Peroral Cholangioscopy-Guided Forceps Mapping Biopsy for Evaluation of the Lateral Extension of Biliary Tract Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Endoscopic Procedure
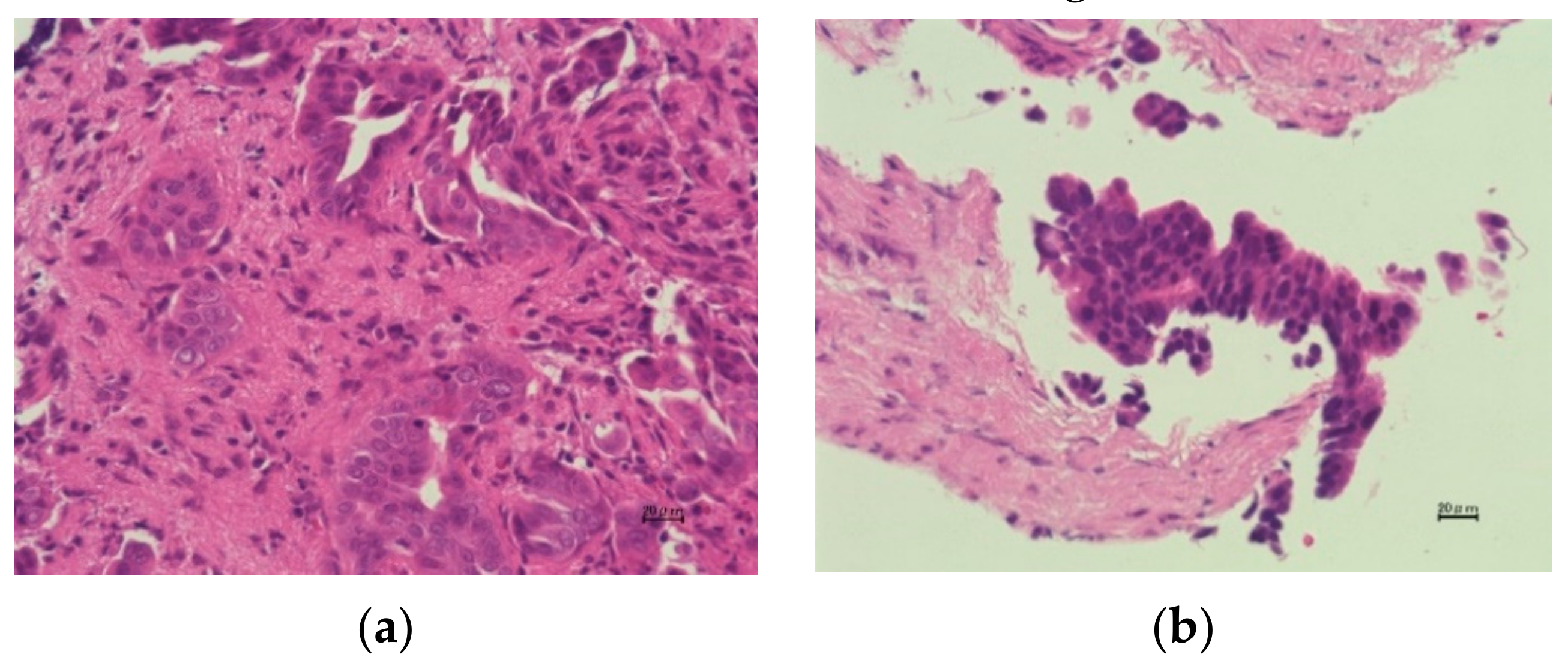
2.3. Diagnostic Criteria of POCS-Guided Forceps Mapping Biopsy
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics and Baseline Evaluation
3.2. Diagnostic Performance of POCS-Guided Forceps Mapping Biopsy
3.3. Factors Affecting the Accuracy of POCS-Guided Forceps Mapping Biopsy
3.4. Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flemming, J.A.; Zhang-Salomons, J.; Nanji, S.; Booth, C.M. Increased incidence but improved median overall survival for biliary tract cancers diagnosed in Ontario from 1994 through 2012: A population-based study. Cancer 2016, 122, 2534–2543. [Google Scholar] [CrossRef]
- Rizzo, A.; Ricci, A.D.; Brandi, G. Futibatinib, an investigational agent for the treatment of intrahepatic cholangiocarcinoma: Evidence to date and future perspectives. Expert Opin. Investig. Drugs 2020, 1–8. [Google Scholar] [CrossRef]
- Ishihara, S.; Horiguchi, A.; Miyakawa, S.; Endo, I.; Miyazaki, M.; Takada, T. Biliary tract cancer registry in Japan from 2008 to 2013. J. Hepatobiliary Pancreat. Sci. 2016, 23, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Wakai, T.; Shirai, Y.; Sakata, J.; Maruyama, T.; Ohashi, T.; Korira, P.V.; Ajioka, Y.; Hatakeyama, K. Clinicopathological features of benign biliary strictures masquerading as biliary malignancy. Am. Surg. 2012, 78, 1388–1391. [Google Scholar] [CrossRef]
- Trikudanathan, G.; Navaneethan, U.; Njei, B.; Vargo, J.J.; Parsi, M.A. Diagnostic yield of bile duct brushings for cholangiocarcinoma in primary sclerosing cholangitis: A systematic review and meta-analysis. Gastrointest. Endosc. 2014, 79, 783–789. [Google Scholar] [CrossRef]
- Badshah, M.B.; Vanar, V.; Kandula, M.; Kalva, N.; Badshah, M.B.; Revenur, V.; Bechtold, M.L.; Forcione, D.G.; Donthireddy, K.; Puli, S.R. Peroral cholangioscopy with cholangioscopy-directed biopsies in the diagnosis of biliary malignancies: A systemic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2019, 31, 935–940. [Google Scholar] [CrossRef]
- Rizzo, A.; Ricci, A.D.; Tavolari, S.; Brandi, G. Circulating tumor DNA in biliary tract cancer: Current evidence and future perspectives. Cancer Genom. Proteom. 2020, 17, 441–452. [Google Scholar] [CrossRef]
- Lapitz, A.; Arbelaiz, A.; O’Rourke, C.J.; Lavin, J.L.; Casta, A.L.; Ibarra, C.; Jimeno, J.P.; Santos-Laso, A.; Izquierdo-Sanchez, L.; Krawczyk, M.; et al. Patients with Cholangiocarcinoma Present Specific RNA Profiles in Serum and Urine Extracellular Vesicles Mirroring the Tumor Expression: Novel Liquid Biopsy Biomarkers for Disease Diagnosis. Cells 2020, 9, 721. [Google Scholar] [CrossRef] [PubMed]
