Impact of 1-Hour Bundle Achievement in Septic Shock
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Definitions and Outcomes
2.3. Statistical Analyses
3. Results
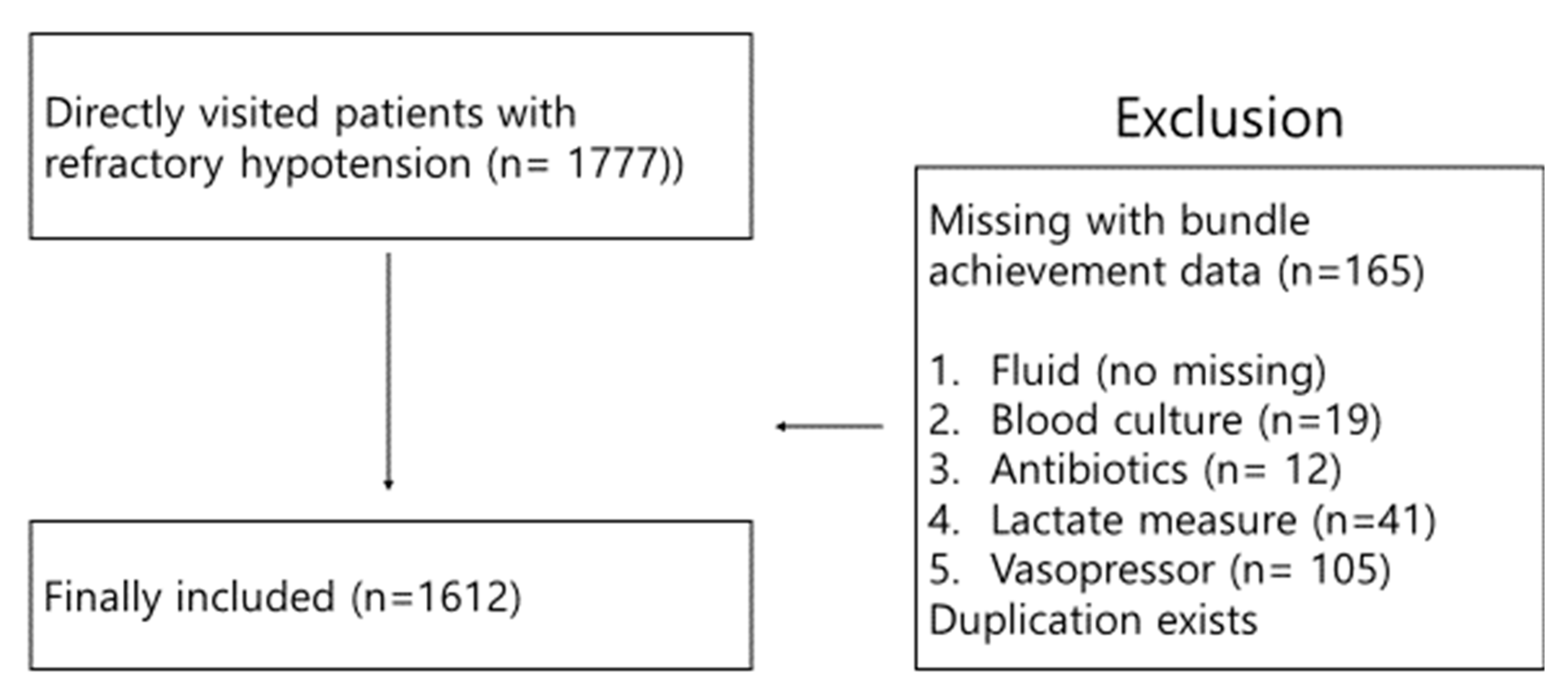
3.1. Participant Characteristics
3.2. Multivariate Logistic Regression Analysis of 1-, 3- and 6- h Bundle Achievement to Predict in-Hospital Mortality (2 Group Comparison)
3.3. Comparison of Outcomes to Examine the Linear Relationship for 3 Groups over Time: Group 1 (≤1 h; Reference), 2 (1–3 h), and 3 (3–6 h)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [Green Version]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.A.; Welch, C.A.; Eddleston, J.M. The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: Secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit. Care 2006, 10, R42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaukonen, K.-M.; Bailey, M.; Suzuki, S.; Pilcher, D.; Bellomo, R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA 2014, 311, 1308–1316. [Google Scholar] [CrossRef]
- Rhee, C.; Gohil, S.; Klompas, M. Regulatory mandates for sepsis care—reasons for caution. N. Engl. J. Med. 2014, 370, 1673–1676. [Google Scholar] [CrossRef] [Green Version]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Levy, M.M.; Evans, L.E.; Rhodes, A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018, 44, 925–928. [Google Scholar] [CrossRef] [Green Version]
- SCCM. Surviving Sepsis Campaign/Guidelines/Adult Patients. Available online: https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/Adult-Patients (accessed on 10 October 2019).
