Admission Dehydration Status Portends Adverse Short-Term Mortality in Patients with Spontaneous Intracerebral Hemorrhage
Abstract
:1. Introduction
2. Materials and Methods
3. Statistics
4. Results
4.1. Patient Characteristics
4.2. Admission Dehydration Status
4.3. Multivariate Analysis
5. Discussion
6. Conclusions
7. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hemphill, J.C., 3rd; Greenberg, S.M.; Anderson, C.S.; Becker, K.; Bendok, B.R.; Cushman, M.; Fung, G.L.; Goldstein, J.N.; Macdonald, R.L.; Mitchell, P.H.; et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2015, 46, 2032–2060. [Google Scholar] [CrossRef] [Green Version]
- Schuss, P.; Bode, C.; Borger, V.; Coch, C.; Guresir, A.; Hadjiathanasiou, A.; Hamed, M.; Kuchelmeister, K.; Lehmann, F.; Muller, M.; et al. MR-Imaging and Histopathological Diagnostic Work-Up of Patients with Spontaneous Lobar Intracerebral Hemorrhage: Results of an Institutional Prospective Registry Study. Diagnostics 2021, 11, 368. [Google Scholar] [CrossRef]
- Hemphill, J.C., 3rd; Bonovich, D.C.; Besmertis, L.; Manley, G.T.; Johnston, S.C. The ICH score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001, 32, 891–897. [Google Scholar] [CrossRef] [Green Version]
- Fung, C.; Murek, M.; Z’Graggen, W.J.; Krahenbuhl, A.K.; Gautschi, O.P.; Schucht, P.; Gralla, J.; Schaller, K.; Arnold, M.; Fischer, U.; et al. Decompressive hemicraniectomy in patients with supratentorial intracerebral hemorrhage. Stroke 2012, 43, 3207–3211. [Google Scholar] [CrossRef]
- Hadjiathanasiou, A.; Schuss, P.; Ilic, I.; Borger, V.; Vatter, H.; Guresir, E. Decompressive craniectomy for intracerebral haematoma: The influence of additional haematoma evacuation. Neurosurg. Rev. 2018, 41, 649–654. [Google Scholar] [CrossRef]
- Divani, A.A.; Liu, X.; Di Napoli, M.; Lattanzi, S.; Ziai, W.; James, M.L.; Jafarli, A.; Jafari, M.; Saver, J.L.; Hemphill, J.C.; et al. Blood Pressure Variability Predicts Poor In-Hospital Outcome in Spontaneous Intracerebral Hemorrhage. Stroke 2019, 50, 2023–2029. [Google Scholar] [CrossRef] [PubMed]
- Gessler, F.; Schmitz, A.K.; Dubinski, D.; Bernstock, J.D.; Lehmann, F.; Won, S.Y.; Wittstock, M.; Guresir, E.; Hadjiathanasiou, A.; Zimmermann, J.; et al. Neurosurgical Considerations Regarding Decompressive Craniectomy for Intracerebral Hemorrhage after SARS-CoV-2-Vaccination in Vaccine Induced Thrombotic Thrombocytopenia-VITT. J. Clin. Med. 2021, 10, 2777. [Google Scholar] [CrossRef]
- Faigle, R.; Chen, B.J.; Krieger, R.; Marsh, E.B.; Alkhachroum, A.; Xiong, W.; Urrutia, V.C.; Gottesman, R.F. Novel Score for Stratifying Risk of Critical Care Needs in Patients with Intracerebral Hemorrhage. Neurology 2021, 96, e2458–e2468. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, F.; Schenk, L.M.; Ilic, I.; Putensen, C.; Hadjiathanasiou, A.; Borger, V.; Zimmermann, J.; Guresir, E.; Vatter, H.; Bode, C.; et al. Prolonged Mechanical Ventilation in Patients with Deep-Seated Intracerebral Hemorrhage: Risk Factors and Clinical Implications. J. Clin. Med. 2021, 10, 1015. [Google Scholar] [CrossRef]