- Wakai, T.; Shirai, Y.; Moroda, T.; Yokoyama, N.; Hatakeyama, K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer 2005, 103, 1210–1216. [Google Scholar] [CrossRef] [PubMed]
- Tsukahara, T.; Ebata, T.; Shimoyama, Y.; Yokoyama, Y.; Igami, T.; Sugawara, G.; Mizuno, T.; Nagino, M. Residual Carcinoma in Situ at the Ductal Stump has a Negative Survival Effect: An Analysis of Early-stage Cholangiocarcinomas. Ann. Surg. 2017, 266, 126–132. [Google Scholar] [CrossRef]
- Igami, T.; Nagino, M.; Oda, K.; Nishio, H.; Ebata, T.; Yokoyama, Y.; Shimoyama, Y. Clinicopathologic study of cholangiocarcinoma with superficial spread. Ann. Surg. 2009, 249, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Ruys, A.T.; Van Beem, B.E.; Engelbrecht, M.R.W.; Bipat, S.; Stoker, J.; Van Gulik, T.M. Radiological staging in patients with hilar cholangiocarcinoma: A systematic review and meta-analysis. Br. J. Radiol. 2012, 85, 1255–1262. [Google Scholar] [CrossRef]
- Campbell, W.L.; Peterson, M.S.; Federle, M.P.; Siqueira, E.S.; Slivka, A.; Grazioli, L.; Ichikawa, T.; Oliver, J.H., 3rd; Kim, T.; Li, W. Using CT and cholangiography to diagnose biliary tract carcinoma complicating primary sclerosing cholangitis. AJR Am. J. Roentgenol. 2001, 177, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Hijioka, S.; Hara, K.; Mizuno, N.; Imaoka, H.; Mekky, M.A.; Nagashio, Y.; Sekine, M.; Tajika, M.; Tanaka, T.; Ishihara, M.; et al. A novel technique for endoscopic transpapillary “mapping biopsy specimens” of superficial intraductal spread of bile duct carcinoma (with videos). Gastrointest. Endosc. 2014, 79, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Navaneethan, U.; Hasan, M.K.; Lourdusamy, V.; Njei, B.; Varadarajulu, S.; Hawes, R.H. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: A systematic review. Gastrointest. Endosc. 2015, 82, 608–614.e2. [Google Scholar] [CrossRef]
- Almadi, M.A.; Itoi, T.; Moon, J.H.; Goenka, M.K.; Seo, D.W.; Rerknimitr, R.; Lau, J.Y.; Maydeo, A.P.; Lee, J.K.; Nguyen, N.Q.; et al. Using single-operator cholangioscopy for endoscopic evaluation of indeterminate biliary strictures: Results from a large multinational registry. Endoscopy 2020, 52, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Itoi, T.; Igarashi, Y.; Tanaka, K.; Kida, M.; Maguchi, H.; Yasuda, K.; Okano, N.; Imaizumi, H.; Itokawa, F. Peroral video cholangioscopy to evaluate indeterminate bile duct lesions and preoperative mucosal cancerous extension: A prospective multicenter study. Endoscopy 2013, 45, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Kim, M.H.; Lee, S.K.; Kim, T.K.; Seo, D.W.; Park, J.S.; Hwang, C.Y.; Chang, H.S.; Min, Y. Il MR cholangiography versus cholangioscopy for evaluation of longitudinal extension of hilar cholangiocarcinoma. Gastrointest. Endosc. 2002, 56, 25–32. [Google Scholar] [CrossRef]
