Relationship between Endothelial Function, Antiretroviral Treatment and Cardiovascular Risk Factors in HIV Patients of African Descent in South Africa: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Inclusion/Exclusion Criteria
2.3. Ethical Approval
2.4. Data Collection
2.5. Anthropometric Measurements
2.6. Blood Pressure Measurements
2.7. Blood Collection and Biochemical Analysis
2.8. Assessment of Vascular Function
2.9. Data and Statistical Analysis
3. Results
3.1. Characteristics of Study Population
3.2. Relationship of HIV and ART with Cardiovascular Risk Factors
3.3. The Interaction between Hypertension and ART with Cardiovascular Risk Factors
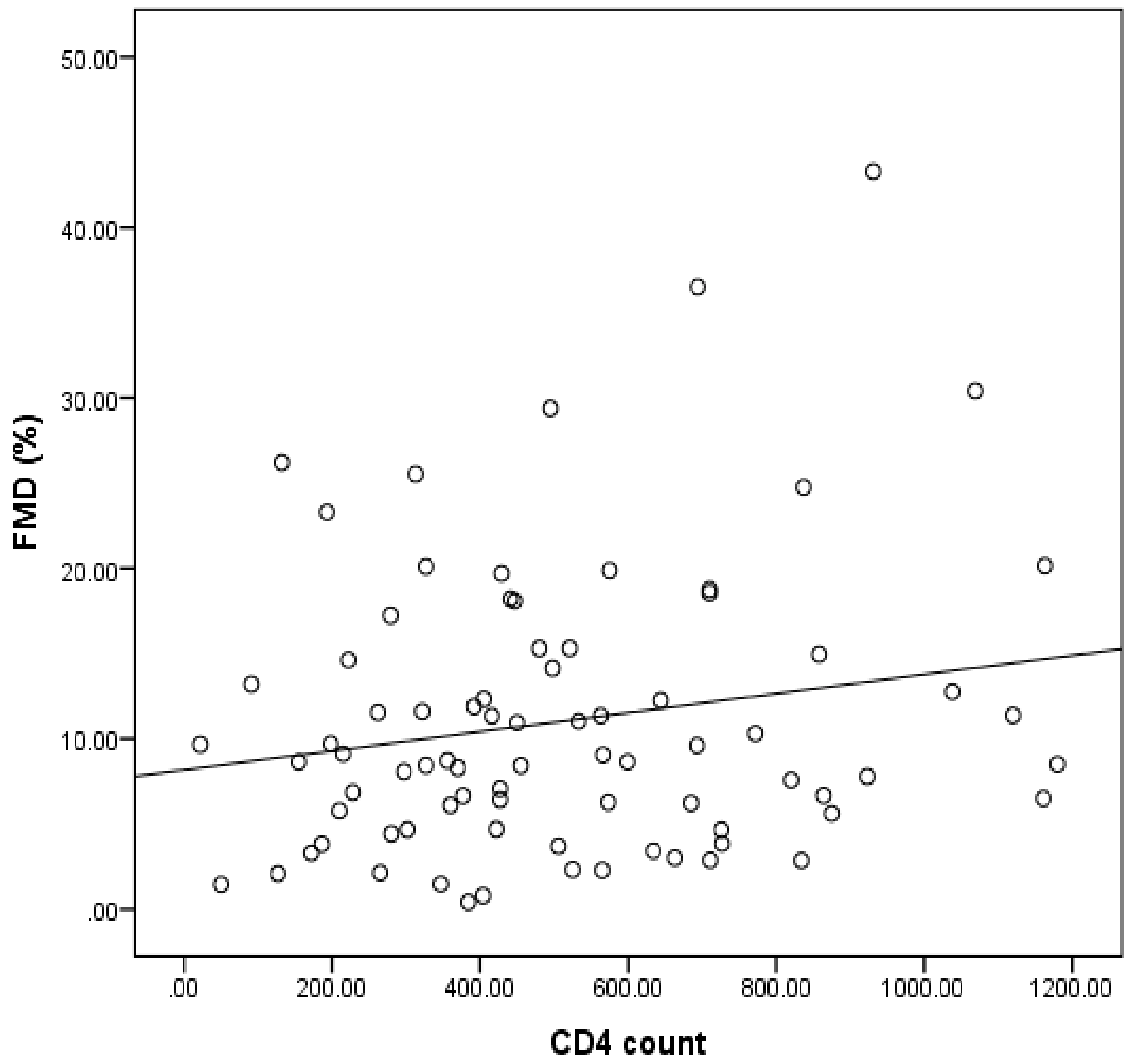
3.4. Relationship of Endothelial Function and ART With Cardiovascular Risk Factors in HIV
3.5. Relationship between ART, Endothelial Function and Cardiovascular Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Cardiovascular Diseases (CVDs); World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 11 August 2020).
