Novelties in 3D Transthoracic Echocardiography
Abstract
1. Introduction
2. Assessment of Valve Pathologies
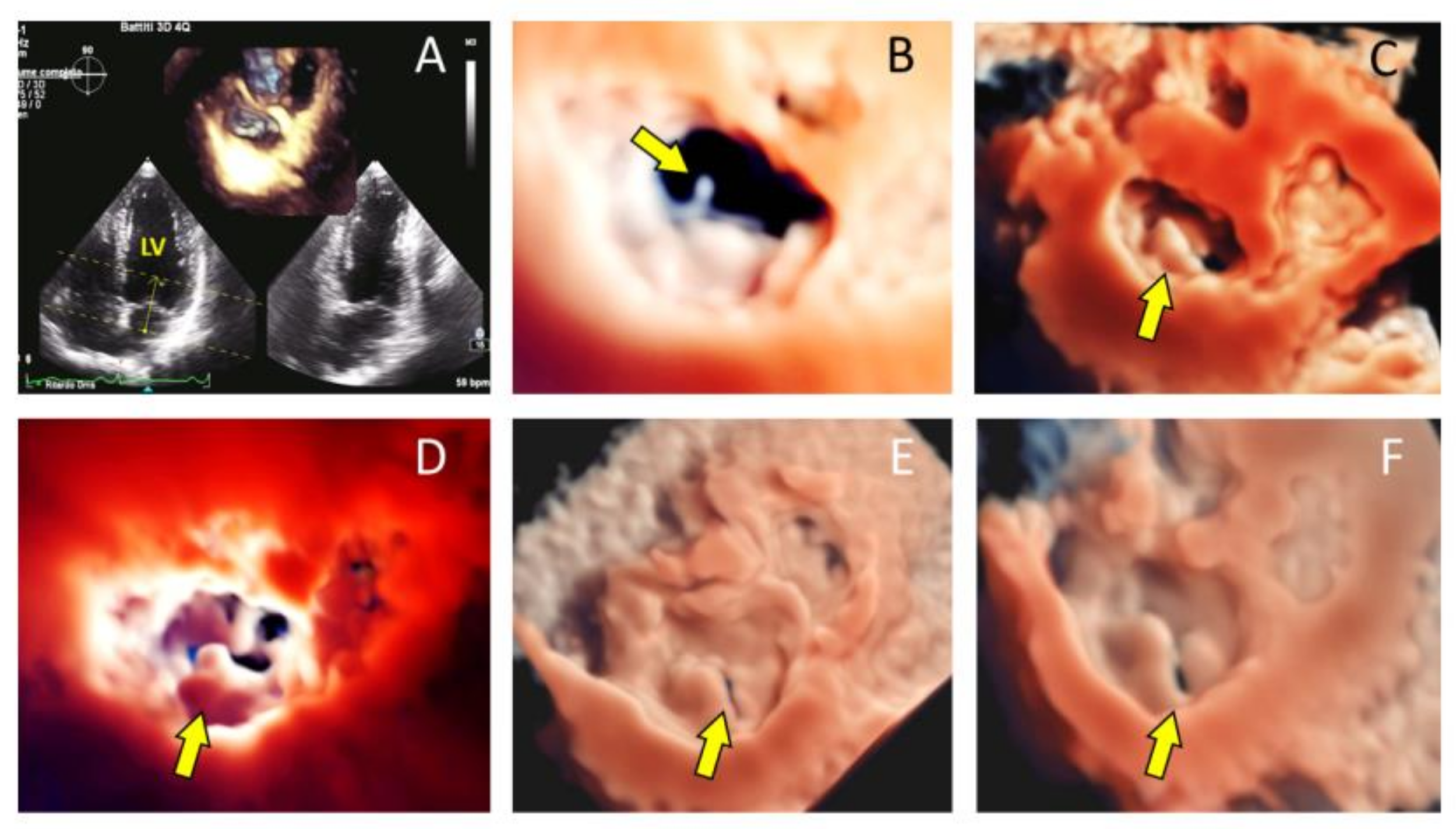
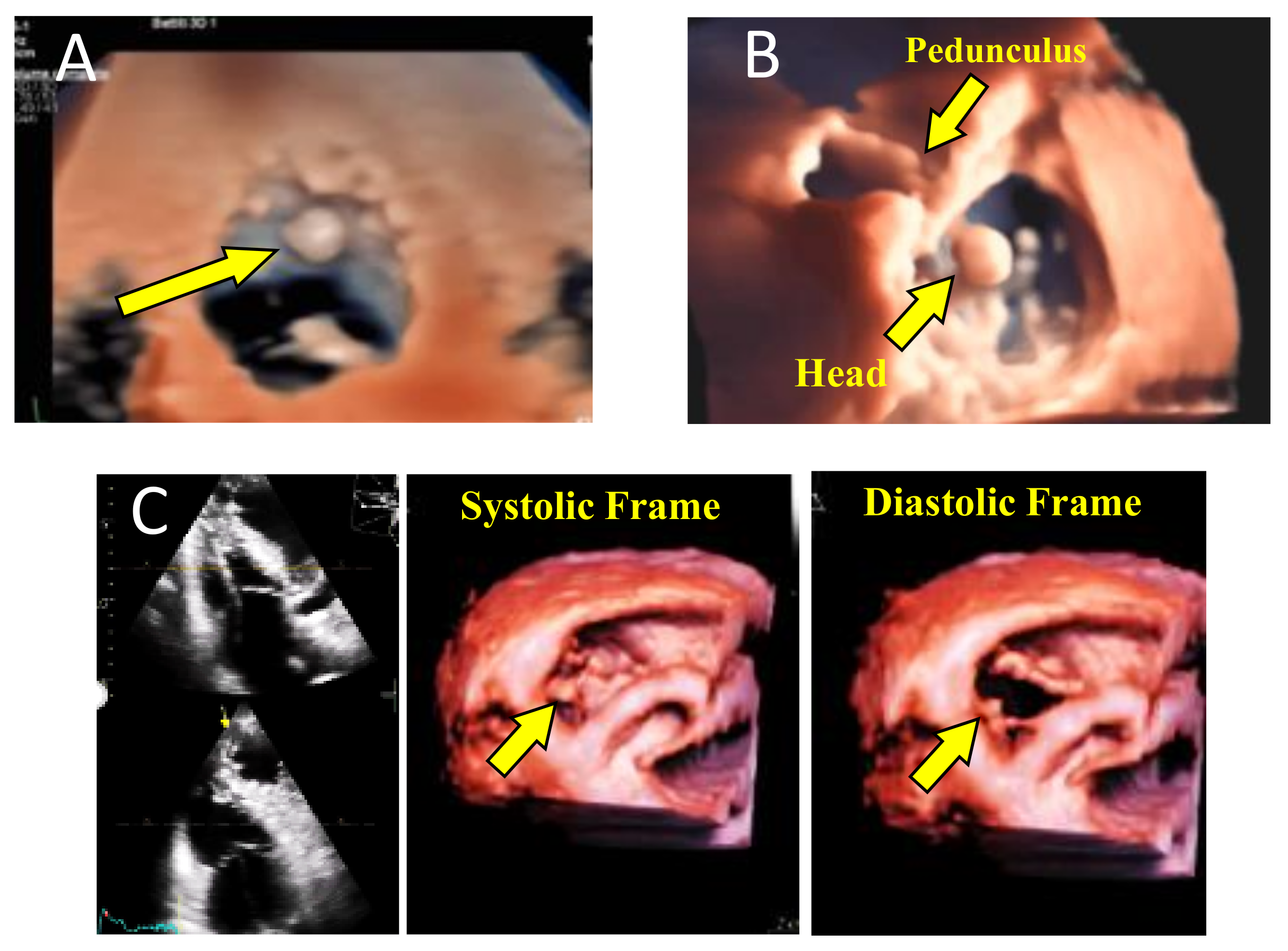
2.1. Mitral Valve
2.2. Tricuspid Valve
2.3. Aortic Valve
2.4. Grading the Severity of Valve Lesions
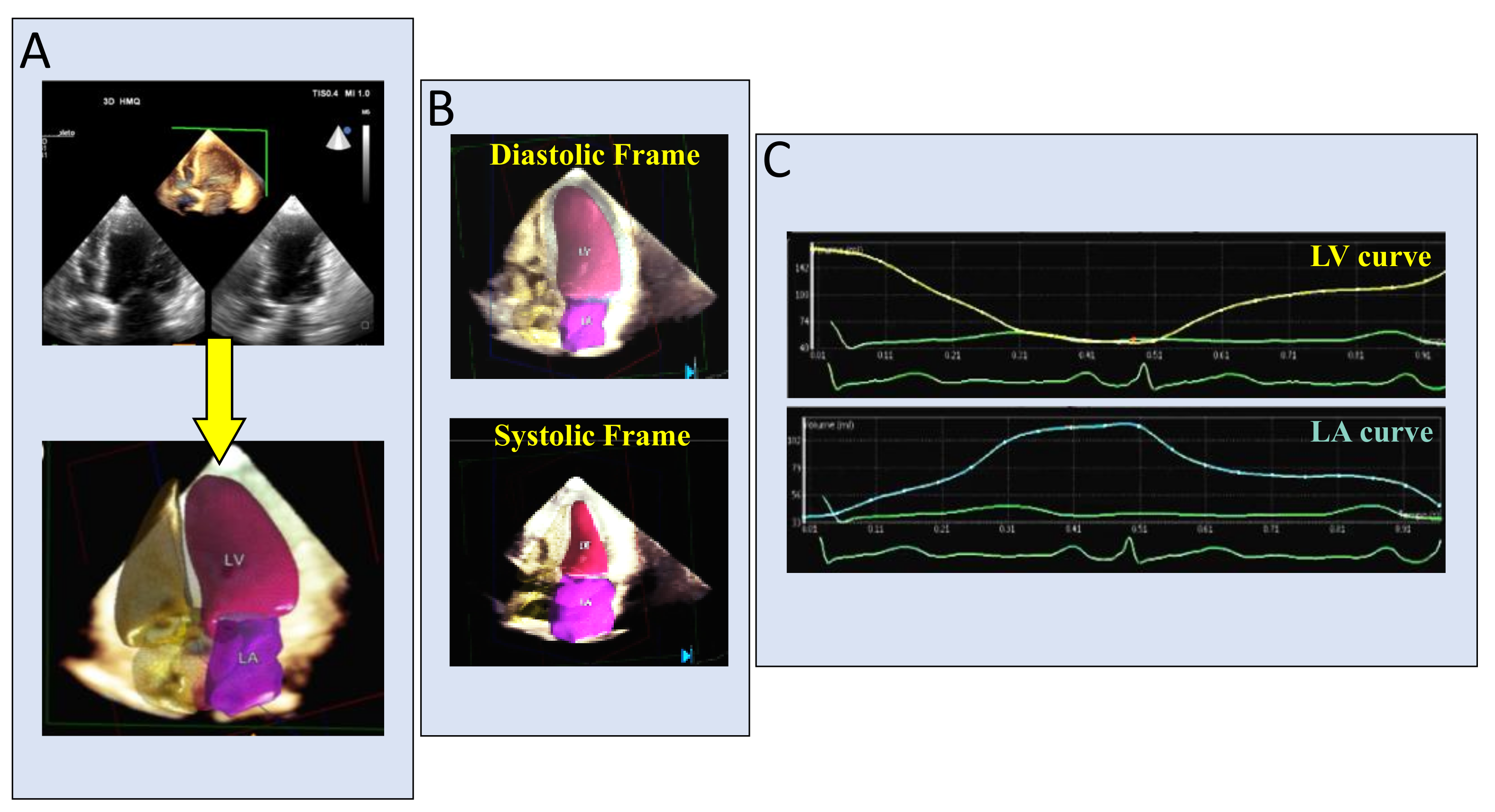
2.5. Left Ventricular Volumetric and Functional Assessment
2.6. Right Ventricular Assessment
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lang, R.M.; Badano, L.P.; Tsang, W.; Adams, D.H.; Agricola, E.; Buck, T.; Faletra, F.F.; Franke, A.; Hung, J.; Pérez de Isla, L.; et al. EAE/ASE Reccomendations for image acquisition and display using three-dimensional echocardiography. J. Am. Soc. Echocardiogr. 2012, 25, 3–46. [Google Scholar] [CrossRef] [PubMed]
- Zamorano, J.L.; Badano, L.P.; Bruce, C.; Chan, K.L.; Gonçalves, A.; Hahn, R.T.; Keane, M.G.; La Canna, G.; Monaghan, M.J.; Nihoyannopoulos, P.; et al. EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. J. Am. Soc. Echocardiogr. 2011, 24, 937–965. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Addetia, K.; Narang, A.; Mor-Avi, V. 3-Dimensional Echocardiography: Latest Developments and Future Directions. JACC Cardiovasc. Imaging 2018, 11, 1854–1878. [Google Scholar] [CrossRef] [PubMed]
- Pepi, M.; Tamborini, G.; Maltagliati, A.; Galli, C.; Sisillo, E.; Salvi, L.; Naliato, M.; Porqueddu, M.; Parolari, A.; Zanobini, M.; et al. Head-to-head comparison of two-dimensional and three-dimensional transthoracic and transesophageal echocardiography in the localization of mitral valve prolapse. J. Am. Coll. Cardiol. 2006, 48, 2524–2530. [Google Scholar] [CrossRef]
- Pepi, M.; Tamborini, G.; Pontone, G.; Andreini, D.; Berna, G.; DEVita, S.; Maltagliati, A. Initial experience with a new on-line transthoracic three-dimensional technique: Assessment of feasibility and of diagnostic potential. It. Heart. J. 2003, 4, 544–550. [Google Scholar]
- Gutiérrez-Chico, J.L.; Gómez, J.L.Z.; Rodrigo-López, J.L.; Mataix, L.; de Isla, L.P.; Carlos Almería-Valera, M.D.; Adalia Aubele, M.D.; Macaya-Miguel, C. Accuracy of real-time 3-dimensional echocardiography in the assessment of mitral prolapse. Is transesophageal echocardiography still mandatory? Am. Heart J. 2008, 155, 694–698. [Google Scholar] [CrossRef]
- Addetia, K.; Yamat, M.; Mediratta, A.; Medvedofsky, D.; Patel, M.; Ferrara, P.; Mor-Avi, V.; Lang, R.M. Comprehensive two-dimensional interrogation of the tricuspid valve using knowledge derived from three-dimensional echocardiography. J. Am. Soc. Echocardiogr. 2016, 29, 74–82. [Google Scholar] [CrossRef]
- Badano, L.P.; Agricola, E.; Perez de Isla, L.; Gianfagna, P.; Zamorano, J.L. Evaluation of the tricuspid valve morphology and function by transthoracic real-time three-dimensional echocardiography. Eur. J. Echocardiogr. 2009, 10, 477–484. [Google Scholar] [CrossRef]
- Badano, L.P.; Hahn, R.; Rodríguez-Zanella, H.; Araiza Garaygordobil, D.; Ochoa-Jimenez, R.C.; Muraru, D. Morphological Assessment of the Tricuspid Apparatus and Grading Regurgitation Severity in Patients with Functional Tricuspid Regurgitation Thinking Outside the Box. J. Am. Coll. Cardiol. Img. 2019, 12, 652–664. [Google Scholar] [CrossRef]
