Analysis of Affecting Factors of the Fate of Medial Meniscus Posterior Root Tear Based on Treatment Strategies
Abstract
1. Introduction
2. Materials and Methods
2.1. Extraction of Affecting Factors
2.1.1. Anthropometric Factors
2.1.2. Medical Factors
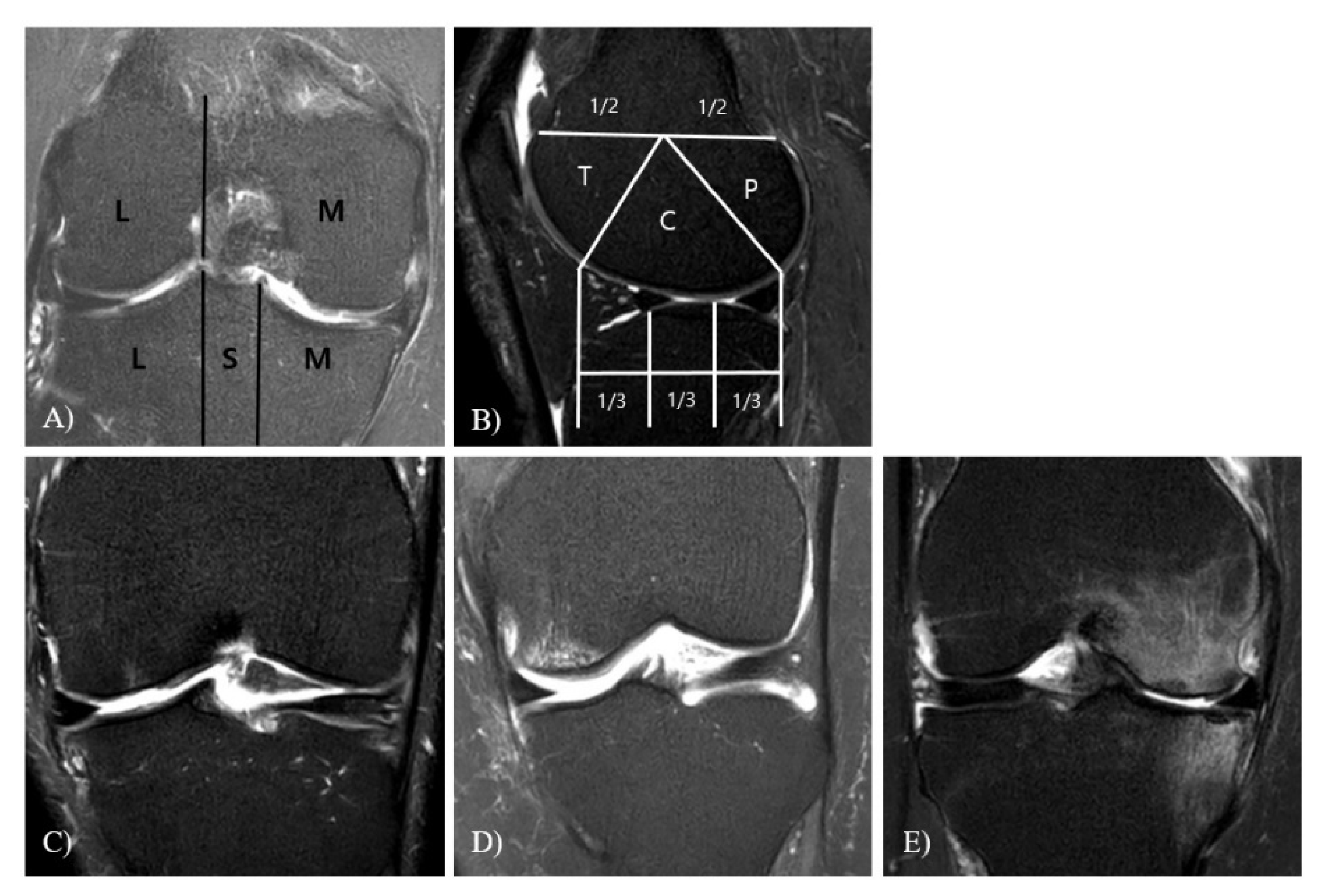
WBL
TVA
PTS
K-L Grade
MOAKS
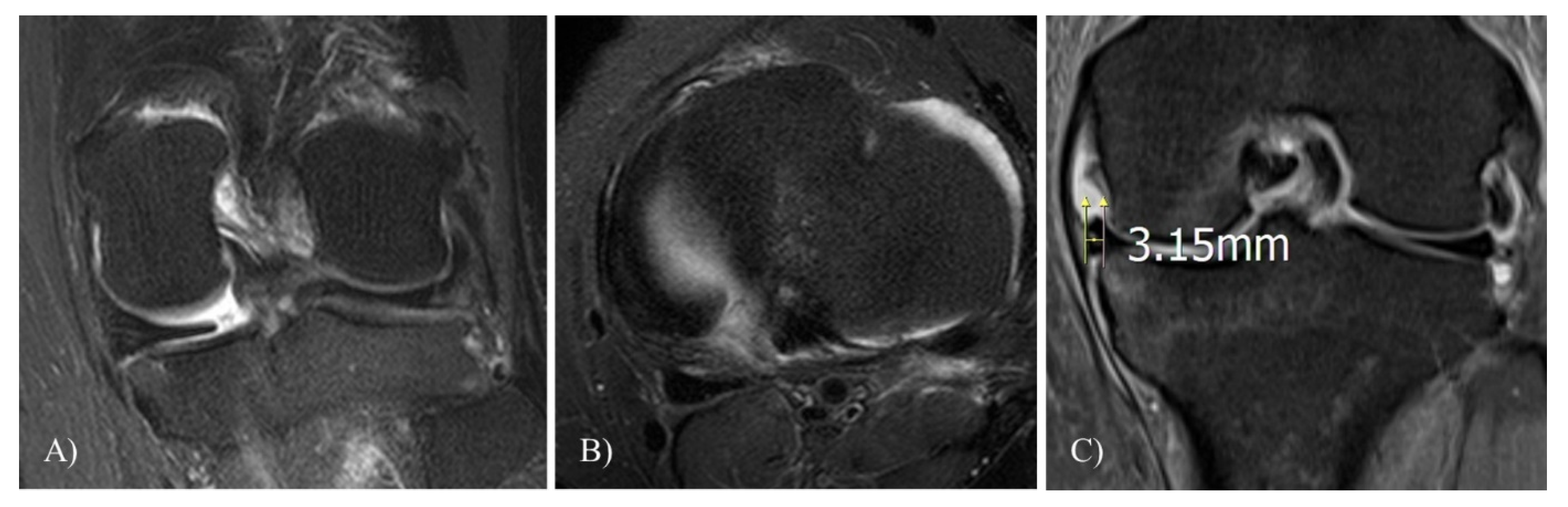
Meniscal Extrusion
2.2. Statistical Analysis
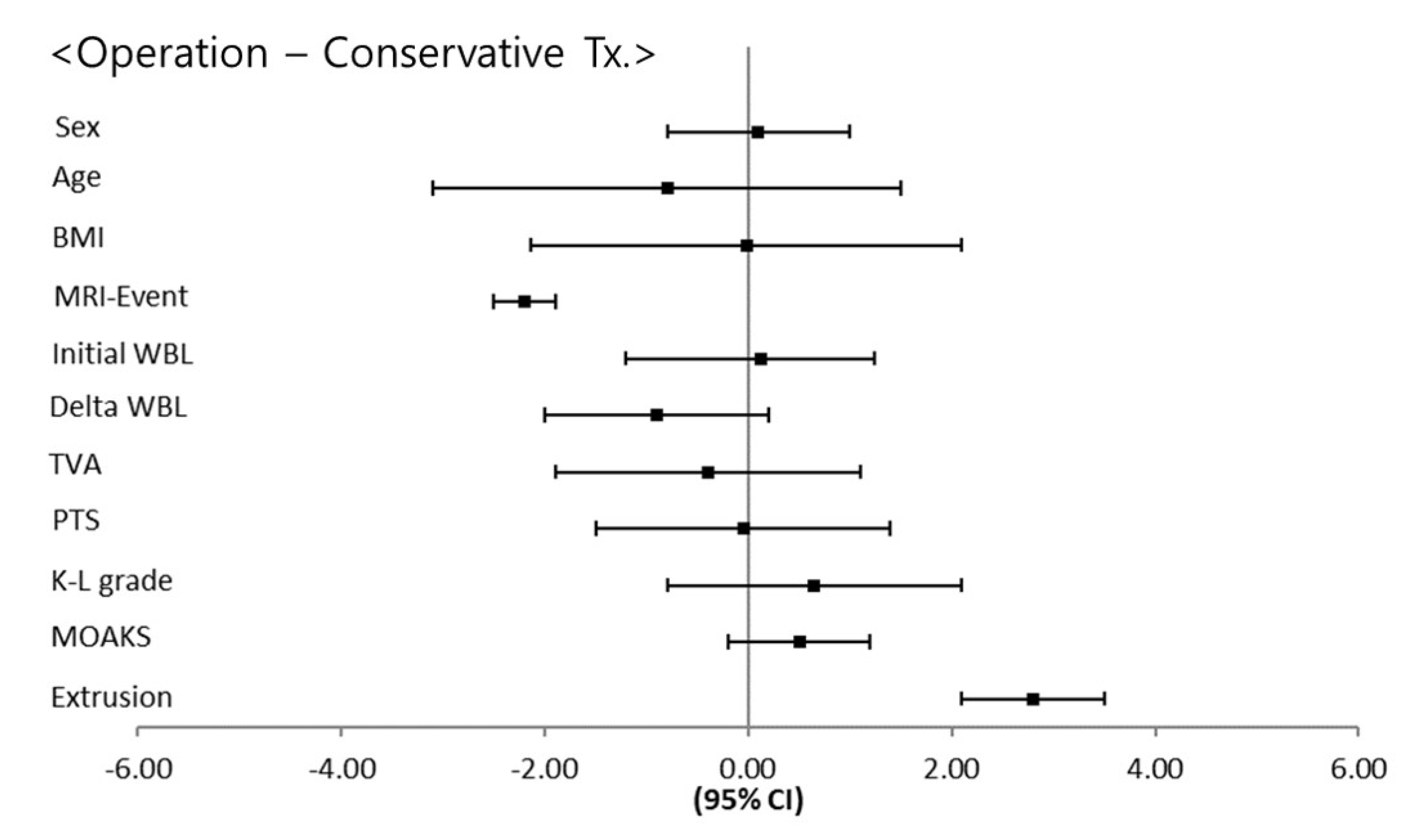
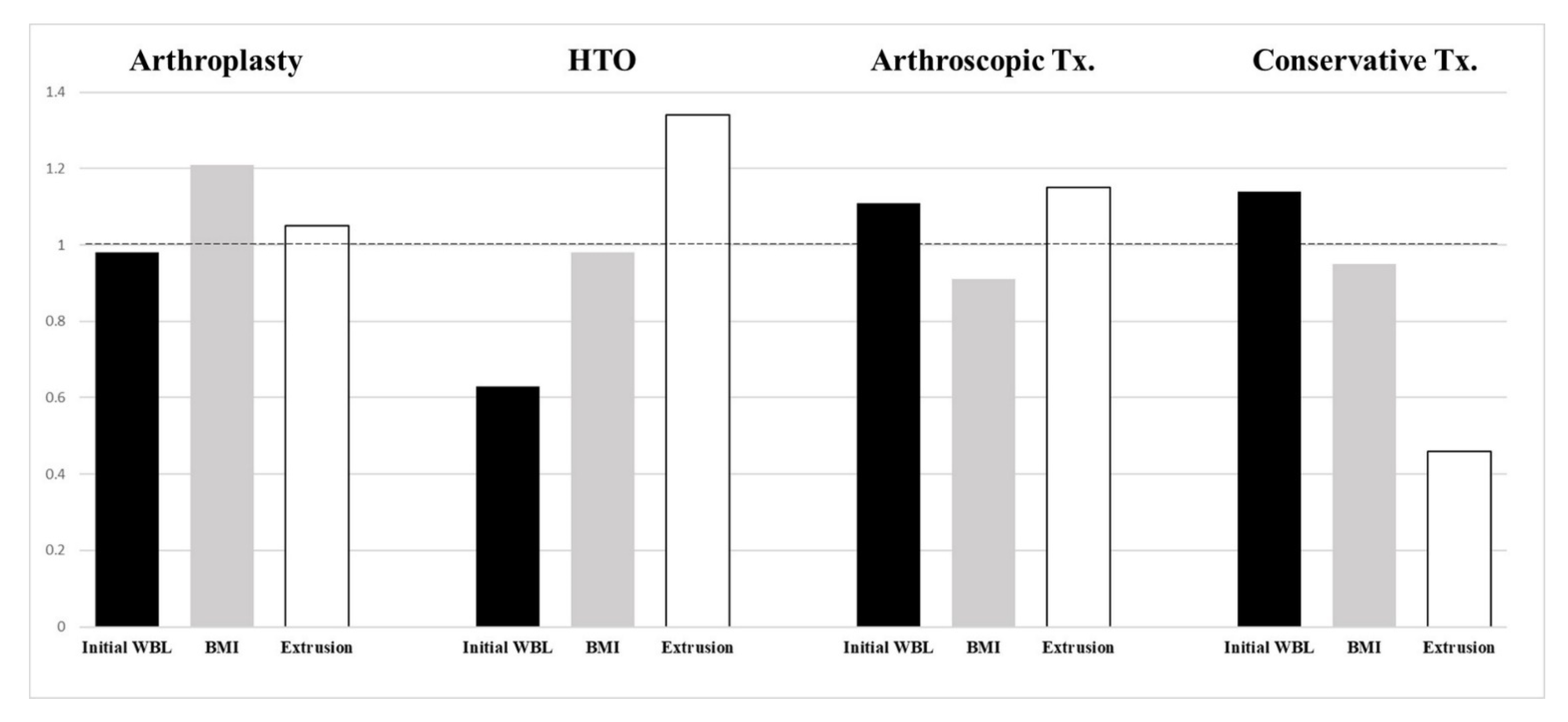
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fithian, D.C.; Kelly, M.A.; Mow, V.C. Material properties and structure-function relationships in the menisci. Clin. Orthop. Relat. Res. 1990, 252, 19–31. [Google Scholar] [CrossRef]
- Koenig, J.H.; Ranawat, A.S.; Umans, H.R.; Difelice, G.S. Meniscal root tears: Diagnosis and treatment. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Greis, P.E.; Bardana, D.D.; Holmstrom, M.C.; Burks, R.T. Meniscal injury: I. Basic science and evaluation. J. Am. Acad. Orthop. Surg. 2002, 10, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Kan, A.; Oshida, M.; Oshida, S.; Imada, M.; Nakagawa, T.; Okinaga, S. Anatomical significance of a posterior horn of medial meniscus: The relationship between its radial tear and cartilage degradation of joint surface. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2010, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Vyas, D.; Harner, C.D. Meniscus root repair. Sports Med. Arthrosc. Rev. 2012, 20, 86–94. [Google Scholar] [CrossRef]
