A Systematic Review and Meta-Analysis of Wound Complications after a Caesarean Section in Obese Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Selection Process and Result Codification
2.4. Critical Reading and Level of Evidence
2.5. Statistical Analysis
3. Results
3.1. Study Selection Process
3.2. Characteristics of Included Studies
3.3. Synthesis of Results
3.3.1. Relationship between Preoperative Factors and Wound Complications
3.3.2. Antibiotic Prophylaxis
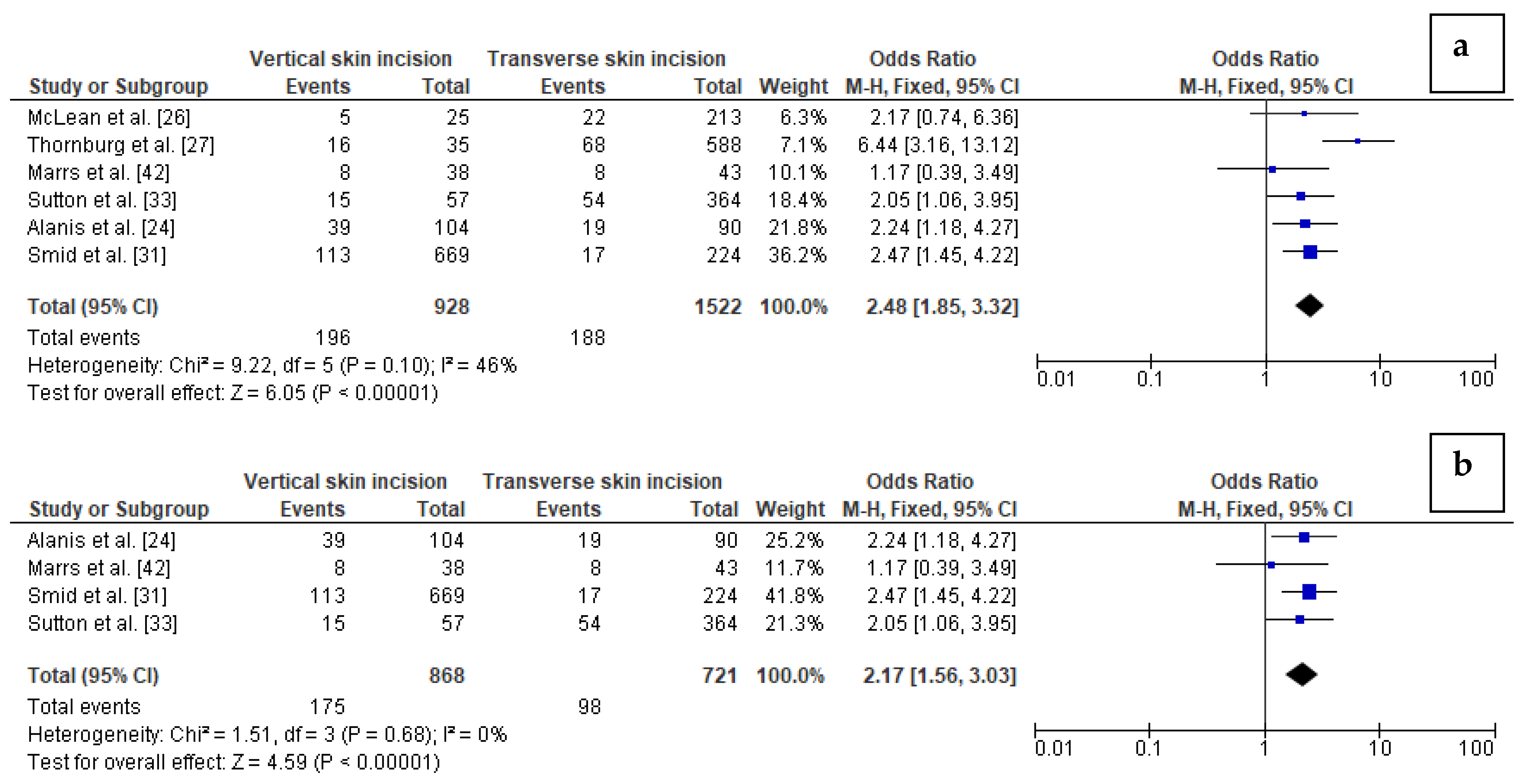
3.3.3. Skin Incisions
3.3.4. Skin and Subcutaneous Tissue Closure
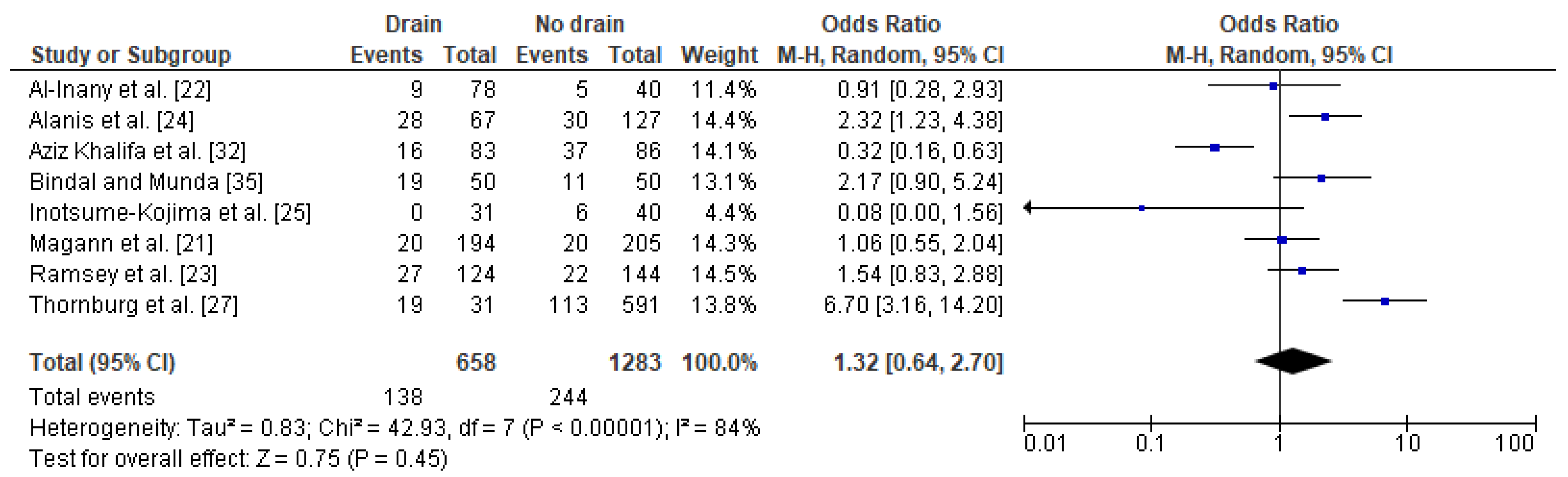
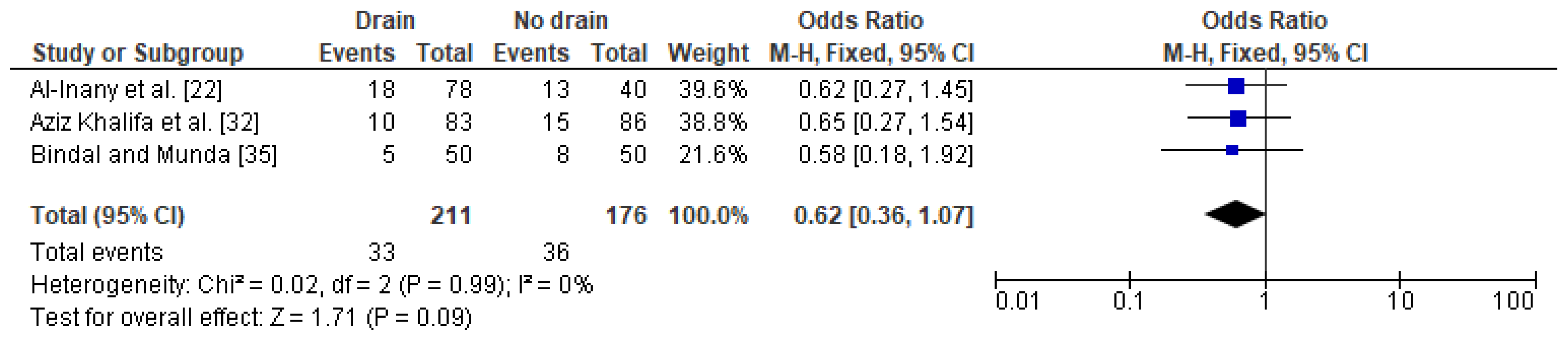
3.3.5. Subcutaneous Tissue Drainage
3.3.6. Negative Pressure Wound Therapy Dressings (VAC Dressings)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sepúlveda, J.; Murray, C. The State of Global Health in 2014. Science 2014, 345, 1275–1278. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 June 2019).
- Ogden, C.L.; Carroll, M.D.; Curtin, L.R.; McDowell, M.A.; Tabak, C.J.; Flegal, K.M. Prevalence of Overweight and Obesity in the United States, 1999–2004. JAMA 2006, 295, 1549–1555. [Google Scholar] [CrossRef]
- Shaikh, H.; Robinson, S.; Teoh, T.G. Management of Maternal Obesity Prior to and During Pregnancy. Semin. Fetal. Neonatal. Med. 2010, 15, 77–82. [Google Scholar] [CrossRef]
- Feig, D.S.; Hwee, J.; Shah, B.R.; Booth, G.L.; Bierman, A.S.; Lipscombe, L.L. Trends in Incidence of Diabetes in Pregnancy and Serious Perinatal Outcomes: A Large, Population-Based Study in Ontario, Canada, 1996–2010. Diabetes Care. 2014, 37, 1590–1596. [Google Scholar] [CrossRef]
- Crane, J.M.G.; White, J.; Murphy, P.; Burrage, L.; Hutchens, D. The Effect of Gestational Weight Gain by Body Mass Index on Maternal and Neonatal Outcomes. J. Obstet. Gynaecol. Can. 2009, 31, 28–35. [Google Scholar] [CrossRef]
- Quiner, T.; Perlow, J.H. The Global Burden of Obesity on Pregnancy Outcomes in the Developed World [17Q]. Obstet. Gynecol. 2017, 1, 177S. [Google Scholar] [CrossRef]
- Vaswani, P.R.; Balachandran, L. Pregnancy Outcomes in a Population with High Prevalence of Obesity: How bad is it? Clin. Epidemiol. Glob. Health 2013, 1, 5–11. [Google Scholar] [CrossRef]
- Marchi, J.; Berg, M.; Dencker, A.; Olander, E.K.; Begley, C. Risks Associated with Obesity in Pregnancy, for the Mother and Baby: A Systematic Review of Reviews. Obes. Rev. 2015, 16, 621–638. [Google Scholar] [CrossRef] [PubMed]
- Conner, S.N.; Verticchio, J.C.; Tuuli, M.G.; Odibo, A.O.; Macones, G.A.; Cahill, A.G. Maternal Obesity and Risk of Postcesarean Wound Complications. Am. J. Perinatol. 2014, 31, 299–304. [Google Scholar]
- Temming, L.A.; Raghuraman, N.; Carter, E.B.; Stout, M.J.; Rampersad, R.M.; Macones, G.A.; Cahill, A.G.; Tuuli, M.G. Impact of Evidence-Based Interventions on Wound Complications after Cesarean Delivery. Am. J. Obstet. Gynecol. 2017, 217, 449.e1–449.e9. [Google Scholar] [CrossRef]
- Salim, R.; Braverman, M.; Teitler, N.; Berkovic, I.; Suliman, A.; Shalev, E. Risk Factors for Infection Following Cesarean Delivery: An Interventional Study. J. Matern. Fetal Neonatal. Med. 2012, 25, 2708–2712. [Google Scholar] [CrossRef] [PubMed]
- Conroy, K.; Koenig, A.F.; Yu, Y.H.; Courtney, A.; Lee, H.J.; Norwitz, E.R. Infectious Morbidity after Cesarean Delivery: 10 Strategies to Reduce Risk. Rev. Obstet. Gynecol. 2012, 5, 69–77. [Google Scholar] [PubMed]
- Mackeen, A.D.; Schuster, M.; Berghella, V. Suture versus Staples for Skin Closure after Cesarean: A Metaanalysis. Am. J. Obstet. Gynecol. 2015, 212, 621.e1–621.e10. [Google Scholar] [CrossRef]
- Kawakita, T.; Landy, H.J. Surgical Site Infections after Cesarean Delivery: Epidemiology, Prevention and Treatment. Matern. Health Neonatol. Perinatol. 2017, 3, 12. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L. Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P). Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, S.; Tatt, I.D.; Higgins, J.P.T. Tools for Assessing Quality and Susceptibility to Bias in Observational Studies in Epidemiology: A Systematic Review and Annotated Bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-analyses of Randomised Controlled Trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Magann, E.F.; Chauhan, S.P.; Rodts-Palenik, S.; Bufkin, L.; Martin, J.N., Jr.; Morrison, J.C. Subcutaneous Stitch Closure versus Subcutaneous Drain to Prevent Wound Disruption after Cesarean Delivery: A Randomized Clinical Trial. Am. J. Obstet. Gynecol. 2002, 186, 1119–1123. [Google Scholar] [CrossRef] [PubMed]
- Al-Inany, H.; Youssef, G.; Abd ElMaguid, A.; Hamid, M.A.; Naguib, A. Value of Subcutaneous Drainage System in Obese Females Undergoing Cesarean Section Using Pfannenstiel Incision. Gynecol. Obstet. Investig. 2002, 53, 75–78. [Google Scholar] [CrossRef]
