Effects of Miosis on Anterior Chamber Structure in Glaucoma Implant Surgery
Abstract
:1. Introduction
2. Methods
2.1. Patients
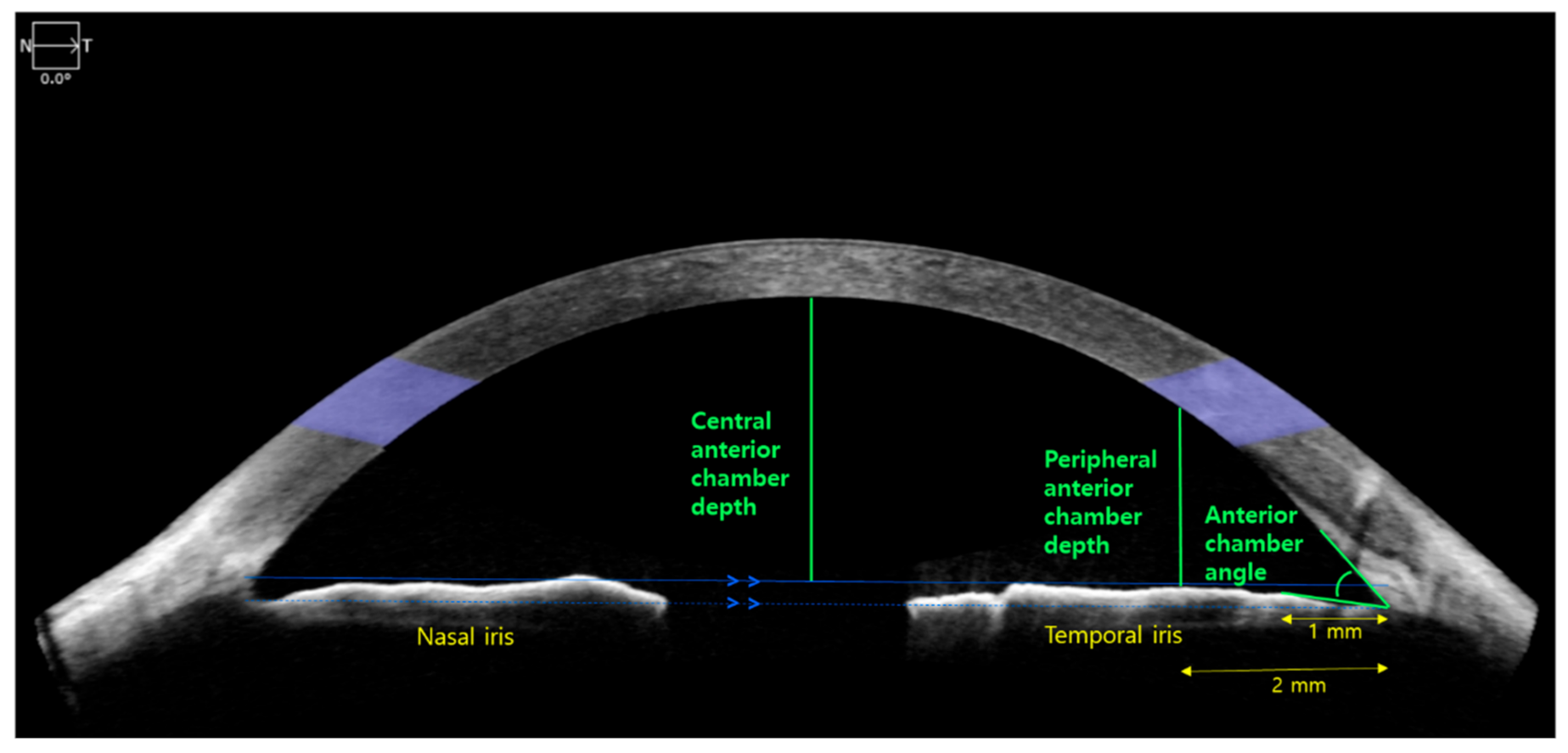
2.2. Anterior Segment Optical Coherence Tomography (AS-OCT)
2.3. Statistical Analysis
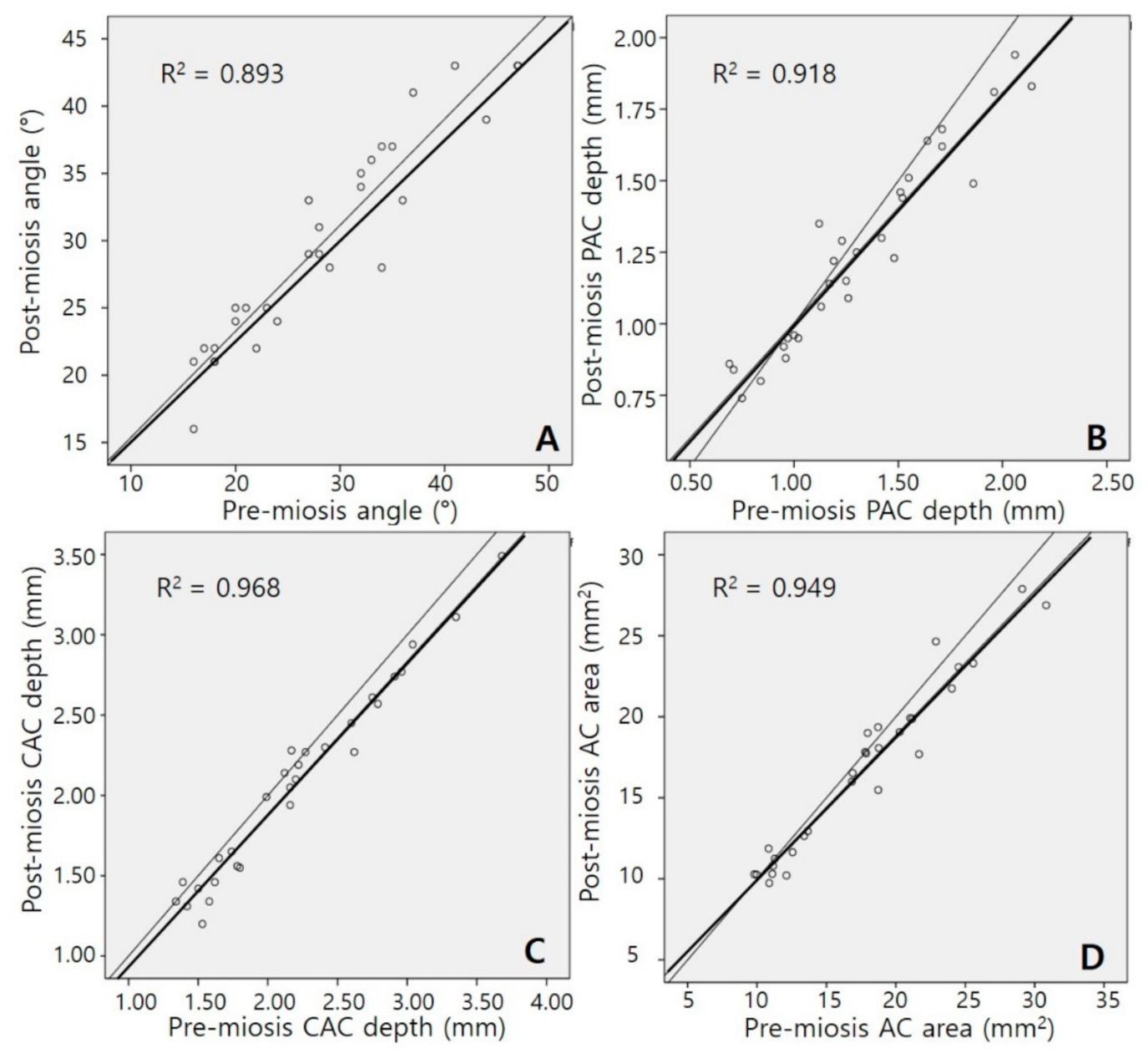
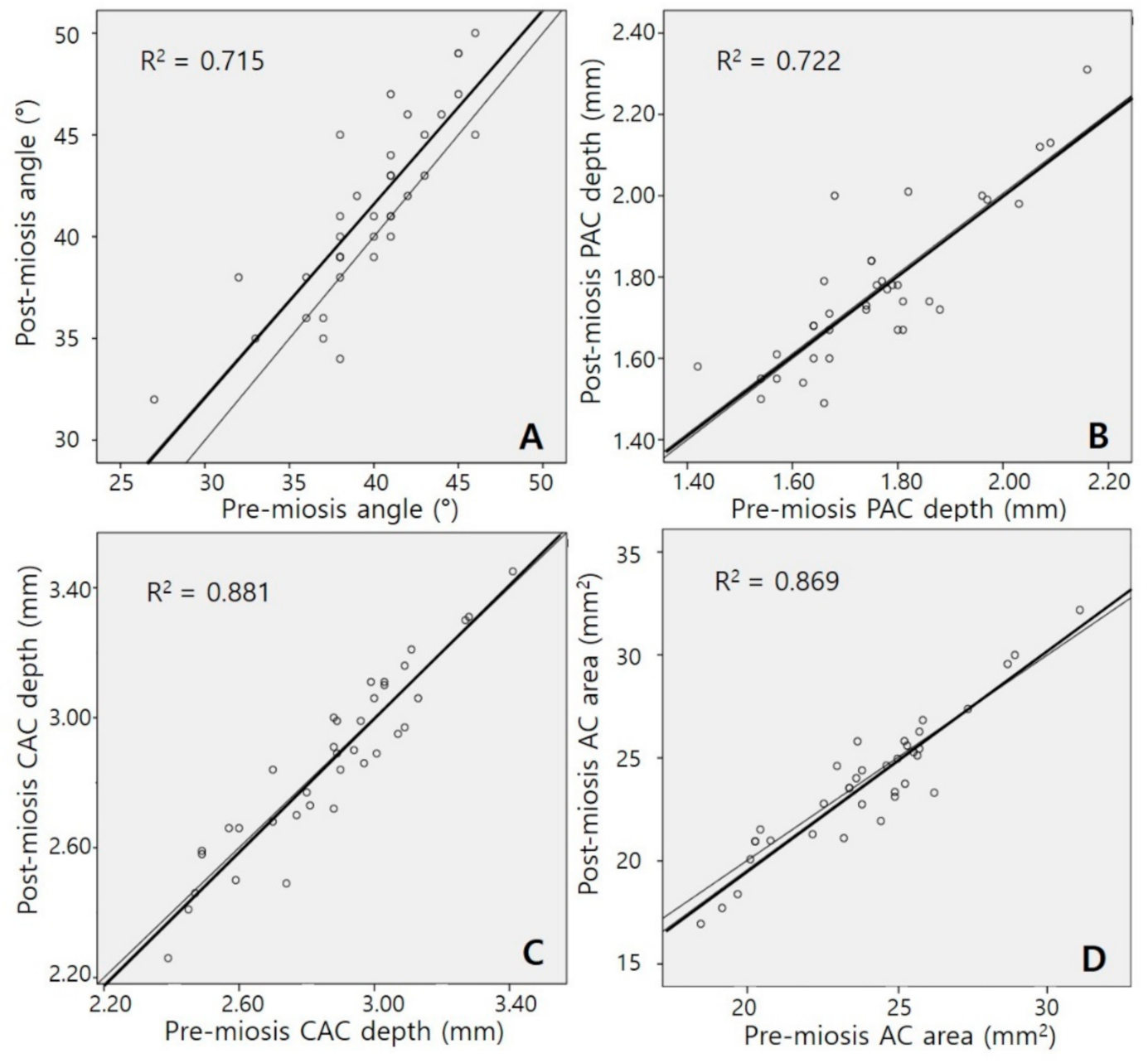
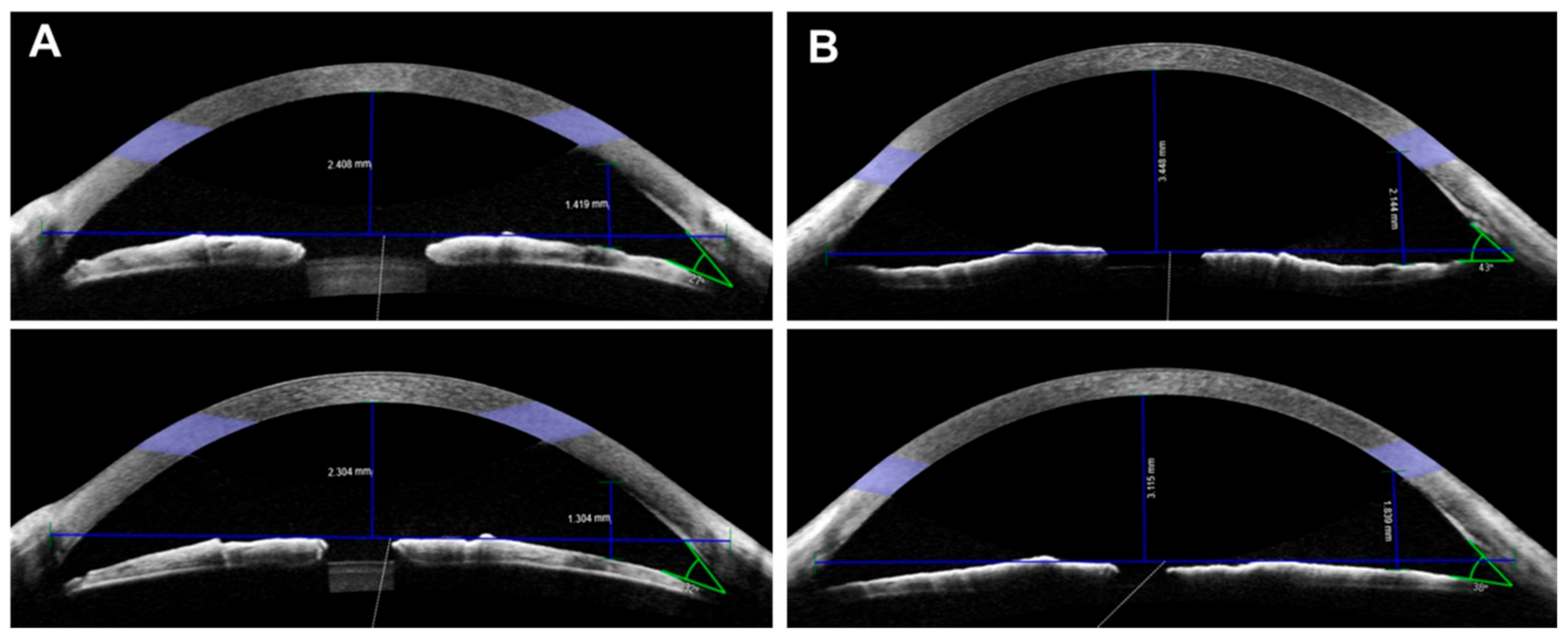
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grierson, I.; Lee, W.R.; Abraham, S. Effects of pilocarpine on the morphology of the human outflow apparatus. Br. J. Ophthalmol. 1978, 62, 302–313. [Google Scholar]
- Watson, P.; Barnett, F. Effectiveness of trabeculectomy in glaucoma. Am. J. Ophthalmol. 1975, 79, 831–845. [Google Scholar]
- Shaarawy, T. Glaucoma, Volume 2: Surgical Management; Saunders Ltd.: Wynnewood, PA, USA, 2009. [Google Scholar]
- Kim, J.; Lee, J.; Kee, C. Tissue incarceration after Ahmed valve implantation. J. Korean Ophthalmol. Soc. 2012, 53, 1053–1056. [Google Scholar]
- Gedde, S.J.; Schiffman, J.C.; Feuer, W.J.; Herndon, L.W.; Brandt, J.D.; Budenz, D.L.; Group, T.v.T.S. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am. J. Ophthalmol. 2012, 153, 789–803.e2. [Google Scholar]
