Internet-Delivered Acceptance and Commitment Therapy Added to Multimodal Pain Rehabilitation: A Cluster Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Recruitment and Participants
2.3. Randomization
2.4. Procedure
2.5. Interventions
2.5.1. MMRP
2.5.2. MMRP-IACT
2.6. Outcome Measures
2.6.1. The Chronic Pain Acceptance Questionnaire (CPAQ)
2.6.2. Psychological Inflexibility in Pain Scale (PIPS)
2.6.3. Pain Self-Efficacy Questionnaire (PSEQ)
2.6.4. Multidimensional Pain Inventory (MPI)
2.7. Statistical Analyses
3. Results
3.1. Pain Acceptance
3.2. Psychological Inflexibility
3.3. Affective Distress
3.4. Pain Self-Efficacy
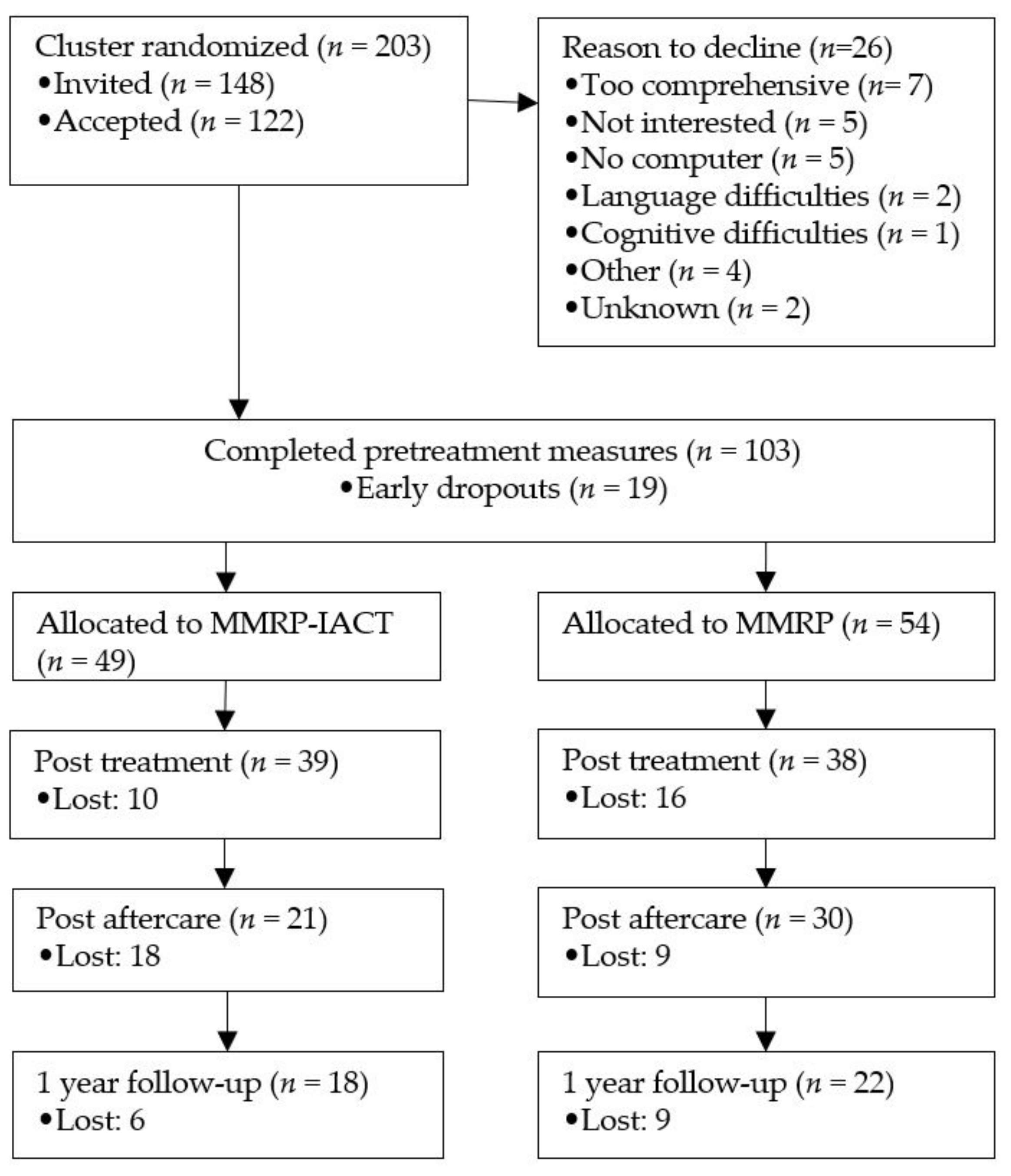
3.5. Attrition
3.6. Delivery of Intervention
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
5. Conclusions and Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287–333. [Google Scholar] [CrossRef]
- Turk, D.C.; Okifuji, A. Psychological factors in chronic pain: Evolution and revolution. J. Consult. Clin. Psychol. 2002, 70, 678–690. [Google Scholar] [CrossRef]
- Gerdle, B.; Molander, P.; Stenberg, G.; Stålnacke, B.M.; Enthoven, P. Weak outcome predictors of multimodal rehabilitation at one-year follow-up in patients with chronic pain—A practice based evidence study from two SQRP centres. BMC Musculoskelet. Disord. 2016, 17, 490. [Google Scholar] [CrossRef] [Green Version]
- Turk, D.C.; Rudy, T.E. Neglected topics in the treatment of chronic pain patients—Relapse, noncompliance, and adherence enhancement. Pain 1991, 44, 5–28. [Google Scholar] [CrossRef]