- Furumatsu, T.; Kamatsuki, Y.; Fujii, M.; Kodama, Y.; Okazaki, Y.; Masuda, S.; Ozaki, T. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop. Traumatol. Surg. Res. 2017, 103, 1179–1182. [Google Scholar] [CrossRef]
- Bin, S.I.; Kim, J.M.; Shin, S.J. Radial tears of the posterior horn of the medial meniscus. Arthrosc. J. Arthrosc. Relat. Surg. 2004, 20, 373–378. [Google Scholar] [CrossRef]
- Pache, S.; Aman, Z.S.; Kennedy, M.; Nakama, G.Y.; Moatshe, G.; Ziegler, C.; LaPrade, R.F. Meniscal Root Tears: Current Concepts Review. Arch. Bone Jt. Surg. 2018, 6, 250–259. [Google Scholar]
- Vedi, V.; Williams, A.; Tennant, S.J.; Spouse, E.; Hunt, D.M.; Gedroyc, W.M. Meniscal movement. An in-vivo study using dynamic MRI. J. Bone Jt. Surg. Br. Vol. 1999, 81, 37–41. [Google Scholar] [CrossRef]
- Yamagami, R.; Taketomi, S.; Inui, H.; Tahara, K.; Tanaka, S. The role of medial meniscus posterior root tear and proximal tibial morphology in the development of spontaneous osteonecrosis and osteoarthritis of the knee. Knee 2017, 24, 390–395. [Google Scholar] [CrossRef]