- Seymour, C.W.; Gesten, F.; Prescott, H.C.; Friedrich, M.E.; Iwashyna, T.J.; Phillips, G.S.; Lemeshow, S.; Osborn, T.; Terry, K.M.; Levy, M.M. Time to treatment and mortality during mandated emergency care for sepsis. N. Engl. J. Med. 2017, 376, 2235–2244. [Google Scholar] [CrossRef]
- Marik, P.E.; Farkas, J.D.; Spiegel, R.; Weingart, S. Rebuttal From Drs Marik, Farkas, Spiegel et al. Chest 2019, 155, 17. [Google Scholar] [CrossRef] [Green Version]
- Marik, P.E.; Farkas, J.D.; Spiegel, R.; Weingart, S.; Aberegg, S.; Beck-Esmay, J.; Carroll, S.; Kenny, J.-E.; Koyfman, A.; Lin, M. POINT: Should the Surviving Sepsis Campaign guidelines be retired? Yes. Chest 2019, 155, 12–14. [Google Scholar] [CrossRef] [Green Version]
- Mouncey, P.R.; Osborn, T.M.; Power, G.S.; Harrison, D.A.; Sadique, M.Z.; Grieve, R.D.; Jahan, R.; Harvey, S.E.; Bell, D.; Bion, J.F. Trial of early, goal-directed resuscitation for septic shock. N. Engl. J. Med. 2015, 372, 1301–1311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Investigators, P. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014, 370, 1683–1693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ko, B.S.; Kim, K.; Choi, S.-H.; Kang, G.H.; Shin, T.G.; Jo, Y.H.; Ryoo, S.M.; Beom, J.H.; Kwon, W.Y.; Han, K.S. Prognosis of patients excluded by the definition of septic shock based on their lactate levels after initial fluid resuscitation: A prospective multi-center observational study. Crit. Care 2018, 22, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, S.M.; Kim, Y.-J.; Ryoo, S.M.; Kim, W.Y. Relationship between low hemoglobin levels and mortality in patients with septic shock. Acute Crit. Care 2019, 34, 141. [Google Scholar] [CrossRef]
- Ryoo, S.M.; Han, K.S.; Ahn, S.; Shin, T.G.; Hwang, S.Y.; Chung, S.P.; Hwang, Y.J.; Park, Y.S.; Jo, Y.H.; Chang, H.L. The usefulness of C-reactive protein and procalcitonin to predict prognosis in septic shock patients: A multicenter prospective registry-based observational study. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef]
- Levy, M.M.; Rhodes, A.; Evans, L.E.; Antonelli, M.; Bailey, H.; Kesecioglu, J.; Zimmerman, J.J.; Beale, R.; De Backer, D.; Roca, R.F. COUNTERPOINT: Should the Surviving Sepsis Campaign guidelines be retired? No. Chest 2019, 155, 14–17. [Google Scholar] [CrossRef] [Green Version]
- Freund, Y.; Khoury, A.; Möckel, M.; Karamercan, M.; Dodt, C.; Leach, R.; Bloom, B.; Garcia-Castrillo, L. European Society of Emergency Medicine position paper on the 1-h sepsis bundle of the Surviving Sepsis Campaign: Expression of concern. Eur. J. Emerg. Med. 2019, 26, 232–233. [Google Scholar] [CrossRef]
- Murri, R.; Taccari, F.; Palazzolo, C.; Fantoni, M.; Cauda, R. IDSA did not endorse the Surviving Sepsis Campaign guidelines. Clin. Infect. Dis. 2018, 66, 1815–1816. [Google Scholar] [CrossRef]
- Rhee, C.; Filbin, M.; Massaro, A.F.; Bulger, A.; McEachern, D.; Tobin, K.A.; Kitch, B.; Thurlo-Walsh, B.; Kadar, A.; Koffman, A. Compliance with the national SEP-1 quality measure and association with sepsis outcomes: A multicenter retrospective cohort study. Crit. Care Med. 2018, 46, 1585. [Google Scholar] [CrossRef]
- Baghdadi, J.D.; Brook, R.H.; Uslan, D.Z.; Needleman, J.; Bell, D.S.; Cunningham, W.E.; Wong, M.D. Association of a Care Bundle for Early Sepsis Management with Mortality Among Patients With Hospital-Onset or Community-Onset Sepsis. JAMA Intern. Med. 2020, 180, 707–716. [Google Scholar] [CrossRef]
- Pepper, D.J.; Jaswal, D.; Sun, J.; Welsh, J.; Natanson, C.; Eichacker, P.Q. Evidence Underpinning the Centers for Medicare & Medicaid Services’ Severe Sepsis and Septic Shock Management Bundle (SEP-1) A Systematic Review. Ann. Intern. Med. 2018, 168, 558–568. [Google Scholar] [PubMed]
