Cytokines and Chemokines Involved in Hepatitis B Surface Antigen Loss in Human Immunodeficiency Virus/Hepatitis B Virus Coinfected Patients
Abstract
1. Introduction
2. Materials and Methods
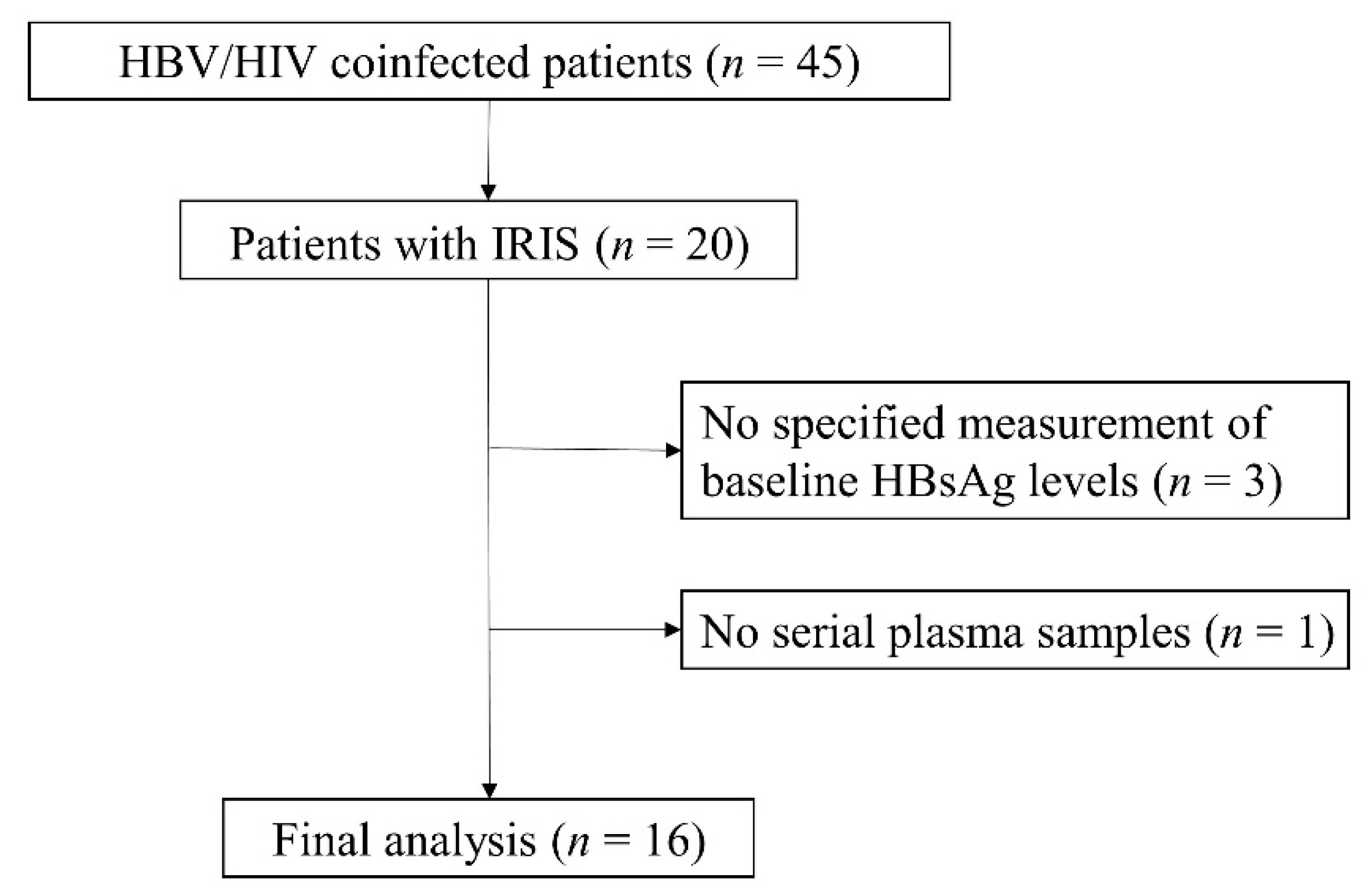
2.1. Patients
2.2. Measurement of HIV-1 RNA and HBV DNA