- Schenk, L.M.; Schneider, M.; Bode, C.; Guresir, E.; Junghanns, C.; Müller, M.; Putensen, C.; Vatter, H.; Zimmermann, J.; Schuss, P.; et al. Early Laboratory Predictors for Necessity of Renal Replacement Therapy in Patients With Spontaneous Deep-Seated Intracerebral Hemorrhage. Front. Neurol. 2021, 12, 636711. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Volbers, B.; Sprugel, M.I.; Hoelter, P.; Engelhorn, T.; Jiang, Y.; Kuramatsu, J.B.; Huttner, H.B.; Dorfler, A.; Schwab, S.; et al. Influence of Early Enteral Nutrition on Clinical Outcomes in Neurocritical Care Patients With Intracerebral Hemorrhage. Front. Neurol. 2021, 12, 665791. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Pei, L.; Gao, Y.; Zhao, L.; Fang, H.; Bunda, B.; Fisher, L.; Wang, Y.; Li, S.; Li, Y.; et al. Dehydration Status Predicts Short-Term and Long-Term Outcomes in Patients with Cerebral Venous Thrombosis. Neurocrit. Care 2019, 30, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Lacey, J.; Corbett, J.; Forni, L.; Hooper, L.; Hughes, F.; Minto, G.; Moss, C.; Price, S.; Whyte, G.; Woodcock, T.; et al. A multidisciplinary consensus on dehydration: Definitions, diagnostic methods and clinical implications. Ann. Med. 2019, 51, 232–251. [Google Scholar] [CrossRef]
- Rowat, A.; Graham, C.; Dennis, M. Dehydration in hospital-admitted stroke patients: Detection, frequency, and association. Stroke 2012, 43, 857–859. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.H.; Lin, S.C.; Lin, J.R.; Yang, J.T.; Chang, Y.J.; Chang, C.H.; Chang, T.Y.; Huang, K.L.; Ryu, S.J.; Lee, T.H. Dehydration is an independent predictor of discharge outcome and admission cost in acute ischaemic stroke. Eur. J. Neurol. 2014, 21, 1184–1191. [Google Scholar] [CrossRef] [PubMed]
- Schrock, J.W.; Glasenapp, M.; Drogell, K. Elevated blood urea nitrogen/creatinine ratio is associated with poor outcome in patients with ischemic stroke. Clin. Neurol. Neurosurg. 2012, 114, 881–884. [Google Scholar] [CrossRef]
- Miller, H.J. Dehydration in the Older Adult. J. Gerontol. Nurs. 2015, 41, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Palevsky, P.M.; Bhagrath, R.; Greenberg, A. Hypernatremia in hospitalized patients. Ann. Intern. Med. 1996, 124, 197–203. [Google Scholar] [CrossRef]
- Warren, J.L.; Bacon, W.E.; Harris, T.; McBean, A.M.; Foley, D.J.; Phillips, C. The burden and outcomes associated with dehydration among US elderly, 1991. Am. J. Public Health 1994, 84, 1265–1269. [Google Scholar] [CrossRef] [Green Version]