- Keates, A.K.; Mocumbi, A.O.; Ntsekhe, M.; Sliwa, K.; Stewart, S. Cardiovascular disease in Africa: Epidemiological profile and challenges. Nat. Rev. Cardiol. 2017, 14, 273–293. [Google Scholar] [CrossRef]
- WHF. Factsheet: Cardiovascular Diseases in South Africa. World Heart Federation (WHF). 2017. Available online: https://www.world-heart-federation.org/wp-content/uploads/2017/05/Cardiovascular_diseases_in_South_Africa.pdf (accessed on 14 August 2020).
- Cois, A.; Day, C. Obesity trends and risk factors in the South African adult population. BMC Obes. 2015, 2, 42. [Google Scholar] [CrossRef]
- Berry, K.M.; Parker, W.; Mchiza, Z.J. Quantifying unmet need for hypertension care in South Africa through a care cascade: Evidence from the SANHANES, 2011–2012. BMJ Glob. Health 2017, 2, e00034. [Google Scholar] [CrossRef]
- Feinstein, M.J.; Hsue, P.Y.; Benjamin, L.A.; Bloomfield, G.S.; Currier, J.S.; Freiberg, M.S.; Grinspoon, S.K.; Levin, J.; Longenecker, C.T.; Post, W.S. Characteristics, prevention, and management of cardiovascular disease in people living with HIV: A scientific statement from the American Heart Association. Circulation 2019, 140, e98–e124. [Google Scholar] [CrossRef]
- Alonso, A.; Barnes, A.E.; Guest, J.L.; Shah, A.; Shao, I.Y.; Marconi, V. HIV infection and incidence of cardiovascular diseases: An analysis of a large healthcare database. J. Am. Heart Assoc. 2019, 8, e012241. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.V.; Stelzle, D.; Lee, K.K.; Beck, E.J.; Alam, S.; Clifford, S.; Longenecker, C.T.; Strachan, F.; Bagchi, S.; Whiteley, W.; et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: Systematic review and meta-analysis. Circulation 2018, 138, 1100–1112. [Google Scholar] [CrossRef] [PubMed]
- Hyle, E.P.; Bekker, L.G.; Martey, E.B. Cardiovascular risk factors among ART-experienced people with HIV in South Africa. J. Int. AIDS Soc. 2019, 22, e25274. [Google Scholar] [CrossRef]
- Bloomfield, G.S.; Hogan, J.W.; Keter, A. Hypertension and obesity as cardiovascular risk factors among HIV seropositive patients in Western Kenya. PLoS ONE 2011, 6, e22288. [Google Scholar] [CrossRef]
- Armah, K.A.; Chang, C.C.; Baker, J.V.; Veterans Aging Cohort Study (VACS) Project Team. Prehypertension, hypertension, and the risk of acute myocardial infarction in HIV-infected and-uninfected veterans. Clin. Infect. Dis. 2014, 58, 121–129. [Google Scholar] [CrossRef]
- Triant, V.A. Cardiovascular disease and HIV infection. Curr. HIV/AIDS Rep. 2013, 10, 199–206. [Google Scholar] [CrossRef]
- Strijdom, H.; Goswami, N.; De Boever, P.; Espach, Y.; Webster, I. Determinants of endothelial function in a cohort of HIV-infected and HIV-free participants: The role of cardiovascular risk factors, biomarkers of inflammation and HIV-dependent parameters. Atherosclerosis 2018, 275, E127. [Google Scholar] [CrossRef]
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Münzel, T. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 74, 1591–1619. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-H.; Park, W.J. Endothelial dysfunction: Clinical implications in cardiovascular disease and therapeutic approaches. J. Korean Med. Sci. 2015, 30, 1213–1225. [Google Scholar] [CrossRef]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef]
- Widmer, R.J.; Lerman, A. Endothelial dysfunction and cardiovascular disease. Glob. Cardiol. Sci. Pract. 2014, 2014, 291–308. [Google Scholar] [CrossRef]
- Francisci, D.; Giannini, S.; Baldelli, F. HIV type 1 infection, and not short-term HAART, induces endothelial dysfunction. AIDS 2009, 23, 589–596. [Google Scholar] [CrossRef]
- Marincowitz, C.; Genis, A.; Goswami, N.; De Boever, P.; Nawrot, T.S.; Strijdom, H. Vascular endothelial dysfunction in the wake of HIV and ART. FEBS J. 2019, 286, 1256–1270. [Google Scholar] [CrossRef]
- Monsuez, J.J.; Charniot, J.C.; Escaut, L. HIV associated vascular diseases: Structural and functional changes, clinical implications. Int. J. Cardiol. 2009, 133, 293–306. [Google Scholar] [CrossRef]
- Collaboration Antiretroviral Therapy Cohort. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: A collaborative analysis of cohort studies. Lancet HIV 2017, 4, e349–e356. [Google Scholar] [CrossRef]
- Bor, J.; Herbst, A.J.; Newell, M.-L.; Bearnighausen, T. Increases in adult life expectancy in rural South Africa: Valuing the scale-up of HIV treatment. Science 2013, 339, 961–965. [Google Scholar] [CrossRef]
- UNAIDS. Number of People Living with HIV. 2017. Available online: http://aidsinfo.unaids.org/ (accessed on 1 February 2019).