- Naylor, M.R.; Keefe, F.J.; Brigidi, B.; Naud, S.; Helzer, J.E. Therapeutic Interactive Voice Response for chronic pain reduction and relapse prevention. Pain 2008, 134, 335–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kloek, C.; Bossen, D.; Bakker, D.H.D.; Veenhof, C.; Dekker, J. Blended interventions to change behavior in patients with Chronic somatic disorders: Systematic review. J. Med. Internet Res. 2017, 19, e418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feliu-Soler, A.; Montesinos, F.; Gutiérrez-Martínez, O.; Scott, W.; McCracken, L.M.; Luciano, J.V. Current status of acceptance and commitment therapy for chronic pain: A narrative review. J. Pain Res. 2018, 11, 2145–2159. [Google Scholar] [CrossRef] [Green Version]
- De Boer, M.J.; Versteegen, G.J.; Vermeulen, K.M.; Sanderman, R.; Struys, M.M.R.F. A randomized controlled trial of an Internet-based cognitive-behavioural intervention for non-specific chronic pain: An effectiveness and cost-effectiveness study. Eur. J. Pain 2014, 18, 1440–1451. [Google Scholar] [CrossRef] [Green Version]
- Buhrman, M.; Gordh, T.; Andersson, G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016, 4, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Bendelin, N.; Gerdle, B.; Andersson, G. Internet-delivered aftercare following multimodal rehabilitation program for chronic pain: A qualitative feasibility study. J. Pain Res. 2018, 11, 1715–1728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, G.; Titov, N.; Dear, B.F.; Rozental, A.; Carlbring, P. Internet-delivered psychological treatments: From innovation to implementation. World Psychiatry 2019, 18, 20–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and Commitment Therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [Green Version]
- APA Task Force 12. Treatment: Acceptance and Commitment Therapy for Chronic Pain. 2016. Available online: https://www.div12.org/treatment/acceptance-and-commitment-therapy-for-chronic-pain/ (accessed on 1 June 2021).