2.3. Laboratory Tests and Measurement of Cytokines/Chemokines
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. The Serum ALT Levels in the HBsAg Clearance and Non-Clearance Groups
3.3. CD4+ and CD8+ T Cell Counts in the HBsAg Clearance and Non-Clearance Groups
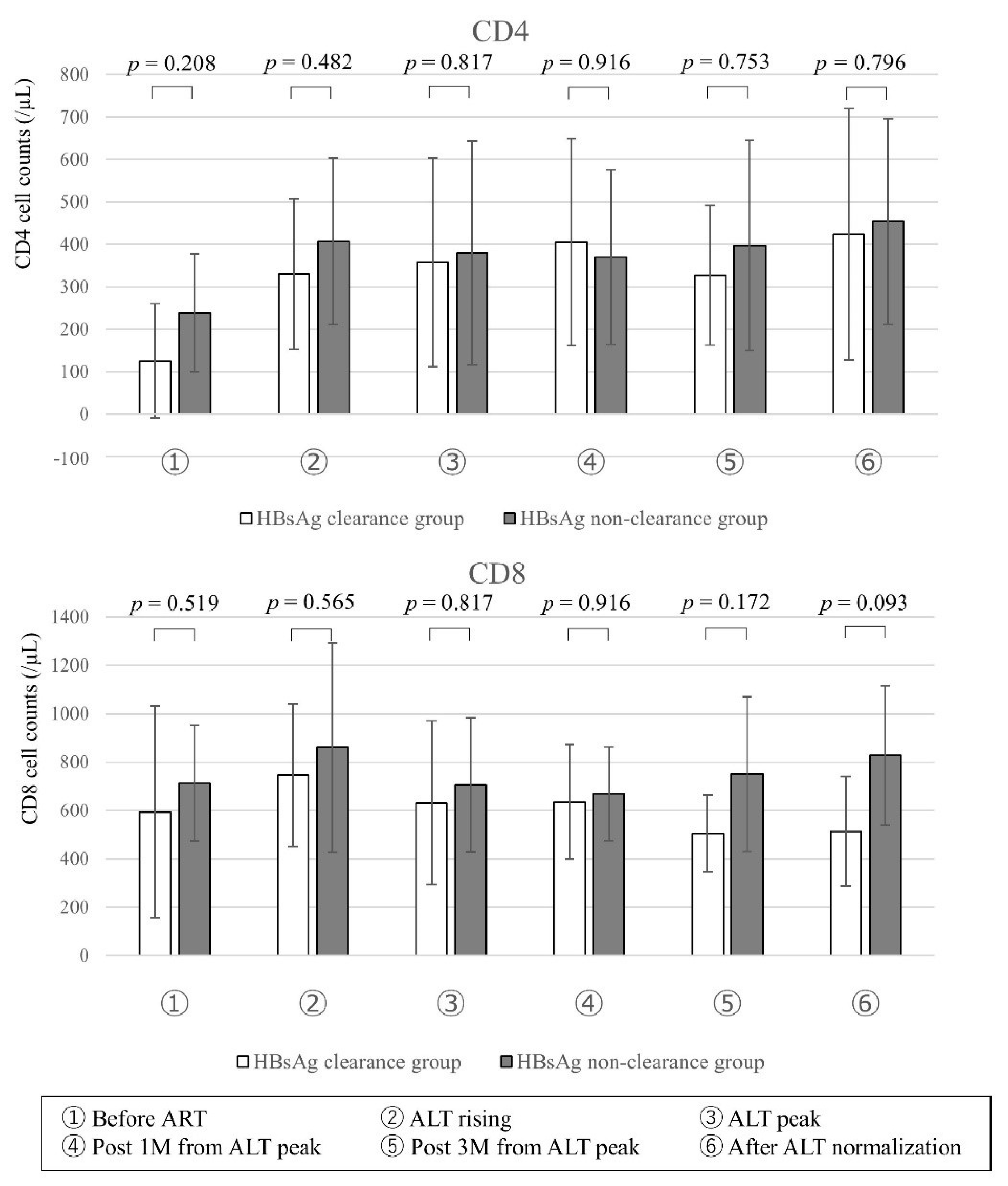
3.4. HBV DNA and HIV-1 RNA in the HBsAg Clearance and Non-Clearance Groups
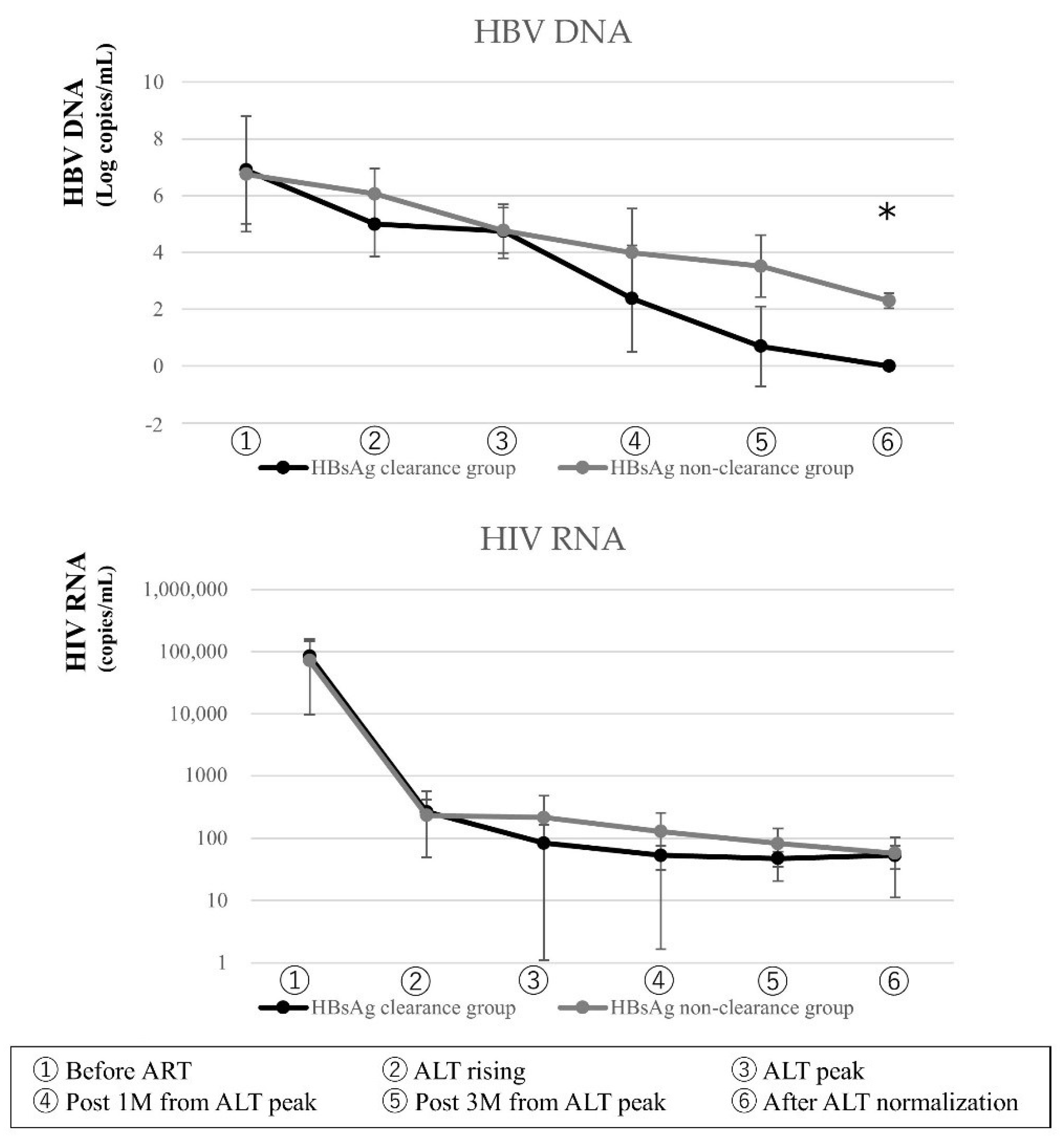
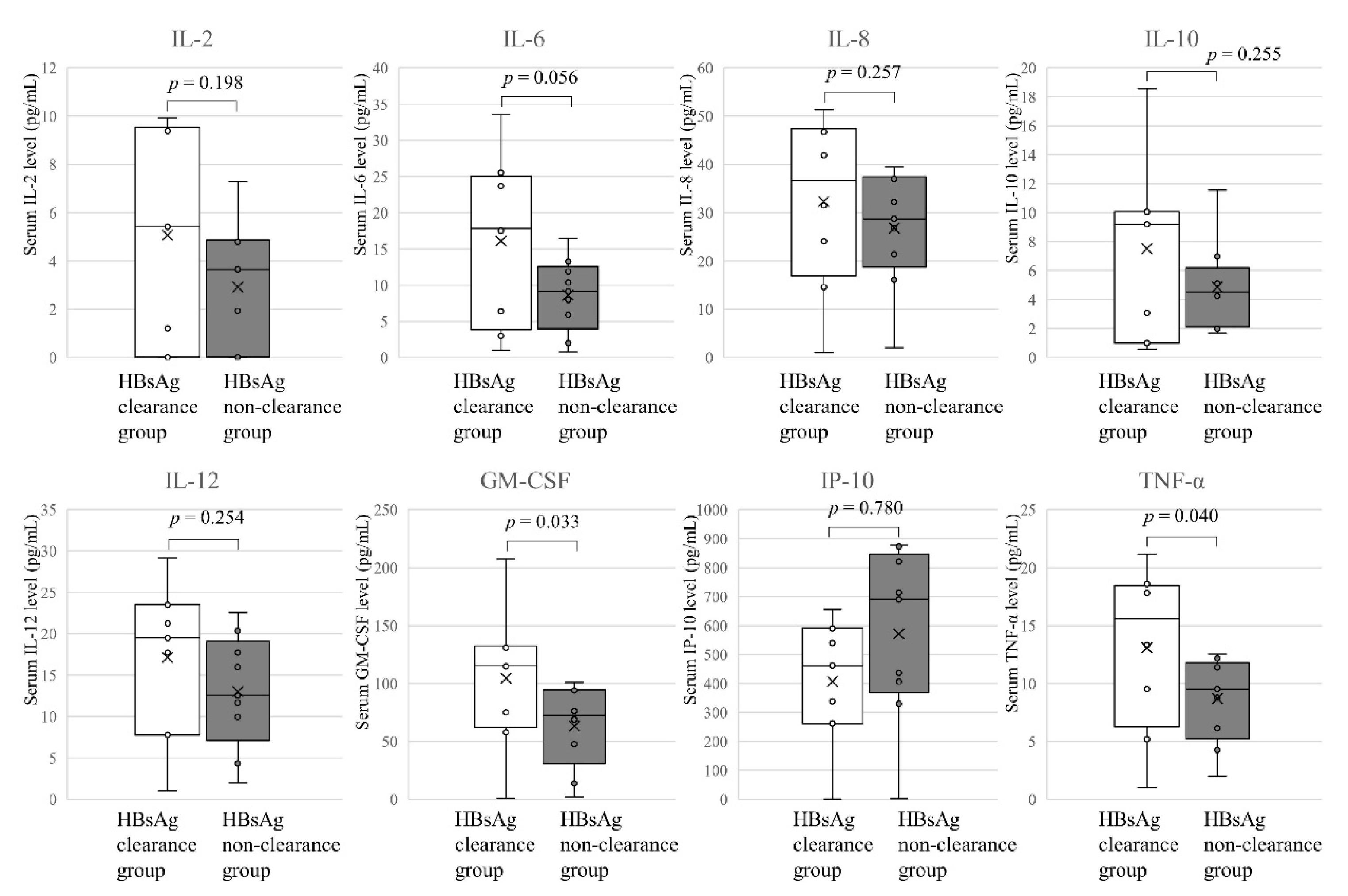
3.5. Cytokines and Chemokines in the HBsAg Clearance and Non-Clearance Groups