- Furumatsu, T.; Kodama, Y.; Kamatsuki, Y.; Hino, T.; Okazaki, Y.; Ozaki, T. Meniscal Extrusion Progresses Shortly after the Medial Meniscus Posterior Root Tear. Knee Surg. Relat. Res. 2017, 29, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.S.; Park, S.J. Clinical Evaluation of the Root Tear of the Posterior Horn of the Medial Meniscus in Total Knee Arthroplasty for Osteoarthritis. Knee Surg. Relat. Res. 2015, 27, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Bonadio, M.B.; Filho, A.G.O.; Helito, C.P.; Stump, X.M.; Demange, M.K. Bone Marrow Lesion: Image, Clinical Presentation, and Treatment. Magn. Reson. Insights 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Van Raaij, T.M.; Takacs, I.; Reijman, M.; Verhaar, J.A. Varus inclination of the proximal tibia or the distal femur does not influence high tibial osteotomy outcome. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 390–395. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef]
- Hunter, D.J.; Guermazi, A.; Lo, G.H.; Grainger, A.J.; Conaghan, P.G.; Boudreau, R.M.; Roemer, F.W. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthr. Cartil. 2011, 19, 990–1002. [Google Scholar] [CrossRef]
- Hackshaw, A.; Kirkwood, A. Interpreting and reporting clinical trials with results of borderline significance. BMJ 2011, 343, d3340. [Google Scholar] [CrossRef]
- Ozkoc, G.; Circi, E.; Gonc, U.; Irgit, K.; Pourbagher, A.; Tandogan, R.N. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 849–854. [Google Scholar] [CrossRef]
