Effects of SARS-CoV-2 Pandemic on the Mental Health of Spanish Ob-Gyn Specialists—A Nationwide Study
Abstract
:1. Introduction
2. Methods
2.1. The Survey
2.2. Instruments
2.3. Population
2.4. Statistics
3. Results
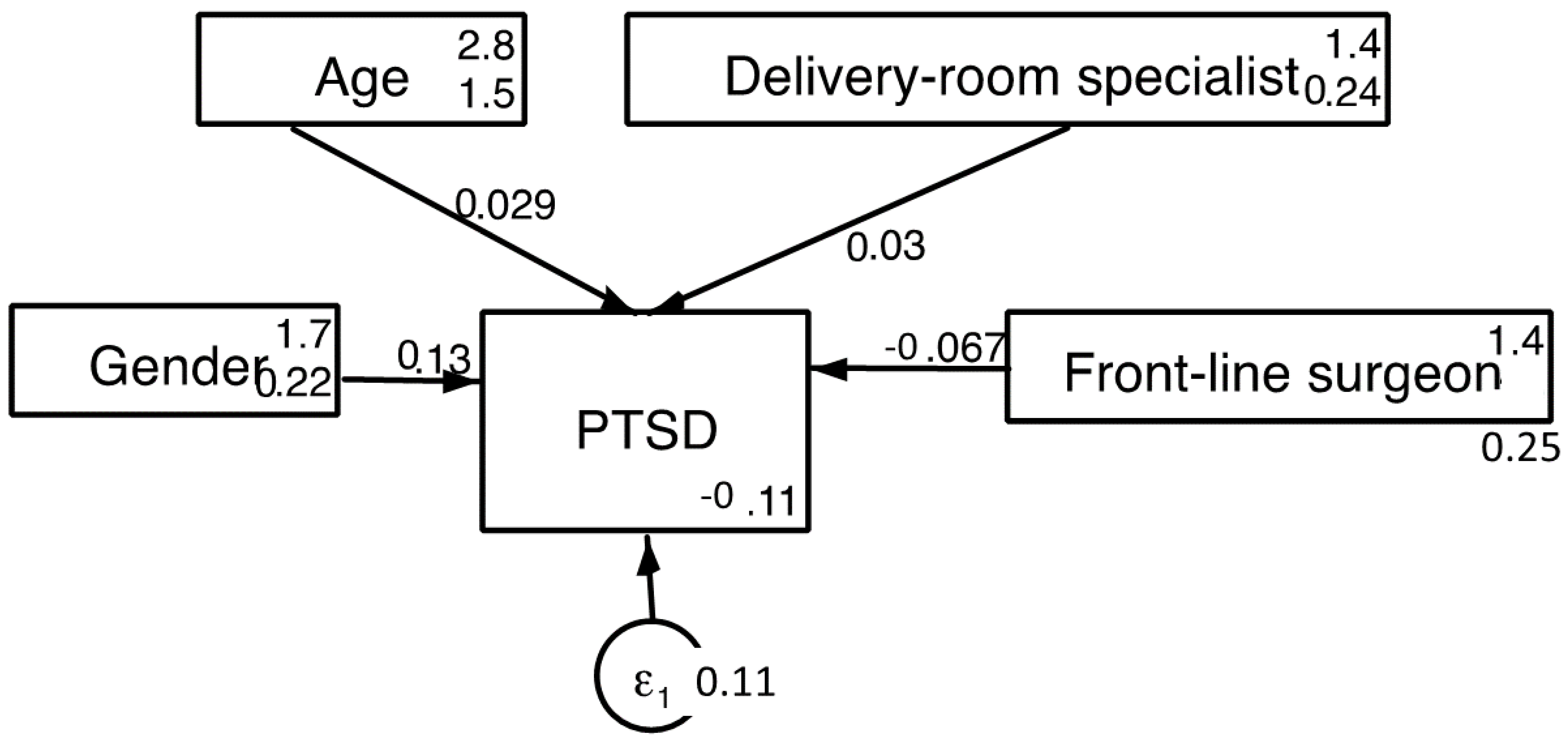