- Minckler, D.S.; Francis, B.A.; Hodapp, E.A.; Jampel, H.D.; Lin, S.C.; Samples, J.R.; Smith, S.D.; Singh, K. Aqueous shunts in glaucoma: A report by the American Academy of Ophthalmology. Ophthalmology 2008, 115, 1089–1098. [Google Scholar]
- Arora, K.S.; Robin, A.L.; Corcoran, K.J.; Corcoran, S.L.; Ramulu, P.Y. Use of various glaucoma surgeries and procedures in Medicare beneficiaries from 1994 to 2012. Ophthalmology 2015, 122, 1615–1624. [Google Scholar]
- Byun, Y.S.; Lee, N.Y.; Park, C.K. Risk factors of implant exposure outside the conjunctiva after Ahmed glaucoma valve implantation. Jpn. J. Ophthalmol. 2009, 53, 114–119. [Google Scholar]
- Allingham, R.R.; Moroi, S.; Shields, M.B.; Damji, K. Shields’ Textbook of Glaucoma; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2020. [Google Scholar]
- Koo, E.B.; Hou, J.; Han, Y.; Keenan, J.D.; Stamper, R.L.; Jeng, B.H. Effect of glaucoma tube shunt parameters on cornea endothelial cells in patients with Ahmed valve implants. Cornea 2015, 34, 37–41. [Google Scholar]
- Tan, A.N.; Webers, C.A.; Berendschot, T.T.; de Brabander, J.; de Witte, P.M.; Nuijts, R.M.; Schouten, J.S.; Beckers, H.J. Corneal endothelial cell loss after Baerveldt glaucoma drainage device implantation in the anterior chamber. Acta Ophthalmol. 2017, 95, 91–96. [Google Scholar]