- Abrahams, Z.; Dave, J.A.; Maartens, G.; Levitt, N.S. Changes in blood pressure, glucose levels, insulin secretion and anthropometry after long term exposure to antiretroviral therapy in South African women. AIDS Res. Ther. 2015, 12, 24. [Google Scholar] [CrossRef] [PubMed]
- Laurence, J.; Elhadad, S.; Ahamed, J. HIV-associated cardiovascular disease: Importance of platelet activation and cardiac fibrosis in the setting of specific antiretroviral therapies. Open Heart 2018, 5, e000823. [Google Scholar] [CrossRef] [PubMed]
- Julius, H.; Basu, D.; Ricci, E.; Wing, J.; Basu, J.K.; Pocaterra, D. The burden of metabolic diseases amongst HIV positive patients on HAART attending The Johannesburg Hospital. Curr. HIV Res. 2011, 9, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Strijdom, H.; De Boever, P.; Nawrot, T.S.; Goswami, N. HIV/AIDS: Emerging threat to cardiovascular health in sub-Saharan Africa. SAMJ S. Afr. Med. J. 2016, 106, 537. [Google Scholar] [CrossRef]
- Strijdom, H.; De Boever, P.; Walz, G.; Essop, M.F.; Nawrot, T.S.; Webster, I.; Westcott, C.; Mashele, N.; Everson, F.; Malherbe, S.T.; et al. Cardiovascular risk and endothelial function in people living with HIV/AIDS: Design of the multi-site, longitudinal EndoAfrica study in the Western Cape Province of South Africa. BMC Infect. Dis. 2017, 17, 41. [Google Scholar] [CrossRef]
- WHO. WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Noncommunicable Disease Risk Factor Surveillance; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/ncds/surveillance/steps/STEPS_Manual.pdf?ua=1 (accessed on 27 November 2020).
- Stewart, A.; Marfell-Jones, M.; Olds, T.; Ridder, H. International Standards for Anthropometric Assessment; ISAK: Lower Hutt, New Zealand, 2011. [Google Scholar]
- WHO. Waist Circumference and Waist–Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Giles, T.D.; Materson, B.J.; Cohn, J.N.; Kostis, J.B. Definition and classification of hypertension: An update. J. Clin. Hypertens. 2009, 11, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- NICE. Chronic Kidney Disease–Early Identification and Management of Chronic Kidney Disease in Adults in Primary and Secondary Care; National Institute for Health and Clinical Excellence (NICE): London, UK, 2014. [Google Scholar]
- Islam, F.M.; Wu, J.; Jansson, J. Relative risk of cardiovascular disease among people living with HIV: A systematic review and meta-analysis. HIV Med. 2012, 13, 60–68. [Google Scholar] [CrossRef]
- Neaton, J.D. HIV and cardiovascular disease: Comment on Islam. HIV Med. 2013, 14, 517–518. [Google Scholar] [CrossRef]
- Bavinger, C.; Bendavid, E.; Niehaus, K. Risk of cardiovascular disease from antiretroviral therapy for HIV: A systematic review. PLoS ONE 2013, 8, e59551. [Google Scholar] [CrossRef]
- Choi, A.I.; Vittinghoff, E.; Deeks, S.G. Cardiovascular risks associated with abacavir and tenofovir exposure in HIV-infected persons. AIDS 2011, 25, 1289–1298. [Google Scholar] [CrossRef] [PubMed]