- Ramsey, P.S.; White, A.M.; Guinn, D.A.; Lu, G.C.; Ramin, S.M.; Davies, J.K.; Neely, C.L.; Newby, C.; Fonseca, L.; Case, A.S.; et al. Subcutaneous Tissue Reapproximation, Alone or in Combination with Drain, in Obese Women Undergoing Cesarean Delivery. Obstet. Gynecol. 2005, 105, 967–973. [Google Scholar] [CrossRef]
- Alanis, M.C.; Villers, M.S.; Law, T.L.; Steadman, E.M.; Robinson, C.J. Complications of Cesarean Delivery in the Massively Obese Parturient. Am. J. Obstet. Gynecol. 2010, 203, 271.e1–271.e7. [Google Scholar] [CrossRef]
- Inotsume-Kojima, Y.; Uchida, T.; Abe, M.; Doi, T.; Kanayama, N. A Combination of Subcuticular Sutures and a Drain for Skin Closure Reduces Wound Complications in Obese Women Undergoing Surgery Using Vertical Incisions. J. Hosp. Infect. 2011, 77, 162–165. [Google Scholar] [CrossRef] [PubMed]
- McLean, M.; Hines, R.; Polinkovsky, M.; Stuebe, A.; Thorp, J.; Strauss, R. Type of Skin Incision and Wound Complications in the Obese Parturient. Am. J. Perinatol. 2012, 29, 301–306. [Google Scholar] [CrossRef]
- Thornburg, L.L.; Linder, M.A.; Durie, D.E.; Walker, B.; Pressman, E.; Glantz, J.C. Risk Factors for Wound Complications in Morbidly Obese Women Undergoing Primary Cesarean Delivery. J. Matern. Fetal. Neonatal. Med. 2012, 25, 1544–1548. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, A.; Jauk, V.C.; Figueroa, D.; Biggio, J.R.; Owen, J.; Tita, A.T. Risk Factors for Wound Disruption Following Cesarean Delivery. J. Matern. Fetal. Neonatal Med. 2014, 27, 1237–1240. [Google Scholar] [CrossRef]
- Stamilio, D.M.; Scifres, C.M. Extreme Obesity and Postcesarean Maternal Complications. Obstet. Gynecol. 2014, 124, 227–232. [Google Scholar] [CrossRef]
- Ibrahim, M.I.; Moustafa, G.F.; Al-Hamid, A.S.; Hussein, M.R. Superficial Incisional Surgical Site Infection Rate after Cesarean Section in Obese Women: A Randomized Controlled Trial of Subcuticular Versus Interrupted Skin Suturing. Arch. Gynecol. Obstet. 2014, 289, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.C.; Kearney, M.S.; Stamilio, D.M. Extreme Obesity and Postcesarean Wound Complications in the Maternal-Fetal Medicine Unit Cesarean Registry. Am. J. Perinatol. 2015, 32, 1336–1341. [Google Scholar] [CrossRef]
- Khalifa, A.A.A.; Abdelrazak, K.M.; Abdelazim, I.A. Routine Subcutaneous Drain versus No Drain in Cesarean Section for Diabetic Obese Women: A Randomized Controlled Trial. Int. J. Curr. Microbiol. App. Sci. 2015, 4, 479–485. [Google Scholar]
- Sutton, A.L.; Sanders, L.B.; Subramaniam, A.; Jauk, V.C.; Edwards, R.K. Abdominal Incision Selection for Cesarean Delivery of Women with Class III Obesity. Am J Perinatol. 2016, 33, 547–551. [Google Scholar] [CrossRef]
- Zaki, M.N.; Truong, M.; Pyra, M.; Kominiarek, M.A.; Irwin, T. Wound Complications in Obese Women after Cesarean: A Comparison of Staples versus Subcuticular Suture. J. Perinatol. 2016, 36, 819–822. [Google Scholar] [CrossRef] [PubMed]
- Bindal, J.A.; Munda, G. Clinical Study to Compare Drain versus No Drain in Post Cesarean Section. Int. J. Reprod. Contracept. Obstet. Gynecol. 2017, 6, 3903–3906. [Google Scholar] [CrossRef]
- Looby, M.A.; Vogel, R.I.; Bangdiwala, A.; Hyer, B.; Das, K. Prophylactic Negative Pressure Wound Therapy in Obese Patients Following Cesarean Delivery. Surg. Innov. 2018, 25, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Ruhstaller, K.; Downes, K.L.; Chandrasekaran, S.; Srinivas, S.; Durnwald, C. Prophylactic Wound Vacuum Therapy after Cesarean Section to Prevent Wound Complications in the Obese Population: A Randomized Controlled Trial (the ProVac Study). Am. J. Perinat. 2017, 34, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Searle, R.J.; Myers, D. A Survey of Caesarean Section Surgical Site Infections with PICO™ Single Use Negative Pressure Wound Therapy System in High-Risk Patients in England and Ireland. J. Hosp. Infect. 2017, 97, 122–124. [Google Scholar] [CrossRef]
- Wihbey, K.A.; Joyce, E.M.; Spalding, Z.T.; Jones, H.J.; MacKenzie, T.A.; Evans, R.H.; Fung, J.L.; Goldman, M.B.; Erekson, E. Prophylactic Negative Pressure Wound Therapy and Wound Complication After Cesarean Delivery in Women With Class II or III Obesity: A Randomized Controlled Trial. Obstet. Gynecol. 2018, 132, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Zaki, M.N.; Wing, D.A.; McNulty, J.A. Comparison of Staples vs Subcuticular Suture in Class III Obese Women Undergoing Cesarean: A Randomized Controlled Trial. Am. J. Obstet. Gynecol. 2018, 218, 451.e1–451.e8. [Google Scholar] [CrossRef]
- Alalfy, M.; Elgazzar, A.; Fares, T.; Nagy, O.; Ellithy, A.; Lasheen, Y.; Kamel, A.; Soliman, M.; Hassan, A.; Samy, A.; et al. Effect of Subcutaneous Tissue Closure Technique in Cesarean Section on Postoperative Wound Complications in Obese Egyptian Women. J. Matern. Fetal. Neonatal. Med. 2019, 32, 2452–2459. [Google Scholar] [CrossRef]
- Marrs, C.; Blackwell, S.; Hester, A.; Olson, G.; Saade, G.R.; Faro, J.; Pedroza, C.; Sibai, B. Pfannenstiel versus Vertical Skin Incision for Cesarean Delivery in Women with Class III Obesity: A Randomized Trial. Am. J. Perinatol. 2019, 36, 97–104. [Google Scholar]