3.1. Post-Traumatic Stress Disorder (ITQ)
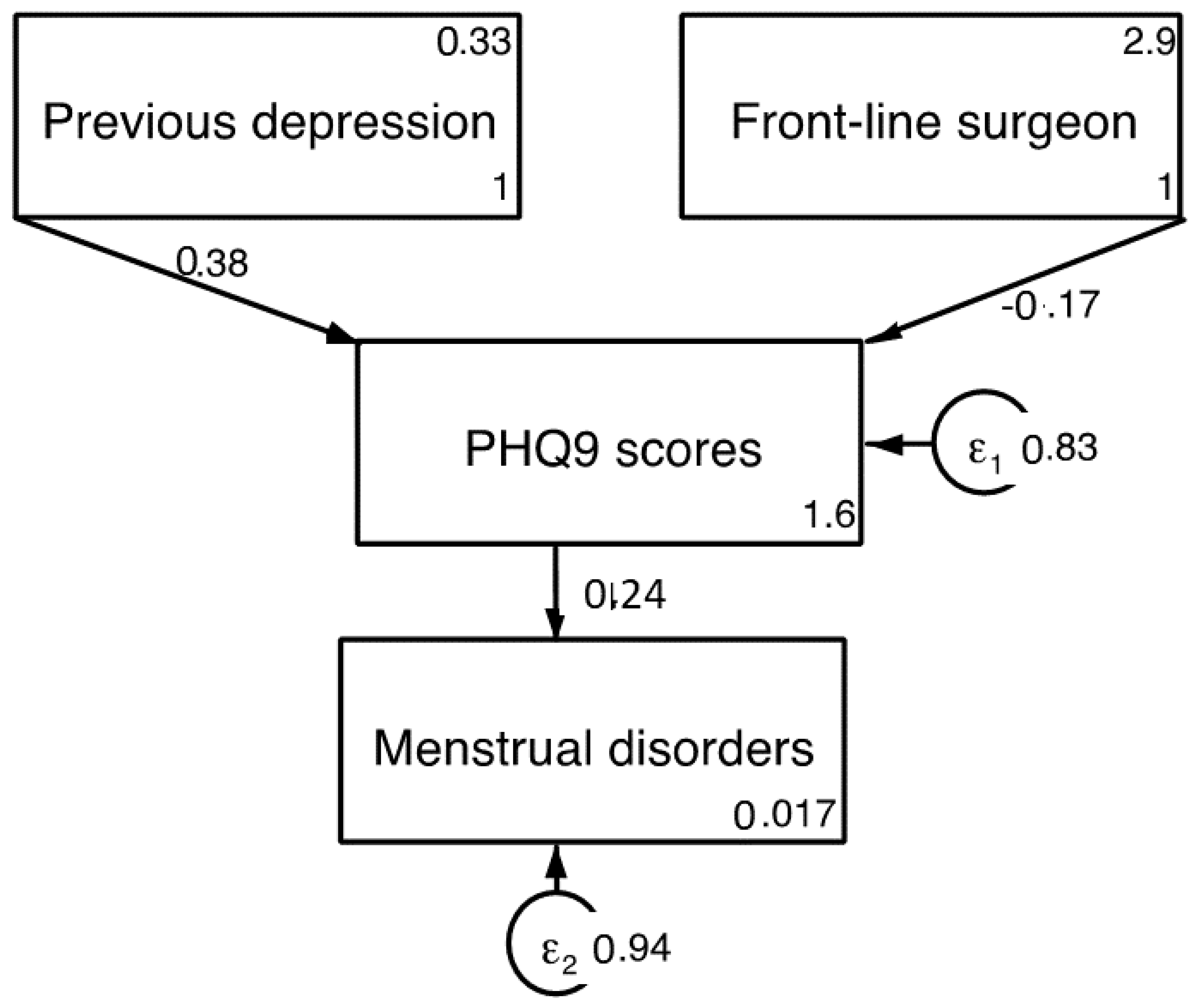
3.2. Depression (PHQ-9)
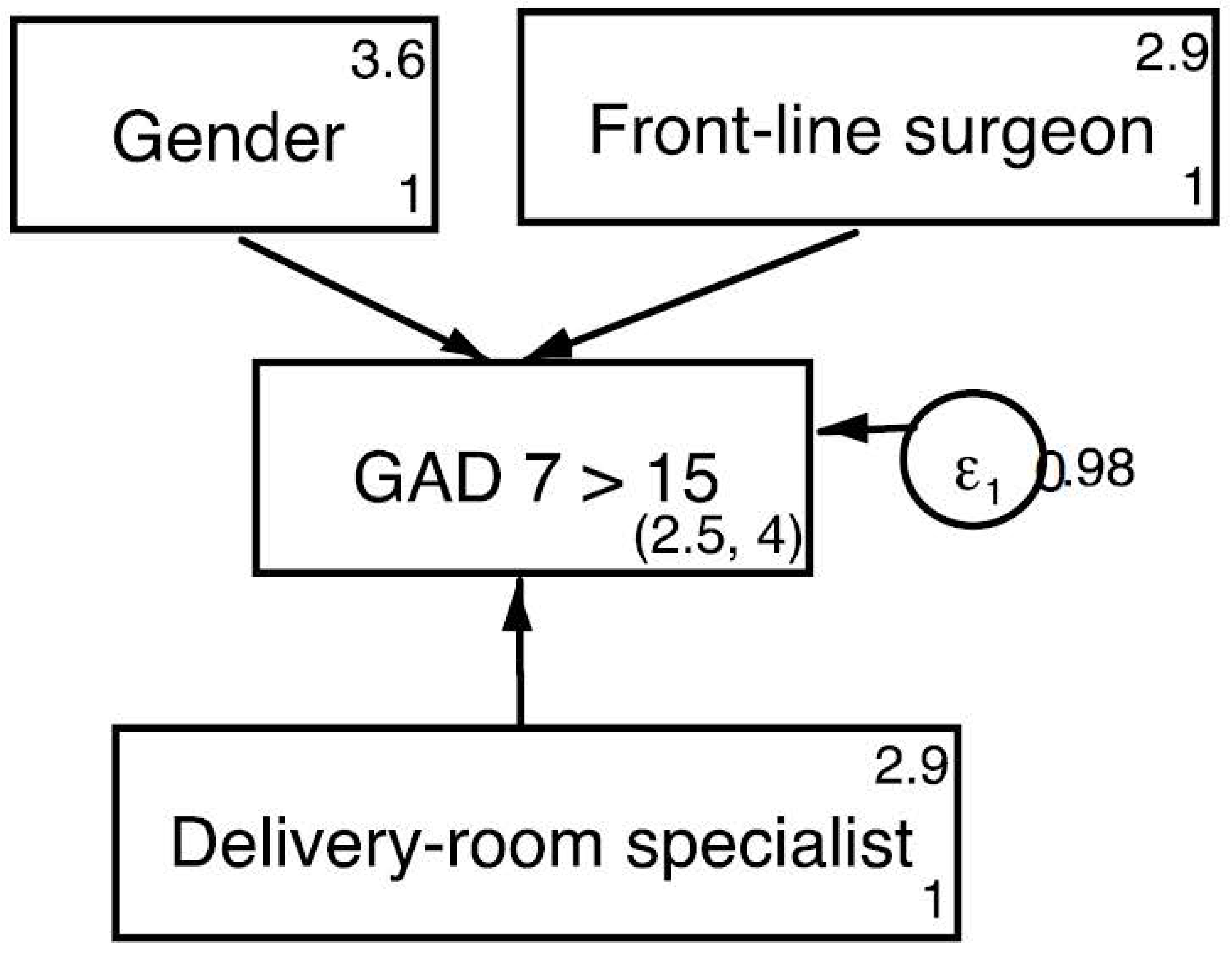
3.3. General Anxiety Disorder (GAD-7)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IHR Emergency Committee on Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed on 9 November 2021).
- Red Nacional de Vigilancia Epidemiológica. Informe No 103. Situación de COVID-19 en España; Instituto de Salud Carlos III: Madrid, Spain, 2021.