- Vugts, M.A.P.; Joosen, M.C.W.; van der Geer, J.E.; Zedlitz, A.M.E.E.; Vrijhoef, H.J.M. The effectiveness of various computer-based interventions for patients with chronic pain or functional somatic syndromes: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0196467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sullivan, M.; Langford, D.J.; Davies, P.S.; Tran, C.; Vilardaga, R.; Cheung, G.; Yoo, D.; McReynolds, J.; Lober, W.B.; Tauben, D.; et al. A Controlled Pilot Trial of PainTracker Self-Manager, a Web-Based Platform Combined with Patient Coaching, to Support Patients’ Self-Management of Chronic Pain. J. Pain 2018, 19, 996–1005. [Google Scholar] [CrossRef] [PubMed]
- Dear, B.F.; Courtney, C.; Khor, K.E.; McDonald, S.; Ricciardi, T.; Gandy, M.; Fogliati, V.J.; Titov, N. The Pain Course: Exploring the Feasibility of an Internet-delivered Pain Management Program When Offered by a Tertiary Pain Management Service. Clin. J. Pain 2018, 34, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Rickardsson, J.; Gentili, C.; Holmström, L.; Zetterqvist, V.; Andersson, E.; Persson, J.; Lekander, M.; Ljótsson, B.; Wicksell, R.K. Internet-delivered acceptance and commitment therapy as microlearning for chronic pain: A randomized controlled trial with 1-year follow-up. Eur. J. Pain 2021, 25, 1012–1030. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.Y.; Moss-Morris, R.; McCracken, L.M. IACT-CEL: A Feasibility Trial of a Face-to-Face and Internet-Based Acceptance and Commitment Therapy Intervention for Chronic Pain in Singapore. Pain Res. Treat. 2017, 2017, 6916915. [Google Scholar] [CrossRef] [PubMed]
- Kelders, S.M.; Kok, R.N.; Ossebaard, H.C.; Van Gemert-Pijnen, J.E.W.C. Persuasive system design does matter: A systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012, 14, e152. [Google Scholar] [CrossRef]
- Carr, J.L.; Klaber Moffett, J.A. Review Paper: The impact of social deprivation on chronic back pain outcomes. Chronic Illn. 2005, 1, 121–129. [Google Scholar] [CrossRef]
- Johansson, C.; Dahl, J.; Jannert, M.; Melin, L.; Andersson, G. Effects of a cognitive-behavioral pain-management program. Behav. Res. Ther. 1998, 36, 915–930. [Google Scholar] [CrossRef]
- Nordin, C.A.; Michaelson, P.; Gard, G.; Eriksson, M.K. Effects of the web behavior change program for activity and multimodal pain rehabilitation: Randomized controlled trial. J. Med. Internet Res. 2016, 18, e5634. [Google Scholar] [CrossRef] [PubMed]
- Calner, T.; Nordin, C.; Eriksson, M.K.; Nyberg, L.; Gard, G.; Michaelson, P. Effects of a self-guided, web-based activity programme for patients with persistent musculoskeletal pain in primary healthcare: A randomized controlled trial. Eur. J. Pain 2017, 21, 1110–1120. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Fisher, E.; Craig, L.; Duggan, G.B.; Rosser, B.A.; Keogh, E. Psychological therapies (Internet-delivered) for the management of chronic pain in adults. Cochrane Database Syst. Rev. 2014, 2014, 10–11. [Google Scholar] [CrossRef]
- Kanters, T.A.; Timman, R.; Zijlstra-Vlasveld, M.C.; Muntingh, A.; Huijbregts, K.M.; Van Steenbergen-Weijenburg, K.M.; Bouwmans, C.A.M.; Van der Feltz-Cornelis, C.M.; Hakkaart-Van Roijen, L. Assessing costs using the treatment inventory cost in psychiatric patients (TiC-P), TiC-P mini and TiC-P MIDI. J. Ment. Health Policy Econ. 2019, 22, 15–24. [Google Scholar] [PubMed]
- Bouwmans, C.; De Jong, K.; Timman, R.; Zijlstra-Vlasveld, M.; Van Der Feltz-Cornelis, C.; Tan, S.S.; Hakkaart-Van Roijen, L. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv. Res. 2013, 13, 217. [Google Scholar] [CrossRef] [Green Version]
- IASP. Task Force on Multimodal Pain Treatment Defines Terms for Chronic Pain Care. 2018. Available online: https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=6981 (accessed on 1 June 2021).