- Ribaudo, H.J.; Benson, C.A.; Zheng, Y. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: Short and long-term results from ACTG A5001/ALLRT. Clin. Infect. Dis. 2011, 52, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Brothers, C.H.; Hernandez, J.E.; Cutrell, A.G. Risk of myocardial infarction and abacavir therapy: No increased risk across 52 GlaxoSmithKline-sponsored clinical trials in adult subjects. J. Acquir. Immune. Defic. Syndr. 2009, 51, 20–28. [Google Scholar] [CrossRef] [PubMed]
- De Gaetano, D.K.; Rabagliati, R.; Tumbarello, M.; Tacconelli, E.; Amore, C.; Cauda, R.; Lacoviello, L. Increased soluble markers of endothelial dysfunction in HIV-positive patients under highly active antiretroviral therapy. AIDS 2003, 17, 765–768. [Google Scholar] [CrossRef] [PubMed]
- O’Halloran, J.A.; Dunne, E.; Gurwith, M.M.P.; Lambert, J.S.; Sheehan, G.J.; Feeney, E.R.; Pozniak, A.; Reiss, P.; Kenny, D.; Mallon, P.W.G. The effect of initiation of antiretroviral therapy on monocyte, endothelial and platelet function in HIV-1 infection. HIV Med. 2015, 16, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Mahlangu, K.; Modjadji, P.; Madiba, S. The nutritional status of adult antiretroviral therapy recipients with a recent HIV diagnosis; a cross-sectional study in primary health facilities in Gauteng, South Africa. Healthcare 2020, 8, 290. [Google Scholar] [CrossRef]
- Obry-Roguet, V.; Brégigeon, S.; Cano, C.E.; Lions, C.; Zaegel-Faucher, O.; Laroche, H.; Galie, S.; De Lamarlière, P.G.; Orticoni, M.; Soavi, M.J.; et al. Risk factors associated with overweight and obesity in HIV-infected people: Aging, behavioral factors but not cART in a cross-sectional study. Medicine 2018, 97, e10956. [Google Scholar] [CrossRef]
- Crum-Cianflone, N.F.; Roediger, M.; Eberly, L.E.; Vyas, K.; Landrum, M.L.; Ganesan, A.; Weintrob, A.C.; Barthel, R.V.; Agan, B.K.; Infectious Disease CLINICAL research Program HIV Working Group. Obesity among HIV-infected persons: Impact of weight on CD4 cell count. AIDS 2010, 24, 1069–1072. [Google Scholar] [CrossRef]
- Rosenblatt, L.; Farr, A.M.; Nkhoma, E.T. Risk of cardiovascular events among patients with HIV treated with atazanavir containing regimens: A retrospective cohort study. BMC Infect. Dis. 2016, 16, 492. [Google Scholar] [CrossRef]
- Desai, M.; Joyce, V.; Bendavid, E. Risk of cardiovascular events associated with current exposure to HIV antiretroviral therapies in a US veteran population. Clin. Infect. Dis. 2015, 61, 445–452. [Google Scholar] [CrossRef]
- Foulkes, A.S.; Wohl, D.A.; Frank, I.; Puleo, E.; Restine, S. Associations among race/ethnicity, apoC-III genotypes, and lipids in HIV1-infected individuals on antiretroviral therapy. PLoS Med. 2006, 3, e52. [Google Scholar] [CrossRef] [PubMed]
- Crane, H.M.; Grunfeld, C.; Willig, J.H.; Mugavero, M.J.; Van Rompaey, S.; Moore, R.; Rodriguez, B.; Feldman, B.J.; Lederman, M.M.; Saag, M.S. Impact of NRTIs on lipid levels among a large HIV-infected cohort initiating antiretroviral therapy in clinical care. AIDS 2011, 25, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Riddler, S.A.; Smit, E.; Cole, S.R. Impact of HIV infection and HAART on serum lipids in men. JAMA. 2003, 289, 2978–2982. [Google Scholar] [CrossRef] [PubMed]