- Gao, B.; Gu, H.; Yu, W.; Liu, S.; Zhou, Q.; Kang, K.; Zhang, J.; Li, Z.; Zhao, X.; Wang, Y. Admission Dehydration is Associated with Significantly Lower In-Hospital Mortality after Intracerebral Hemorrhage. Front. Neurol. 2021, 12, 637001. [Google Scholar] [CrossRef]
- Kothari, R.U.; Brott, T.; Broderick, J.P.; Barsan, W.G.; Sauerbeck, L.R.; Zuccarello, M.; Khoury, J. The ABCs of measuring intracerebral hemorrhage volumes. Stroke 1996, 27, 1304–1305. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; Hunt, B.J.; Lewis, R.R.; Swaminathan, R.; Moody, A.; Seed, P.T.; Rudd, A. Dehydration and venous thromboembolism after acute stroke. QJM 2004, 97, 293–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aasbrenn, M.; Christiansen, C.F.; Esen, B.O.; Suetta, C.; Nielsen, F.E. Mortality of older acutely admitted medical patients after early discharge from emergency departments: A nationwide cohort study. BMC Geriatr. 2021, 21, 410. [Google Scholar] [CrossRef]
- Cortes-Vicente, E.; Guisado-Alonso, D.; Delgado-Mederos, R.; Camps-Renom, P.; Prats-Sanchez, L.; Martinez-Domeno, A.; Marti-Fabregas, J. Corrigendum: Frequency, Risk Factors, and Prognosis of Dehydration in Acute Stroke. Front. Neurol. 2020, 11, 717. [Google Scholar] [CrossRef]
- Elias, S.; Hoffman, R.; Saharov, G.; Brenner, B.; Nadir, Y. Dehydration as a Possible Cause of Monthly Variation in the Incidence of Venous Thromboembolism. Clin. Appl. Thromb./Hemost. 2016, 22, 569–574. [Google Scholar] [CrossRef]
- Saadatnia, M.; Fatehi, F.; Basiri, K.; Mousavi, S.A.; Mehr, G.K. Cerebral venous sinus thrombosis risk factors. Int. J. Stroke 2009, 4, 111–123. [Google Scholar] [CrossRef]
- Paulis, S.J.C.; Everink, I.H.J.; Halfens, R.J.G.; Lohrmann, C.; Schols, J. Prevalence and Risk Factors of Dehydration among Nursing Home Residents: A Systematic Review. J. Am. Med. Dir. Assoc. 2018, 19, 646–657. [Google Scholar] [CrossRef]
- Bunn, D.; Jimoh, F.; Wilsher, S.H.; Hooper, L. Increasing fluid intake and reducing dehydration risk in older people living in long-term care: A systematic review. J. Am. Med. Dir. Assoc. 2015, 16, 101–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buoite Stella, A.; Gaio, M.; Furlanis, G.; Ridolfi, M.; Ajcevic, M.; Sartori, A.; Caruso, P.; Morrison, S.A.; Naccarato, M.; Manganotti, P. Prevalence of hypohydration and its association with stroke severity and independence outcomes in acute ischemic stroke patients. J. Clin. Neurosci. 2020, 72, 281–286. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Choi, H.A.; Samuel, S.; Park, J.H.; Jo, K.W. Elevated Blood Urea Nitrogen/Creatinine Ratio Is Associated with Venous Thromboembolism in Patients with Acute Ischemic Stroke. J. Korean Neurosurg. Soc. 2017, 60, 620–626. [Google Scholar] [CrossRef] [Green Version]
- McPherson, K.; Healy, M.J.; Flynn, F.V.; Piper, K.A.; Garcia-Webb, P. The effect of age, sex and other factors on blood chemistry in health. Clin. Chim. Acta 1978, 84, 373–397. [Google Scholar] [CrossRef]