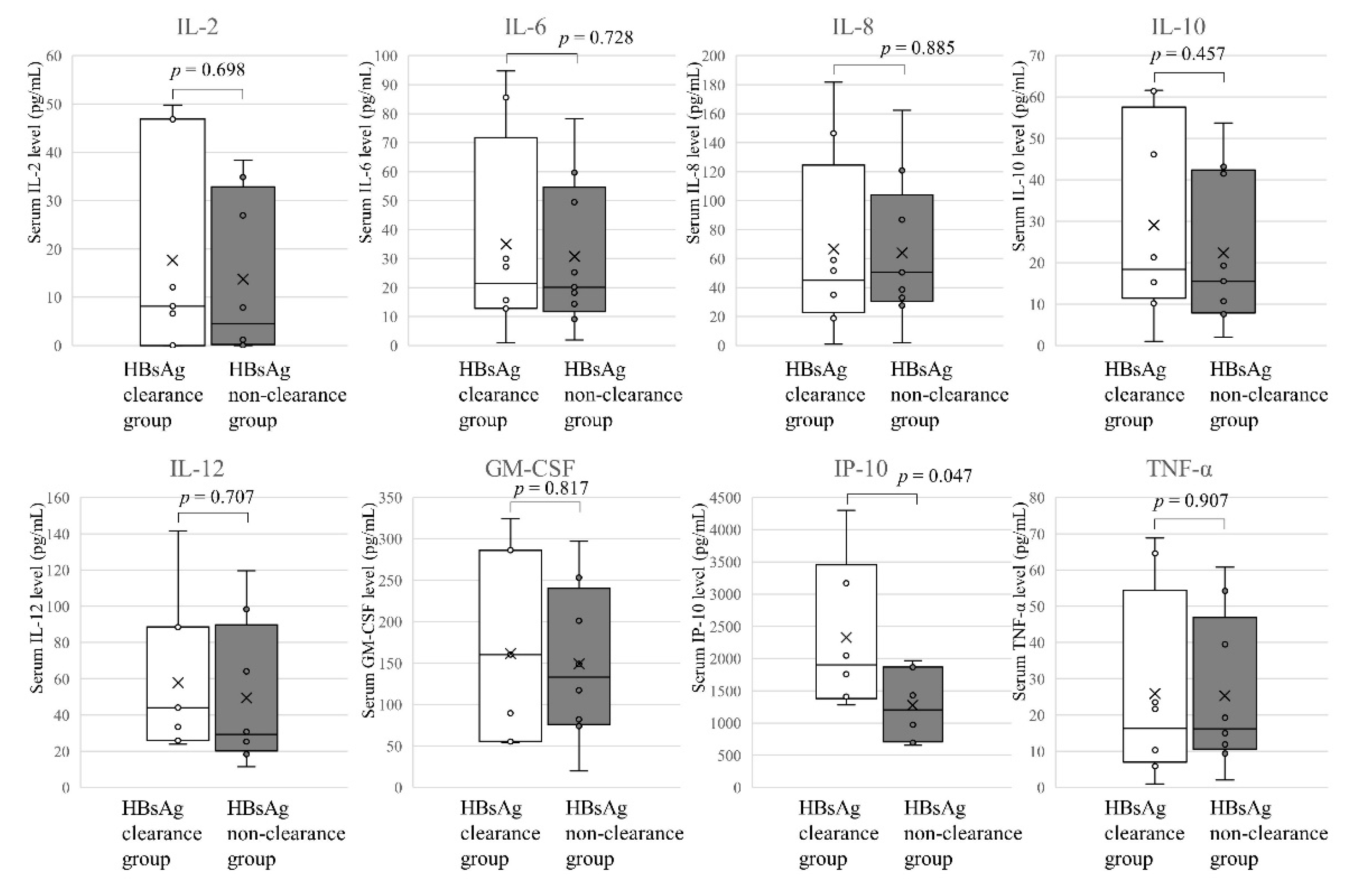
3.6. Changes in the Longitudinal Profiles of the Cytokines and Chemokines
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO HIV/AIDS. Available online: https://www.who.int/news-room/facts-in-pictures/detail/hiv-aids (accessed on 7 December 2020).
- Ministry of Health, Labour and Welfare AIDS Committee. Available online: https://api-net.jfap.or.jp/statsu/japan/nenpo.html (accessed on 7 December 2020).
- WHO Hepatitis, B. Available online: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b (accessed on 7 December 2020).