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, H.; McKenney, M.; Elkbuli, A. Protecting our healthcare workers during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 38, 1527–1528. [Google Scholar] [CrossRef]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.I.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef]
- Nam, H.S.; Yeon, M.Y.; Park, J.W.; Hong, J.Y.; Son, J.W. Healthcare worker infected with Middle East Respiratory Syndrome during cardiopulmonary resuscitation in Korea, 2015. Epidemiol. Health 2017, 39, e2017052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moazzami, B.; Razavi-Khorasani, N.; Dooghaie Moghadam, A.; Farokhi, E.; Rezaei, N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J. Clin. Virol. 2020, 126, 104345. [Google Scholar] [CrossRef]
- Martinez-Perez, O.; Prats Rodriguez, P.; Muner Hernandez, M.; Encinas Pardilla, M.B.; Perez Perez, N.; Vila Hernandez, M.R.; Villalba Yarza, A.; Nieto Velasco, O.; Del Barrio Fernandez, P.G.; Forcen Acebal, L.; et al. The association between SARS-CoV-2 infection and preterm delivery: A prospective study with a multivariable analysis. BMC Pregnancy Childbirth 2021, 21, 273. [Google Scholar] [CrossRef]
- Encinas, B.; Caño, A.; Marcos, B.; Sanz, A.; Rodríguez, I.; Hernando, P.; Fernández, A.; Martínez, O. Registro español de cribado de COVID-19 en gestantes asintomáticas. Rev. Esp. Salud Publica 2020, 94, 63. [Google Scholar]
- Carrasco, I.; Muñoz-Chapuli, M.; Vigil-Vázquez, S.; Aguilera-Alonso, D.; Hernández, C.; Sánchez-Sánchez, C.; Oliver, C.; Riaza, M.; Pareja, M.; Sanz, O.; et al. SARS-CoV-2 infection in pregnant women and newborns in a Spanish cohort (GESNEO-COVID) during the first wave. BMC Pregnancy Childbirth 2021, 21, 326. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Pérez, O.; Merino, E.; Chico-Sánchez, P.; Gras-Valentí, P.; Sánchez-Payá, J. Effectiveness of a SARS-CoV-2 infection prevention model in elective surgery patients—a prospective study: Does universal screening make sense? J. Hosp. Infect. 2021, 115, 27–31. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social. Estrategia de Vacunación COVID-19 en España. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/vacunaCovid19.htm (accessed on 9 December 2021).
- SEGO|Sociedad Española de Ginecología y Obstetricia. Available online: https://sego.es/Guias_de_Asistencia_Practica (accessed on 18 March 2021).
- Cloitre, M.; Shevlin, M.; Brewin, C.R.; Bisson, J.I.; Roberts, N.P.; Maercker, A.; Karatzias, T.; Hyland, P. The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr. Scand. 2018, 138, 536–546. [Google Scholar] [CrossRef] [Green Version]
- The International Trauma Consortium. International Trauma Questionnaire. Available online: https://www.traumameasuresglobal.com/itq (accessed on 30 October 2021).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Diez-Quevedo, C.; Rangil, T.; Sanchez-Planell, L.; Kroenke, K.; Spitzer, R.L. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom. Med. 2001, 63, 679–686. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-Campayo, J.; Zamorano, E.; Ruiz, M.A.; Pardo, A.; Pérez-Páramo, M.; López-Gómez, V.; Freire, O.; Rejas, J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcomes 2010, 8, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef]
- Bradfield, Z.; Wynter, K.; Hauck, Y.; Vasilevski, V.; Kuliukas, L.; Wilson, A.N.; Szabo, R.A.; Homer, C.S.E.; Sweet, L. Experiences of receiving and providing maternity care during the COVID-19 pandemic in Australia: A five-cohort cross-sectional comparison. PLoS ONE 2021, 16, e0248488. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social. Situación Actual Coronavirus. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm (accessed on 7 November 2021).