- Ford, G.M.; Hegmann, K.T.; White, G.L., Jr.; Holmes, E.B. Associations of body mass index with meniscal tears. Am. J. Prev. Med. 2005, 28, 364–368. [Google Scholar]
- Hashikawa, T.; Osaki, M.; Ye, Z.; Tomita, M.; Abe, Y.; Honda, S.; Aoyagi, K. Factors associated with radiographic osteoarthritis of the knee among community-dwelling Japanese women: The Hizen-Oshima Study. J. Orthop. Sci. 2011, 16, 51–55. [Google Scholar] [CrossRef]
- Primeau, C.A.; Birmingham, T.B.; Leitch, K.M.; Appleton, C.T.; Giffin, J.R. Degenerative Meniscal Tears and High Tibial Osteotomy: Do Current Treatment Algorithms Need to Be Realigned? Clin. Sports Med. 2019, 38, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Shelburne, K.B.; Kim, H.J.; Sterett, W.I.; Pandy, M.G. Effect of posterior tibial slope on knee biomechanics during functional activity. J. Orthop. Res. 2011, 29, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, Y.; Furumatsu, T.; Kodama, Y.; Kamatsuki, Y.; Okazaki, Y.; Hiranaka, T.; Ozaki, T. Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg. Sports Traumatol. Arthrosc. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Choi, Y.J.; Shin, K.Y.; Choi, C.H. Medial meniscal tears in anterior cruciate ligament-deficient knees: Effects of posterior tibial slope on medial meniscal tear. Knee Surg. Relat. Res. 2011, 23, 227–230. [Google Scholar] [CrossRef] [PubMed]
