Assessment of Disability Progression Independent of Relapse and Brain MRI Activity in Patients with Multiple Sclerosis in Poland
Abstract
1. Introduction
2. Materials and Methods
Confirmed Disability Progression
3. Results
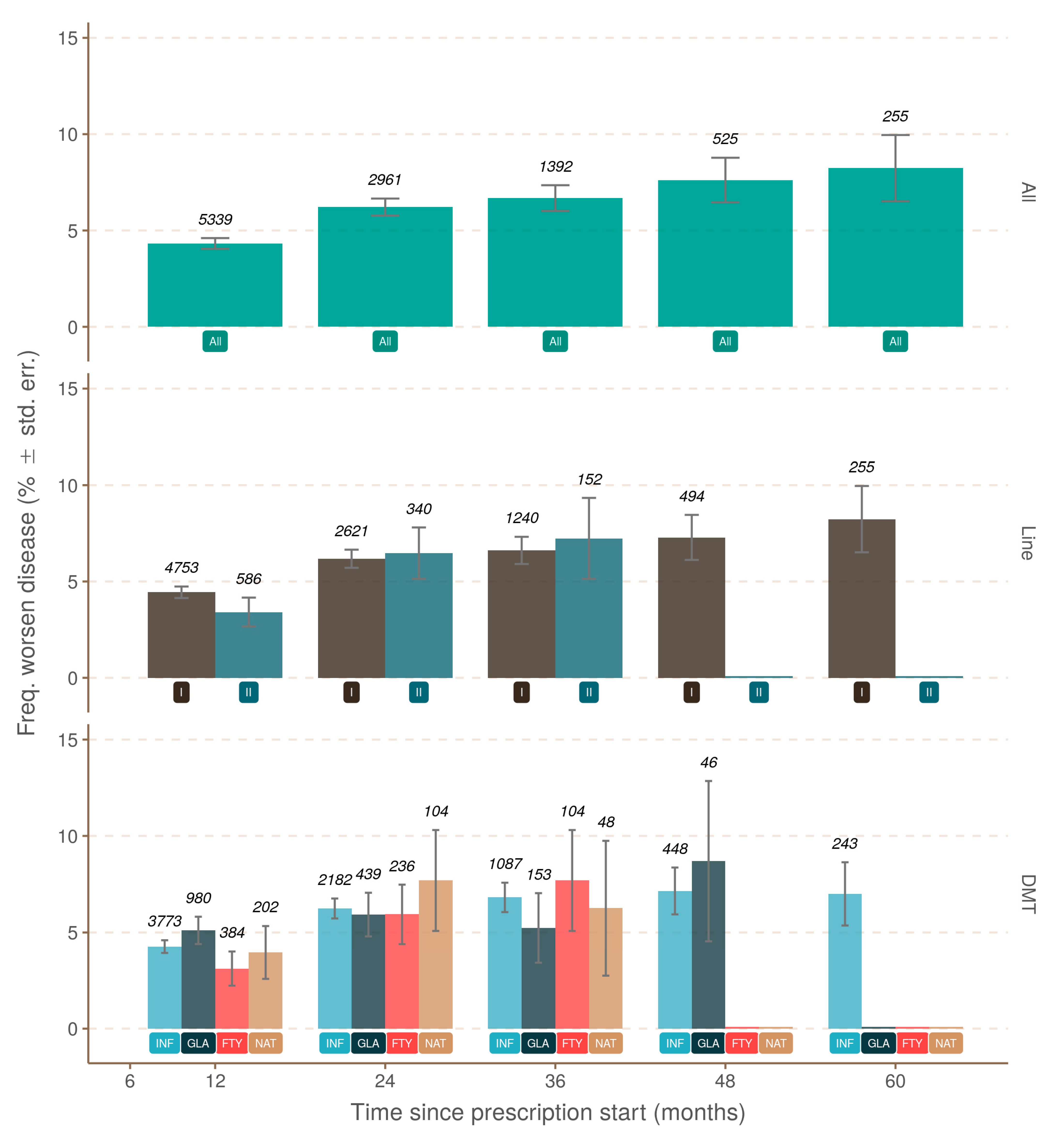
3.1. Progression Independent of Relapse Activity (PIRA)
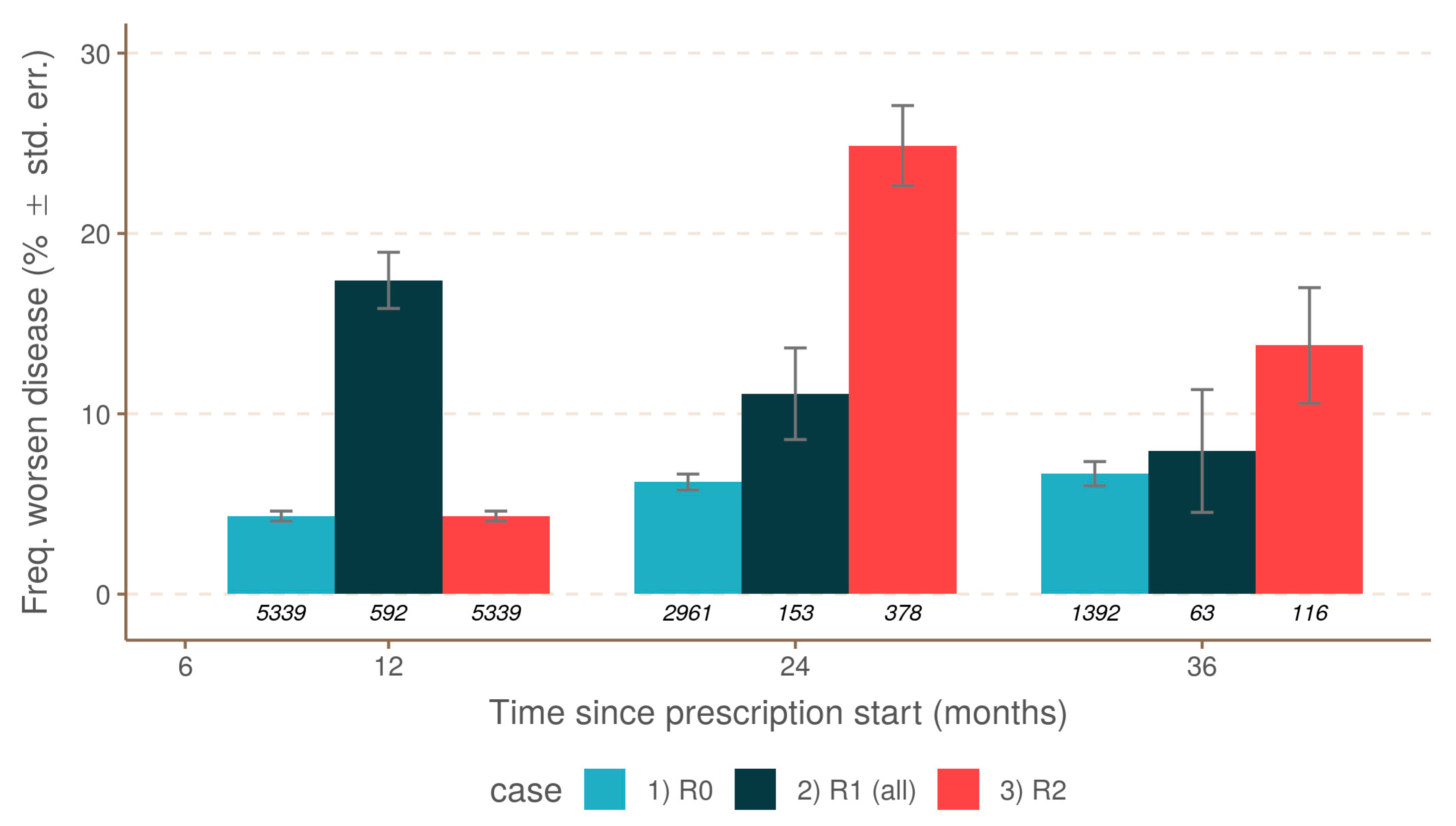
3.2. Relapse-Associated Worsening (RAW)
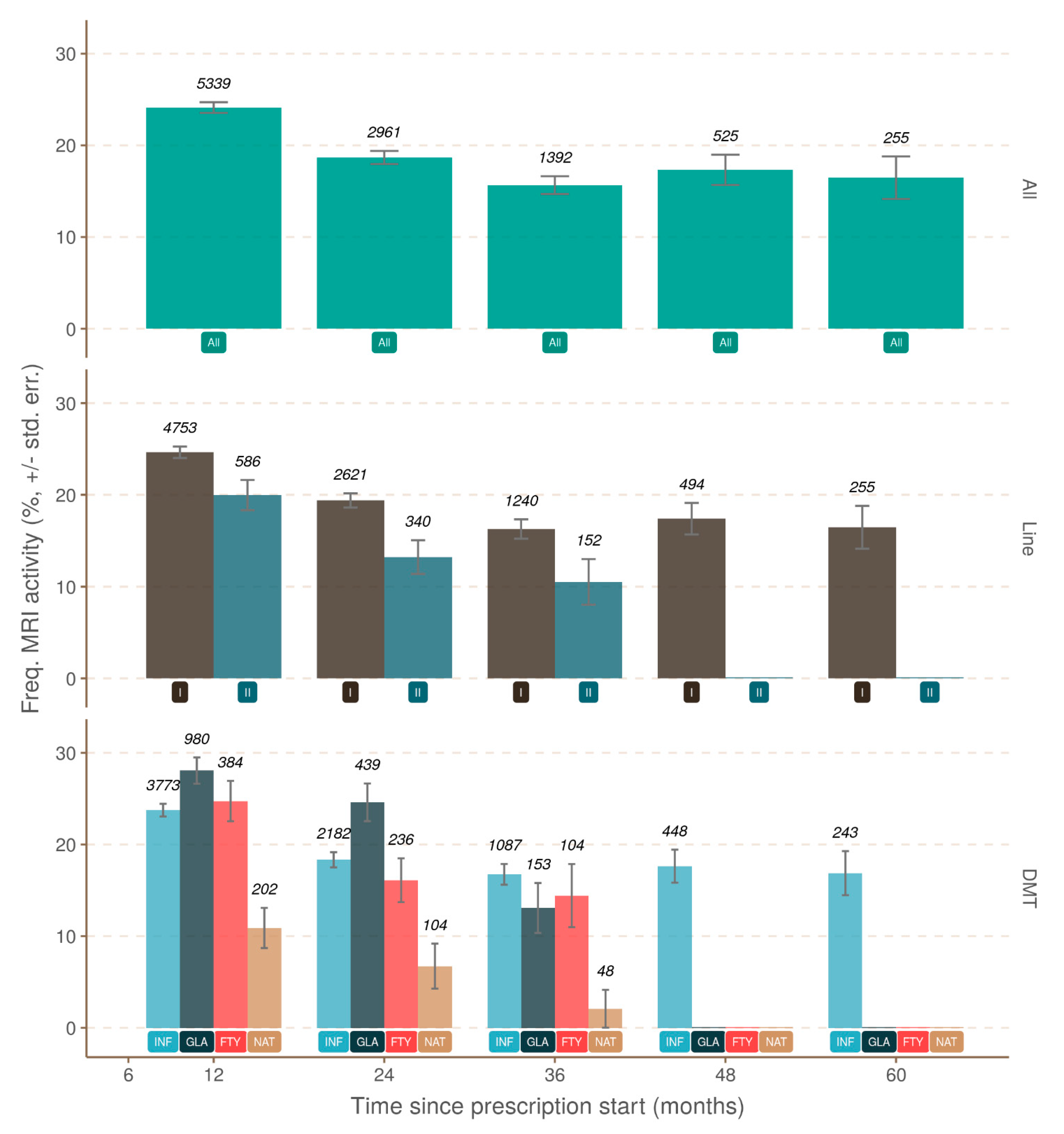
3.3. Progression Independent of Brain MRI Activity
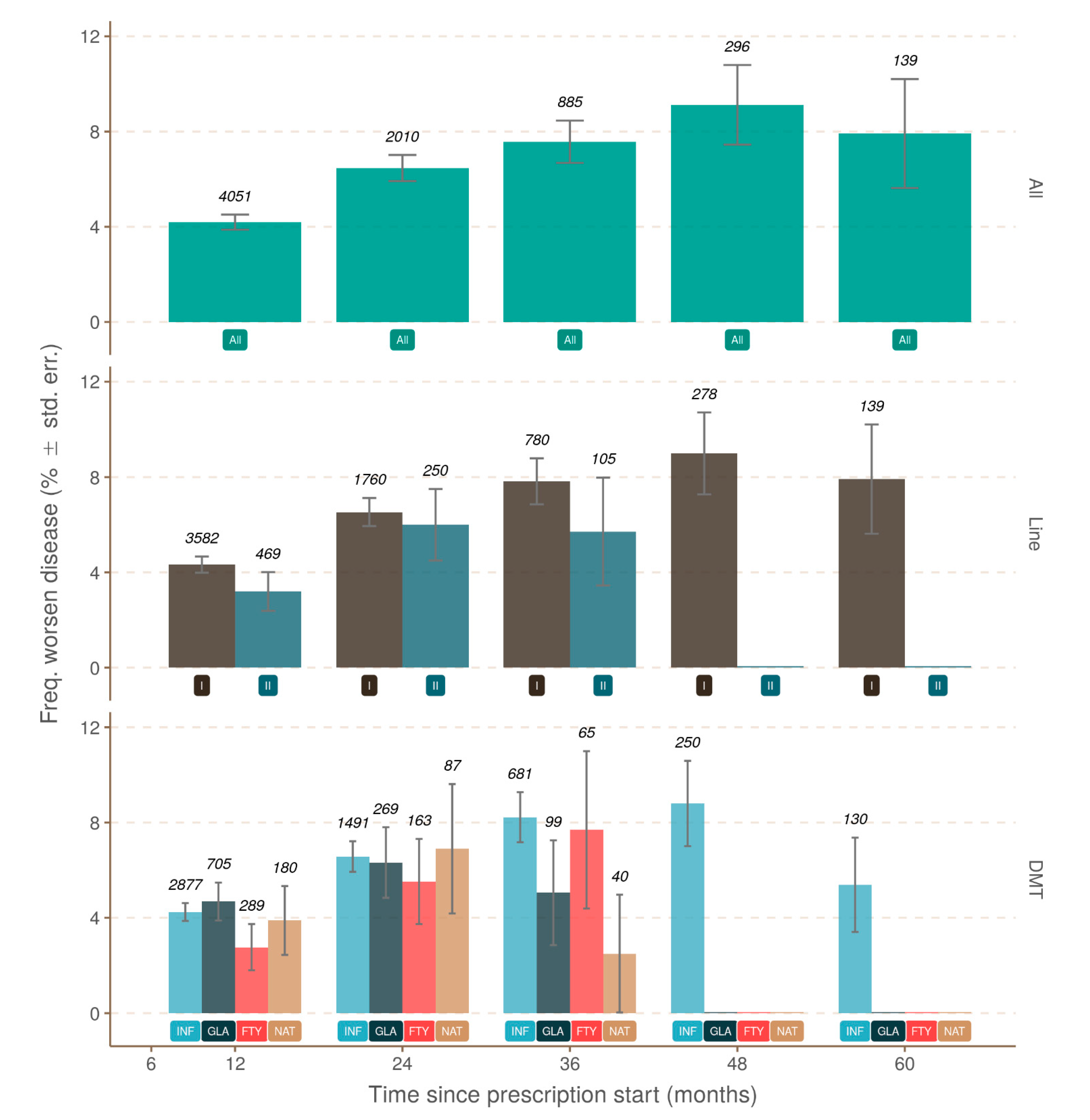
3.4. Progression Independent of Relapse and Brain MRI Activity (PIRMA)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; Van Der Mei, I.; et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444. [Google Scholar] [CrossRef] [PubMed]
- Kappos, L.; Butzkueven, H.; Wiendl, H.; Spelman, T.; Pellegrini, F.; Chen, Y.; Dong, Q.; Koendgen, H.; Belachew, S.; Trojano, M.; et al. Greater sensitivity to multiple sclerosis disability worsening and progression events using a roving versus a fixed reference value in a prospective cohort study. Mult. Scler. J. 2017, 24, 963–973. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Baier, M.; Cutter, G. Effect of relapses on development of residual deficit in multiple sclerosis. Neurology 2003, 61, 1528–1532. [Google Scholar] [CrossRef]
- Cree, B.A.C.; Hollenbach, J.A.; Bove, R.; Kirkish, G.; Sacco, S.; Caverzasi, E.; Bischof, A.; Gundel, T.; Zhu, A.H.; Papinutto, N.; et al. Silent progression in disease activity–free relapsing multiple sclerosis. Ann. Neurol. 2019, 85, 653–666. [Google Scholar] [CrossRef]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sørensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F.; et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef]