- INSIGHT Start Study Group; Lundgren, J.D.; Babiker, A.G. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N. Engl. J. Med. 2015, 373, 795–807. [Google Scholar] [PubMed]
- Babiker, A.G.; Emery, S.; Fatkenheuer, G. Considerations in the rationale, design and methods of the Strategic Timing of AntiRetroviral Treatment (START) study. Clin. Trials. 2013, 10, S5–S36. [Google Scholar] [CrossRef]
- Venter, W.D.F.; Moorhouse, M.; Sokhela, S.; Fairlie, L.; Mashabane, N.; Masenya, M.; Serenata, C.; Akpomiemie, G.; Qavi, A.; Chandiwana, N.; et al. Dolutegravir plus two different prodrugs of tenofovir to treat HIV. N. Engl. J. Med. 2019, 381, 803–815. [Google Scholar] [CrossRef]
- Mineo, C.; Shaul, P.W. Novel biological functions of high-density lipoprotein cholesterol. Circ. Res. 2012, 111, 1079–1090. [Google Scholar] [CrossRef]
- Adewole, O.O.; Eze, S.; Betiku, Y.; Anteyi, E.; Wada, I.; Ajuwon, Z.; Erhabor, G. Lipid profile in HIV/AIDS patients in Nigeria. Afri. Health Sci. 2010, 10, 144–149. [Google Scholar]
- MacInnes, A.; Lazzarin, A.; Di Perri, G.; Sierra-Madero, J.G.; Aberg, J.; Heera, J.; Rajicic, N.; Goodrich, J.; Mayer, H.; Valdez, H. Maraviroc can improve lipid profiles in dyslipidemic patients with HIV: Results from the MERIT Trial. HIV Clin. Trials 2011, 12, 24–36. [Google Scholar] [CrossRef]
- Bernal, E.; Masiá, M.; Padilla, S.; Gutiérrez, F. High-Density lipoprotein cholesterol in HIV-Infected patients: Evidence for an association with HIV-1 viral load, antiretroviral therapy status, and regimen composition. AIDS Patients Care STDs 2008, 22, 569–575. [Google Scholar] [CrossRef]
- Singh, A.; Satchell, S.C. Microalbuminuria: Causes and implications. Pediatr. Nephrol. 2011, 26, 1957–1965. [Google Scholar] [CrossRef] [PubMed]
- Szczech, L.A.; Grunfeld, C.; Scherzer, R.; Canchola, J.A.; van der Horst, C.; Sidney, S.; Wohl, D.; Shlipak, M.G. Microalbuminuria in HIV infection. AIDS 2007, 21, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Hadigan, C.; Edwards, E.; Rosenberg, A.; Purdy, J.B.; Fleischman, E.; Howard, L.; Mican, J.M.; Sampath, K.; Oyalowo, A.; Johnson, A. Microalbuminuria in HIV Disease. Am. J. Nephrol. 2013, 37, 443–451. [Google Scholar] [CrossRef]
- Falasca, K.; Di Nicola, M.; Porfilio, I.; Ucceferri, C.; Schiaroli, E.; Gabrielli, C.; Francisci, D.; Vecchiet, J. Predictive factors and prevalence of microalbuminuria in HIV-infected patients: A cross-sectional analysis. BMC Nephrol. 2017, 18, 255. [Google Scholar] [CrossRef]
- Barthelmes, J.; Nägele, M.P.; Ludovici, V.; Ruschitzka, F.; Sudano, I.; Flammer, A.J. Endothelial dysfunction in cardiovascular disease and Flammer syndrome—Similarities and differences. EPMA J. 2017, 8, 99–109. [Google Scholar] [CrossRef]
- Bush, K.N.V.; Teel, J.L.; Watts, J.A. Association of endothelial dysfunction and antiretroviral therapy in early HIV infection. JAMA Netw. Open 2019, 2, e1913615. [Google Scholar] [CrossRef]