- Lee, H.M.; Kim, K.N.; Park, K.S.; Lee, N.H.; Lee, S.B.; Kim, C.-S. Relationship between Tube Parameters and Corneal Endothelial Cell Damage after Ahmed Glaucoma Valve Implantation: A Comparative Study. J. Clin. Med. 2020, 9, 2546. [Google Scholar]
- Poinoosawmy, D.; Nagasubramanian, S.; Brown, N. Effect of pilocarpine on visual acuity and on the dimensions of the cornea and anterior chamber. Br. J. Ophthalmol. 1976, 60, 676–679. [Google Scholar]
- Abramson, D.H.; Coleman, D.J.; Forbes, M.; Franzen, L.A. Pilocarpine: Effect on the anterior chamber and lens thickness. Arch. Ophthalmol. 1972, 87, 615–620. [Google Scholar]
- Koeppl, C.; Findl, O.; Menapace, R.; Kriechbaum, K.; Wirtitsch, M.; Buehl, W.; Sacu, S.; Drexler, W. Pilocarpine-induced shift of an accommodating intraocular lens: AT-45 Crystalens. J. Cataract Refract. Surg. 2005, 31, 1290–1297. [Google Scholar]
- Langenbucher, A.; Seitz, B.; Huber, S.; Nguyen, N.X.; Küchle, M. Theoretical and measured pseudophakic accommodation after implantation of a new accommodative posterior chamber intraocular lens. Arch. Ophthalmol. 2003, 121, 1722–1727. [Google Scholar]
- Kriechbaum, K.; Findl, O.; Koeppl, C.; Menapace, R.; Drexler, W. Stimulus-driven versus pilocarpine-induced biometric changes in pseudophakic eyes. Ophthalmology 2005, 112, 453–459. [Google Scholar]