- Zamorano, J.; de Agustín, J.A. Three-dimensional echocardiography for assessment of mitral valve stenosis. Curr. Opin. Cardiol. 2009, 24, 415–419. [Google Scholar] [CrossRef]
- Tamborini, G.; Muratori, M.; Maltagliati, A.; Galli, C.A.; Naliato, M.; Zanobini, M.; Alamanni, F.; Salvi, L.; Sisillo, E.; Fiorentini, C.; et al. Pre-operative transthoracic real-time three-dimensional echocardiography in patients undergoing mitral valve repair: Accuracy in cases with simple vs. complex prolapse lesions. Eur. J. Echocardiogr. 2010, 11, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Gianstefani, S.; Monaghan, M.J. Accurate assessment of the true mitral valve area in rheumatic mitral stenosis. Heart 2013, 99, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., III; Guyton, R.A.; O’Gara, P.T.; Ruiz, C.E.; Skubas, N.J.; Sorajja, P.; et al. Thomas. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2438–2488. [Google Scholar] [CrossRef] [PubMed]
- Cimino, S.; Guarracino, F.; Valenti, V.; Frati, G.; Sciarretta, S.; Miraldi, F.; Agati, L.; Greco, E. Echocardiography and Correction of Mitral Regurgitation: An Unbreakable Link. Cardiology 2020, 145, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Tamborini, G.; Mantegazza, V.; Penso, M.; Muratori, M.; Fusini, L.; Ali, S.G.; Cefalù, C.; Italiano, G.; Volpato, V.; Gripari, P.; et al. Predictive Value of Pre-Operative 2D and 3D Transthoracic Echocardiography in Patients Undergoing Mitral Valve Repair: Long Term Follow Up of Mitral Valve Regurgitation Recurrence and Heart Chamber Remodeling. J. Cardiovasc. Dev. Dis. 2020, 7, 46. [Google Scholar] [CrossRef]
- Genovese, D.; Addetia, K.; Kebed, K.; Kruse, E.; Yamat, M.; Narang, A.; Patel, A.R.; Badano, L.P.; Muraru, D.; Gonçalves, A.; et al. First Clinical Experience With 3-Dimensional Echocardiographic Transillumination Rendering. JACC Cardiovasc. Imaging 2019, 12, 1868–1871. [Google Scholar] [CrossRef]
- Volpato, V.; Mantegazza, V.; Tamborini, G.; Muratori, M.; Gripari, P.; Andreini, D.; Fusini, L.; Ghulam Alù, S.; Cefalù, C.; Italiano, G.; et al. Diagnostic Accuracy of Transillumination in Mitral Valve Prolapse: Side-by-Side Comparison of Standard Transthoracic Three-Dimensional Echocardiography against Surgical Findings. J. Am. Soc. Echocardiogr. 2020, 20, 30549-6. [Google Scholar] [CrossRef]
- Caiani, E.G.; Fusini, L.; Veronesi, F.; Tamborini, G.; Maffessanti, F.; Gripari, P.; Corsi, C.; Naliato, M.; Zanobini, M.; Alamanni, F.; et al. Quantification of mitral annulus dynamic morphology in patients with mitral valve prolapse undergoing repair and annuloplasty during a 6-month follow-up. Eur. J. Echocardiogr. 2011, 12, 375–383. [Google Scholar] [CrossRef][Green Version]
- Grewal, J.; Suri, R.; Mankad, S.; Tanaka, A.; Mahoney, D.W.; Schaff, H.V.; Fletcher , A., Jr.; Sarano, M.E. Mitral annular dynamics in myxomatous valve disease: New insights with real-time 3-dimensional echocardiography. Circulation 2010, 121, 1423–1431. [Google Scholar] [CrossRef]