- Hussamy, D.J.; Wortman, A.C.; McIntire, D.D.; Leveno, K.J.; Casey, B.M.; Roberts, S.W. Closed Incision Negative Pressure Therapy in Morbidly Obese Women Undergoing Cesarean Delivery: A Randomized Controlled Trial. Obstet. Gynecol. 2019, 134, 781–789. [Google Scholar] [CrossRef]
- Hyldig, N.; Vinter, C.A.; Kruse, M.; Mogensen, O.; Bille, C.; Sorensen, J.A.; Lamont, R.F.; Wu, C.; Heidemann, L.N.; Ibsen, M.H.; et al. Prophylactic Incisional Negative Pressure Wound Therapy Reduces the Risk of Surgical Site Infection after Caesarean Section in Obese Women: A Pragmatic Randomised Clinical Trial. Int. J. Obstet. Gynaecol. 2019, 126, 628–635. [Google Scholar] [CrossRef]
- Connery, S.A.; Yankowitz, J.; Odibo, L.; Raitano, O.; Nikolic-Dorschel, D.; Louis, J.M. Effect of Using Silver Nylon Dressings to Prevent Superficial Surgical Site Infection after Cesarean Delivery: A Randomized Clinical Trial. Am. J. Obstet. Gynecol. 2019, 221, 57.e1–57.e7. [Google Scholar] [CrossRef] [PubMed]
- Dias, M.; Dick, A.; Reynolds, R.M.; Lahti-Pulkkinen, M.; Denison, F.C. Predictors of Surgical Site Skin Infection and Clinical Outcome at Caesarean Section in the Very Severely Obese: A Retrospective Cohort Study. PLoS ONE 2019, 14, e0216157. [Google Scholar] [CrossRef]
- Tuuli, M.G.; Liu, J.; Tita, A.T.N.; Longo, S.; Trudell, A.; Carter, E.B.; Shanks, A.; Woolfolk, C.; Caughey, A.B.; Warren, D.K.; et al. Effect of Prophylactic Negative Pressure Wound Therapy vs Standard Wound Dressing on Surgical-Site Infection in Obese Women After Cesarean Delivery: A Randomized Clinical Trial. JAMA 2020. [Google Scholar] [CrossRef]
- Pevzner, L.; Swank, M.; Krepel, C.; Wing, D.A.; Chan, K.; Edmiston, C.E., Jr. Effects of Maternal Obesity on Tissue Concentrations of Prophylactic Cefazolin During Cesarean Delivery. Obstet. Gynecol. 2011, 117, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Stitely, M.; Sweet, M.; Slain, D.; Alons, L.; Holls, W.; Hochberg, C.; Briggs, F. Plasma and Tissue Cefazolin Concentrations in Obese Patients Undergoing Cesarean Delivery and Receiving Differing Pre-operative Doses of Drug. Surg. Infect. 2013, 14, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzia, H.K.; Patel, E.M.; Joshi, D.; Liao, C.; Witter, F.; Heine, R.P.; Coleman, J.S. Obstetric Surgical Site Infections: 2 grams Compared with 3 grams of Cefazolin in Morbidly Obese Women. Obstet. Gynecol. 2015, 126, 708–715. [Google Scholar] [CrossRef]
- Young, O.M.; Shaik, I.H.; Twedt, R.; Binstock, A.; Althouse, A.D.; Venkataramanan, R.; Simhan, H.N.; Wiesenfeld, H.C.; Caritis, S.N. Pharmacokinetics of Cefazolin Prophylaxis in Obese Gravidae at Time of Cesarean Delivery. Am. J. Obstet. Gynecol. 2015, 213, 541.e1–541.e7. [Google Scholar] [CrossRef] [PubMed]
- Swank, M.L.; Wing, D.A.; Nicolau, D.P.; McNulty, J.A. Increased 3-gram Cefazolin Dosing for Cesarean Delivery Prophylaxis in Obese Women. Am. J. Obstet. Gynecol. 2015, 213, 415.e1–415.e8. [Google Scholar] [CrossRef]
- Maggio, L.; Nicolau, D.P.; DaCosta, M.; Rouse, D.J.; Hughes, B.L. Cefazolin Prophylaxis in Obese Women Undergoing Cesarean Delivery: A Randomized Controlled Trial. Obstet. Gynecol. 2015, 125, 1205–1210. [Google Scholar] [CrossRef]
- Lillico, R.; Sayre, C.L.; Sitar, D.S.; Davies, N.M.; Baron, C.M.; Lakowski, T.M. Quantification of Cefazolin in Serum and Adipose Tissue by Ultra High Performance Liquid Chromatography-Tandem Mass Spectrometry (UHPLC-MS/MS): Application to a Pilot Study of Obese Women Undergoing Cesarean Delivery. J. Chromatogr. B. Analyt. Technol. Biomed. Life Sci. 2016, 1031, 94–98. [Google Scholar] [CrossRef]
- Groff, S.M.; Fallatah, W.; Yang, S.; Murphy, J.; Crutchfield, C.; Marzinke, M.; Kurtzberg, J.; Lee, C.K.K.; Burd, I.; Farzin, A. Effect of Maternal Obesity on Maternal-Fetal Transfer of Preoperative Cefazolin at Cesarean Section. J. Pediatr. Pharmacol. Ther. 2017, 22, 227–232. [Google Scholar] [CrossRef]
- Grupper, M.; Kuti, J.L.; Swank, M.L.; Maggio, L.; Hughes, B.L.; Nicolau, D.P. Population Pharmacokinetics of Cefazolin in Serum and Adipose Tissue from Overweight and Obese Women Undergoing Cesarean Delivery. J. Clin. Pharmacol. 2017, 7, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Kram, J.J.F.; Greer, D.M.; Cabrera, O.; Burlage, R.; Forgie, M.M.; Siddiqui, D.S. Does Current Cefazolin Dosing Achieve Adequate Tissue and Blood Concentrations in Obese Women Undergoing Cesarean Section? Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 210, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Eley, V.A.; Christensen, R.; Ryan, R.; Jackson, D.; Parker, S.L.; Smith, M.; van Zundert, A.A.; Wallis, S.C.; Lipman, J.; Roberts, J.A. Prophylactic Cefazolin Dosing in Women with Body Mass Index >35 kg·m2 Undergoing Cesarean Delivery: A Pharmacokinetic Study of Plasma and Interstitial Fluid. Anesth. Analg. 2020, 131, 199–207. [Google Scholar] [CrossRef]