- Kappos, L.; Wolinsky, J.S.; Giovannoni, G.; Arnold, D.L.; Wang, Q.; Bernasconi, C.; Model, F.; Koendgen, H.; Manfrini, M.; Belachew, S.; et al. Contribution of Relapse-Independent Progression vs Relapse-Associated Worsening to Overall Confirmed Disability Accumulation in Typical Relapsing Multiple Sclerosis in a Pooled Analysis of 2 Randomized Clinical Trials. JAMA Neurol. 2020, 77, 1132. [Google Scholar] [CrossRef]
- Kapica-Topczewska, K.; Tarasiuk, J.; Collin, F.; Brola, W.; Chorąży, M.; Czarnowska, A.; Kwaśniewski, M.; Bartosik-Psujek, H.; Adamczyk-Sowa, M.; Kochanowicz, J.; et al. The effectiveness of interferon beta versus glatiramer acetate and natalizumab versus fingolimod in a Polish real-world population. PLoS ONE 2019, 14, e0223863. [Google Scholar] [CrossRef] [PubMed]
- Kapica-Topczewska, K.; Collin, F.; Tarasiuk, J.; Chorąży, M.; Czarnowska, A.; Kwaśniewski, M.; Brola, W.; Bartosik-Psujek, H.; Adamczyk-Sowa, M.; Kochanowicz, J.; et al. Clinical and epidemiological characteristics of multiple sclerosis patients receiving disease-modifying treatment in Poland. Neurol. Neurochir. Polska 2020, 54, 161–168. [Google Scholar] [CrossRef]
- Sąsiadek, M.; Katulska, K.; Majos, A.; Siger, M.; Hartel, M.; Kalinowska, A.; Walecki, J. Guidelines of the Polish Medical Society of radiology for the routinely used MRI protocol in patients with multiple sclerosis. Neurol. Neurochir. Polska 2018, 52, 638–642. [Google Scholar] [CrossRef]
- Ness, N.-H.; Schriefer, D.; Haase, R.; Ettle, B.; Cornelissen, C.; Ziemssen, T. Differentiating societal costs of disability worsening in multiple sclerosis. J. Neurol. 2019, 267, 1035–1042. [Google Scholar] [CrossRef]
- Kapica-Topczewska, K.; Brola, W.; Fudala, M.; Tarasiuk, J.; Chorazy, M.; Snarska, K.; Kochanowicz, J.; Kulakowska, A. Prevalence of multiple sclerosis in Poland. Mult. Scler. Relat. Disord. 2018, 21, 51–55. [Google Scholar] [CrossRef]
