Intra-Aortic Balloon Pump and Ischemic Cardiogenic Shock May Still Be a Valuable Association
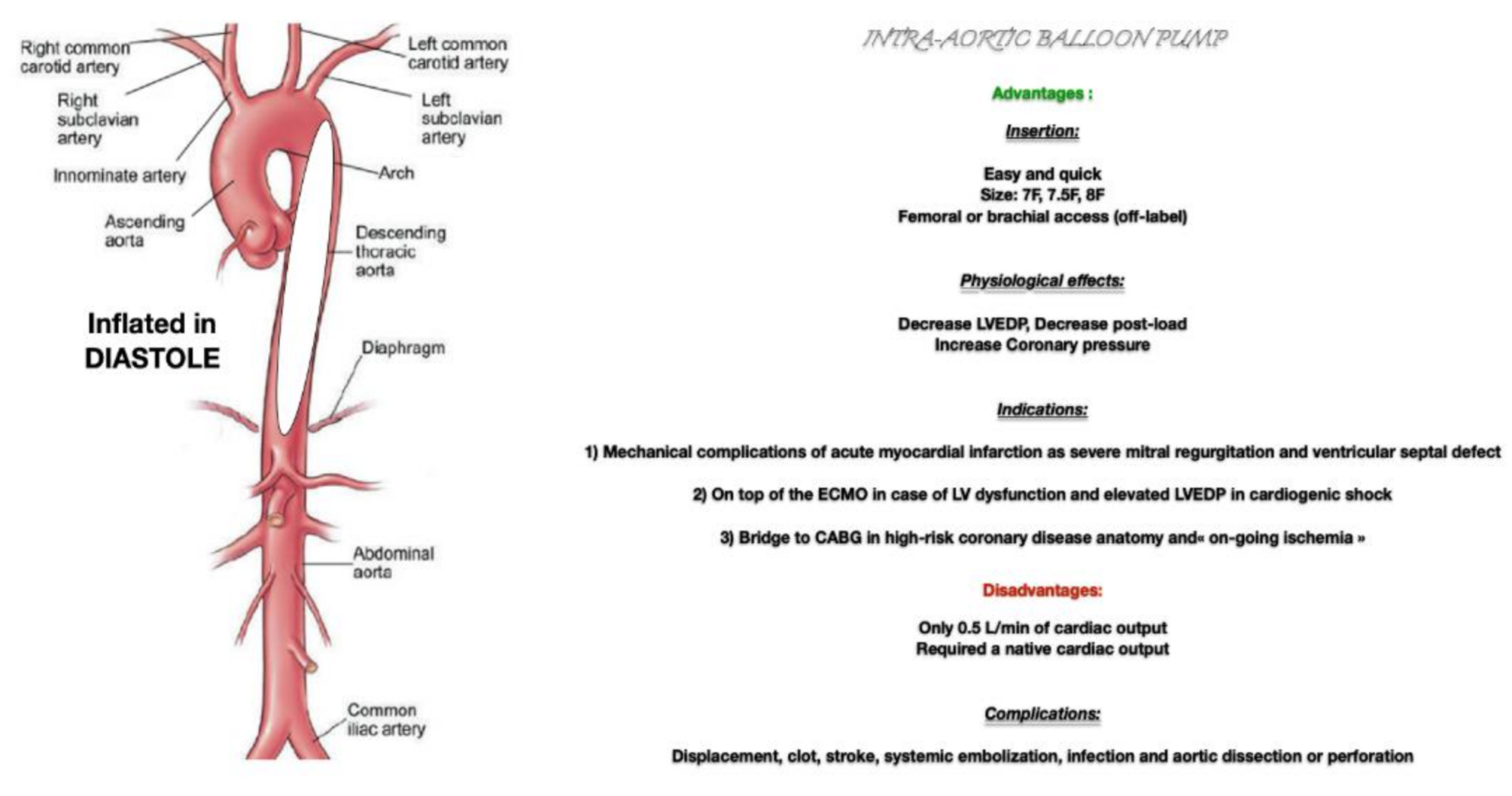
1. Physiology of the Intra-Aortic Balloon Pump (IABP)
2. Evidence-Based Medicine Concerning IABP
3. Our Point of View
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Myat, A.; Patel, N.; Tehrani, S.; Banning, A.P.; Redwood, S.R.; Bhatt, D.L. Percutaneous circulatory assist devices for high-risk coronary intervention. JACC Cardiovasc. Interv. 2015, 8, 229–244. [Google Scholar] [CrossRef] [PubMed]
- Ouweneel, D.M.; Eriksen, E.; Sjauw, K.D.; van Dongen, I.M.; Hirsch, A.; Packer, E.J.; Vis, M.M.; Wykrzykowska, J.J.; Koch, K.T.; Baan, J.; et al. Percutaneous Mechanical Circulatory Support Versus Intra-Aortic Balloon Pump in Cardiogenic Shock after Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2017, 69, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Zeymer, U.; Neumann, F.J.; Ferenc, M.; Olbrich, H.G.; Hausleiter, J.; de Waha, A.; Richardt, G.; Hennersdorf, M.; Empen, K.; et al. Intraaortic balloon pump in cardiogenic shock II (IABP-SHOCK II) trial investigators. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): Final 12 month results of a randomised, open-label trial. Lancet 2013, 382, 1638–1645. [Google Scholar] [CrossRef] [PubMed]
- Seyfarth, M.; Sibbing, D.; Bauer, I.; Fröhlich, G.; Bott-Flügel, L.; Byrne, R.; Dirschinger, J.; Kastrati, A.; Schömig, A. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J. Am. Coll. Cardiol. 2008, 52, 1584–1588. [Google Scholar] [CrossRef] [PubMed]