- Scheck, S.M.; Blackmore, T.; Maharaj, D.; Langdana, F.; Elder, R.E. Caesarean Section Wound Infection Surveillance: Information for Action. Aust. N. Z. J. Obstet. Gynaecol. 2018, 58, 518–524. [Google Scholar] [CrossRef]
- Rayatt, S.S.; Dancey, A.L.; Jaffe, W. Soft Fluted Silicone Drains: A Prospective, Randomized, Patient-Controlled Study. Plast. Reconstr. Surg. 2005, 115, 1605–1608. [Google Scholar] [CrossRef] [PubMed]
- Hellums, E.K.; Lin, M.G.; Ramsey, P.S. Prophylactic Subcutaneous Drainage for Prevention of Wound Complications after Cesarean Delivery-A Metaanalysis. Am. J. Obstet. Gynecol. 2007, 197, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Smaill, F.M.; Grivell, R.M. Antibiotic Prophylaxis versus No Prophylaxis for Preventing Infection after Cesarean Section. Cochrane Database Syst. Rev. 2014, 28, CD007482. [Google Scholar] [CrossRef]
- Baaqeel, H.; Baaqeel, R. Timing of Administration of Prophylactic Antibiotics for Caesarean Section: A Systematic Review and Meta-analysis. BJOG 2013, 120, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Toma, O.; Suntrup, P.; Stefanescu, A.; London, A.; Mutch, M.; Kharasch, E. Pharmacokinetics and Tissue Penetration of Cefoxitin in Obesity: Implications for Risk of Surgical Site Infection. Anesth. Analg. 2011, 113, 730e7. [Google Scholar] [CrossRef] [PubMed]
- Chelmow, D.; Rodriguez, E.J.; Sabatini, M.M. Suture Closure of Subcutaneous Fat and Wound Disruption after Cesarean Delivery: A Meta-analysis. Obstet. Gynecol. 2004, 103, 974e80. [Google Scholar] [CrossRef]
- Mccurdy, R.J.; Felder, L.A.; Saccone, G.; Edwards, R.K.; Thornburg, L.L.; Marrs, C.; Conner, S.N.; Strauss, R.; Berghella, V. The Association of Skin Incision Placement During Cesarean Delivery with Wound Complications in Obese Women: A Systematic Review and Meta-analysis. J. Matern. Fetal. Neonatal. Med. 2020, 7, 1–13. [Google Scholar] [CrossRef]
- Yu, L.; Kronen, R.J.; Simon, L.E.; Stoll, C.R.T.; Colditz, G.A.; Tuuli, M.G. Prophylactic Negative-Pressure Wound Therapy after Cesarean is Associated with Reduced Risk of Surgical Site Infection: A Systematic Review and Meta-analysis. Am. J. Obstet. Gynecol. 2018, 218, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.C.; Dotters-Katz, S.K.; Grace, M.; Wright, S.T.; Villers, M.S.; Hardy-Fairbanks, A.; Stamilio, D.M. Prophylactic Negative Pressure Wound Therapy for Obese Women After Cesarean Delivery: A Systematic Review and Meta-analysis. Obstet. Gynecol. 2017, 130, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Coletta, D.; Del Basso, C.; Giuliani, G.; Guerra, F. Subcutaneous Suction Drains Do Not Prevent Surgical Site Infections in Clean-Contaminated Abdominal Surgery-Results of a Systematic Review and Meta-analysis. Langenbecks Arch. Surg. 2019, 404, 663–668. [Google Scholar] [CrossRef]
- Kosins, A.M.; Scholz, T.; Cetinkaya, M.; Evans, G.R. Evidence-Based Value of Subcutaneous Surgical Wound Drainage: The Largest Systematic Review and Meta-analysis. Plast. Reconstr. Surg. 2013, 132, 443–450. [Google Scholar] [CrossRef]



| Study | Date | Country | Study Design | N | Exclusion Criteria | Definition of Obesity | Primary Outcomes |
|---|---|---|---|---|---|---|---|
| Magann et al., 2002 * [21] | 1998–2001 | Australia | Prospective randomized study | 964 | - Declined participation in investigation, - Emergency caesarean section without consent to participate in the study | At least 2 cm of subcutaneous fat tissue on admission to delivery | Risk of wound disruption after caesarean delivery |
| Al-Inany et al., 2002 * [22] | 1999–2000 | Egypt | Prospective controlled clinical study | 118 | - Prolonged premature rupture of membranes, - Prolonged labor, - Long preoperative hospitalization, - Malignancy, - Diabetes mellitus, - Chronic lung disease | BMI > 32 kg/m2 subcutaneous fat of at least 2 cm | The incidence of wound breakdown in both groups together with the rate of hematoma formation and occurrence of fever |
| Ramsey et al., 2005 * [23] | 2001–2004 | USA | Randomized study | 280 | - Inability to obtain informed consent, - Moribund caesarean delivery required, - No plan for follow-up | BMI > 30 kg/m2 on admission | Composite wound morbidity rate, defined as any of the following noted during the post-hospital discharge wound follow-up assessments: subcutaneous dehiscence (1 cm), seroma, hematoma, abscess, or fascial dehiscence |
| Alanis et al., 2010 * [24] | 2005–2009 | USA | Retrospective cohort study | 194 | - Maternal death | Pre-delivery BMI ≥ 50 kg/m2 | Wound complications (wound disruption, cellulitis, NOT superficial wound |
| Inotsume-Kojima et al., 2011 * [25] | 2006–2009 | Japan | Retrospective cohort study | 71 | - Informed consent for the new surgical method was not obtained preoperatively, - A Pfannenstiel incision was made, - Surgery revealed malignancy, - Subcutaneous fat thickness was <2 cm, - Hospitalization before surgery was longer than 24 h, - Surgery was performed in response to premature labor, - Patient was not a native of Japan | BMI ≥ 28 kg/m2 at the time of admission | Wound complications |