- Sharma, R.; Mann, J.; Drummond, L.; Livesey, S.A.; Simpson, I.A. The evaluation of real-time 3-dimensional transthoracic echocardiography for the preoperative functional assessment of patients with mitral valve prolapse: A comparison with 2-dimensional transesophageal echocardiography. J. Am. Soc. Echocardiogr. 2007, 20, 934–940. [Google Scholar] [CrossRef]
- Addetia, K.; Harb, S.C.; Hahn, R.T.; Kapadia, S.; Lang, R.M. Cardiac Implantable Electronic Device Lead-Induced Tricuspid Regurgitation. JACC Cardiovasc. Imaging 2019, 12, 622–636. [Google Scholar] [CrossRef] [PubMed]
- Volpato, V.; Lang, R.M.; Yamat, M.; Veronesi, F.; Weinert, L.; Tamborini, G.; Muratori, M.; Fusini, L.; Pepi, M.; Genovese, D.; et al. A Echocardiographic Assessment of the Tricuspid Annulus: The Effects of the Third Dimension and Measurement Methodology. J. Am. Soc. Echocardiogr. 2019, 32, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Muraru, D.; Badano, L.P.; Vannan, M.; Iliceto, S. Assessment of aortic valve complex by three-dimensional echocardiography: A framework for its effective application in clinical practice. Eur. Heart J. Cardiovasc. Imaging 2012, 13, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Tamborini, G.; Fusini, L.; Muratori, M.; Cefalù, C.; Gripari, P.; Ali, S.G.; Pontone, G.; Andreini, D.; Bartorelli, A.L.; Alamanni, F.; et al. Feasibility and accuracy of three-dimensional transthoracic echocardiography vs. multidetector computed tomography in the evaluation of aortic valve annulus in patient candidates to transcatheter aortic valve implantation. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 1316–1323. [Google Scholar] [CrossRef] [PubMed]
- Prihadi, E.A.; van Rosendael, P.J.; Vollema, E.M.; Bax, J.J.; Delgado, V.; Ajmone Marsan, N. Feasibility, accuracy, and reproducibility of aortic annular and root sizing for transcatheter aortic valve replacement using novel automated three-dimensional echocardiographic software: Comparison with multi-detector row computed tomography. J. Am. Soc. Echocardiogr. 2018, 31, 505–514.e3. [Google Scholar] [CrossRef]
- Hahn, R.T.; Pibarot, P. Accurate measurement of left ventricular outflow tract diameter: Comment on the updated recommendations for the echocardiographic assessment of aortic valve stenosis. J. Am. Soc. Echocardiogr. 2017, 30, 1038–1041. [Google Scholar] [CrossRef]
- Chacon, M.M.; Markin, N.W.; Shillcutt, S.K. 3D Geometry of the aortic valve: The future of aortic valve repair or just another measurement? J. Cardiothorac. Vasc. Anesth. 2017, 31, 1301–1303. [Google Scholar] [CrossRef]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Zamorano, J.L.; Gonçalves, A. Three dimensional echocardiography for quantification of valvular heart disease. Heart 2013, 99, 811–818. [Google Scholar] [CrossRef]
- Sotaquirá, M.; Pepi, M.; Tamborini, G.; Caiani, E.G. Anatomical Regurgitant Orifice Detection and Quantification from 3-D Echocardiographic Images. Ultrasound Med. Biol. 2017, 43, 1048–1057. [Google Scholar] [CrossRef][Green Version]