- Lea, S.H.; Rubinstein, M.; Snead, M.; Haworth, S. Pseudophakic accommodation? A study of the stability of capsular bag supported, one piece, rigid tripod, or soft flexible implants. Br. J. Ophthalmol. 1990, 74, 22–25. [Google Scholar]
- Findl, O.; Kiss, B.; Petternel, V.; Menapace, R.; Georgopoulos, M.; Rainer, G.; Drexler, W. Intraocular lens movement caused by ciliary muscle contraction. J. Cataract Refract. Surg. 2003, 29, 669–676. [Google Scholar]
- Vinod, K.; Gedde, S.J.; Feuer, W.J.; Panarelli, J.F.; Chang, T.C.; Chen, P.P.; Parrish, R.K. Practice preferences for glaucoma surgery: A survey of the American Glaucoma Society. J. Glaucoma 2017, 26, 687. [Google Scholar]
- Hau, S.; Scott, A.; Bunce, C.; Barton, K. Corneal endothelial morphology in eyes implanted with anterior chamber aqueous shunts. Cornea 2011, 30, 50–55. [Google Scholar]
- Kim, J.-H.; Kim, C.-S. The change in corneal endothelial cells after ahmed glaucoma valve implantation. J. Korean Ophthalmol. Soc. 2006, 47, 1972–1980. [Google Scholar]
- Lee, E.-K.; Yun, Y.-J.; Lee, J.-E.; Yim, J.-H.; Kim, C.-S. Changes in corneal endothelial cells after Ahmed glaucoma valve implantation: 2-year follow-up. Am. J. Ophthalmol. 2009, 148, 361–367. [Google Scholar]
- Park, H.L.; Jung, K.; Park, C. Serial intracameral visualization of the Ahmed glaucoma valve tube by anterior segment optical coherence tomography. Eye 2012, 26, 1256–1262. [Google Scholar]