| McLean et al., 2011 [26] | 1998–2005 | USA | Retrospective cohort study | 242 | Incomplete medical reports | BMI ≥ 30 kg/m2 at delivery | Type of skin incision and partial or complete wound separation |
| Thornburg et al., 2012 * [27] | 1994–2008 | USA | Retrospective cohort study | 623 | - Prior caesarean delivery, - Skin incision other than vertical or low transverse, - Missing prepregnancy height or weight, or unavailable follow-up data | BMI ≥ 35 kg/m2 at delivery | Presence of any wound complication defined as a wound separation, including both spontaneous and indicated as resulting from seroma formation or wound infection/cellulitis |
| Subramanian et al., 2014 [28] | 2009–2010 | USA | Retrospective cohort study | 340 | - Primary wound infections (purulent drainage, cellulitis, and/or abscess requiring antibiotics or surgical treatment) | BMI ≥ 30 kg/m2 at delivery | Risk factors for non-infectious wound disruption following a caesarean delivery |
| Stamilio et al., 2014 [29] | 2008–2010 | USA | Retrospective cohort study | 585 | - Emergency surgery - Human immunodeficiency virus infection, - Chronic corticosteroid therapy or other immunosuppressive therapy, - General anesthesia, - Diagnosis of extrauterine infection | BMI ≥ 30 kg/m2 at delivery | Composite of wound infection and endometritis |
| Conner et al., 2014 [10] | 2004–2008 | USA | Retrospective cohort study | 2444 | - No completed follow-up data | BMI ≥ 30 kg/m2 at delivery | A wound complication defined as the occurrence of a wound seroma, hematoma, separation, dehiscence or infection from the time of delivery to 6 weeks postoperative |
| Ibrahim et al., 2014 [30] | March 2012–August 2012 | Egypt | Retrospective cohort study | 130 | - Infection (e.g., chorioamnionitis, pyelonephritis or chest infection), intraoperative events predispose to perioperative infection (e.g., bowel injury, - Operative time more than 90 min, - Major blood loss (hemoglobin less than 10 g/dL), - Pre-eclampsia, diabetes mellitus or rupture of membranes for more than 12 h, - Immunosuppressive drugs, - non-Pfannenstiel incision, - nonelective caesarean section, - BMI <30 kg/m2 | BMI ≥ 30 kg/m2 at delivery | Superficial incisional surgical site infection (SSI) |
| Smid et al., 2015 [31] | 1999–2002 | USA | Retrospective cohort study | 38,299 | - Incomplete demographic, exposure, or outcome data | BMI ≥ 30–45 kg/m2 extremely obese BMI ≥ 45 kg/m2 at delivery | A wound complication composite of a wound infection, endometritis, a wound opening, a seroma/hematoma, and hospital readmission |
| Khalifa et al., 2015 * [32] | 2012–2013 | Egypt | Randomized controlled trial | 169 | - Major intraoperative complications (bowel or urinary tract injuries, massive blood loss, transfusion) | BMI ≥ 30 kg/m2 | The rate of superficial surgical site infection |
| Sutton et al., 2016 [33] | 2010–2013 | USA | Retrospective cohort study | 421 | - Prenatally diagnosed fetal anomalies, - Planned caesarean hysterectomies | BMI ≥ 40 kg/m2 at the time of delivery | A wound composite (cellulitis, abscess, hematoma, seroma, or dehiscence) |
| Zaki et al., 2016 [34] | 2006–2011 | USA | Retrospective cohort study | 1147 | - Women with fascial dehiscence, - Multipregnancy, - Second pregnancy | Pre pregnancy BMI ≥ 30 kg/m2 | A composite of wound disruption or infection occurring within 6 weeks postpartum |
| Bindal & Munda, 2017 * [35] | 2015–2016 | India | Retrospective cohort study | 100 | - Major intraoperative complications (bowel or urinary tract injuries, massive blood loss, and transfusion) | BMI ≥ 30 kg/m2 at the time of caesarean section | The rate of superficial surgical site infection defined as the presence of wound discharge that yielded a positive result on bacteriological culture |
| Looby et al., 2017 ** [36] | 2007–2014 | USA | Retrospective cohort study | 467 | - Vaginal delivery - BMI less than 40 kg/m2, - Loss of follow-up, - Multiple deliveries - Use of nonpunch through (NPT) devices prior to official start date | BMI ≥ 40 kg/m2 | A surgical site infection (SSI), within 30 days of surgery |
| Rusthaller et al., 2017 ** [37] | 2014–2016 | USA | Retrospective cohort study | 136 | - Initiation of prenatal care after 23 weeks (no early BMI), - Chronic steroid use, - Pregestational diabetes, treatment for an active malignancy, - Allergy to silver (contraindication to Prevena negative pressure wound therapy device (NPWT), - Scheduled caesarean section, - Planned vertical skin incision | BMI ≥ 30 kg/m2 at the first prenatal visit <22 weeks | A composite of wound morbidity at 4 weeks postpartum including a surgical site infection (SSI) and/or wound opening |
| Temming et al., 2017 [11] | 2011–2015 | USA | Retrospective cohort study | 1082 | - Allergy to chlorhexidine, alcohol, iodine or shellfish, - Skin infection near the operative site, - Without follow-up after discharge | BMI ≥ 30 kg/m2 | A composite of wound complications, including surgical site infection (SSI), cellulitis, seroma, hematoma, and separation within 30 days |