- Rosenhek, R.; Rader, F.; Klaar, U.; Gabriel, H.; Krejc, M.; Kalbeck, D.; Schemper, M.; Maurer, G.; Baumgartner, H. Outcome of watchful waiting in asymptomatic severe mitral regurgitation. Circulation 2006, 113, 2238–2244. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.H.; Kim, J.H.; Rim, J.H.; Kim, M.J.; Yun, S.C.; Song, J.M.; Song, H.; Choi, K.J.; Song, J.K.; Lee, J.W. Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation. Circulation 2009, 119, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Zilberszac, R.; Heinze, G.; Binder, T.; Laufer, G.; Gabriel, H.; Rosenhek, R. Long-term outcome of active surveillance in severe but asymptomatic primary mitral regurgitation. JACC Cardiovasc. Imaging 2018, 11, 1213–1221. [Google Scholar] [CrossRef] [PubMed]
- Vandvik, P.O.; Otto, C.M.; Siemieniuk, R.A.; Bagur, R.; Guyatt, G.H.; Lytvyn, L.; Whitlock, R.; Vartdal, T.; Brieger, D.; Aertgeerts, B.; et al. Transcatheter or surgical aortic valve replacement for patients with severe, symptomatic, aortic stenosis at low to intermediate surgical risk: A clinical practice guideline. BMJ 2016, 354, i5085. [Google Scholar] [CrossRef]
- Kang, D.H.; Park, S.J.; Rim, J.H.; Yun, S.C.; Kim, D.H.; Song, J.M.; Choo, S.J.; Park, S.W.; Song, J.K.; Lee, J.W.; et al. Early surgery versus conventional treatment in asymptomatic very severe aortic stenosis. Circulation 2010, 121, 1502–1509. [Google Scholar] [CrossRef] [PubMed]
- Lindman, B.R.; Dweck, M.R.; Lancellotti, P.; Généreux, P.; Piérard, L.A.; O’Gara, P.T.; Bonow, R.O. Management of Asymptomatic Severe Aortic Stenosis: Evolving Concepts in Timing of Valve Replacement. JACC Cardiovasc. Imaging 2020, 13, 481–493. [Google Scholar] [CrossRef] [PubMed]
- Clavel, M.A.; Pibarot, P.; Messika-Zeitoun, D.; Capoulade, R.; Malouf, J.; Aggarval, S.; Araoz, P.A.; Michelena, H.I.; Cueff, C.; Larose, E.; et al. Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: Results of an international registry study. J. Am. Coll. Cardiol. 2014, 64, 1202–1213. [Google Scholar] [CrossRef] [PubMed]
- Pawade, T.; Clavel, M.A.; Tribouilloy, C.; Dreyfus, J.; Mathieu, T.; Tastet, L.; Renard, C.; Gun, M.; Jenkins, W.S.A.; Macron, L.; et al. Computed Tomography Aortic Valve Calcium Scoring in Patients with Aortic Stenosis. Circ. Cardiovasc. Imaging 2018, 11, e007146. [Google Scholar] [CrossRef]
- Song, Y.; Lee, S.; Kwak, Y.L.; Shim, C.Y.; Chang, B.C.; Shim, J.K. Tissue Doppler imaging predicts left ventricular reverse remodeling after surgery for mitral regurgitation. Ann. Thorac. Surg. 2013, 96, 2109–2115. [Google Scholar] [CrossRef]
- Florescu, M.; Benea, D.C.; Rimbas, R.C.; Cerin, G.; Diena, M.; Lanzzillo, G.; Enescu, O.A.; Cinteza, M.; Vinereanu, D. Myocardial systolic velocities and deformation assessed by speckle tracking for early detection of left ventricular dysfunction in asymptomatic patients with severe primary mitral regurgitation. Echocardiography 2012, 29, 326–333. [Google Scholar] [CrossRef]