| Variables | Group 1 (<1 h) (n = 461) | Group 2 (1–3 h) (n = 637) | Group 3 (3–6 h) (n = 293) | p Value |
|---|---|---|---|---|
| Age, years | 68 (60–76) | 70 (59–78) | 71 (60–78) | 0.063 |
| Male, n (%) | 255 (55.3) | 352 (55.2) | 173 (59) | 0.514 |
| Initial vital signs | ||||
| SBP, mm Hg | 91 (77–111) | 89 (74–108) | 88 (74–107) | 0.152 |
| DBP, mm Hg | 56 (48–67) | 54 (45–64) | 54 (46–64) | 0.057 |
| Heart rate, beat per min | 111 (94–128) | 111 (93–127) | 111 (94–130) | 0.899 |
| Respiratory rate, per min | 20 (18–24) | 20 (18–22) | 20 (18–23) | 0.054 |
| Body temperature, ℃ | 38.1 (37.1–38.9) | 38 (36.9–39) | 38 (36.8–38.8) | 0.256 |
| Comorbidities, n (%) | ||||
| Hypertension | 184 (39.9) | 252 (39.5) | 103 (35.1) | 0.361 |
| Diabetes mellitus | 105 (22.7) | 180 (28.2) | 73 (24.9) | 0.114 |
| Cardiac disease | 81 (17.5) | 72 (11.3) | 33 (11.2) | 0.005 |
| COPD | 40 (8.6) | 46 (7.2) | 20 (6.8) | 0.566 |
| CKD | 33 (7.1) | 47 (7.3) | 17 (5.8) | 0.668 |
| Chronic liver disease | 57 (12.3) | 68 (10.6) | 25 (8.5) | 0.253 |
| Infection site, n (%) | ||||
| Respiratory | 123 (26.6) | 128 (20.1) | 66 (22.5) | 0.036 |
| Urinary tract | 93 (20.1) | 140 (21.9) | 51 (17.4) | 0.271 |
| Gastrointestinal tract | 48 (10.4) | 104 (16.3) | 37 (12.6) | 0.016 |
| Hepato-biliary and pancreas | 85 (18.4) | 96 (15.1) | 57 (19.4) | 0.167 |
| Others * | 20 (4.3) | 32 (5) | 18 (6.1) | 0.543 |
| Lactate, mmol/L | 2.5 (1.7–3.5) | 2.7 (1.6–4.8) | 3.2 (1.9–5) | <.0001 |
| SOFA | 6 (4–8) | 6 (4–8) | 6 (4–8) | 0.635 |
| APACHE 2 | 19 (13–25) | 19 (13–25) | 21 (15–27) | 0.021 |
| Positive blood culture, n (%) | 208 (45.1) | 289 (45.3) | 135 (46) | 0.966 |
| Outcomes, n (%) | ||||
| In-hospital mortality | 64 (13.8) | 108 (16.9) | 59 (20.1) | 0.075 |
| 28-day mortality (n = 1292) | 57 (13.2) | 98 (16.4) | 55 (20.6) | 0.037 |
| 90-day mortality (n = 1148) | 102 (26.1) | 138 (26.4) | 75 (31.7) | 0.243 |
| Variables | Unadjusted OR | 95% CI of OR | p Value | Adjusted OR | 95% CI of OR | p Value |
|---|---|---|---|---|---|---|
| Bundle achievement (2 group comparison) | ||||||
| 1-h bundle (<1 h vs. >1 h) | 0.649 | 0.481–0.877 | 0.005 | 0.74 | 0.522–1.049 | 0.091 |
| 3-h bundle (<3 h vs. >3 h) | 0.603 | 0.465–0.783 | <0.001 | 0.604 | 0.446–0.819 | 0.001 |
| 6-h bundle (<6 h vs. >6 h) | 0.511 | 0.369–0.707 | <0.001 | 0.458 | 0.312–0.672 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, B.S.; Choi, S.-H.; Shin, T.G.; Kim, K.; Jo, Y.H.; Ryoo, S.M.; Park, Y.S.; Kwon, W.Y.; Choi, H.S.; Chung, S.P.; et al. Impact of 1-Hour Bundle Achievement in Septic Shock. J. Clin. Med. 2021, 10, 527. https://doi.org/10.3390/jcm10030527
Ko BS, Choi S-H, Shin TG, Kim K, Jo YH, Ryoo SM, Park YS, Kwon WY, Choi HS, Chung SP, et al. Impact of 1-Hour Bundle Achievement in Septic Shock. Journal of Clinical Medicine. 2021; 10(3):527. https://doi.org/10.3390/jcm10030527
Chicago/Turabian StyleKo, Byuk Sung, Sung-Hyuk Choi, Tae Gun Shin, Kyuseok Kim, You Hwan Jo, Seung Mok Ryoo, Yoo Seok Park, Woon Yong Kwon, Han Sung Choi, Sung Phil Chung, and et al. 2021. "Impact of 1-Hour Bundle Achievement in Septic Shock" Journal of Clinical Medicine 10, no. 3: 527. https://doi.org/10.3390/jcm10030527
APA StyleKo, B. S., Choi, S.-H., Shin, T. G., Kim, K., Jo, Y. H., Ryoo, S. M., Park, Y. S., Kwon, W. Y., Choi, H. S., Chung, S. P., Suh, G. J., Kang, H., Lim, T. H., Son, D., & Kim, W. Y. (2021). Impact of 1-Hour Bundle Achievement in Septic Shock. Journal of Clinical Medicine, 10(3), 527. https://doi.org/10.3390/jcm10030527