| Searle et al., 2017 ** [38] | 2012–2016 | Ireland, England | Retrospective cohort study | 399 | - Patient BMI < 35 kg/m2 or patient BMI missing; - Missing data in follow-up time (time between procedure date and follow-up date) less than seven days or missing | BMI ≥ 35 kg/m2 at the time of caesarean section | Postoperative wound complications including surgical site infection (SSI) |
| Wihbey et al., 2018 ** [39] | 2015–2017 | USA | Retrospective cohort study | 166 | - Under 18 years old, - Did not speak English, - Had an allergy to silver or adhesive products, - Skin incision that would not fit the device or standard dressing (e.g., “T” skin incision) | BMI ≥ 35 kg/m2 | A superficial surgical site infection, an infection involving only the skin or subcutaneous tissue occurring within 30 days of surgery with at least one of the following: purulent drainage from the wound or organism identified by culture or wound deliberately opened by the surgeon |
| Zaki et al., 2018 [40] | 205–2016 | USA | Retrospective cohort study | 242 | - Hypersensitivity to staples, - Potential immunosuppression including infection with human immunodeficiency virus, chronic steroid use or active lupus | BMI ≥ 40 kg/m2 | A composite wound complication defined as a superficial or deep separation and infection occurring up to 6 weeks following delivery |
| Alalfy et al., 2018 [41] | From June 2017–December 2017 | Egypt | Retrospective cohort study | 397 | - BMI <30 kg/m2 - Previous caesarean section - Medical disorders diabetes mellitus, hypertension with pregnancy | BMI ≥ 30 kg/m2 | Wound outcome results regarding postoperative wound complications compared to two widely implemented techniques in subcutaneous tissue closure (interrupted versus continuous methods) |
| Marrs et al., 2019 [42] | 2013–2017 | USA | Retrospective cohort study | 91 | - Rupture of membranes for more than 18 h, - Clinical chorioamnionitis at the time of delivery, - Subsequent vaginal delivery, - Participants enrolled in other trials, - Women with strong indications for a certain skin incision type (i.e., placenta accreta necessitating caesarean hysterectomy) | BMI ≥ 40 kg/m2 | A composite wound complication that included any of the following: surgical site infection (SSI), cellulitis, seroma/hematoma, or separation up to 6 weeks postpartum |
| Hussamy et al., 2019 ** [43] | 2015–2016 | USA | Retrospective cohort study | 441 | - Anticoagulation therapy, - Human immunodeficiency virus infection, - Silver or acrylic allergy | BMI ≥ 40 kg/m2 measured within 2 weeks of admission for delivery | A wound complication defined as a wound disruption or wound infection (including cellulitis) |
| Hyldig et al., 2019 ** [44] | 2013–2016 | Denmark | Retrospective cohort study | 876 | - Vaginal delivery, - Missing data | Pre-pregnancy BMI ≥ 30 kg/m2 | A surgical site infection was defined as a surgical site infection requiring antibiotic treatment within the first 30 days after the caesarean section |
| Connery et al., 2019 [45] | 2013–2016 | USA | Retrospective cohort study | 657 | - Patients did not receive routine prophylactic dose of antibiotics in the operating room, - Skin incisions other than Pfannenstiel, - Uterine incisions other than low transverse, - Patients with known or discovered allergies to silver or nylon | BMI ≥ 40 kg/m2 | A superficial surgical site infection at any time within the first 6 weeks after caesarean delivery |
| Dias et al., 2019 * [46] | 2011–2015 | Scotland | Retrospective cohort study | 453 | -missing data | BMI > 40 kg/m | Maternal and surgical predictors of surgical site infection |
| Tuuli et al., 2020 ** [47] | 2017–2019 | USA | Retrospective cohort study | 1624 | - Postoperative follow-up not available, - Contraindication to negative pressure use (pre-existing infection at the incision site), - Bleeding disorder, - Therapeutic anticoagulation, - Allergy to silicone or adhesive tape | BMI ≥ 30 kg/m2 at or beyond 23 weeks of gestation | A superficial or deep surgical site infection |
| Study | Country | Study Design | N | BMI of Participants | Primary Outcomes | Dose of Antibiotics | Results |
|---|---|---|---|---|---|---|---|
| Pevzner et al., 2011 [48] | USA | Prospective study | 29 | BMI < 30 kg/m2 (n = 10) BMI 30–39.9 kg/m2 (n = 10) BMI ≥ 40 kg/m2 (n = 9) | Cefazolin concentration in adipose tissue and surgical site infection | 2 g of cefazolin 30–60 min before skin incision | No significant difference in cefazolin concentration observed in mean closure adipose, myometrial or serum specimens across the BMI categories |
| Stitely et al., 2013 [49] | New Zealand | Retrospective cohort study | 20 | BMI ≥ 35 kg/m2 | Tissue concentration of antibiotics | Cefazolin 2 g vs. 4 g i.v. | Mean cefazolin plasma, umbilical cord, and myometrial concentrations significantly higher in the 4 g treatment group (p < 0.05) |