- Mascle, S.; Schnell, F.; Thebault, C.; Corbineau, H.; Laurent, M.; Hamonic, S.; Veillard, D.; Mabo, P.; Leguerrier, A.; Donal, E. Predictive value of global longitudinal strain in a surgical population of organic mitral regurgitation. J. Am. Soc. Echocardiogr. 2012, 25, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.A.; Lee, S.C.; Kim, E.Y.; Hahm, S.H.; Jang, S.Y.; Park, S.J.; Choi, J.O.; Park, S.W.; Choe, Y.H.; Oh, J.K. Feasibility of single-beat full-volume capture real-time three-dimensional echocardiography and auto-contouring algorithm for quantification of left ventricular volume: Validation with cardiac magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2011, 24, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Asch, F.M.; Poilvert, N.; Abraham, T.; Jankowski, M.; Cleve, J.; Adams, M.; Romano, N.; Hong, H.; Mor-Avi, V.; Martin, R.P.; et al. Automated Echocardiographic Quantification of Left Ventricular Ejection Fraction Without Volume Measurements Using a Machine Learning Algorithm Mimicking a Human Expert. Circ Cardiovasc. Imaging 2019, 12, e009303. [Google Scholar] [CrossRef] [PubMed]
- Levy, F.; Dan Schouver, E.; Iacuzio, L.; Civaia, F.; Rusek, S.; Dommerc, C.; Marechaux, S.; Dora, V.; Tribouilloy, C.; Dreyfusa, G. Performance of new automated transthoracic three-dimensional echocardiographic software for left ventricular volumes and function assessment in routine clinical practice: Comparison with 3 Tesla cardiac magnetic resonance. Arch. Cardiovasc. Dis. 2017, 110, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, L.D.; Salgo, I.S.; Goonewardena, S.; Weinert, L.; Coon, P.; Bardo, D.; Gerard, O.; Allain, P.; Zamorano, J.L.; de Isla, L.P.; et al. Rapid online quantification of left ventricular volume from real-time three-dimensional echocardiographic data. Eur. Heart J. 2006, 27, 460–468. [Google Scholar] [CrossRef]
- Tsang, W.; Salgo, I.S.; Medvedofsky, D.; Takeuchi, M.; Prater, D.; Weinert, L.; Yamat, M.; Mor-Avi, V.; Patel, A.R.; Lang, R.M. Transthoracic 3D echocardiographic left heart chamber quantification using an automated adaptive analytics algorithm. JACC. Cardiovasc. Imaging 2016, 9, 769–782. [Google Scholar] [CrossRef]
- Medvedofsky, D.; Mor-Avi, V.; Amzulescu, M.; Fernandez-Golfin, C.; Hinojar, R.; Monaghan, M.J.; Otani, K.; Reiken, J.; Takeuchi, M.; Tsang, W.; et al. Three-dimensional echocardiographic quantification of the left-heart chambers using an automated adaptive analytics algorithm: Multicenter validation study. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 47–58. [Google Scholar] [CrossRef]
- Sabharwal, N.; Cemin, R.; Rajan, K.; Hickman, M.; Lahiri, A.; Senior, R. Usefulness of left atrial volume as a predictor of mortality in patients with ischemic cardiomyopathy. Am. J. Cardiol. 2004, 94, 760–763. [Google Scholar] [CrossRef]
- Ristow, B.; Ali, S.; Whooley, M.A.; Schiller, N.B. Usefulness of left atrial volume index to predict heart failure hospitalization and mortality in ambulatory patients with coronary heart disease and comparison to left ventricular ejection fraction (from the Heart and Soul Study). Am. J. Cardiol. 2008, 102, 70–76. [Google Scholar] [CrossRef]