- White, J.M.; Ruygrok, P.N. Intra-aortic balloon counterpulsation in contemporary practice—Where are we? Heart Lung Circ. 2015, 24, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Helleu, B.; Auffret, V.; Bedossa, M.; Gilard, M.; Letocart, V.; Chassaing, S.; Angoulvant, D.; Commeau, P.; Range, G.; Prunier, F.; et al. Current indications for the intra-aortic balloon pump: The CP-GARO registry. Arch. Cardiovasc. Dis. 2018, 111, 739–748. [Google Scholar] [CrossRef] [PubMed]
| Name | Year | Clinical Picture | Patients Number | IABP vs. Which MCS | Length of FU (Months) | Outcomes |
|---|---|---|---|---|---|---|
| Impress trial 1 | 2017 | CS | 48 | Impella CP | 1 | No difference in mortality |
| IABP SHOCK II trial 2 | 2012 | CA and CS | 600 | Control (standard of care) | 12 | CA: no difference in mortality;CS: no difference in mortality |
| ISAR-SHOCK trial 3 | 2008 | CS | 25 | Impella 2.5 | 1 | No difference in mortality |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rey, F.; Giraud, R.; Bendjelid, K. Intra-Aortic Balloon Pump and Ischemic Cardiogenic Shock May Still Be a Valuable Association. J. Clin. Med. 2021, 10, 778. https://doi.org/10.3390/jcm10040778
Rey F, Giraud R, Bendjelid K. Intra-Aortic Balloon Pump and Ischemic Cardiogenic Shock May Still Be a Valuable Association. Journal of Clinical Medicine. 2021; 10(4):778. https://doi.org/10.3390/jcm10040778
Chicago/Turabian StyleRey, Florian, Raphaël Giraud, and Karim Bendjelid. 2021. "Intra-Aortic Balloon Pump and Ischemic Cardiogenic Shock May Still Be a Valuable Association" Journal of Clinical Medicine 10, no. 4: 778. https://doi.org/10.3390/jcm10040778
APA StyleRey, F., Giraud, R., & Bendjelid, K. (2021). Intra-Aortic Balloon Pump and Ischemic Cardiogenic Shock May Still Be a Valuable Association. Journal of Clinical Medicine, 10(4), 778. https://doi.org/10.3390/jcm10040778