| Ahmadzia et al., 2015 [50] | USA | Retrospective cohort study | 335 | >250 pounds | Incidence of surgical site infections, (superficial, deep, and organ/space—i.e., endometritis infections) | Cefazolin 2 g vs. cefazolin 3 g | No difference in surgical site infection among women who received 2 g compared with 3 g cefazolin |
| Young et al., 2015 [51] | USA | Double-blind randomized controlled trial | 28 | A pregnancy BMI ≥ 30 kg/m2 | Cefazolin Concentrations in maternal plasma, umbilical cord blood, and maternal adipose tissue | 2 g or 3 g cefazolin concentrations within 30 min of skin incision | Cefazolin concentrations in plasma and adipose tissue were related to both dose and body mass index. No difference between 2 and 3 g cefazolin doses to maintain adipose tissue concentrations above the minimum inhibitory concentration |
| Swank et al., 2015 [52] | USA | Prospective control study | 29 | BMI ≥ 30 kg/m2 | Cefazolin concentration in tissue | 2 g or 3 g cefazolin concentrations within 30–60 min of skin incision | Higher adipose concentrations of cefazolin were observed after the administration of an increased prophylactic dose |
| Maggio et al., 2015 [53] | USA | Double-blind randomized controlled trial | 57 | BMI ≥ 30 kg/m2 | Adipose tissue cefazolin concentration | 2 g vs. 3 g cefazolin | Prophylaxis with 3 g of cefazolin did not significantly increase adipose tissue concentration |
| Lilico et al., 2016 [54] | Canada | Prospective control study | 6 | BMI ≥ 35 kg/m2 | Cefazolin concentration in tissue | 25 mg/kg of cefazolin | Obese patients required a higher dose of cefazolin |
| Groff et al., 2017 [55] | USA | Prospective controlled study | 8 | BMI ≥ 30 kg/m2 | Prevention of wound infection | 2 g of cefazolin | No difference between groups in total and free cefazolin concentrations |
| Gupper et al., 2017 [56] | USA | Analysis of 3 retrospective controlled studies | 67 | BMI ≥ 30 kg/m2 | Cefazolin adipose tissue concentration | 2 g or 3 g cefazolin concentrations within 30–60 min of skin incision | A 2 g dose of cefazolin had a high probability of providing adipose tissue concentrations above the target pathogens’ MIC for overweight and obese females |
| Kram et al., 2017 [57] | USA | Prospective controlled study | 84 | BMI ≥ 30 kg/m2 | Cefazolin blood and adipose tissue concentration | 2 g and 3 g of cefazolin for body weights <120 kg and ≥120 kg | Dosage groups did not differ in cefazolin concentration (median [interquartile range]) in adipose tissue following skin incision, and in adipose tissue before skin closure. Mean concentrations were significantly lower than the MIC of 8 mg/g (P < 0.03) in both groups |
| Eley et al., 2020 [58] | Australia | Prospective study | 12 | BMI ≥ 35 kg/m2 | Plasma and interstitial fluid pharmacokinetics of intravenous cefazolin | 2 g of cefazolin i.v. | Wound closure did not occur within 2 h; redosing is suggested following either a 2 or 3 g initial bolus |
| Study | N | BMI of Participants | Primary Outcomes | Dose of Antibiotics | Results |
|---|---|---|---|---|---|
| Pevzner et al., [48] | 29 | BMI < 30 kg/m2 (n = 10) BMI 30–39.9 kg/ m2 (n = 10) BMI ≥ 40 kg/m2 (n = 9) | Cefazolin concentration in adipose tissue and surgical site infection | 2 g of cefazolin 30–60 min before the skin incision | No significant difference in cefazolin concentration was observed in mean closure adipose, myometrial, or serum specimens across the BMI categories |
| Stitely et al., [49] | 20 | BMI ≥ 35 kg/m2 | Tissue concentration of antibiotics | Cefazolin 2 g vs. 4 g i.v. | The mean cefazolin plasma, umbilical cord, and myometrial concentrations were significantly higher in the 4 g treatment group (p < 0.05) |
| Ahmadzia et al., [50] | 335 | >250 pounds | Incidence of surgical site infections, (superficial, deep, and organ/space—i.e., endometritis) infections) | Cefazolin 2 g vs. cefazolin 3 g | No difference in surgical site infection among women who received 2 g compared with 3 g cefazolin |
| Young et al., [51] | 28 | Pregnancy BMI ≥ 30 kg/m2 | Cefazolin concentrations in maternal plasma, umbilical cord blood, and maternal adipose tissue | 2 g or 3 g within 30 min of the skin incision | Cefazolin concentrations in plasma and adipose tissue are related to both the dose and the body mass index. No difference between 2 g and 3 g cefazolin doses to maintain adipose tissue concentrations above the minimum inhibitory concentration |
| Swank et al., [52] | 29 | BMI ≥ 30 kg/m2 | Cefazolin concentration in tissue | 2 g or 3 g within 30–60 min of the skin incision | Higher adipose concentrations of cefazolin were observed after the administration of an increased prophylactic dose |
| Maggio et al., [53] | 57 | BMI ≥ 30 kg/m2 | Adipose tissue cefazolin concentration measured by high pressure liquid chromatography | 2 g vs. 3 g cefazolin | Prophylaxis with 3 g of cefazolin did not significantly increase adipose tissue concentration |