- McCracken, L.M. Contextual Cognitive-Behavioral Therapy for Chronic Pain; IASP Press: Seattle, WA, USA, 2005. [Google Scholar]
- Robinson, P.; Wicksell, R.K.; Olsson, G.L. Acceptance and Commitment Therapy with chronic pain patients. In A Practical Guide to Acceptance and Commitment Therapy; Hayes, S., Strosahl, K., Eds.; Springer Science + Business Media: New York, NY, USA, 2004; pp. 315–345. [Google Scholar]
- Dahl, J.C.; Wilson, K.G.; Luciano, C.; Hayes, S.C. Acceptance and Commitment Therapy for Chronic Pain; Context Press: Reno, NV, USA, 2005. [Google Scholar]
- Currie, S.R.; Wilson, K.G.; Pontefract, A.J.; DeLaplante, L. Cognitive-behavioral treatment of insomnia secondary to chronic pain. J. Consult. Clin. Psychol. 2000, 68, 407–416. [Google Scholar] [CrossRef]
- Buhrman, M.; Skoglund, A.; Husell, J.; Bergström, K.; Gordh, T.; Hursti, T.; Bendelin, N.; Furmark, T.; Andersson, G. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: A randomized controlled trial. Behav. Res. Ther. 2013, 51, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy. An Experiential Approach to Behavior Change; Guilford Publications: New York, NY, USA, 1999. [Google Scholar]
- Lundgren, T.; Luoma, J.B.; Dahl, J.; Strosahl, K.; Melin, L. The Bull’s-Eye values survey: A psychometric evaluation. Cogn. Behav. Pract. 2012, 19, 518–526. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Turk, D.C.; Dworkin, R.H.; Revicki, D.; Harding, G.; Burke, L.B.; Cella, D.; Cleeland, C.S.; Cowan, P.; Farrar, J.T.; Hertz, S.; et al. Identifying important outcome domains for chronic pain clinical trials: An IMMPACT survey of people with pain. Pain 2008, 137, 276–285. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Vowles, K.E.; Eccleston, C. Accepfctance of chronic pain: Component analysis and a revised assessment method. Pain 2004, 107, 159–166. [Google Scholar] [CrossRef]
- Wicksell, R.K.; Olsson, G.L.; Melin, L. The Chronic Pain Acceptance Questionnaire (CPAQ)-further validation including a confirmatory factor analysis and a comparison with the Tampa Scale of Kinesiophobia. Eur. J. Pain 2009, 13, 760–768. [Google Scholar] [CrossRef]
- Fish, R.A.; McGuire, B.; Hogan, M.; Morrison, T.G.; Stewart, I. Validation of the Chronic Pain Acceptance Questionnaire (CPAQ) in an Internet sample and development and preliminary validation of the CPAQ-8. Pain 2010, 149, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Wicksell, R.K.; Lekander, M.; Sorjonen, K.; Olsson, G.L. The Psychological Inflexibility in Pain Scale (PIPS)—Statistical properties and model fit of an instrument to assess change processes in pain related disability. Eur. J. Pain 2010, 14, 771.e1–771.e14. [Google Scholar] [CrossRef] [PubMed]
- Trompetter, H.R.; Bohlmeijer, E.T.; Fox, J.P.; Schreurs, K.M.G. Psychological flexibility and catastrophizing as associated change mechanisms during online Acceptance & Commitment Therapy for chronic pain. Behav. Res. Ther. 2015, 74, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, M.K. The pain self-efficacy questionnaire: Taking pain into account. Eur. J. Pain 2007, 11, 153–163. [Google Scholar] [CrossRef]
- Asghari, A.; Nicholas, M.K. Pain self-efficacy beliefs and pain behaviour. A prospective study. Pain 2001, 94, 85–100. [Google Scholar] [CrossRef]