- Czarnowska, A.; Kapica-Topczewska, K.; Zajkowska, O.; Świerzbińska, R.; Chorąży, M.; Tarasiuk, J.; Zajkowska, J.; Kochanowicz, J.; Kułakowska, A. Herpesviridae Seropositivity in Patients with Multiple Sclerosis: First Polish Study. Eur. Neurol. 2018, 80, 229–235. [Google Scholar] [CrossRef]
- Confavreux, C.; Vukusic, S.; Moreau, T.; Adeleine, P. Relapses and Progression of Disability in Multiple Sclerosis. N. Engl. J. Med. 2000, 343, 1430–1438. [Google Scholar] [CrossRef]
- Confavreux, C.; Vukusic, S.; Adeleine, P. Early clinical predictors and progression of irreversible disability in multiple sclerosis: An amnesic process. Brain 2003, 126, 770–782. [Google Scholar] [CrossRef]
- Tremlett, H.; Yousefi, M.; Devonshire, V.; Rieckmann, P.; Zhao, Y.; Neurologists, U.B.C. Impact of multiple sclerosis relapses on progression diminishes with time. Neurology 2009, 73, 1616–1623. [Google Scholar] [CrossRef]
- Leray, E.; Yaouanq, J.; Le Page, E.; Coustans, M.; Laplaud, D.; Oger, J.; Edan, G. Evidence for a two-stage disability progression in multiple sclerosis. Brain 2010, 133, 1900–1913. [Google Scholar] [CrossRef]
- Eriksson, M.; Andersen, O.; Runmarker, B. Long-term follow up of patients with clinically isolated syndromes, relapsing-remitting and secondary progressive multiple sclerosis. Mult. Scler. J. 2003, 9, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Scalfari, A.; Neuhaus, A.; Degenhardt, A.; Rice, G.P.; Muraro, P.A.; Daumer, M.; Ebers, G.C. The natural history of multiple sclerosis: A geographically based study 10: Relapses and long-term disability. Brain 2010, 133, 1914–1929. [Google Scholar] [CrossRef] [PubMed]