| Lilico et al., [54] | 6 | BMI ≥ 35 kg/m2 | Cefazolin concentration in tissue | 25 mg/kg of cefazolin | Obese patients need a higher dose of cefazolin |
| Groff et al., [55] | 8 | BMI ≥ 30 kg/m2 | Prevention of wound infection | 2 g of cefazolin | No difference between groups in total and free cefazolin concentrations |
| Gupper et al., [56] | 67 | BMI ≥ 30 kg/m2 | Cefazolin adipose tissue concentration | 2 g or 3 g within 30–60 min of skin incision | 2 g dose has a high probability of providing adipose tissue concentrations above the target pathogens’ MIC for overweight and obese females |
| Kram et al., [57] | 84 | BMI ≥30 kg/m2 | Cefazolin blood and adipose tissue concentration | 2 g and 3 g of cefazolin for body weights of <120 kg and ≥120 kg | Dosage groups did not differ in cefazolin concentration (median [interquartile range]) in adipose tissue following the skin incision, and in adipose tissue before the skin closure. Mean concentrations were significantly lower than the MIC of 8 mg/g (P < 0.03) in both groups |
| Eley et al., [58] | 12 | BMI ≥ 35 kg/m2 | plasma and interstitial fluid pharmacokinetics of intravenous cefazolin | 2 g of cefazolin i.v. | Wound closure did not occur within 2 h; redosing is suggested following either a 2 or 3 g initial bolus |
| Study | N | BMI (kg/m2) | Wound Complications | Results | |
|---|---|---|---|---|---|
| N | OR | ||||
| Alanis et al. [24] | 194 | ≥50 | V 39/104 T 19/90 | 2.24 (1.18–4.27) | Vertical abdominal incisions were associated with wound complications |
| McLean et al. [26] | 242 | ≥30 | V 5/25 T 22/213 | 2.17 (0.74–6.36) | Type of skin incision does not appear to be associated with wound complications in obese patients |
| Tornburg et al. [27] | 623 | ≥35 | V 16/35 T 68/588 | 6.44 (3.16–13.12) | Vertical skin incisions are associated with an increased risk of wound complications |
| Smid et al. [31] | 2411 | >45 | V 113/669 T 17/224 | 2.47 (1.45–4.22) | Vertical skin incisions are associated with an increased risk of wound complications |
| Sutton et al. [33] | 421 | ≥40 | V 15/57 T 54/364 | 2.05 (1.06–3.95) | Vertical incisions are associated with more wound complications |
| Marrs et al. [42] | 91 | ≥40 | V 8/38 T 8/43 | 1.17 (0.39–3.49) | Pfannenstiel skin incisions were associated with lower wound complications |
| Study | N | BMI (kg/m2) | Surgical Site Infection (SSI) | Results | |
|---|---|---|---|---|---|
| N | OR | ||||
| Looby et al. [36] | 467 | ≥40 | NPWT 13/234 SD 23/233 | 0.45 (0.22–0.95) | NPT after caesarean delivery in women with a BMI of ≥40 kg/m2 is an efficacious method to reduce the incidence of postoperative wound infections |
| Ruhstaller et al. [37] | 119 | ≥ 30 | NPWT 3/61 SD 4/58 | 0.70 (0.15–3.26) | Routine clinical use of a NPWT system after a caesarean delivery did not result in a significant reduction in wound morbidity over standard wound complications |
| Searle et al. [38] | 399 | ≥35 | NPWT 36/399 | - | Use of NPWT on closed surgical incisions may be associated with low incidence of SSI |
| Wihbey et al. [39] | 166 | ≥35 | NPWT 25/80 SD 29/86 | 0.89 (0.47–1.71) | There were no differences in the occurrence of composite wound complications between women using prophylactic NPWT |
| Hussamy et al. [43] | 441 | ≥40 | NPWT 37/222 SD 42/219 | 0.84 (0.52–1.37) | A NPWT device compared with a standard dressing did not significantly lower the wound complication rate in morbidly obese women undergoing caesarean delivery |
| Hylding et al. [44] | 876 | ≥ 30 | NPWT 20/432 SD 41/444 | 0.5 (0.30–0.84) | Prophylactic use of incisional NPWT reduced the risk of surgical site infections |
| Tuuli et al. [47] | 1624 | ≥ 30 | NPWT 52/806 SD 54/802 | 0.95 (0.66–1.37) | Prophylactic NPWT compared with a standard wound dressing did not significantly reduce the risk of surgical-site infection |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Słabuszewska-Jóźwiak, A.; Szymański, J.K.; Jóźwiak, Ł.; Sarecka-Hujar, B. A Systematic Review and Meta-Analysis of Wound Complications after a Caesarean Section in Obese Women. J. Clin. Med. 2021, 10, 675. https://doi.org/10.3390/jcm10040675
Słabuszewska-Jóźwiak A, Szymański JK, Jóźwiak Ł, Sarecka-Hujar B. A Systematic Review and Meta-Analysis of Wound Complications after a Caesarean Section in Obese Women. Journal of Clinical Medicine. 2021; 10(4):675. https://doi.org/10.3390/jcm10040675
Chicago/Turabian StyleSłabuszewska-Jóźwiak, Aneta, Jacek Krzysztof Szymański, Łukasz Jóźwiak, and Beata Sarecka-Hujar. 2021. "A Systematic Review and Meta-Analysis of Wound Complications after a Caesarean Section in Obese Women" Journal of Clinical Medicine 10, no. 4: 675. https://doi.org/10.3390/jcm10040675
APA StyleSłabuszewska-Jóźwiak, A., Szymański, J. K., Jóźwiak, Ł., & Sarecka-Hujar, B. (2021). A Systematic Review and Meta-Analysis of Wound Complications after a Caesarean Section in Obese Women. Journal of Clinical Medicine, 10(4), 675. https://doi.org/10.3390/jcm10040675