- Kerns, R.D.; Turk, D.C.; Rudy, T.E. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985, 23, 345–356. [Google Scholar] [CrossRef]
- Turk, D.C.; Rudy, T.E. Towards a comprehensive assessment of chronic pain patients. Behav. Res. Ther. 1987, 25, 237–249. [Google Scholar] [CrossRef]
- Turk, D.C.; Rudy, T.E. Toward an Empirically Derived Taxonomy of Chronic Pain Patients: Integration of Psychological Assessment Data. J. Consult. Clin. Psychol. 1988, 56, 233–238. [Google Scholar] [CrossRef]
- Bergström, G.; Jensen, I.B.; Bodin, L.; Linton, S.J.; Nygren, A.L.; Carlsson, S.G. Reliability and factor structure of the multidimensional pain inventory—Swedish language version (MPI-S). Pain 1998, 75, 101–110. [Google Scholar] [CrossRef]
- Nyberg, V.E.; Novo, M.; Sjölund, B.H. Do Multidimensional Pain Inventory Scale score changes indicate risk of receiving sick leave benefits 1 year after a pain rehabilitation programme? Disabil. Rehabil. 2011, 33, 1548–1556. [Google Scholar] [CrossRef] [PubMed]
- Gold, S.M.; Enck, P.; Hasselmann, H.; Friede, T.; Hegerl, U.; Mohr, D.C.; Otte, C. Control conditions for randomised trials of behavioural interventions in psychiatry: A decision framework. Lancet Psychiatry 2017, 4, 725–732. [Google Scholar] [CrossRef]
- Cuijpers, P.; Van Straten, A.; Andersson, G. Internet-administered cognitive behavior therapy for health problems: A systematic review. J. Behav. Med. 2008, 31, 169–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ringqvist, Å.; Dragioti, E.; Björk, M.; Larsson, B.; Gerdle, B. Moderate and Stable Pain Reductions as a Result of Interdisciplinary Pain Rehabilitation—A Cohort Study from the Swedish Quality Registry for Pain Rehabilitation (SQRP). J. Clin. Med. 2019, 8, 905. [Google Scholar] [CrossRef] [Green Version]
- Lenhard, W.; Lenhard, A. Calculation of Effect Sizes. Dettelbach (Germany): Psychometrica. 2016. Available online: https://www.psychometrica.de/effect_size.html (accessed on 1 June 2021).
- Jakobsen, J.C.; Gluud, C.; Wetterslev, J.; Winkel, P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—A practical guide with flowcharts. BMC Med. Res. Methodol. 2017, 17, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dragioti, E.; Evangelou, E.; Larsson, B.; Gerdle, B. Effectiveness of multidisciplinary programmes for clinical pain conditions: An umbrella review. J. Rehabil. Med. 2018, 50, 779–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCracken, L.M.; Marin, F.M. Current and future trends in psychology and chronic pain: Time for a change? Pain Manag. 2014, 4, 113–121. [Google Scholar] [CrossRef]
- Lin, J.; Paganini, S.; Sander, L.; Lüking, M.; Daniel Ebert, D.; Buhrman, M.; Andersson, G.; Baumeister, H. An Internet-based intervention for chronic pain—A three-arm randomized controlled study of the effectiveness of guided and unguided acceptance and commitment therapy. Dtsch. Ärztebl. Int. 2017, 114, 681–688. [Google Scholar] [PubMed] [Green Version]