- Scott, T.F.; Schramke, C.J. Poor recovery after the first two attacks of multiple sclerosis is associated with poor outcome five years later. J. Neurol. Sci. 2010, 292, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Jokubaitis, V.G.; Spelman, T.; Kalincik, T.; Lorscheider, J.; Havrdova, E.; Horakova, D.; Duquette, P.; Girard, M.; Prat, A.; Izquierdo, G.; et al. Predictors of long-term disability accrual in relapse-onset multiple sclerosis. Ann. Neurol. 2016, 80, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Brex, P.A.; Ciccarelli, O.; O’Riordan, J.I.; Sailer, M.; Thompson, A.J.; Miller, D.H. A longitudinal study of abnormalities on MRI and disability from multiple sclerosis. N. Eng. J. Med. 2002, 346, 158–164. [Google Scholar] [CrossRef]
- Fisniku, L.K.; Brex, P.A.; Altmann, D.R.; Miszkiel, K.A.; Benton, C.E.; Lanyon, R.; Thompson, A.J.; Miller, D.H. Disability and T2 MRI lesions: A 20-year follow-up of patients with relapse onset of multiple sclerosis. Brain 2008, 131, 808–817. [Google Scholar] [CrossRef]
- Barkhof, F. MRI in multiple sclerosis: Correlation with expanded disability status scale (EDSS). Mult. Scler. 1999, 5, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Barkhof, F. The clinico-radiological paradox in multiple sclerosis revisited. Curr. Opin. Neurol. 2002, 15, 239–245. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, N.; Giorgio, A.; Battaglini, M.; Rovaris, M.; Sormani, M.P.; Barkhof, F.; Korteweg, T.; Enzinger, C.; Fazekas, F.; Calabrese, M.; et al. Assessing brain atrophy rates in a large population of untreated multiple sclero-sis subtypes. Neurology 2010, 74, 1868–1876. [Google Scholar] [CrossRef]
- Tiberio, M.; Chard, D.; Altmann, D.R.; Davies, G.; Griffin, C.M.; Rashid, W.; Sastre-Garriga, J.; Thompson, A.J.; Miller, D.H. Gray and white matter volume changes in early RRMS: A 2-year longitudinal study. Neurology 2005, 64, 1001–1007. [Google Scholar] [CrossRef] [PubMed]