- Seo, J.W.; Lee, J.Y.; Nam, D.H.; Lee, D.Y. Comparison of the changes in corneal endothelial cells after pars plana and anterior chamber ahmed valve implant. J. Ophthalmol. 2015, 2015, 486832. [Google Scholar]
- Gandham, S.B.; Costa, V.P.; Katz, L.J.; Wilson, R.P.; Sivalingam, A.; Belmont, J.; Smith, M. Aqueous tube-shunt implantation and pars plana vitrectomy in eyes with refractory glaucoma. Am. J. Ophthalmol. 1993, 116, 189–195. [Google Scholar]
- Faghihi, H.; Hajizadeh, F.; Mohammadi, S.F.; Kadkhoda, A.; Peyman, G.A.; Riazi-Esfahani, M. Pars plana Ahmed valve implant and vitrectomy in the management of neovascular glaucoma. Ophthalmic Surg. Lasers Imaging Retin. 2007, 38, 292–300. [Google Scholar]
- Weiner, A.; Cohn, A.D.; Balasubramaniam, M.; Weiner, A.J. Glaucoma tube shunt implantation through the ciliary sulcus in pseudophakic eyes with high risk of corneal decompensation. J. Glaucoma 2010, 19, 405–411. [Google Scholar]
- Eslami, Y.; Mohammadi, M.; Fakhraie, G.; Zarei, R.; Moghimi, S. Ahmed glaucoma valve implantation with tube insertion through the ciliary sulcus in pseudophakic/aphakic eyes. J. Glaucoma 2014, 23, 115–118. [Google Scholar]
- Drugs.com. Available online: https://www.drugs.com/ppa/pilocarpine-ophthalmic.html (accessed on 17 August 2020).