- Scher, C.; Craig, J.; Nelson, F. Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skelet. Radiol. 2008, 37, 609–617. [Google Scholar] [CrossRef]
- Kon, E.; Ronga, M.; Filardo, G.; Farr, J.; Madry, H.; Milano, G.; Shabshin, N. Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1797–1814. [Google Scholar] [CrossRef]


| Arthroplasty (36) | HTO (150) | Arthroscopic Tx. (55) | Conservative Tx. (399) | p-Value | |
|---|---|---|---|---|---|
| Male/Female ratio | 5:31 | 31:119 | 24:31 | 155:244 | n.s. |
| Anthropometric | |||||
| Age (years) | 69.25 ± 6.02 | 58.12 ± 4.18 | 43.26 ± 15.26 | 57.13 ± 15.16 | 0.001 * |
| BMI (kg/m²) | 29.72 ± 2.83 | 26.67 ± 3.16 | 26.42 ± 2.63 | 25.92 ± 2.87 | 0.001 * |
| MRI—Event (years) | 1.17 ± 0.97 | 0.88 ± 1.32 | 0.95 ± 0.41 | 3.13 ± 2.21 | 0.001 * |
| Medical factors | |||||
| Initial WBL (ratio) | 31.44 ± 16.42 | 21.06 ± 11.03 | 38.22 ± 10.59 | 36.24 ± 9.32 | 0.001 * |
| Delta WBL (ratio) | 4.21 ± 1.77 | 7.32 ± 3.46 | 3.06 ± 2.10 | 2.76 ± 1.09 | 0.001 * |
| TVA (degree) | 5.32 ± 1.17 | 5.44 ± 0.85 | 5.18 ± 0.84 | 5.07 ± 1.60 | n.s. |
| PTS (degree) | 11.25 ± 2.55 | 11.03 ± 1.72 | 10.85 ± 1.44 | 11.11 ± 3.48 | n.s. |
| K-L grade | 3.78 ± 0.42 | 2.18 ± 0.39 | 2.05 ± 0.65 | 2.01 ± 1.06 | 0.001 * |
| MOAKS | 2.11 ± 0.67 | 1.96 ± 0.69 | 1.98 ± 0.71 | 1.83 ± 1.02 | n.s. |