- Filippi, M.; Rocca, M.A. Classifying silent progression in relapsing–remitting MS. Nat. Rev. Neurol. 2019, 15, 315–316. [Google Scholar] [CrossRef]
- Tremlett, H.; Zhao, Y.; Devonshire, V. Natural history of secondary-progressive multiple sclerosis. Mult. Scler. J. 2008, 14, 314–324. [Google Scholar] [CrossRef]
- Confavreux, C.; Vukusic, S. Age at disability milestones in multiple sclerosis. Brain 2006, 129, 595–605. [Google Scholar] [CrossRef]
- Scalfari, A.; Neuhaus, A.; Daumer, M.; Ebers, G.C.; Muraro, P.A. Age and disability accumulation in multiple sclerosis. Neurology 2011, 77, 1246–1252. [Google Scholar] [CrossRef]
- Lorscheider, J.; Buzzard, K.; Jokubaitis, V.; Spelman, T.; Havrdova, E.; Horakova, D.; Trojano, M.; Izquierdo, G.; Girard, M.; Duquette, P.; et al. Defining secondary progressive multiple sclerosis. Brain 2016, 139, 2395–2405. [Google Scholar] [CrossRef]
- Brown, J.W.L.; Coles, A.; Horakova, D.; Havrdova, E.; Izquierdo, G.; Prat, A.; Girard, M.; Duquette, P.; Trojano, M.; Lugaresi, A.; et al. Association of initial disease-modifying therapy with later conversion to secondary progressive multiple sclerosis. JAMA 2019, 321, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Cree, B.A.C.; Hauser, S.L. Reply to “Silent Progression or Bout Onset Progressive Multiple Sclerosis?”. Ann. Neurol. 2019, 86, 472–473. [Google Scholar] [CrossRef]
- Kappos, L.; Bar-Or, A.; Cree, B.A.C.; Fox, R.J.; Giovannoni, G.; Gold, R.; Vermersch, P.; Arnold, D.L.; Arnould, S.; Scherz, T.; et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): A double-blind, randomised, phase 3 study. Lancet 2018, 391, 1263–1273. [Google Scholar] [CrossRef]