- Åkerblom, S.; Cervin, M.; Perrin, S.; Rivano Fischer, M.; Gerdle, B.; McCracken, L.M. A Network Analysis of Clinical Variables in Chronic Pain: A Study from the Swedish Quality Registry for Pain Rehabilitation (SQRP). Pain Med. 2021, 22, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Trompetter, H.R.; Bohlmeijer, E.T.; Veehof, M.M.; Schreurs, K.M.G. Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: A randomized controlled trial. J. Behav. Med. 2015, 38, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Dear, B.F.; Titov, N.; Perry, K.N.; Johnston, L.; Wootton, B.M.; Terides, M.D.; Rapee, R.M.; Hudson, J.L. The Pain Course: A randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. Pain 2013, 154, 942–950. [Google Scholar] [CrossRef] [PubMed]
- Berman, R.L.H.; Iris, M.A.; Bode, R.; Drengenberg, C. The Effectiveness of an Online Mind-Body Intervention for Older Adults with Chronic Pain. J. Pain 2009, 10, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Gerdle, B.; Åkerblom, S.; Jansen, G.; Enthoven, P.; Ernberg, M.; Dong, H.J.; Stålnacke, B.M.; Äng, B.O.; Boersma, K. Who benefits from multimodal rehabilitation—An exploration of pain, psychological distress, and life impacts in over 35,000 chronic pain patients identified in the swedish quality registry for pain rehabilitation. J. Pain Res. 2019, 12, 891–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scascighini, L.; Toma, V.; Dober-Spielmann, S.; Sprott, H. Multidisciplinary treatment for chronic pain: A systematic review of interventions and outcomes. Rheumatology 2008, 47, 670–678. [Google Scholar] [CrossRef] [Green Version]
- Linton, S.J.; Nicholas, M.; Shaw, W. Why wait to address high-risk cases of acute low back pain? A comparison of stepped, stratified, and matched care. Pain 2018, 159, 2437–2441. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Mazza, S.; Frot, M.; Rey, A.E. A comprehensive literature review of chronic pain and memory. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2018, 87, 183–192. [Google Scholar] [CrossRef]
- De Guevara, C.M.L.; Fernández-Serrano, M.J.; Reyes del Paso, G.A.; Duschek, S. Executive function impairments in fibromyalgia syndrome: Relevance of clinical variables and body mass index. PLoS ONE 2018, 13, e0196329. [Google Scholar] [CrossRef] [Green Version]
- Andersson, G. The Internet and CBT: A Clinical Guide; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Andersson, G. Internet interventions: Past, present and future. Internet Interv. 2018, 12, 181–188. [Google Scholar] [CrossRef]
- Bendelin, N.; Björkdahl, P.; Risell, M.; Nelson, K.Z.; Gerdle, B.; Andersson, G.; Buhrman, M. Patients’ experiences of internet-based acceptance and commitment therapy for chronic pain: A qualitative study. BMC Musculoskelet. Disord. 2020, 21, 212. [Google Scholar] [CrossRef] [Green Version]
- Devan, H.; Hale, L.; Hempel, D.; Saipe, B.; Perry, M.A. What works and does not work in a self-management intervention for people with chronic pain? Qualitative systematic review and meta-synthesis. Phys. Ther. 2018, 98, 381–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buhrman, M.; Fredriksson, A.; Edström, G.; Shafiei, D.; Tärnqvist, C.; Ljótsson, B.; Hursti, T.; Gordh, T.; Andersson, G. Guided Internet-delivered cognitive behavioural therapy for chronic pain patients who have residual symptoms after rehabilitation treatment: Randomized controlled trial. Eur. J. Pain 2013, 17, 753–765. [Google Scholar] [CrossRef]