- Gatanaga, H.; Ibe, S.; Matsuda, M.; Yoshida, S.; Asagi, T.; Kondo, M.; Sadamasu, K.; Tsukada, H.; Masakane, A.; Mori, H.; et al. Drug-resistant HIV-1 prevalence in patients newly diagnosed with HIV/AIDS in Japan. Antivir. Res. 2007, 75, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Thio, C.L.; Seaberg, E.C.; Skolasky, R., Jr.; Phair, J.; Vsscher, B.; Muñoz, A.; Thomas, D.L. HIV-1, hepatitis B virus, and risk of liver-related mortality in the Multicenter Cohort Study (MACS). Lancet 2002, 360, 1921–1926. [Google Scholar] [CrossRef]
- Sharma, S.K.; Soneja, M. HIV & Immune reconstitution inflammatory syndrome (IRIS). Indian J. Med. Res. 2011, 134, 866–877. [Google Scholar] [PubMed]
- Sereti, I.; Rodger, A.J.; French, M.A. Biomarkers in Immune Reconstitution Inflammatory Syndrome: Signals from Pathogenesis. Curr. Opin. HIV AIDS 2010, 5, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Crane, M.; Oliver, B.; Matthews, G.; Avihingsanon, A.; Ubolyam, S.; Markovska, V.; Chang, J.J.; Dore, G.J.; Price, P.; Visvanathan, K.; et al. Immunopathogenesis of hepatic flare in HIV/hepatitis B virus (HBV) coinfected individuals after the initiation of HBV-active antiretroviral therapy. J. Infect. Dis. 2009, 199, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Mitsumoto, F.; Murata, M.; Kato, Y.; Ura, K.; Takayama, K.; Hiramine, S.; Ikezaki, H.; Shimizu, M.; Toyoda, K.; Ogawa, E.; et al. Hepatitis B virus-related Immune Reconstitution Inflammatory Syndrome in two patients coinfected with human immunodeficiency virus diagnosed with a liver biopsy. Intern. Med. 2014, 53, 2165–2170. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rowley, M.W.; Patel, A.; Zhou, W.; Wong, M.; Seetharam, A.B. Immune Reconstitution Syndrome with initiation of treatment of HBV/HIV co-infection: Activity flare associated with E antigen seroconversion. Ann. Hepatol. 2019, 18, 220–224. [Google Scholar] [CrossRef] [PubMed]
- David, M.I.; Anchalee, A.; Naruemon, W.; Alexander, J.T.; Alison, B.; Gail, V.M.; Stephen, A.L.; John, S.; Paul, V.D.; Sharon, R.L. Increased intrahepatic apoptosis but reduced immune activation in HIV-HBV co-infected patients with advanced immunosuppression. AIDS 2011, 14, 197–205. [Google Scholar]
- Li, R.B.; Chen, H.S.; Xie, Y.; Fei, R.; Cong, X.; Jiang, D.; Wang, S.X.; Wei, L.; Wang, Y. Dendritic cells from chronic hepatitis B patients can induce HBV antigen-specific T cell responses. World J. Gastroenterol. 2004, 10, 1578–1582. [Google Scholar] [CrossRef] [PubMed]
- Hirohata, S. Human Th1 responses driven by IL-12 are associated with enhanced expression of CD40 ligand. Clin. Exp. Immunol. 1999, 115, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Dang, Y.; Wagner, W.M.; Gad, E.; Rastetter, L.; Berger, C.M.; Holt, G.E.; Disis, M.L. Dendritic cell activating vaccine adjuvants differ in the ability to elicit anti-tumor immunity due to an adjuvant specific induction of immune suppressive cells. Clin. Cancer Res. 2012, 18, 3122–3131. [Google Scholar] [CrossRef] [PubMed]
- Rossol, S.; Marinos, G.; Carucci, P.; Singer, M.V.; Williams, R.; Naoumov, N.V. Interleukin-12 induction of Th1 cytokines is important for viral clearance in chronic hepatitis B. J. Clin. Investig. 1997, 99, 3025–3033. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Ando, K.; Ishikawa, T.; Seishima, M. Role of tumor necrosis factor-α in acute hepatitis B virus infection. Inflamm. Regen 2010, 30, 445–450. [Google Scholar] [CrossRef]