- Nishikawa, T.; Tsuyuguchi, T.; Sakai, Y.; Sugiyama, H.; Kishimoto, T.; Ohtsuka, M.; Miyazaki, M.; Yokosuka, O. Preoperative assessment of longitudinal extension of cholangiocarcinoma with peroral video-cholangioscopy: A prospective study. Dig. Endosc. 2014, 26, 450–457. [Google Scholar] [CrossRef]
- Tamada, K.; Ushio, J.; Sugano, K. Endoscopic diagnosis of extrahepatic bile duct carcinoma: Advances and current limitations. World J. Clin. Oncol. 2011, 2, 203. [Google Scholar] [CrossRef]
- Domagk, D.; Wessling, J.; Reimer, P.; Hertel, L.; Poremba, C.; Senninger, N.; Heinecke, A.; Domschke, W.; Menzel, J. Endoscopic retrograde cholangiopancreatography, intraductal ultrasonography, and magnetic resonance cholangiopancreatography in bile duct strictures: A prospective comparison of imaging diagnostics with histopathological correlation. Am. J. Gastroenterol. 2004, 99, 1684–1689. [Google Scholar] [CrossRef]
- Unno, M.; Okumoto, T.; Katayose, Y.; Rikiyama, T.; Sato, A.; Motoi, F.; Oikawa, M.; Egawa, S.; Ishibashi, T. Preoperative assessment of hilar cholangiocarcinoma by multidetector row computed tomography. J. Hepatobiliary Pancreat. Surg. 2007, 14, 434–440. [Google Scholar] [CrossRef]
- Asada-Hirayama, I.; Kodashima, S.; Sakaguchi, Y.; Ono, S.; Niimi, K.; Mochizuki, S.; Tsuji, Y.; Minatsuki, C.; Shichijo, S.; Matsuzaka, K.; et al. Magnifying endoscopy with narrow-band imaging is more accurate for determination of horizontal extent of early gastric cancers than chromoendoscopy. Endosc. Int. Open 2016, 4, E690–E698. [Google Scholar] [CrossRef]
- Nagahama, T.; Yao, K.; Uedo, N.; Doyama, H.; Ueo, T.; Uchita, K.; Ishikawa, H.; Kanesaka, T.; Takeda, Y.; Wada, K.; et al. Delineation of the extent of early gastric cancer by magnifying narrow-band imaging and chromoendoscopy: A multicenter randomized controlled trial. Endoscopy 2018, 50, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Ito, K.; Koshita, S.; Kanno, Y.; Masu, K.; Kusunose, H.; Sakai, T.; Murabayashi, T.; Hasegawa, S.; Noda, Y. Usefulness of cholangioscopic-guided mapping biopsy using SpyGlass DS for preoperative evaluation of extrahepatic cholangiocarcinoma: A pilot study. Endosc. Int. Open 2018, 6, E199–E204. [Google Scholar] [CrossRef] [PubMed]
- Onoyama, T.; Takeda, Y.; Kawata, S.; Kurumi, H.; Koda, H.; Yamashita, T.; Hamamoto, W.; Sakamoto, Y.; Matsumoto, K.; Isomoto, H. Adequate tissue acquisition rate of peroral cholangioscopy-guided forceps biopsy. Ann. Transl. Med. 2020, 8, 1073. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, T.; Tsuyuguchi, T.; Sakai, Y.; Sugiyama, H.; Miyazaki, M.; Yokosuka, O. Comparison of the diagnostic accuracy of peroral video-cholangioscopic visual findings and cholangioscopy-guided forceps biopsy findings for indeterminate biliary lesions: A prospective study. Gastrointest. Endosc. 2013, 77, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Maetani, I.; Terada, K.; Ukita, T.; Tada, T.; Shigoka, H.; Omuta, S.; Takahashi, K. Usefulness of endoscopic retrograde biliary biopsy using large-capacity forceps for extrahepatic biliary strictures: A prospective randomized study. Endoscopy 2010, 42, 837–841. [Google Scholar] [CrossRef] [PubMed]