- Johansson, O.; Michel, T.; Andersson, G.; Paxling, B. Experiences of non-adherence to Internet-delivered cognitive behavior therapy: A qualitative study. Internet Interv. 2015, 2, 137–142. [Google Scholar] [CrossRef] [Green Version]
- Larsson, B.; Gard, G.; Karlsson, L.; Persson, A.L. Patient expectations for a multimodal pain rehabilitation programme: Active participation and coping skills. A qualitative study. Disabil. Rehabil. 2016, 38, 2135–2143. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef] [Green Version]
- Rozental, A.; Castonguay, L.; Dimidjian, S.; Lambert, M.; Shafran, R.; Andersson, G.; Carlbring, P. Negative effects in psychotherapy: Commentary and recommendations for future research and clinical practice. BJPsych Open 2018, 4, 307–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Intervention | Control | ||
|---|---|---|---|
| (n = 49) | (n = 54) | ||
| Age, mean (SD) | 36.35 (9.690) | 35.93 (9.75) | |
| Pain severity last week (VAS 0–10), mean (SD) | 6.93 (1.83) | 7.17 (1.45) | |
| Years since pain onset, mean (SD) | 8.4 (7.7) | 5.9 (6.0) | |
| 0–1 years, n (%) | 9 (18.4) | 7 (13) | |
| 1–5 years | 9 (18.4) | 17 (31.5) | |
| 5–10 years | 6 (12.2) | 9 (16.7) | |
| 10–15 years | 6 (12.2) | 4 (7.4) | |
| 15–20 years | 5 (10.2) | 2 (3.7) | |
| >20 years | 3 (6.1) | 2 (3.7) | |
| Women, n (%) | 43 (87.5) | 45 (83.3) | |
| Educational attainment, n (%) | |||
| Elementary (1–9 years) | 4 (8.2) | 5 (9.3) | |
| Secondary (10–12 years) | 28 (57.1) | 32 (59.3) | |
| University (>12 years) | 13 (26.5) | 11 (20.4) | |
| Other | 1 (2.0) | 0 (0) | |
| Unknown | 3 (6.1) | 6 (11.1) | |
| Working condition at enrollment, n (%) | |||
| Permanent or self–employed | 35 (71.4) | 28 (51.9) | |
| Temporary employment | 4 (8.2) | 2 (3.7) | |
| Unemployed | 9 (18.4) | 14 (25.9) | |
| Student | 2 (4.1) | 1 (1.9) | |
| Outside the labor market | 0 (0.0) | 4 (7.4) | |
| Working full time | 14 (28.6) | 10 (18.5) | |
| Working to any degree | 36 (73.5) | 32 (59.3) | |
| Sickness benefits to any degree, n (%) | 19 (38.8) | 19 (35.2) | |
| Group | Pretreatment | Post Treatment | Post Aftercare | 1 Year Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Md | n | Mean (SD) | Md | n | Mean (SD) | Md | n | Mean (SD) | Md | ||
| CPAQ | |||||||||||||
| Pain willingness | MMRP-IACT | 49 | 23.6 (8.0) | 23.0 | 39 | 29.1 (7.4) | 29.0 | 19 | 33.3 (7.9) | 35.0 | 27 | 30.0 (8.7) | 30.0 |
| MMRP | 54 | 21.7 (8.0) | 21.0 | 37 | 25.2 (7.3) | 24.0 | 30 | 28.7 (7.1) | 28.5 | 30 | 28.80 (9.0) | 27.0 | |
| Activity engagement | MMRP-IACT | 49 | 26.1 (12.6) | 25.0 | 38 | 35.6 (12.6) | 36.5 | 19 | 39.8 (14.1) | 39.0 | 25 | 36.5 (13.1) | 37.0 |
| MMRP | 54 | 25.6 (9.9) | 24.5 | 37 | 32.3 (10.1) | 31.0 | 30 | 34.1 (10.5) | 33.5 | 28 | 33.5 (13.4) | 31.0 | |
| Total | MMRP-IACT | 49 | 49.7 (18.6) | 49.0 | 37 | 64.8 (17.0) | 67.0 | 19 | 73.1 (20.0) | 77.0 | 25 | 67.0 (19.2) | 64.0 |
| MMRP | 54 | 47.3 (14.4) | 45.0 | 37 | 57.5 (15.9) | 56.0 | 30 | 62.8 (16.0) | 59.5 | 28 | 62.6 (21.4) | 59.0 | |
| PIPS | |||||||||||||
| Avoidance | MMRP-IACT | 49 | 35.8 (11.5) | 35.0 | 39 | 30.0 (10.3) | 29.0 | 21 | 24.4 (9.0) | 23.0 | 18 | 26.6 (10.2) | 26.5 |