- Alonso, J.; Vilagut, G.; Mortier, P.; Ferrer, M.; Alayo, I.; Aragón-Peña, A.; Aragonès, E.; Campos, M.; Cura-González, I.D.; Emparanza, J.I.; et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Rev. Psiquiatr. Salud Ment. 2021, 14, 90–105. [Google Scholar] [CrossRef]
- Dosil, M.; Ozamiz-Etxebarria, N.; Redondo, I.; Picaza, M.; Jaureguizar, J. Psychological Symptoms in Health Professionals in Spain After the First Wave of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 1527–1528. [Google Scholar] [CrossRef]
- Mortier, P.; Vilagut, G.; Ferrer, M.; Serra, C.; de Dios Molina, J.; López-Fresneña, N.; Puig, T.; Pelayo-Terán, J.M.; Pijoan, J.I.; Emparanza, J.I.; et al. Thirty-day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain COVID-19 outbreak. Depress. Anxiety 2021, 38, 528–544. [Google Scholar] [CrossRef] [PubMed]
- Martín, J.; Padierna, Á.; Villanueva, A.; Quintana, J.M. Evaluation of the mental health of health professionals in the COVID-19 era. What mental health conditions are our health care workers facing in the new wave of coronavirus? Int. J. Clin. Pract. 2021, 75, e14607. [Google Scholar] [CrossRef] [PubMed]
- Dosil Santamaría, M.; Ozamiz-Etxebarria, N.; Redondo Rodríguez, I.; Jaureguizar Alboniga-Mayor, J.; Picaza Gorrotxategi, M. Impacto psicológico de la COVID-19 en una muestra de profesionales sanitarios españoles. Rev. Psiquiatr. Salud Ment. 2021, 14, 106–112. [Google Scholar] [CrossRef]
- Male, V. Menstrual changes after COVID-19 vaccination. BMJ 2021, 374, n2211. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.M.; Shilen, A.; Heslin, K.M.; Ishimwe, P.; Allen, A.M.; Jacobs, E.T.; Farland, L.V. SARS-CoV-2 infection and subsequent changes in the menstrual cycle among participants in the Arizona CoVHORT study. Am. J. Obstet. Gynecol. 2021, in press. [Google Scholar] [CrossRef]
- Edozien, L.C. Mind over matter: Psychological factors and the menstrual cycle. Curr. Opin. Obstet. Gynecol. 2006, 18, 452–456. [Google Scholar] [CrossRef]
- Khan, S.; Siddique, R.; Xiaoyan, W.; Zhang, R.; Nabi, G.; Sohail Afzal, M.; Liu, J.; Xue, M. Mental health consequences of infections by coronaviruses including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Brain Behav. 2021, 11, e01901. [Google Scholar] [CrossRef]
- Luo, Y.; Chua, C.R.; Xiong, Z.; Ho, R.C.; Ho, C.S.H. A Systematic Review of the Impact of Viral Respiratory Epidemics on Mental Health: An Implication on the Coronavirus Disease 2019 Pandemic. Front. Psychiatry 2020, 11, 1247. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, N.S.; Chung, C.H.; Chang, C.C.; Chang, H.A.; Kao, Y.C.; Chang, S.Y.; Chien, W.C. What could we learn from SARS when facing the mental health issues related to the COVID-19 outbreak? A nationwide cohort study in Taiwan. Transl. Psychiatry 2020, 10, 339. [Google Scholar] [CrossRef] [PubMed]
- Lubián López, D.M.; Butrón Hinojo, C.A.; Arjona Bernal, J.E.; Fasero Laiz, M.; Alcolea Santiago, J.; Guerra Vilches, V.; Casaus Fernández, M.; Bueno Moral, A.; Olvera Perdigones, A.; Rodríguez Rodríguez, B.; et al. Resilience and psychological distress in pregnant women during quarantine due to the COVID-19 outbreak in Spain: A multicentre cross-sectional online survey. J. Psychosom. Obstet. Gynecol. 