- Kamau, F.; Strijdom, H.; Nwangi, P.; Blackhurst, D.; Imperial, E.; Salie, R. Antiretroviral drug-endothelial dysfunction is improved by dual PPARα/γ stimulation in Obesity. Vasc. Pharmacol. 2019, 121, 106577. [Google Scholar] [CrossRef]
- Dysangco, A.; Liu, Z.; Stein, J.H.; DubeÂ, M.P.; Gupta, S.K. HIV infection, antiretroviral therapy, and measures of endothelial function, inflammation, metabolism, and oxidative stress. PLoS ONE 2017, 12, e0183511. [Google Scholar] [CrossRef]
- Thijssen, D.H.; Black, M.A.; Pyke, K.E.; Padilla, J.; Atkinson, G.; Harris, R.A.; Parker, B.; Widlansky, M.E.; Tschakovsky, M.E.; Green, D.J. Assessment of flow-mediated dilation in humans: A methodological and physiological guideline. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H2–H12. [Google Scholar] [CrossRef]
- Charakida, M.; De Groot, E.; Loukogeorgakis, S.P.; Khan, T.; Lüscher, T.; Kastelein, J.J.; Gasser, E.J. Variability and reproducibility of flow-mediated dilatation in a multicentre clinical trial. Eur. Heart J. 2013, 34, 3501–3507. [Google Scholar] [CrossRef]
- Ghiadoni, L.; Faita, F.; Salvetti, M.; Cordiano, C.; Biggi, A.; Puato, M.; Di Monaco, A.; De Siati, L.; Volpe, M.; Ambrosio, G. Assessment of flow-mediated dilation reproducibility: A nationwide multicenter study. J. Hypertens. 2012, 30, 1399–1405. [Google Scholar] [CrossRef]
- Greyling, A.; Van Mil, A.C.; Zock, P.L.; Green, D.J.; Ghiadoni, L.; Thijssen, D.H.; TIFN International Working Group on Flow Mediated Dilation. Adherence to guidelines strongly improves reproducibility of brachial artery flow-mediated dilation. Atherosclerosis 2016, 248, 196–202. [Google Scholar] [CrossRef]
| HIV− | HIV+ART− | HIV+ART+ | p-Value | |
|---|---|---|---|---|
| N | 171 | 163 | 146 | |
| Smoking (P/A) | 42/128 | 33/127 | 28/118 | 0.295 |
| Diabetes (P/A) | 1/170 | 1/162 | 1/145 | 0.993 |
| Age (years) | 28.9 ± 7.9 | 31.9 ± 6.9 | 34.4 ± 8.4 | <0.001 |
| Weight (kg) | 70.1 ± 15.9 | 66.9 ± 14.9 | 70.8 ± 16.8 | 0.077 |
| Height (cm) | 165.9 ± 7.9 | 163.13 ± 7.3 | 163.8 ± 9.2 | 0.006 |
| HC (cm) | 103.3 ± 13.2 | 104.4 ± 14.7 | 100.6 ± 15.2 | 0.093 |
| WC (cm) | 85.2 ± 15.7 | 88.9 ± 16.2 | 88.4 ± 16.9 | 0.091 |
| BMI (kg/m2) | 25.5 ± 6.1 | 25.1 ± 6.2 | 26.5 ± 6.9 | 0.136 |
| WHC | 0.9 ± 0.5 | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.917 |
| SBP (mmHg) | 124.6 ± 18.1 | 123.0 ± 34.9 | 121.5 ± 25.9 | 0.528 |
| DBP (mmHg) | 81.7 ± 12.5 | 78.0 ± 17.9 | 79.9 ± 19.3 | 0.132 |
| HR (bpm) | 77.3 ± 25.8 | 80.04 ± 18.8 | 65.9 ± 23.4 a,b | <0.001 |
| TC (mmol/L) | 3.9 ± 0.9 | 3.9 ± 0.9 | 4.6 ± 5.1 | 0.114 |
| HDL-c (mmol/L) | 1.3 ± 0.4 | 1.2 ± 0.4 | 1.4 ± 0.5 b | 0.004 |
| LDL-c (mmol/L) | 2.1 ± 0.9 | 2.2 ± 0.8 | 2.6 ± 0.7 | 0.557 |
| TG (mmol/L) | 1.1 ± 0.6 | 1.1 ± 0.6 | 1.3 ± 0.8 | 0.058 |
| FG (mmol/L) | 4.9 ± 0.6 | 4.9 ± 1.1 | 5.3 ± 0.9 | 0.127 |
| HBA1c (%) | 5.4 ± 0.4 | 5.4 ± 0.5 | 5.4 ± 0.4 | 0.738 |
| BC (μmol/L) | 70.2 ± 13.9 | 66.0 ± 14.2 | 67.6 ± 13.8 | 0.072 |