- Boziki, M.K.; Kesidou, E.; Theotokis, P.; Mentis, A.-F.A.; Karafoulidou, E.; Melnikov, M.; Sviridova, A.; Rogovski, V.; Boyko, A.; Grigoriadis, N. Microbiome in Multiple Sclerosis: Where Are We, What We Know and Do Not Know. Brain Sci. 2020, 10, 234. [Google Scholar] [CrossRef] [PubMed]


| Arm | M | n | F:M | Age | Age Symptoms | Symptoms | Relapse Number | EDSS Baseline | Worsening Number |
|---|---|---|---|---|---|---|---|---|---|
| R0 | 12 | 5339 | 2.32 | 36 | 30 | 3.61 | 0 | 1.5 | 231 |
| R0 | 24 | 2961 | 2.24 | 37 | 30 | 3.78 | 0 | 1.5 | 184 |
| R0 | 36 | 1392 | 2.2 | 36 | 30 | 3.38 | 0 | 1.5 | 93 |
| R0 | 48 | 525 | 2.28 | 36 | 31 | 3.48 | 0 | 1.5 | 40 |
| R0 | 60 | 255 | 2.04 | 36 | 31 | 3.16 | 0 | 1 | 21 |
| R1 | 12 | 592 | 2.23 | 35 | 28 | 4.06 | 592 | 2 | 103 |
| R1 | 24 | 153 | 2.48 | 35 | 28 | 4.37 | 0 | 2 | 17 |
| R1 | 36 | 63 | 1.86 | 37 | 29 | 3.69 | 0 | 2 | 5 |
| R1 | 48 | 21 | 2 | 32 | 28 | 2.57 | 0 | 1.5 | 0 |
| R1 | 60 | 10 | 1.5 | 30 | 27 | 2.03 | 0 | 1.5 | 1 |
| R1+ | 12 | 342 | 2.05 | 35 | 28 | 4 | 342 | 2 | 90 |
| R1+ | 24 | 73 | 2.04 | 34 | 28 | 3.98 | 0 | 2 | 15 |
| R1+ | 36 | 23 | 1.3 | 36 | 27 | 4.31 | 0 | 2 | 5 |
| R1+ | 48 | 9 | 2 | 35 | 30 | 2.79 | 0 | 1.5 | 0 |
| R1+ | 60 | 4 | 1 | 28 | 24 | 2.97 | 0 | 1.2 | 0 |
| R1− | 12 | 250 | 2.52 | 35 | 28 | 4.21 | 250 | 2 | 13 |
| R1− | 24 | 80 | 3 | 36 | 28 | 4.77 | 0 | 2.2 | 2 |
| R1− | 36 | 40 | 2.33 | 37 | 29.5 | 3.32 | 0 | 2 | 0 |
| R1− | 48 | 12 | 2 | 30 | 27 | 2.45 | 0 | 2 | 0 |
| R1− | 60 | 6 | 2 | 33 | 29 | 1.81 | 0 | 2 | 1 |
| R2 | 12 | 5339 | 2.32 | 36 | 30 | 3.61 | 0 | 1.5 | 231 |
| R2 | 24 | 378 | 2.26 | 37 | 30 | 3.46 | 378 | 2 | 94 |
| R2 | 36 | 116 | 1.37 | 38 | 32 | 2.89 | 0 | 2 | 16 |
| R2 | 48 | 31 | 2.1 | 38 | 32 | 2.16 | 0 | 1.5 | 5 |
| R2 | 60 | 12 | 3 | 38 | 34 | 1.75 | 0 | 1.2 | 3 |