2021, 42, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.W.; Yau, J.K.Y.; Chan, C.L.W.; Kwong, R.S.Y.; Ho, S.M.Y.; Lau, C.C.; Lau, F.L.; Lit, C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005, 12, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Chau, S.W.H.; Wong, O.W.H.; Ramakrishnan, R.; Chan, S.S.M.; Wong, E.K.Y.; Li, P.Y.T.; Raymont, V.; Elliot, K.; Rathod, S.; Delanerolle, G.; et al. History for some or lesson for all? A systematic review and meta-analysis on the immediate and long-term mental health impact of the 2002–2003 Severe Acute Respiratory Syndrome (SARS) outbreak. BMC Public Health 2021, 21, 670. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.M.; Lin, C.C.; Lin, C.Y.; Chen, J.Y.; Chue, C.M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Chua, S.E.; Cheung, V.; Cheung, C.; McAlonan, G.M.; Wong, J.W.S.; Cheung, E.P.T.; Chan, M.T.Y.; Wong, M.M.C.; Tang, S.W.; Choy, K.M.; et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can. J. Psychiatry 2004, 49, 391–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, L.; Lin, G.; Tang, L.; Yu, L.; Zhou, Z. Special attention to nurses’ protection during the COVID-19 epidemic. Crit. Care 2020, 24, 120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maunder, R. The experience of the 2003 SARS outbreak as atraumatic stress among frontline healthcare workersin Toronto: Lessons learned. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2004, 359, 117–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | n (%) |
|---|---|
| Gender | |
| Women | 150 (68.1%) |
| Men | 70 (31.9%) |
| Age | |
| 26–35 | 41 (18.9%) |
| 36–45 | 53 (24.4%) |
| 46–55 | 52 (24.0%) |
| 56–65 | 55 (25.3%) |
| Older than 65 | 16 (7.4%) |
| Region | |
| Región de Murcia | 12 (5.5%) |
| Principado de Asturias | 5 (2.3%) |
| País Vasco | 6 (2.8%) |
| La Rioja | 1 (0.5%) |
| Islas Baleares | 4 (1.8%) |
| Galicia | 10 (4.6%) |
| Extremadura | 5 (2.3%) |
| Comunidad Valenciana | 18 (8.3%) |
| Comunidad de Navarra | 2 (0.9%) |
| Comunidad de Madrid | 44 (20.3%) |
| Ceuta | 1 (0.5%) |
| Cataluña | 15 (6.9%) |
| Castilla-La Mancha | 15 (6.9%) |
| Castilla y León | 10 (4.6%) |
| Cantabria | 2 (0.9%) |
| Canarias | 6 (2.8%) |
| Aragón | 6 (2.8%) |
| Andalucía | 55 (25.3%) |
| Variable | n (%) | Variable | n (%) |
|---|---|---|---|
| Menstrual disorders * | (only pre-menopausal women) | ||
| No | 129 (89.9%) | Depression * | 193 (87.7%) |
| Before pandemic | 6 (4.6%) | No | 8 (3.6%) |
| Now | 15 (11.6%) | Before pandemic | 18 (8.1%) |
| χ2 = 4.05; p < 0.05 | Now | χ2 = 4.087; p ≥ 0.05 | |
| Diabetes Mellitus | SSRI | ||
| No | 210 (96.8%) | No | 204 (92.7%) |
| Before pandemic | 3 (1.8%) | Before pandemic | 7 (3.1%) |
| Now | 3 (1.8%) | Now | 7 (3.1%) |
| High blood pressure | Insomnia | ||
| No | 196 (90.3%) | No | 156 (71.9%) |
| Before pandemic | 15 (3.7%) | Before pandemic | 33 (15.2%) |
| Now | 17 (5.2%) | Now | 37 (17.0%) |
| Thyroid disorders | Benzodiazepines * | ||
| No | 206 (94.9%) | No | 203 (92.2%) |
| Before pandemic | 6 (2.5%) | Before pandemic | 3 (1.3%) |
| Now | 6 (2.5%) | Now | 13 (5.9%) |
|
χ2 = 10.62; p < 0.0001 | |||
| Anxiety * | Sleeping pills | ||
| No | No | 191 (86.8%) | |
| Before pandemic | 187 (85.0%) | Before pandemic | 13 (5.9%) |
| Now | 6 (2.7%) | Now | 16 (7.2%) |
| 30 (13.6%) | |||
| χ2 = 16.42; p < 0.0001 | |||
| Phobias | |||
| No | 205 (93.1%) | ||
| Before pandemic | 4 (1.8%) | ||
| Now | 9 (4.1%) |
| Overall | Women | Men | |
|---|---|---|---|
| Infected by SARS-CoV-2 | |||