| MMRP | 54 | 38.0 (8.9) | 38.0 | 38 | 31.5 (8.4) | 30.5 | 30 | 30.7 (9.9) | 31.5 | 22 | 30.3 (8.7) | 30.5 | |
| Fusion | MMRP-IACT | 49 | 20.4 (5.0) | 21.0 | 39 | 17.0 (5.4) | 18.0 | 21 | 14.4 (4.7) | 16.0 | 18 | 15.5 (3.5) | 15.5 |
| MMRP | 54 | 22.0 (4.2) | 22.0 | 38 | 18.5 (4.1) | 18.0 | 30 | 17.6 (4.7) | 18.5 | 22 | 17.7 (4.4) | 19.0 | |
| Total | MMRP-IACT | 49 | 56.3 (14.4) | 55.0 | 39 | 46.9 (13.4) | 48.0 | 21 | 38.8 (11.9) | 36.0 | 18 | 42.1 (12.3) | 42.5 |
| MMRP | 54 | 60.1 (11.7) | 59.5 | 38 | 50.0 (11.4) | 49.5 | 30 | 48.3 (13.2) | 51.0 | 22 | 48.0 (12.0) | 50.5 | |
| PSEQ | |||||||||||||
| MMRP-IACT | 48 | 26.8 (12.9) | 26.5 | 38 | 36.2 (13.5) | 36.0 | 21 | 40.5 (11.1) | 42.0 | 18 | 38.9 (13.2) | 41.5 | |
| MMRP | 54 | 25.7 (11.9) | 23.0 | 38 | 30.8 (11.2) | 30.5 | 30 | 31.0 (13.5) | 31.0 | 22 | 29.8 (13.2) | 31.5 | |
| MPI | |||||||||||||
| Pain severity | MMRP-IACT | 46 | 4.1 (1.1) | 4.0 | 42 | 4.0 (1.2) | 4.3 | 16 | 3.6 (0.7) | 3.5 | 27 | 4.0 (1.2) | 4.0 |
| MMRP | 52 | 3.9 (1.0) | 4.0 | 37 | 4.2 (1.1) | 4.3 | 29 | 3.5 (1.2) | 3.5 | 30 | 3.7 (0.9) | 3.8 | |
| Pain interference | MMRP-IACT | 46 | 4.0 (1.1) | 3.9 | 42 | 4.1 (0.9) | 4.1 | 16 | 3.1 (1.2) | 3.3 | 27 | 3.8 (1.1) | 3.9 |
| MMRP | 52 | 4.0 (1.0) | 4.1 | 37 | 4.2 (1.0) | 4.3 | 29 | 3.5 (1.4) | 3.9 | 30 | 4.0 (1.2) | 4.3 | |
| Life control | MMRP-IACT | 46 | 2.6 (1.1) | 2.8 | 41 | 3.3 (1.2) | 3.3 | 16 | 3.5 (0.8) | 3.5 | 27 | 2.9 (1.4) | 2.5 |
| MMRP | 52 | 2.9 (0.8) | 3.0 | 37 | 2.8 (0.9) | 2.8 | 29 | 3.1 (1.1) | 3.3 | 30 | 3.1 (1.2) | 3.0 | |
| Affective distress | MMRP-IACT | 46 | 3.3 (1.4) | 3.0 | 41 | 2.9 (1.3) | 2.7 | 16 | 2.9 (1.6) | 2.8 | 27 | 3.6 (1.3) | 3.7 |
| MMRP | 52 | 3.4 (1.0) | 3.3 | 37 | 3.5 (1.1) | 3.3 | 29 | 2.9 (1.1) | 3.0 | 30 | 3.2 (1.5) | 3.0 | |
| Social support | MMRP-IACT | 46 | 4.1 (1.4) | 4.5 | 41 | 3.7 (1.2) | 4.0 | 16 | 3.5 (1.7) | 3.8 | 27 | 3.7 (1.1) | 3.7 |
| MMRP | 52 | 3.9 (1.4) | 4.0 | 37 | 3.8 (1.3) | 4.0 | 29 | 3.5 (1.7) | 3.5 | 30 | 3.4 (1.4) | 3.7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bendelin, N.; Gerdle, B.; Blom, M.; Södermark, M.; Andersson, G. Internet-Delivered Acceptance and Commitment Therapy Added to Multimodal Pain Rehabilitation: A Cluster Randomized Controlled Trial. J. Clin. Med. 2021, 10, 5872. https://doi.org/10.3390/jcm10245872
Bendelin N, Gerdle B, Blom M, Södermark M, Andersson G. Internet-Delivered Acceptance and Commitment Therapy Added to Multimodal Pain Rehabilitation: A Cluster Randomized Controlled Trial. Journal of Clinical Medicine. 2021; 10(24):5872. https://doi.org/10.3390/jcm10245872
Chicago/Turabian StyleBendelin, Nina, Björn Gerdle, Marie Blom, Martin Södermark, and Gerhard Andersson. 2021. "Internet-Delivered Acceptance and Commitment Therapy Added to Multimodal Pain Rehabilitation: A Cluster Randomized Controlled Trial" Journal of Clinical Medicine 10, no. 24: 5872. https://doi.org/10.3390/jcm10245872
APA StyleBendelin, N., Gerdle, B., Blom, M., Södermark, M., & Andersson, G. (2021). Internet-Delivered Acceptance and Commitment Therapy Added to Multimodal Pain Rehabilitation: A Cluster Randomized Controlled Trial. Journal of Clinical Medicine, 10(24), 5872. https://doi.org/10.3390/jcm10245872