| R0 + MRI0 | 12 | 4051 | 2.38 | 37 | 31 | 3.9 | 0 | 2 | 170 |
| R0 + MRI0 | 24 | 2010 | 2.33 | 38 | 31 | 4.22 | 0 | 1.5 | 130 |
| R0 + MRI0 | 36 | 885 | 2.16 | 38 | 31 | 3.78 | 0 | 1.5 | 67 |
| R0 + MRI0 | 48 | 296 | 2.75 | 38 | 32 | 3.78 | 0 | 1.5 | 27 |
| R0 + MRI0 | 60 | 139 | 2.56 | 38 | 32 | 3.65 | 0 | 1 | 11 |
| Arm | Time | Covariate | Prob | SE | Asymp.LCL | Asymp.UCL | Group |
|---|---|---|---|---|---|---|---|
| R1− | 12 | none | 0.052 | 0.0140 | 0.030 | 0.087 | a |
| R1− | 24 | none | 0.025 | 0.0174 | 0.006 | 0.094 | a |
| R1+ | 12 | [EDSS = 2] [Sex = female] | 0.226 | 0.0269 | 0.177 | 0.283 | a |
| R1+ | 24 | [EDSS = 2] [Sex = female] | 0.165 | 0.0430 | 0.096 | 0.267 | a |
| R1+ | 36 | [EDSS = 2] [Sex = female] | 0.173 | 0.0756 | 0.069 | 0.371 | a |
| R0 | 12 | [EDSS = 2] [Age = 30] | 0.033 | 0.0026 | 0.027 | 0.037 | a |
| R0 | 24 | [EDSS = 2] [Age = 30] | 0.046 | 0.0039 | 0.039 | 0.054 | b |
| R0 | 36 | [EDSS = 2] [Age = 30] | 0.050 | 0.0055 | 0.039 | 0.061 | b |
| R0 | 48 | [EDSS = 2] [Age = 30] | 0.056 | 0.0091 | 0.040 | 0.077 | b |
| R0 | 60 | [EDSS = 2] [Age = 30] | 0.061 | 0.0133 | 0.039 | 0.092 | ab |
| R0 + MRI0 | 12 | [EDSS = 2] [Age = 30] | 0.030 | 0.0029 | 0.024 | 0.036 | a |
| R0 + MRI0 | 24 | [EDSS = 2] [Age = 30] | 0.045 | 0.0048 | 0.036 | 0.055 | b |
| R0 + MRI0 | 36 | [EDSS = 2] [Age = 30] | 0.052 | 0.0162 | 0.040 | 0.068 | b |
| R0 + MRI0 | 48 | [EDSS = 2] [Age = 30] | 0.062 | 0.0124 | 0.041 | 0.090 | b |
| R0 + MRI0 | 60 | [EDSS = 2] [Age = 30] | 0.052 | 0.0160 | 0.028 | 0.094 | ab |
| R1 | 12 | [EDSS = 2] [Sex = female] | 0.156 | 0.0177 | 0.123 | 0.193 | a |
| R1 | 24 | [EDSS = 2] [Sex = female] | 0.097 | 0.0249 | 0.059 | 0.154 | a |
| R1 | 36 | [EDSS = 2] [Sex = female] | 0.068 | 0.0301 | 0.027 | 0.156 | a |