| Yes | 54 (24.9%) | 35 (23.5%) | 19 (28.4%) |
| No | 162 (74.7%) | 114 (76.5%) | 48 (71.6%) |
| COVID-19 severity | |||
| Asymptomatic | 7 (2.8%) | 3 (8.5%) | 4 (21.0%) |
| Mild | 35 (16.1%) | 23 (65.5%) | 12 (63.1%) |
| Pneumonia | 9 (4.1%) | 7 (20.0%) | 2 (10.5%) |
| Intensive Care | 3 (1.4%) | 2 (5.7%) | 1 (5.2%) |
| Severely ill/deceased relatives | |||
| Yes | 49 (24.9%) | 31 (20.81%) | 18 (26.9%) |
| No | 167 (74.7%) | 118 (79.2%) | 49 (73.1%) |
| Frontline workers | |||
| Yes | 181 (83.4%) | 127 (85.8%) | 54 (80.6%) |
| No | 34 (15.7%) | 21 (14.2%) | 13 (19.4%) |
| Treated COVID-19 patients | |||
| Birth/Delivery room * | 130 (59.9%) | 97 (65.5%) | 33 (49.3%) |
| Chi Sq 5.11; p < 0.05 | |||
| Surgical areas | 120 (55.3%) | 88 (59.5%) | 32 (47.8%) |
| Consultations | 170 (78.3%) | 121 (81.8%) | 49 (73.1%) |
| Non-Ob-Gyn areas | 57 (26.3%) | 40 (27%) | 17 (25.4%) |
| Needed Personal Protective Equipment * | |||
| Yes | |||
| No | 142 (79.3%) | 125 (84.5%) | 47 (70.1%) |
| Chi Sq 5.093; p < 0.005 | 43 (19.8%) | 23 (15.5%) | 20 (29.9%) |
| Vaccinated against SARS-CoV-2 | |||
| Yes | 217 (99%) | 147 (99.3%) | 65 (97%) |
| No | 3 (1%) | 1 (0.7%) | 2 (3%) |
| Sick leave or quarantined | |||
| Yes | 66 (30.4%) | 52 (35.1%) | 14 (20.9%) |
| No | 149 (68.7%) | 96 (64.9%) | 53 (79.1%) |
| Chi Sq 4.39; p < 0.005 |
| ITQ | GAD-7 | PHQ9 | |
|---|---|---|---|
| Mean | 5.26 | 8.46 | 8.86 |
| Median | 4 | 8 | 8 |
| Std. Deviation | 5.129 | 6.155 | 7.069 |
| Percentiles 25th | 1 | 3 | 3 |
| 50th | 4 | 8 | 8 |
| 75th | 8 | 13 | 14 |
| Pearson’s r | |||
| ITQ | 1 | 0.63 * | 0.61 * |
| GAD-7 | 0.63 * | 1 | 0.84 * |
| PHQ-9 | 0.61 * | 0.84 * | 1 |
| Unstandardized B | Std. Error | Beta Coefficient | t-Value | p | |
|---|---|---|---|---|---|
| (Constant) | 11.52 | 1.357 | 8.49 | 0.00 | |
| Frontline surgical | −2.44 | 0.88 | −0.172 | −2.75 | 0.00 |
| Previous depression | 4.66 | 0.74 | 0.381 | 6.10 | 0.00 |
| Unstandardized B | Std. Error | Beta Coefficient | t-Value | Sig. | |
|---|---|---|---|---|---|
| (Constant) | 6.058 | 2.018 | 8.97 | 0.00 | |
| Frontline surgical | −1.92 | 0.812 | −0.15 | −2.36 | 0.01 |
| Gender | 3.11 | 0.871 | 0.23 | 3.57 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Mesa, E.; Jiménez-López, J.S.; Blasco-Alonso, M.; Anderica-Herrero, J.R.; Lubián-López, D. Effects of SARS-CoV-2 Pandemic on the Mental Health of Spanish Ob-Gyn Specialists—A Nationwide Study. J. Clin. Med. 2021, 10, 5899. https://doi.org/10.3390/jcm10245899
González-Mesa E, Jiménez-López JS, Blasco-Alonso M, Anderica-Herrero JR, Lubián-López D. Effects of SARS-CoV-2 Pandemic on the Mental Health of Spanish Ob-Gyn Specialists—A Nationwide Study. Journal of Clinical Medicine. 2021; 10(24):5899. https://doi.org/10.3390/jcm10245899
Chicago/Turabian StyleGonzález-Mesa, Ernesto, Jesus Salvador Jiménez-López, Marta Blasco-Alonso, Jose Ramon Anderica-Herrero, and Daniel Lubián-López. 2021. "Effects of SARS-CoV-2 Pandemic on the Mental Health of Spanish Ob-Gyn Specialists—A Nationwide Study" Journal of Clinical Medicine 10, no. 24: 5899. https://doi.org/10.3390/jcm10245899
APA StyleGonzález-Mesa, E., Jiménez-López, J. S., Blasco-Alonso, M., Anderica-Herrero, J. R., & Lubián-López, D. (2021). Effects of SARS-CoV-2 Pandemic on the Mental Health of Spanish Ob-Gyn Specialists—A Nationwide Study. Journal of Clinical Medicine, 10(24), 5899. https://doi.org/10.3390/jcm10245899