- Rękas, M.; Barchan-Kucia, K.; Konopińska, J.; Mariak, Z.; Żarnowski, T. Analysis and modeling of anatomical changes of the anterior segment of the eye after cataract surgery with consideration of different phenotypes of eye structure. Curr. Eye Res. 2015, 40, 1018–1027. [Google Scholar]
- Olsen, T. Prediction of the effective postoperative (intraocular lens) anterior chamber depth. J. Cataract Refract. Surg. 2006, 32, 419–424. [Google Scholar]
- Memarzadeh, F.; Tang, M.; Li, Y.; Chopra, V.; Francis, B.A.; Huang, D. Optical coherence tomography assessment of angle anatomy changes after cataract surgery. Am. J. Ophthalmol. 2007, 144, 464–465. [Google Scholar]
- Shin, H.C.; Subrayan, V.; Tajunisah, I. Changes in anterior chamber depth and intraocular pressure after phacoemulsification in eyes with occludable angles. J. Cataract Refract. Surg. 2010, 36, 1289–1295. [Google Scholar]
- Altan, C.; Bayraktar, S.; Altan, T.; Eren, H.; Yilmaz, O.F. Anterior chamber depth, iridocorneal angle width, and intraocular pressure changes after uneventful phacoemulsification in eyes without glaucoma and with open iridocorneal angles. J. Cataract Refract. Surg. 2004, 30, 832–838. [Google Scholar]
- Huang, G.; Gonzalez, E.; Peng, P.-H.; Lee, R.; Leeungurasatien, T.; He, M.; Porco, T.; Lin, S.C. Anterior chamber depth, iridocorneal angle width, and intraocular pressure changes after phacoemulsification: Narrow vs open iridocorneal angles. Arch. Ophthalmol. 2011, 129, 1283–1290. [Google Scholar]
| Phakia Group (n = 29) | Pseudophakia Group (n = 36) | p-Value * | |
|---|---|---|---|
| Age (years) | 62.1 ± 12.9 | 64.8 ± 13.9 | 0.419 |
| Sex (male/female) | 13/16 | 20/16 | 0.459 † |
| Diabetes mellitus (n) | 8 (27.6%) | 17 (47.2%) | 0.129 † |
| Hypertension (n) | 10 (34.5%) | 16 (44.4%) | 0.455 † |
| Type of glaucoma (n) | |||
| Primary open-angle | 11 | 14 | |
| Primary angle-closure | 7 | 5 | |
| Uveitic | 3 | 4 | |
| Neovascular | 5 | 9 | |
| Pseudoexfoliation | 3 | 4 | |
| Axial length (mm) | 23.4 ± 1.4 | 23.8 ± 1.2 | 0.180 |
| Anterior chamber depth (mm) | 3.0 ± 0.6 | 4.3 ± 0.7 | <0.001 |
| Keratometry (diopter) | 44.7 ± 1.8 | 44.1 ± 1.5 | 0.131 |
| Central corneal thickness (um) | 536.5 ± 30.1 | 538.8 ± 24.3 | 0.729 |
| Spherical equivalent (diopter) | −0.6 ± 3.6 | −0.9 ± 1.2 | 0.695 |
| Phakia Group (n = 29) | Pseudophakia Group (n = 36) | p-Value * | |
|---|---|---|---|
| Pre-miosis | |||
| Anterior chamber angle (°) | 28.4 ± 9.3 | 39.7 ± 4.0 | <0.001 |
| Peripheral anterior chamber depth (mm) | 1.31 ± 0.40 | 1.76 ± 0.17 | <0.001 |
| Central anterior chamber depth (mm) | 2.20 ± 0.62 | 2.86 ± 0.25 | <0.001 |