- Lim, T.K.; Dwivedi, G.; Hayat, S.; Majumdar, S.; Senior, R. Independent value of left atrial volume index for the prediction of mortality in patients with suspected heart failure referred from the community. Heart 2009, 95, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.I.; Shim, C.Y.; Kim, Y.J.; Kim, S.A.; Rhee, S.J.; Choi, E.Y.; Choi, D.; Jang, Y.; Chung, N.; Cho, S.Y.; et al. Left atrial volume index: A predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 2009, 22, 1338–1343. [Google Scholar] [CrossRef] [PubMed]
- Mor-Avi, V.; Yodwut, C.; Jenkins, C.; Kühl, H.; Nesser, H.J.; Marwick, T.H.; Franke, A.; Weinert, L.; Niel, J.; Steringer-Mascherbauer, R.; et al. Real-time 3D echocardiographic quantification of left atrial volume: Multicenter study for validation with CMR. JACC Cardiovasc. Imaging 2012, 5, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.A.; Lavie, C.J.; Milani, R.V.; Ventura, H.O. Left atrial volume index predictive of mortality independent of left ventricular geometry in a large clinical cohort with preserved ejection fraction. Mayo. Clin. Proc. 2011, 86, 730–737. [Google Scholar] [CrossRef]
- Tamborini, G.; Piazzese, C.; Lang, R.M.; Muratori, M.; Chiorino, E.; Mapelli, M.; Fusini, L.; Ali, S.G.; Gripari, P.; Pontone, G.; et al. Feasibility and accuracy of automated software for transthoracic three-dimensional left ventricular volume and function analysis: Comparisons with two-dimensional echocardiography, three-dimensional transthoracic manual method, and cardiac magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2017, 30, 1049–1058. [Google Scholar]
- Narang, A.; Mor-Avi, V.; Prado, A.; Volpato, V.; Prater, D.; Tamborini, G.; Fusini, L.; Pepi, M.; Goyal, N.; Addetia, K.; et al. Machine learning based automated dynamic quantification of left heart chamber volumes. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 541–549. [Google Scholar] [CrossRef]
- Mor-Avi, V.; Jenkins, C.; Kühl, H.P.; Nesser, H.J.; Marwick, T.; Franke, A.; Ebner, C.; Freed, B.H.; Steringer-Mascherbauer, R.; Pollard, H.; et al. Real-time 3-dimensional echocardiographic quantification of left ventricular volumes: Multicenter study for validation with magnetic resonance imaging and investigation of sources of error. JACC Cardiovasc. Imaging 2008, 1, 413–423. [Google Scholar] [CrossRef]
- Volpato, V.; Mor-Avi, V.; Narang, A.; Prater, D.; Gonçalves, A.; Tamborini, G.; Fusini, L.; Pepi, M.; Patel, A.R.; Lang, R.M. Automated, machine learning-based, 3D echocardiographic quantification of left ventricular mass. Echocardiography 2019, 36, 312–319. [Google Scholar] [CrossRef]
- Lang, R.; Badano, L.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.; Foster, E.; Goldstein Kuznetsova, T.; Lancellotti, P.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Nagata, Y.; Wu, V.C.; Kado, Y.; Otani, K.; Lin, F.C.; Otsuji, Y.; Negishi, K.; Takeuchi, M. Prognostic Value of Right Ventricular Ejection Fraction Assessed by Transthoracic 3D Echocardiography. Circ. Cardiovasc. Imaging 2017, 10, e005384. [Google Scholar] [CrossRef]