- Qureshi, A.I. Acute hypertensive response in patients with stroke: Pathophysiology and management. Circulation 2008, 118, 176–187. [Google Scholar] [CrossRef] [Green Version]
- Frey, M.A.; Lathers, C.; Davis, J.; Fortney, S.; Charles, J.B. Cardiovascular responses to standing: Effect of hydration. J. Clin. Pharmacol. 1994, 34, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Diringer, M.N.; Scalfani, M.T.; Zazulia, A.R.; Videen, T.O.; Dhar, R. Cerebral hemodynamic and metabolic effects of equi-osmolar doses mannitol and 23.4% saline in patients with edema following large ischemic stroke. Neurocrit. Care 2011, 14, 11–17. [Google Scholar] [CrossRef] [Green Version]
- Qureshi, A.I.; Wilson, D.A.; Traystman, R.J. Treatment of elevated intracranial pressure in experimental intracerebral hemorrhage: Comparison between mannitol and hypertonic saline. Neurosurgery 1999, 44, 1055–1063; discussion 1063–1064. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Wilson, D.A.; Traystman, R.J. Treatment of transtentorial herniation unresponsive to hyperventilation using hypertonic saline in dogs: Effect on cerebral blood flow and metabolism. J. Neurosurg. Anesthesiol. 2002, 14, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Radholm, K.; Arima, H.; Lindley, R.I.; Wang, J.; Tzourio, C.; Robinson, T.; Heeley, E.; Anderson, C.S.; Chalmers, J.; Investigators, I. Older age is a strong predictor for poor outcome in intracerebral haemorrhage: The INTERACT2 study. Age Ageing 2015, 44, 422–427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortes, M.B.; Owen, J.A.; Raymond-Barker, P.; Bishop, C.; Elghenzai, S.; Oliver, S.J.; Walsh, N.P. Is this elderly patient dehydrated? Diagnostic accuracy of hydration assessment using physical signs, urine, and saliva markers. J. Am. Med. Dir. Assoc. 2015, 16, 221–228. [Google Scholar] [CrossRef] [Green Version]
- Shokoohi, H.; Berry, G.W.; Shahkolahi, M.; King, J.; King, J.; Salimian, M.; Poshtmashad, A.; Pourmand, A. The diagnostic utility of sonographic carotid flow time in determining volume responsiveness. J. Crit. Care 2017, 38, 231–235. [Google Scholar] [CrossRef]
- Bahouth, M.N.; Gottesman, R.F.; Szanton, S.L. Primary ‘dehydration’ and acute stroke: A systematic research review. J. Neurol. 2018, 265, 2167–2181. [Google Scholar] [CrossRef] [PubMed]
| Patients with Spontaneous ICH, n = 249 | |
|---|---|
| Median age (years, IQR) | 76 (65–82) |
| Female sex | 128 (51%) |
| Anticoagulation/antiplatelet medication prior ictus | 125 (50%) |
| Pre-existing hypertension | 204 (82%) |
| Pre-existing diuretic treatment | 77 (31%) |
| Initial ICH score > 3 | 48 (19%) |
| GCS ≥ 13 | 122 (49%) |
| patient age ≥ 80 years | 83 (33%) |
| infratentorial location | 37 (15%) |