| Anterior chamber area (mm2) | 17.63 ± 5.87 | 23.97 ± 2.83 | <0.001 |
| Post-miosis | |||
| Anterior chamber angle (°) | 29.90 ± 7.77 | 41.33 ± 4.46 | <0.001 |
| Peripheral anterior chamber depth (mm) | 1.26 ± 0.34 | 1.77 ± 0.19 | <0.001 |
| Central anterior chamber depth (mm) | 2.07 ± 0.60 | 2.86 ± 0.27 | <0.001 |
| Anterior chamber area (mm2) | 16.76 ± 5.36 | 23.78 ± 3.24 | <0.001 |
| Differences † | |||
| Anterior chamber angle (°) | 1.48 ± 3.21 (0.019) | 1.64 ± 2.39 (<0.001) | 0.823 |
| Peripheral anterior chamber depth (mm) | −0.06 ± 0.13 (0.571) | −0.003 ± 0.089 (0.590) | 0.043 |
| Central anterior chamber depth (mm) | −0.12 ± 0.11 (<0.001) | −0.004 ± 0.095 (0.784) | <0.001 |
| Anterior chamber area (mm2) | −0.88 ± 1.38 (0.02) | −0.19 ± 1.19 (0.335) | 0.036 |
| Enhancement | Reduction | p-Value | |
|---|---|---|---|
| Anterior chamber angle | |||
| Phakia group (n) | 23 | 6 | 0.678 |
| Pseudophakia group (n) | 30 | 6 | |
| Peripheral anterior chamber depth | |||
| Phakia group (n) | 7 | 22 | 0.019 |
| Pseudophakia group (n) | 19 | 17 | |
| Central anterior chamber depth | |||
| Phakia group (n) | 4 | 25 | 0.002 |
| Pseudophakia group (n) | 19 | 17 | |
| Anterior chamber area | |||
| Phakia group (n) | 7 | 22 | 0.019 |
| Pseudophakia group (n) | 19 | 17 | |
| Phakia Group (n = 29) | Pseudophakia Group (n = 36) | ||||
|---|---|---|---|---|---|
| Anterior Chamber Angle | Anterior Chamber Angle | ||||
| Enhancement | Reduction | Enhancement | Reduction | ||
| Central anterior chamber depth | Enhancement | 4 (13.8%) | 0 | 19 (52.8%) | 0 |
| Reduction | 19 (65.5%) | 6 (20.7%) | 11 (30.6%) | 6 (16.6%) | |
| p-value | 0.004 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, K.S.; Kim, K.N.; Kim, J.; Lee, Y.H.; Lee, S.B.; Kim, C.-s. Effects of Miosis on Anterior Chamber Structure in Glaucoma Implant Surgery. J. Clin. Med. 2021, 10, 1017. https://doi.org/10.3390/jcm10051017
Park KS, Kim KN, Kim J, Lee YH, Lee SB, Kim C-s. Effects of Miosis on Anterior Chamber Structure in Glaucoma Implant Surgery. Journal of Clinical Medicine. 2021; 10(5):1017. https://doi.org/10.3390/jcm10051017
Chicago/Turabian StylePark, Kee Sup, Kyoung Nam Kim, Jaeyoung Kim, Yeon Hee Lee, Sung Bok Lee, and Chang-sik Kim. 2021. "Effects of Miosis on Anterior Chamber Structure in Glaucoma Implant Surgery" Journal of Clinical Medicine 10, no. 5: 1017. https://doi.org/10.3390/jcm10051017
APA StylePark, K. S., Kim, K. N., Kim, J., Lee, Y. H., Lee, S. B., & Kim, C.-s. (2021). Effects of Miosis on Anterior Chamber Structure in Glaucoma Implant Surgery. Journal of Clinical Medicine, 10(5), 1017. https://doi.org/10.3390/jcm10051017