- Yoshino, S.; Mano, Y.; Doi, H.; Shoji, H.; Shimagaki, T.; Sakamoto, Y.; Kawai, H.; Matsuda, M.; Mori, T.; Osawa, Y.; et al. Cytokine and chemokine signatures associated with hepatitis B surface antigen loss in hepatitis B patients. JCI Insight 2018, 3, e122268. [Google Scholar] [CrossRef] [PubMed]
- Tseng, T.C.; Huang, L.R. Immunopathogenesis of hepatitis B virus. J. Infect. Dis. 2017, 216, S765–S770. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.; Kakimi, K.; Weiland, S.; Guidotti, L.G.; Chisari, F.V. Activated intrahepatic antigen-presenting cells inhibit hepatitis B virus replication in the liver of transgenic mice. J. Immunol. 2002, 169, 5188–5195. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, M.; Azam, M.; Sami, H.; Shukla, I.; Malik, A.; Ajmal, M.; Khan, F.; Sultan, A. Role of IL-8, IL10, IL-12, IFN-γ and TNF-α in the immunopathogenesis of acute hepatitis B virus infection. J. Gastroenterol. Hepatol. Res. 2013, 2, 646–651. [Google Scholar]



| All (n = 16) | HBsAg Clearance Group (n = 8) | HBsAg Non-Clearance Group (n = 8) | p | |
|---|---|---|---|---|
| Age (years) | 34.5 (29–63) | 37 (29–63) | 32.5 (29–58) | 0.206 |
| Sex | All male | |||
| ALT (U/L) | 43 (22–193) | 45 (22–95) | 43 (28–193) | 0.793 |
| HBsAg (IU/mL) | 125,000 (23,327–125,000) | 89,034 (23,327–125,000) | 125,000 (40,550–125,000) | 0.298 |
| HBV DNA (Log10 copies/mL) | 6.9 (3.3–9.1) | 6.9 (4.0–9.1) | 6.9 (3.3–8.8) | 0.710 |
| CD4 (/µL) | 150 (3–458) | 76.5 (3–458) | 296.5 (10–391) | 0.208 |
| HIV-1 RNA (copies/mL) | 23,050 (450–220,000) | 51,550 (13,500–210,000) | 23,000 (450–220,000) | 0.833 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urata, N.; Watanabe, T.; Hirashima, N.; Yokomaku, Y.; Imamura, J.; Iwatani, Y.; Shimada, M.; Tanaka, Y. Cytokines and Chemokines Involved in Hepatitis B Surface Antigen Loss in Human Immunodeficiency Virus/Hepatitis B Virus Coinfected Patients. J. Clin. Med. 2021, 10, 833. https://doi.org/10.3390/jcm10040833
Urata N, Watanabe T, Hirashima N, Yokomaku Y, Imamura J, Iwatani Y, Shimada M, Tanaka Y. Cytokines and Chemokines Involved in Hepatitis B Surface Antigen Loss in Human Immunodeficiency Virus/Hepatitis B Virus Coinfected Patients. Journal of Clinical Medicine. 2021; 10(4):833. https://doi.org/10.3390/jcm10040833
Chicago/Turabian StyleUrata, Noboru, Tsunamasa Watanabe, Noboru Hirashima, Yoshiyuki Yokomaku, Junji Imamura, Yasumasa Iwatani, Masaaki Shimada, and Yasuhito Tanaka. 2021. "Cytokines and Chemokines Involved in Hepatitis B Surface Antigen Loss in Human Immunodeficiency Virus/Hepatitis B Virus Coinfected Patients" Journal of Clinical Medicine 10, no. 4: 833. https://doi.org/10.3390/jcm10040833
APA StyleUrata, N., Watanabe, T., Hirashima, N., Yokomaku, Y., Imamura, J., Iwatani, Y., Shimada, M., & Tanaka, Y. (2021). Cytokines and Chemokines Involved in Hepatitis B Surface Antigen Loss in Human Immunodeficiency Virus/Hepatitis B Virus Coinfected Patients. Journal of Clinical Medicine, 10(4), 833. https://doi.org/10.3390/jcm10040833