- Tamborini, G.; Ajmone Marsan, N.; Gripari, P.; Maffessanti, F.; Brusoni, D.; Muratori, M.; Caiani, E.; Fiorentini, C.; Pepi, M. Reference values for right ventricular volumes and ejection fraction with real-time three-dimensional echocardiography: Evaluation in a large series of normal subjects. J. Am. Soc. Echocardiogr. 2010, 23, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Gopal, A.S.; Chukwu, E.O.; Iwuchukwu, C.J.; Katz, A.S.; Toole, R.S.; Schapiro, W.; Reichek, N. Normal values of right ventricular size and function by real-time 3-dimensional echocardiography: Comparison with cardiac magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2007, 20, 445–455. [Google Scholar] [CrossRef]
- Sugeng, L.; Mor-Avi, V.; Weinert, L.; Niel, J.; Ebner, C.; Steringer-Mascherbauer, R.; Bartolles, R.; Baumann, R.; Schummers, G.; Lang, R.M.; et al. Multimodality comparison of quantitative volumetric analysis of the right ventricle. JACC Cardiovasc. Imaging 2010, 3, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Maffessanti, F.; Muraru, D.; Esposito, R.; Gripari, P.; Ermacora, D.; Santoro, C.; Tamborini, G.; Galderisi, M.; Pepi, M.; Badano, L.P. Age-, body size-, and sex-specific reference values for right ventricular volumes and ejection fraction by three-dimensional echocardiography: A multicenter echocardiographic study in 507 healthy volunteers. Circ. Cardiovasc. Imaging 2013, 6, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Tamborini, G.; Muratori, M.; Brusono, D.; Celesate, F.; Maffessanti, F.; Caiani, E.; Alamanni, F.; Pepi, M. Is right ventricular systolic function reduced after cardiac surgery? A two- and theree-dimensional echocardiographic study. Eur. J. Echocardiogr. 2009, 10, 630–634. [Google Scholar] [CrossRef]
- Tamborini, G.; Brusoni, D.; Torres Molina, J.; Galli, C.; Maltagliati, A.; Muratori, M.; Susini, F.; Colombo, C.; Maffessanti, F.; Pepi, M. Feasibility of a new generation three-dimensional echocardiography for right ventricular volumetric and functional measurements. Am. J. Cardiol. 2008, 102, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Tamborini, G.; Cefalù, C.; Celeste, F.; Fusini, L.; Garlaschè, A.; Muratori, M.; Ghulam Ali, S.; Gripari, P.; Berna, G.; Pepi, M. Multi-parametric "on board" evaluation of right ventricular function using three-dimensional echocardiography: Feasibility and comparison to traditional two-and three dimensional echocardiographic measurements. Int. J. Cardiovasc. Imaging 2019, 35, 275–284. [Google Scholar] [CrossRef]
- Fernández-Golfín, C.; Zamorano, J.L. Three-Dimensional Echocardiography and Right Ventricular Function: The Beauty and the Beast? Circ. Cardiovasc. Imaging 2017, 10, e006099. [Google Scholar] [CrossRef]
- Genovese, D.; Rashedi, N.; Weinert, L.; Narang, A.; Addetia, K.; Patel, A.R.; Prater, D.; Gonçalves, A.; Mor-Avi, V.; Lang, R.M. Machine Learning-Based Three-Dimensional Echocardiographic Quantification of Right Ventricular Size and Function: Validation Against Cardiac Magnetic Resonance. J. Am. Soc. Echocardiogr. 2019, 32, 969–977. [Google Scholar] [CrossRef]