| Extrusion (mm) | 3.13 ± 1.36 | 3.98 ± 1.01 | 3.43 ± 1.09 | 1.36 ± 1.51 | 0.001 * |
| Variable | Sex | Age | BMI | MRI-Event | Initial WBL | Delta WBL | TVA | PTS | K-L Grade | MOAKS | Extrusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | 1 | 0.091 | 0.121 | 0.131 | 0.089 | 0.187 | 0.023 | 0.119 | 0.087 | 0.076 | 0.107 |
| Age | 1 | −0.008 | 0.093 | 0.121 | 0.129 | −0.019 | 0.110 | 0.251 | 0.095 | 0.117 | |
| BMI | 1 | −0.217 | 0.093 | 0.212 | 0.091 | 0.034 | 0.367 * | 0.198 | 0.201 | ||
| MRI-Event | 1 | 0.132 | −0.229 | 0.079 | 0.101 | 0.211 | −0.103 | −0.418 * | |||
| Initial WBL | 1 | −0.332 * | 0.013 | 0.094 | 0.202 | 0.081 | 0.071 | ||||
| Delta WBL | 1 | 0.113 | 0.019 | 0.204 | 0.109 | 0.208 | |||||
| TVA | 1 | 0.131 | 0.042 | 0.077 | 0.016 | ||||||
| PTS | 1 | 0.076 | 0.109 | 0.129 | |||||||
| K-L Grade | 1 | 0.098 | 0.142 | ||||||||
| MOAKS | 1 | 0.173 | |||||||||
| Extrusion | 1 |
| Independent Variable | Dependent Variable | Regression Coefficient (ß) | p Value |
|---|---|---|---|
| Initial WBL | Delta WBL | −0.195 | 0.034 * |
| BMI | K-L grade | 0.492 | 0.021 * |
| Meniscal extrusion | MRI-Event | −0.924 | 0.029 * |
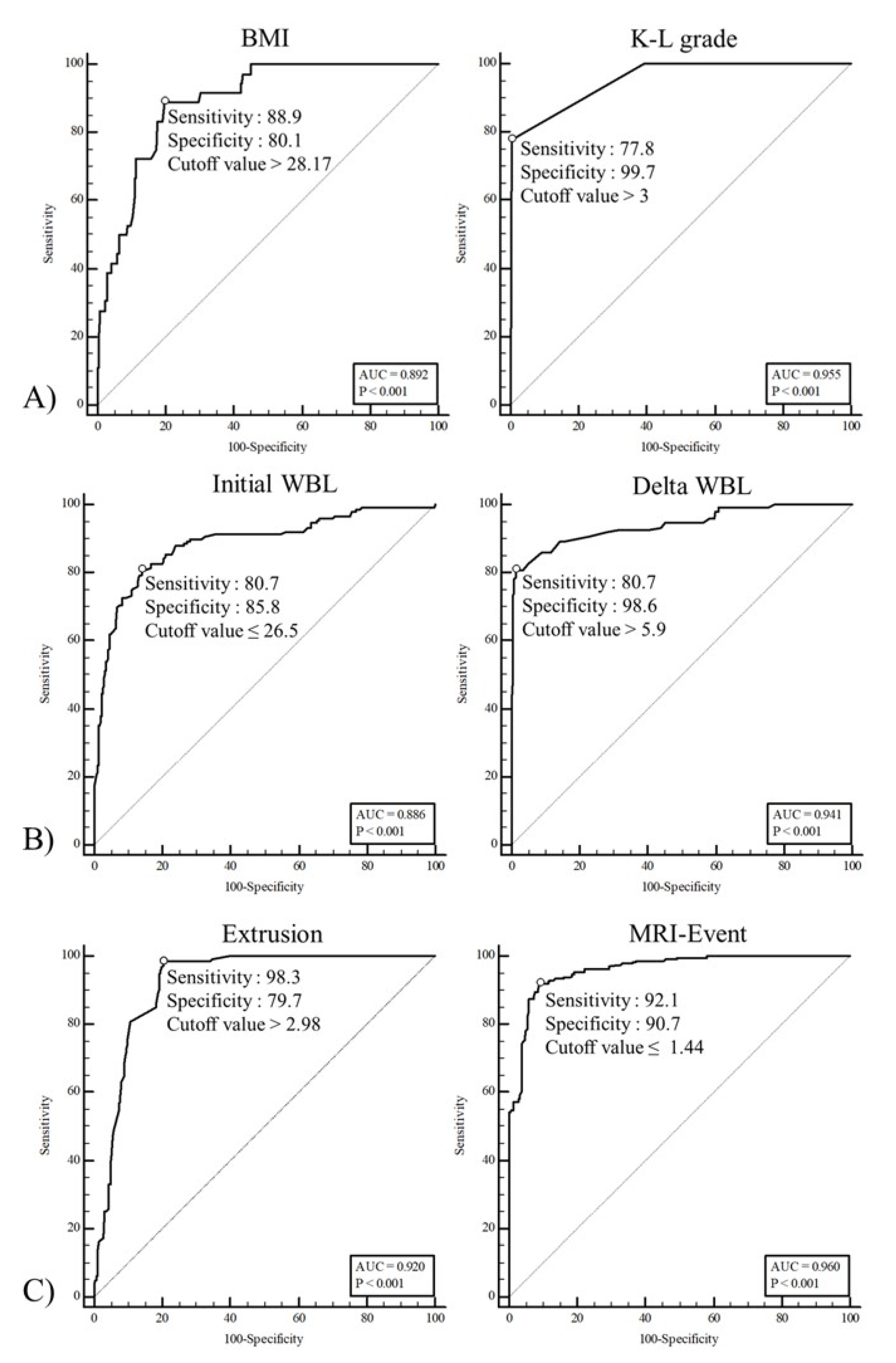
| Variable | AUC | SE | p Value | 95% CI |
|---|---|---|---|---|
| BMI | 0.892 | 0.021 | 0.001 * | 0.865–0.915 |