| Patients with BTC (n = 23) | |
|---|---|
| Age, years | 72 (56–84) |
| Sex, male/female | 16/7 |
| Location of BTC (n = 24) | |
| Distal | 16 |
| Perihilar | 4 |
| Cystic duct | 3 |
| Gall bladder | 1 |
| Length of stricture, mm (n = 24) | 16.8 (4.8–45.6) |
| Acute cholangitis (presence/absence) (n = 24) | 22/2 |
| Total bilirubin, mg/dL | 1.6 (0.5–14.8) |
| Tumor marker | |
| CEA, ng/mL | 2.6 (0.8–8.3) |
| CA19-9, U/mL | 35.2 (6.4–9052.0) |
| Macroscopic type (n = 24) | |
| Papillary type | 5 |
| Nodular type | 13 |
| Flat type | 6 |
| Histological differentiation (n = 24) | |
| Well differentiated tubular adenocarcinoma | 12 |
| Moderately differentiated tubular adenocarcinoma | 7 |
| Poorly differentiated adenocarcinoma | 3 |
| Papillary adenocarcinoma | 2 |
| TNM classification/Stage (n = 24) | |
| Distal | |
| T category 1/2/3/4 | 2/8/6/0 |
| N category 0/1 | 4/12 |
| M category 0/1 | 16/0 |
| Stage IA/IB/IIA/IIB/III/IV | 2/4/6/4/0/0 |
| Perihilar | |
| T category 1/2/3/4 | 0/4/0/0 |
| N category 0/1 | 1/3 |
| M category 0/1 | 4/0 |
| Stage I/II/IIIA/IIIB/IVA/IVB | 0/3/0/1/0/0 |
| Gall bladder/Cystic duct | |
| T category 1/2/3/4 | 0/2/2/0 |
| N category 0/1 | 4/0 |
| M category 0/1 | 4/0 |
| Stage I/II/IIIA/IIIB/IVA/IVB | 0/2/2/0/0/0 |
| POCS (n = 24) | |
|---|---|
| Procedure time, minutes | 85.0 (57–124) |
| EST, previous/with/without | 7/14/3 |
| Number of biopsy, times | 2 (1–4) |
| Biopsy Site | Sensitivity, % | Specificity, % | Accuracy, % |
|---|---|---|---|
| Total | 53.8 (7/13) | 63.9 (46/71) | 63.1 (53/84) |
| Distal bile duct | 50.0 (1/2) | 40.0 (2/5) | 42.9 (3/7) |
| Junction of the cystic duct | 50.0 (2/4) | 100 (4/4) | 75.0 (6/8) |
| Perihilar bile duct | 0 (0/1) | 0 (0/2) | 0 (0/3) |
| Confluence of the hepatic duct | 66.7 (2/3) | 70.6 (12/17) | 70.0 (14/20) |
| Right hepatic duct | 0 (0/1) | 50.0 (1/2) | 33.3 (1/3) |
| Confluence of the anterior and posterior segmental ducts | 100 (1/1) | 58.3 (7/12) | 61.5 (8/13) |
| Confluence of B5 and B8 segmental ducts | 100 (1/1) | 50.0 (2/4) | 60.0 (3/5) |
| Confluence of B6 and B7 segmental ducts | - | 100 (2/2) | 100 (2/2) |
| Left hepatic duct | - | 60.0 (3/5) | 60.0 (3/5) |
| B4 confluence | - | 50.0 (4/8) | 50.0 (4/8) |
| Confluence of B2 and B3 segmental ducts | - | 90.0 (9/10) | 90.0 (9/10) |
| Univariate Analyses | |||
| Subgroup | Odds Ratio | 95% CI | p Value |
| Age, <75 years or ≥75 years | 0.554 | 0.226–1.357 | 0.196 |
| Sex, male or female | 1.744 | 0.700–4.344 | 0.232 |
| Location of biliary tract cancer, distal or not distal | 2.411 | 0.904–6.434 | 0.079 |
| Length of stricture of biliary tract, <15mm or ≥15mm | 0.909 | 0.369–2.237 | 0.835 |
| Macroscopic type, flat type or not-flat type | 0.669 | 0.232–1.927 | 0.669 |
