRef]
- Kekatpure, A.L.; Ahn, T.; Kim, C.H.; Lee, S.J.; Yoon, K.S.; Yoon, P.W. Clinical Outcomes of an Initial 3-month Trial of Conservative Treatment for Femoroacetabular Impingement. Indian J. Orthop. 2017, 51, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Spiers, L.; Takla, A.; O’Donnell, J.; Kasza, J.; Hunter, D.J.; Hinman, R.S. Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: A randomised controlled trial (FAIR). BMJ Open 2017, 7, e014658. [Google Scholar] [CrossRef]
- Spencer-Gardner, L.; Eischen, J.J.; Levy, B.A.; Sierra, R.J.; Engasser, W.M.; Krych, A.J. A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 848–859. [Google Scholar] [CrossRef]
- Öhlin, A.; Ahldén, M.; Lindman, I.; Jónasson, P.; Desai, N.; Baranto, A.; Ayeni, O.R.; Sansone, M. Good 5-year outcomes after arthroscopic treatment for femoroacetabular impingement syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2019, 28, 1311–1316. [Google Scholar] [CrossRef]
- Beck, E.C.; Nwachukwu, B.U.; Kunze, K.N.; Chahla, J.; Nho, S.J. How Can We Define Clinically Important Improvement in Pain Scores After Hip Arthroscopy for Femoroacetabular Impingement Syndrome? Minimum 2-Year Follow-up Study. Am. J. Sports Med. 2019, 47, 3133–3140. [Google Scholar] [CrossRef]
- Kahlenberg, C.A.; Nwachukwu, B.U.; Schairer, W.W.; McCormick, F.; Ranawat, A.S. Patient Satisfaction Reporting for the Treatment of Femoroacetabular Impingement. Arthroscopy 2016, 32, 1693–1699. [Google Scholar] [CrossRef]
- Levy, D.M.; Kuhns, B.D.; Chahal, J.; Philippon, M.J.; Kelly, B.T.; Nho, S.J. Hip Arthroscopy Outcomes With Respect to Patient Acceptable Symptomatic State and Minimal Clinically Important Difference. Arthroscopy 2016, 32, 1877–1886. [Google Scholar] [CrossRef]
- Cheatham, S.W.; Enseki, K.R.; Kolber, M.J. Postoperative Rehabilitation after Hip Arthroscopy: A Search for the Evidence. J. Sport Rehabil. 2015, 24, 413–418. [Google Scholar] [CrossRef]
- Memon, M.; Kay, J.; Hache, P.; Simunovic, N.; Harris, J.D.; O’Donnell, J.; Ayeni, O.R. Athletes experience a high rate of return to sport following hip arthroscopy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3066–3104. [Google Scholar] [CrossRef]
- Frank, R.M.; Ukwuani, G.; Clapp, I.; Chahla, J.; Nho, S.J. High Rate of Return to Cycling After Hip Arthroscopy for Femoroacetabular Impingement Syndrome. Sports Health 2018, 10, 259–265. [Google Scholar] [CrossRef]
- Kemp, J.L.; Schache, A.G.; Makdissia, M.; Pritchard, M.G.; Sims, K.; Crossley, K.M. Is hip range of motion and strength impaired in people with hip chondrolabral pathology? J. Musculoskelet. Neuronal Interact. 2014, 14, 334–342. [Google Scholar]
- Freke, M.D.; Crossley, K.; Sims, K.; Russell, T.; Weinrauch, P.; Gamboa, G.; Semciw, A. Acute and Subacute Changes in Hip Strength and Range of Movement after Arthroscopy to Address Chondrolabral Pathology. Am. J. Sports Med. 2019, 47, 1939–1948. [Google Scholar] [CrossRef]
- Wörner, T.; Nilsson, J.; Thorborg, K.; Granlund, V.; Stålman, A.; Eek, F. Hip Function 6 to 10 Months After Arthroscopic Surgery: A Cross-sectional Comparison of Subjective and Objective Hip Function, Including Performance-Based Measures, in Patients Versus Controls. Orthop. J. Sports Med. 2019, 7. [Google Scholar] [CrossRef]
- Casartelli, N.C.; Maffiuletti, N.A.; Item-Glatthorn, J.F.; Impellizzeri, F.M.; Leunig, M. Hip muscle strength recovery after hip arthroscopy in a series of patients with symptomatic femoroacetabular impingement. Hip Int. 2014, 24, 387–393. [Google Scholar] [CrossRef]
- Tijssen, M.; van Cingel, R.; de Visser, E.; Nijhuis-van der Sanden, M. A clinical observational study on patient-reported outcomes, hip functional performance and return to sports activities in hip arthroscopy patients. Phys. Ther. Sport 2016, 20, 45–55. [Google Scholar] [CrossRef]


| Movement | Operated Limb | Nonoperated Limb | Difference | p |
|---|---|---|---|---|
| Flexion | 117.00 (±12.05) | 126.42 (±9.11) | 9.42 | 0.02 |
| Abduction | 17.50 (±4.68) | 21.17 (±6.31) | 3.67 | 0.01 |
| Adduction | 9.83 (±4.11) | 10.17 (±2.62) | 0.33 | 0.65 |
| Extension | 19.83 (±7.22) | 24.58 (±9.54) | 4.75 | 0.01 |
| Internal rotation | 26.50 (±17.55) | 32.17 (±15.16) | 5.67 | 0.10 |
| External rotation | 39.58 (±8.49) | 48.33 (±9.55) | 8.75 | 0.04 |
| Movement | Operated Limb | Nonoperated Limb | Difference | p |
|---|---|---|---|---|
| Extension | 185.58 (±85.92) | 210.43 (±88.28) | 24.85 | 0.002 |
| Abduction | 165.40 (±65.88) | 171.77 (±59.49) | 6.37 | 0.40 |
| Adduction | 160.12 (±71.68) | 180.95 (±61.98) | 20.83 | 0.02 |
| Flexion | 223.82 (±69.21) | 218.67 (±69.41) | −5.15 | 0.43 |
| Internal rotation | 109.80 (±45.00) | 105.50 (±39.27) | −4.30 | 0.43 |
| External rotation | 121.67 (±52.97) | 133.27 (±56.52) | 11.60 | 0.10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nieszporska, O.; Truszczyńska-Baszak, A. Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI—Femoroacetabular Impingement: A Case–Control Study and Preliminary Report. J. Clin. Med. 2021, 10, 1023. https://doi.org/10.3390/jcm10051023
Nieszporska O, Truszczyńska-Baszak A. Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI—Femoroacetabular Impingement: A Case–Control Study and Preliminary Report. Journal of Clinical Medicine. 2021; 10(5):1023. https://doi.org/10.3390/jcm10051023
Chicago/Turabian StyleNieszporska, Olga, and Aleksandra Truszczyńska-Baszak. 2021. "Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI—Femoroacetabular Impingement: A Case–Control Study and Preliminary Report" Journal of Clinical Medicine 10, no. 5: 1023. https://doi.org/10.3390/jcm10051023
APA StyleNieszporska, O., & Truszczyńska-Baszak, A. (2021). Functional Condition of Patients after Unilateral Hip Arthroscopy in the Process of FAI—Femoroacetabular Impingement: A Case–Control Study and Preliminary Report. Journal of Clinical Medicine, 10(5), 1023. https://doi.org/10.3390/jcm10051023