| K-L grade | 0.955 | 0.014 | 0.001 * | 0.935– 0.969 |
| Initial WBL ratio | 0.886 | 0.017 | 0.001 * | 0.859–0.910 |
| Delta WBL ratio | 0.941 | 0.013 | 0.001 * | 0.919–0.958 |
| Extrusion | 0.920 | 0.011 | 0.001 * | 0.896–0.940 |
| MRI-event | 0.960 | 0.007 | 0.001 * | 0.942–0.974 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.I.; Kim, D.H.; Choi, H.G.; Kim, T.W.; Lee, Y.S. Analysis of Affecting Factors of the Fate of Medial Meniscus Posterior Root Tear Based on Treatment Strategies. J. Clin. Med. 2021, 10, 557. https://doi.org/10.3390/jcm10040557
Lee JI, Kim DH, Choi HG, Kim TW, Lee YS. Analysis of Affecting Factors of the Fate of Medial Meniscus Posterior Root Tear Based on Treatment Strategies. Journal of Clinical Medicine. 2021; 10(4):557. https://doi.org/10.3390/jcm10040557
Chicago/Turabian StyleLee, Jae Ik, Dong Hyun Kim, Han Gyeol Choi, Tae Woo Kim, and Yong Seuk Lee. 2021. "Analysis of Affecting Factors of the Fate of Medial Meniscus Posterior Root Tear Based on Treatment Strategies" Journal of Clinical Medicine 10, no. 4: 557. https://doi.org/10.3390/jcm10040557
APA StyleLee, J. I., Kim, D. H., Choi, H. G., Kim, T. W., & Lee, Y. S. (2021). Analysis of Affecting Factors of the Fate of Medial Meniscus Posterior Root Tear Based on Treatment Strategies. Journal of Clinical Medicine, 10(4), 557. https://doi.org/10.3390/jcm10040557