| histological differentiation (tubular adenocarcinoma or not) | 0.734 | 0.229–2.353 | 0.603 |
| T category, T<3 or ≥3 | 0.726 | 0.286–1.844 | 0.500 |
| Cholangitis, presence or absence | 0.972 | 0.216–4.380 | 0.971 |
| T-Bil, <1.5 mg/dl or ≥1.5 mg/dl | 0.584 | 0.239–1.429 | 0.239 |
| CEA, < 5.0 ng/mL or ≥5.0 ng/mL | 1.496 | 0.519–4.311 | 0.456 |
| CA19-9, U/mL <35 U/mL or ≥35 U/mL | 0.809 | 0.331–1.978 | 0.642 |
| Procedure time, <75 min or ≥75 min | 1.003 | 0.348–2.895 | 0.995 |
| EST or non-EST | 4.000 | 0.923–17.340 | 0.064 |
| Number of biopsy, <2 or ≥2 | 0.841 | 0.300–2.357 | 0.743 |
| Previous biliary stenting, presence or absence | 0.682 | 0.280–1.660 | 0.399 |
| Biopsy site | |||
| Intrahepatic bile duct or extrahepatic bile duct | 1.525 | 0.619–3.755 | 0.359 |
| Bifurcation of biliary tract or not | 3.614 | 1.223–10.678 | 0.020 |
| Right side or left side | 0.681 | 0.201–2.307 | 0.537 |
| Multivariate Analyses | |||
| Subgroup | Odds Ratio | 95% CI | p Value |
| Location of biliary tract cancer, distal or not distal | 1.974 | 0.695–5.604 | 0.201 |
| EST or non-EST | 3.924 | 0.849–18.130 | 0.080 |
| Biopsy site, bifurcation or not | 3.538 | 1.151–10.875 | 0.027 |
| Adverse Event | POCS-Guided Forceps Mapping Biopsy (n = 24) |
|---|---|
| Pancreatitis | 12.5% (3/24) |
| Bleeding | 0 |
| Infection | 4.2% (1/24) |
| Perforation | 0 |
| Cardiac | 0 |
| Pulmonary | 0 |
| Medication reaction | 0 |
| Other | 0 |
| Overall | 16.7% (4/24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onoyama, T.; Hamamoto, W.; Sakamoto, Y.; Kawahara, S.; Yamashita, T.; Koda, H.; Kawata, S.; Takeda, Y.; Matsumoto, K.; Isomoto, H. Peroral Cholangioscopy-Guided Forceps Mapping Biopsy for Evaluation of the Lateral Extension of Biliary Tract Cancer. J. Clin. Med. 2021, 10, 597. https://doi.org/10.3390/jcm10040597
Onoyama T, Hamamoto W, Sakamoto Y, Kawahara S, Yamashita T, Koda H, Kawata S, Takeda Y, Matsumoto K, Isomoto H. Peroral Cholangioscopy-Guided Forceps Mapping Biopsy for Evaluation of the Lateral Extension of Biliary Tract Cancer. Journal of Clinical Medicine. 2021; 10(4):597. https://doi.org/10.3390/jcm10040597
Chicago/Turabian StyleOnoyama, Takumi, Wataru Hamamoto, Yuri Sakamoto, Shiho Kawahara, Taro Yamashita, Hiroki Koda, Soichiro Kawata, Yohei Takeda, Kazuya Matsumoto, and Hajime Isomoto. 2021. "Peroral Cholangioscopy-Guided Forceps Mapping Biopsy for Evaluation of the Lateral Extension of Biliary Tract Cancer" Journal of Clinical Medicine 10, no. 4: 597. https://doi.org/10.3390/jcm10040597
APA StyleOnoyama, T., Hamamoto, W., Sakamoto, Y., Kawahara, S., Yamashita, T., Koda, H., Kawata, S., Takeda, Y., Matsumoto, K., & Isomoto, H. (2021). Peroral Cholangioscopy-Guided Forceps Mapping Biopsy for Evaluation of the Lateral Extension of Biliary Tract Cancer. Journal of Clinical Medicine, 10(4), 597. https://doi.org/10.3390/jcm10040597