| UC (mmol/L) | 14.2 ± 7.9 | 14.5 ± 8.2 | 12.6 ± 5.8 | 0.163 |
| Albumin (mg/L) | 2.8 ± 8.3 | 22.4 ± 38.2 | 11.1 ± 18.5 | 0.011 |
| ACR (mg/mol) | 0.2 ± 0.7 | 1.2 ± 5.0 | 0.9 ± 1.8 | 0.062 |
| eGFR ((mL/min) | 140.8 ± 56.9 | 136.9 ± 47.6 | 129.1 ± 41.6 | 0.273 |
| CD4 count (cells/μL) | 941.2 ± 1123.7 | 425.0 ± 328.7 a | 519.9 ± 273.8 a | <0.001 |
| Viral load (1000 copies/mL) | ----- | 171.5 ± 319 | 27.8 ± 132 | 0.003 |
| FMD (%) | 12.5 ± 10.1 | 14.5 ± 10.4 | 12.2 ± 11.8 | 0.162 |
| HIV− (%) | HIV+ART− (%) | HIV+ART+ (%) | Total (%) | χ2 | p-Value | ||
|---|---|---|---|---|---|---|---|
| BP | Normal | 146 (86.4) | 142 (87.1) | 118 (81.5%) | 406 (85.1) | 0.342 | 0.843 |
| HT | 23 (13.6) | 21 (12.9) | 27 (18.5) | 71 (14.9) | |||
| WHR | Lean | 117 (68.2) | 94 (57.7) | 99 (67.8) | 310 (64.6) | 18.77 | <0.001 |
| Obese | 54 (31.8) | 69 (42.3) | 47 (32.2) | 170 (35.4) | |||
| TC | Normal | 106 (92.2) | 121(92.1) | 82 (87.2) | 309 (91.2) | 2.535 | 0.282 |
| High | 9 (7.8) | 9 (6.9) | 12 (12.8) | 30 (8.8) | |||
| HDL-c | Normal | 160 (93.0) | 147 (90.2) | 141 (96.6) | 348 (93.1) | 14.74 | 0.022 |
| Low | 12 (7.0) | 16 (9.8) | 5 (3.4) | 33 (6.9) | |||
| LDL-c | Normal | 166 (96.5) | 156 (95.7) | 142 (97.3) | 464 (96.5) | 11.69 | 0.069 |
| High | 6 (3.5) | 7 (4.3) | 4 (2.7) | 17 (3.5) | |||
| TG | Normal | 162 (94.2) | 151 (82.6) | 131 (89.7) | 444 (92.3) | 0.089 | 0.352 |
| High | 10 (5.8) | 12 (7.4) | 15 (10.3) | 37 (7.7) | |||
| AU | Normal | 170 (99.4) | 155 (95.1) | 138 (94.5) | 464 (96.5) | 7.707 | 0.021 |
| High | 1 (0.6) | 8 (4.9) | 8 (5.5) | 17 (3.5) |
| HIV− | HIV+ART− | HIV+ART+ | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Group (n) | NT (146) | HT (23) | NT (142) | HT (21) | NT (118) | HT (27) | |
| BMI (kg/m2) | 26.2 ± 6.2 | 25.4 ± 4.5 | 22.3 ± 2.8 | 23.3 ± 3.2 | 23.9 ± 4.1 | 26.3 ± 6.3 | 0.649 |
| WHC | 0.8 ± 0.1 | 0.8 ± 0.1 | 0.8 ± 0.2 | 0.7 ± 0.2 | 0.8 ± 0.1 | 0.9 ± 0.1 | 0.566 |
| TC (mmol/L) | 3.9 ± 0.9 | 3.6 ± 1.6 | 4.2 ± 1.2 | 3.9 ± 0.6 | 4.1 ± 0.9 | 12.7 ± 19.3 | 0.006 |
| HDL-c (mmol/L) | 1.3 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.4 ± 0.5 | 1.4 ± 0.3± | 1.4 ± 0.6 | 0.652 |
| LDL-c (mmol/L) | 2.1 ± 0.7 | 1.3 ± 1.7 | 2.5 ± 0.9 | 2.1 ± 0.8 | 2.1 ± 0.8 | 10.5 ± 19.5 | 0.005 |
| TG (mmol/L) | 1.0 ± 0.4 | 1.9 ± 0.9 | 1.2 ± 0.6 | 1.1 ± 0.4 | 1.2 ± 0.4 | 1.7 ± 0.8 | 0.014 |
| FBG (mmol/L) | 4.9 ± 0.6 | 4.9 ± 0.3 | 4.9 ± 0.6 | 5.1 ± 0.9 | 5.1 ± 0.5 | 5.3 ± 0.4 | 0.904 |
| HBA1c (%) | 5.3 ± 0.4 | 5.4 ± 0.4 | 5.4 ± 0.2 | 5.0 ± 0.4 | 5.6 ± 0.4 | 5.6 ± 0.4 | 0.096 |
| BC (μmol/L) | 68.6 ± 11.6 | 76.2 ± 10.0 | 73.0 ± 19.9 | 72.4 ± 10.2 | 74.0 ± 13.6 | 64.2 ± 8.8 | 0.176 |
| UC (mmol/L) | 13.8 ± 6.9 | 15.9 ± 6.5 | 15.8 ± 8.5 | 12.1 ± 6.8 | 13.5 ± 6.4 | 14.0 ± 2.8 | 0.448 |
| Albumin (mg/L) | 3.8 ± 11.7 | 7.7 ± 8.7 | 1.9 ± 2.2 | 0.9 ± 0.6 | 2.6 ± 3.3 | 8.1 ± 8.9 | 0.539 |
| ACR (mg/mmol) | 0.3 ± 0.9 | 0.5 ± 0.7 | 0.1 ± 0.2 | 0.1 ± 0.1 | 0.3 ± 0.5 | 0.6 ± 0.7 | 0.789 |
| FMD (%) | 12.6 ± 10.3 | 11.2 ± 6.7 | 13.5 ± 9.8 | 14.7 ± 9.2 | 11.4 ± 19.1 | 11.3 ± 11.7 | 0.939 |