| R2 | 12 | [EDSS = 2] [Age = 30] | 0.031 | 0.0028 | 0.026 | 0.037 | a |
| R2 | 24 | [EDSS = 2] [Age = 30] | 0.207 | 0.0212 | 0.168 | 0.251 | b |
| R2 | 36 | [EDSS = 2] [Age = 30] | 0.109 | 0.0269 | 0.066 | 0.173 | b |
| R2 | 48 | [EDSS = 2] [Age = 30] | 0.121 | 0.0528 | 0.049 | 0.267 | b |
| R2 | 60 | [EDSS = 2] [Age = 30] | 0.178 | 0.0991 | 0.054 | 0.449 | b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapica-Topczewska, K.; Collin, F.; Tarasiuk, J.; Czarnowska, A.; Chorąży, M.; Mirończuk, A.; Kochanowicz, J.; Kułakowska, A. Assessment of Disability Progression Independent of Relapse and Brain MRI Activity in Patients with Multiple Sclerosis in Poland. J. Clin. Med. 2021, 10, 868. https://doi.org/10.3390/jcm10040868
Kapica-Topczewska K, Collin F, Tarasiuk J, Czarnowska A, Chorąży M, Mirończuk A, Kochanowicz J, Kułakowska A. Assessment of Disability Progression Independent of Relapse and Brain MRI Activity in Patients with Multiple Sclerosis in Poland. Journal of Clinical Medicine. 2021; 10(4):868. https://doi.org/10.3390/jcm10040868
Chicago/Turabian StyleKapica-Topczewska, Katarzyna, François Collin, Joanna Tarasiuk, Agata Czarnowska, Monika Chorąży, Anna Mirończuk, Jan Kochanowicz, and Alina Kułakowska. 2021. "Assessment of Disability Progression Independent of Relapse and Brain MRI Activity in Patients with Multiple Sclerosis in Poland" Journal of Clinical Medicine 10, no. 4: 868. https://doi.org/10.3390/jcm10040868
APA StyleKapica-Topczewska, K., Collin, F., Tarasiuk, J., Czarnowska, A., Chorąży, M., Mirończuk, A., Kochanowicz, J., & Kułakowska, A. (2021). Assessment of Disability Progression Independent of Relapse and Brain MRI Activity in Patients with Multiple Sclerosis in Poland. Journal of Clinical Medicine, 10(4), 868. https://doi.org/10.3390/jcm10040868