| ICH volume ≥ 30 mL | 105 (42%) |
| presence of IVH | 114 (46%) |
| Presence of clinical signs of herniation at admission | 41 (17%) |
| MLS > 5 mm | 62 (25%) |
| Surgical treatment | 65 (26%) |
| Short-term mortality | 101 (41%) |
| Non-Dehydration U/Cr ≤ 80, n = 173 | Dehydration U/Cr > 80, n = 76 | ||
|---|---|---|---|
| Median age (years, IQR) | 75 (63–82) | 76 (70–82) | p < 0.001 |
| Female sex | 77 (45%) | 51 (67%) | p = 0.001, OR |
| Anticoagulation/antiplatelet medication prior ictus | 86 (50%) | 39 (51%) | p = 0.9 |
| Pre-existing hypertension | 140 (81%) | 64 (84%) | p = 0.6 |
| Pre-existing diuretic treatment | 56 (32%) | 21 (28%) | p = 0.6 |
| Supratentorial ICH location | 151 (87%) | 61 (80%) | p = 0.2 |
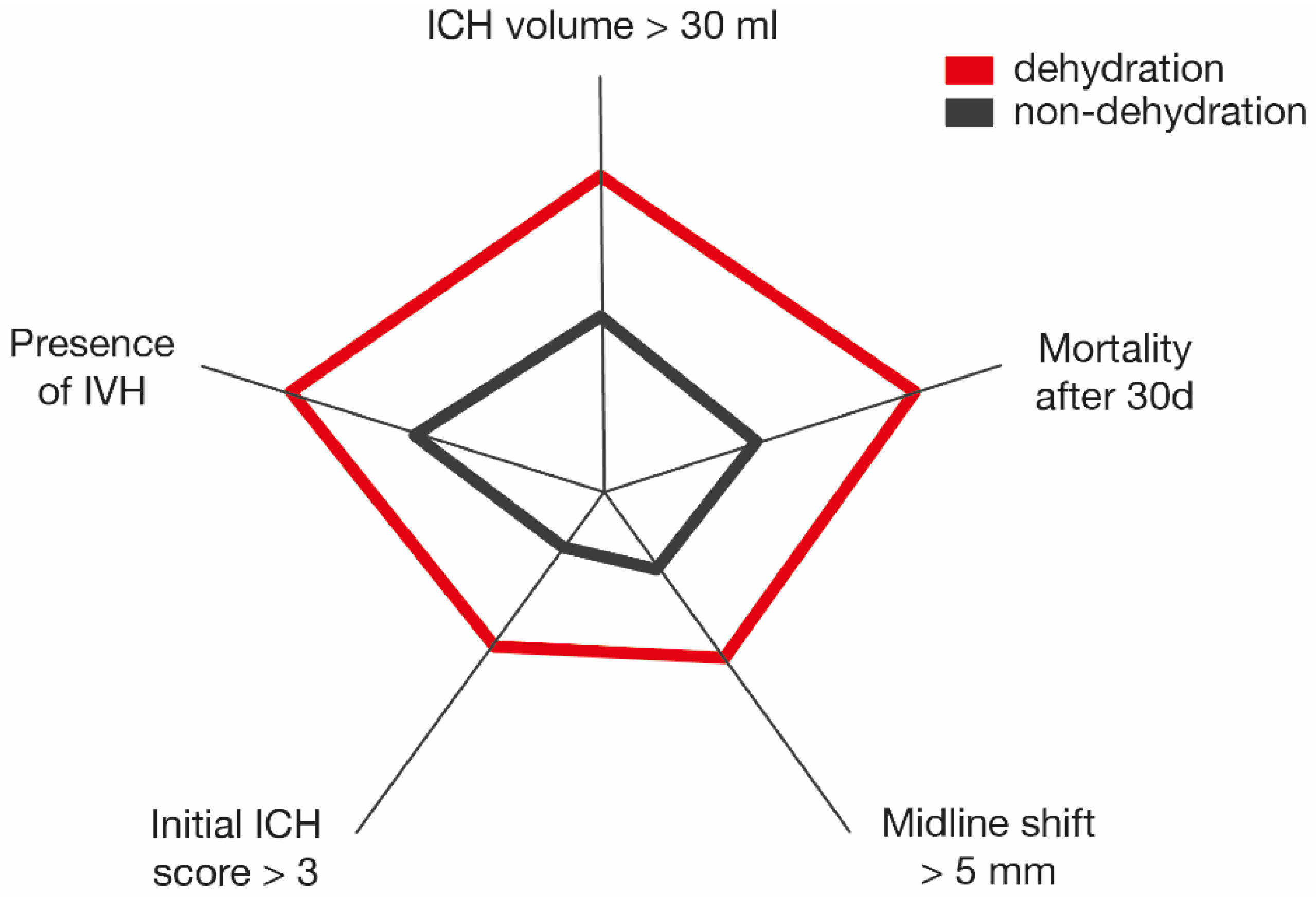
| ICH volume ≥ 30 mL | 59 (34%) | 46 (61%) | p < 0.001, OR 3.0, 95% CI 1.7–5.2 |
| Presence of IVH | 66 (38%) | 48 (63%) | p < 0.001, OR 2.8, 95% CI 1.6–4.9 |
| Initial ICH score > 3 | 21 (12%) | 27 (36%) | p < 0.001, OR 3.9, 95% CI 2.1–7.7 |
| Presence of clinical signs of herniation at admission | 21 (12%) | 20 (26%) | p = 0.009, OR 2.6, 95% CI 1.3–5.1 |
| MLS > 5 mm | 32 (18%) | 30 (39%) | p = 0.001, OR 2.9, 95% CI 1.6–5.2 |
| Short-term mortality | 53 (31%) | 48 (63%) | p < 0.001, OR 3.9, 95% CI 2.2–6.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lehmann, F.; Schenk, L.M.; Bernstock, J.D.; Bode, C.; Borger, V.; Gessler, F.; Güresir, E.; Hamed, M.; Potthoff, A.-L.; Putensen, C.; et al. Admission Dehydration Status Portends Adverse Short-Term Mortality in Patients with Spontaneous Intracerebral Hemorrhage. J. Clin. Med. 2021, 10, 5939. https://doi.org/10.3390/jcm10245939
Lehmann F, Schenk LM, Bernstock JD, Bode C, Borger V, Gessler F, Güresir E, Hamed M, Potthoff A-L, Putensen C, et al. Admission Dehydration Status Portends Adverse Short-Term Mortality in Patients with Spontaneous Intracerebral Hemorrhage. Journal of Clinical Medicine. 2021; 10(24):5939. https://doi.org/10.3390/jcm10245939
Chicago/Turabian StyleLehmann, Felix, Lorena M. Schenk, Joshua D. Bernstock, Christian Bode, Valeri Borger, Florian Gessler, Erdem Güresir, Motaz Hamed, Anna-Laura Potthoff, Christian Putensen, and et al. 2021. "Admission Dehydration Status Portends Adverse Short-Term Mortality in Patients with Spontaneous Intracerebral Hemorrhage" Journal of Clinical Medicine 10, no. 24: 5939. https://doi.org/10.3390/jcm10245939
APA StyleLehmann, F., Schenk, L. M., Bernstock, J. D., Bode, C., Borger, V., Gessler, F., Güresir, E., Hamed, M., Potthoff, A.-L., Putensen, C., Schneider, M., Zimmermann, J., Vatter, H., Schuss, P., & Hadjiathanasiou, A. (2021). Admission Dehydration Status Portends Adverse Short-Term Mortality in Patients with Spontaneous Intracerebral Hemorrhage. Journal of Clinical Medicine, 10(24), 5939. https://doi.org/10.3390/jcm10245939