- Tamborini, G.; Fusini, L.; Muratori, M.; Gripari, P.; Ghulam Ali, S.; Fiorentini, C.; Pepi, M. Right heart chamber geometry and tricuspid annulus morphology in patients undergoing mitral valve repair with and without tricuspid valve annuloplasty. Int. J. Cardiovasc. Imaging 2016, 32, 885–894. [Google Scholar] [CrossRef]


| 2DTTE | 2DTEE | 3DTTE (Standard) | 3DTTE (Advanced *) | 3DTEE | |
|---|---|---|---|---|---|
| Feasibility (all valves) | +++ | ++++ | +++ | ++++ | ++++ |
| Training and communication | ++ | ++ | +++ | ++++ | ++++ |
| Accuracy in MV morphology assessment vs. surgical inspection | ++ | +++ | +++ | +++ | ++++ |
| Accuracy in MV cleft and chordal rupture assessment vs. surgical inspection | ++ | +++ | ++ | +++ | ++++ |
| Accuracy in TV morphology assessment | ++ | ++ | +++ | ++++ | +++ |
| Accuracy in annulus quantification (Ao, MV and TV) | ++ | ++ | +++ | ++++ | ++++ |
| MV and TV regurgitant jet quantification | +++ | +++ | +++ | +++ | ++++ |
| Accuracy in Ao morphology assessment | ++ | ++++ | ++ | +++ | ++++ |
| Usefulness in percutaneous procedure assessment | + | +++ | ++ | ++ | ++++ |
| 2DTTE | 2DTEE | 3DTTE (Standard) | 3DTTE (Advanced *) | 3DTEE | |
|---|---|---|---|---|---|
| Feasibility of acquisition/measurements | +++ | ++ | +++ | ++++ | ++ |
| Time for acquisition/measurements | ++ | ++ | +++ | ++++ | ++ |
| Accuracy in LV volume quantification vs. MRI | ++ | ++ | +++ | ++++ | ++ |
| Accuracy in LV Ejection fraction vs. MRI | ++ | + | +++ | ++++ | + |
| Reproducibility of LV quantification | ++ | ++ | +++ | ++++ | ++ |
| Accuracy in RV volume quantification vs. MRI | + | ++ | +++ | ++++ | ++ |
| Accuracy in RV ejection fraction vs. MRI | + | + | +++ | ++++ | + |
| Reproducibility in RV quantification | + | + | +++ | ++++ | ++ |
| Accuracy in LA quantification vs. MRI | ++ | + | +++ | ++++ | ++ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Italiano, G.; Fusini, L.; Mantegazza, V.; Tamborini, G.; Muratori, M.; Ghulam Ali, S.; Penso, M.; Garlaschè, A.; Gripari, P.; Pepi, M. Novelties in 3D Transthoracic Echocardiography. J. Clin. Med. 2021, 10, 408. https://doi.org/10.3390/jcm10030408
Italiano G, Fusini L, Mantegazza V, Tamborini G, Muratori M, Ghulam Ali S, Penso M, Garlaschè A, Gripari P, Pepi M. Novelties in 3D Transthoracic Echocardiography. Journal of Clinical Medicine. 2021; 10(3):408. https://doi.org/10.3390/jcm10030408
Chicago/Turabian StyleItaliano, Gianpiero, Laura Fusini, Valentina Mantegazza, Gloria Tamborini, Manuela Muratori, Sarah Ghulam Ali, Marco Penso, Anna Garlaschè, Paola Gripari, and Mauro Pepi. 2021. "Novelties in 3D Transthoracic Echocardiography" Journal of Clinical Medicine 10, no. 3: 408. https://doi.org/10.3390/jcm10030408
APA StyleItaliano, G., Fusini, L., Mantegazza, V., Tamborini, G., Muratori, M., Ghulam Ali, S., Penso, M., Garlaschè, A., Gripari, P., & Pepi, M. (2021). Novelties in 3D Transthoracic Echocardiography. Journal of Clinical Medicine, 10(3), 408. https://doi.org/10.3390/jcm10030408