| HIV− | HIV+ART− | HIV+ART+ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FMD (n) | 1st (41) | 2nd (38) | 3rd (38) | 4th (35) | 1st (25) | 2nd (36) | 3rd (41) | 4th (42) | 1st (37) | 2nd (37) | 3rd (31) | 4th (27) | p-Value |
| BMI (kg/m2) | 26.8 ± 6.2 | 24.9 ± 4.5 | 26.9 ± 7.1 | 26.3 ± 6.9 | 22.5 ± 3.2 | 21.6 ± 2.2 | 21.9 ± 2.9 | 23.5 ± 2.8 | 24.1 ± 3.7 | 26.4 ± 9.1 | 26.6 ± 4.3 | 23.3 ± 1.2 | 0.886 |
| WHR | 0.86 ± 0.2 | 0.79 ± 0.19 | 0.81 ± 0.2 | 0.79 ± 0.1 | 0.82 ± 0.1 | 0.86 ± 0.1 | 0.81 ± 0.3 | 0.73 ± 0.3 | 0.8 ± 0.1 | 0.91 ± 0.1 | 0.92 ± 0.1 | 0.81 ± 0.1 | 0.763 |
| TC (mmol/L) | 3.8 ± 1.2 | 3.7 ± 1.1 | 4.4 ± 0.8 | 3.8 ± 0.7 | 3.7 ± 1.1 | 4.3 ± 0.5 | 3.9 ± 1.1 | 4.7 ± 1.3 | 4.1 ± 1.0 | 16.4 ± 23.8 | 3.8 ± 1.3 | 4.8 ± 1.6 | 0.007 |
| HDL-c (mmol/L) | 1.3 ± 0.5 | 1.3 ± 0.4 | 1.3 ± 0.2 | 1.4 ± 0.5 | 1.2 ± 0.7 | 1.3 ± 0.1 | 1.1 ± 0.4 | 1.4 ± 0.3 | 1.4 ± 0.4 | 1.4 ± 0.6 | 1.5 ± 0.4 | 1.3 ± 0.3 | 0.938 |
| LDL-c (mmol/L) | 1.9 ± 0.7 | 2.0 ± 1.2 | 2.6 ± 0.7 | 1.9 ± 0.7 | 1.9 ± 0.7 | 2.5 ± 0.8 | 2.3 ± 0.9 | 2.8 ± 1.3 | 2.1 ± 0.9 | 14.1 ± 24.09 | 1.9 ± 0.9 | 3.1 ± 1.4 | 0.011 |
| TG (mmol/L) | 1.4 ± 0.6 | 1.0 ± 0.5 | 0.9 ± 0.6 | 1.0 ± 0.4 | 1.2 ± 0.6 | 1.2 ± 0.4 | 1.2 ± 0.7 | 1.1 ± 0.4 | 1.5 ± 0.7 | 1.7 ± 0.3 | 0.9 ± 0.0 | 0.9 ± 0.3 | 0.555 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nkeh-Chungag, B.N.; Goswami, N.; Engwa, G.A.; Sewani-Rusike, C.R.; Mbombela, V.; Webster, I.; De Boever, P.; Kessler, H.H.; Stelzl, E.; Strijdom, H. Relationship between Endothelial Function, Antiretroviral Treatment and Cardiovascular Risk Factors in HIV Patients of African Descent in South Africa: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 392. https://doi.org/10.3390/jcm10030392
Nkeh-Chungag BN, Goswami N, Engwa GA, Sewani-Rusike CR, Mbombela V, Webster I, De Boever P, Kessler HH, Stelzl E, Strijdom H. Relationship between Endothelial Function, Antiretroviral Treatment and Cardiovascular Risk Factors in HIV Patients of African Descent in South Africa: A Cross-Sectional Study. Journal of Clinical Medicine. 2021; 10(3):392. https://doi.org/10.3390/jcm10030392
Chicago/Turabian StyleNkeh-Chungag, Benedicta N., Nandu Goswami, Godwill A. Engwa, Constance R. Sewani-Rusike, Vuyolwethu Mbombela, Ingrid Webster, Patrick De Boever, Harald H. Kessler, Evelyn Stelzl, and Hans Strijdom. 2021. "Relationship between Endothelial Function, Antiretroviral Treatment and Cardiovascular Risk Factors in HIV Patients of African Descent in South Africa: A Cross-Sectional Study" Journal of Clinical Medicine 10, no. 3: 392. https://doi.org/10.3390/jcm10030392
APA StyleNkeh-Chungag, B. N., Goswami, N., Engwa, G. A., Sewani-Rusike, C. R., Mbombela, V., Webster, I., De Boever, P., Kessler, H. H., Stelzl, E., & Strijdom, H. (2021). Relationship between Endothelial Function, Antiretroviral Treatment and Cardiovascular Risk Factors in HIV Patients of African Descent in South Africa: A Cross-Sectional Study. Journal of Clinical Medicine, 10(3), 392. https://doi.org/10.3390/jcm10030392






