Early Diagnosis and Real-Time Monitoring of Regional Lung Function Changes to Prevent Chronic Obstructive Pulmonary Disease Progression to Severe Emphysema
Abstract
1. Introduction
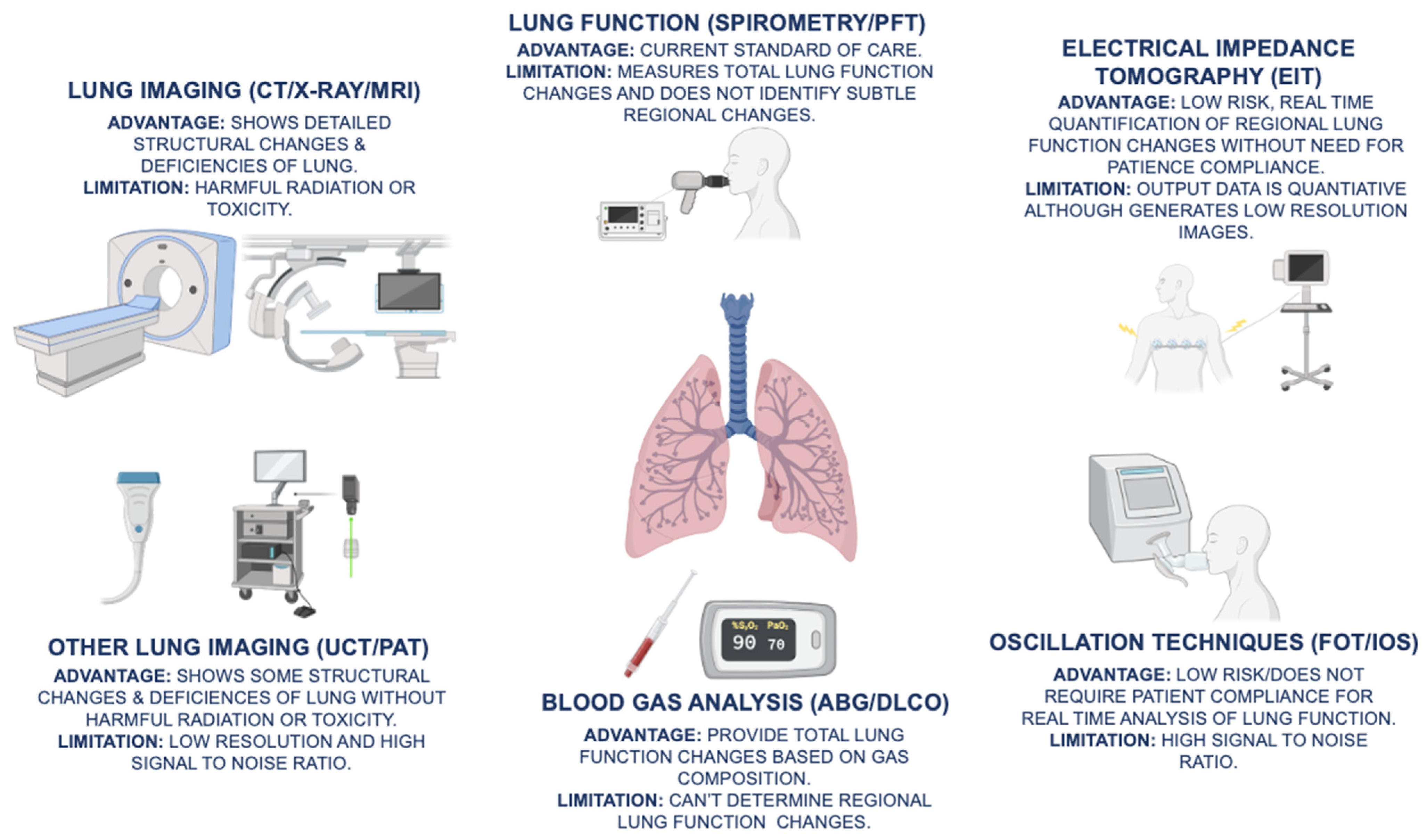
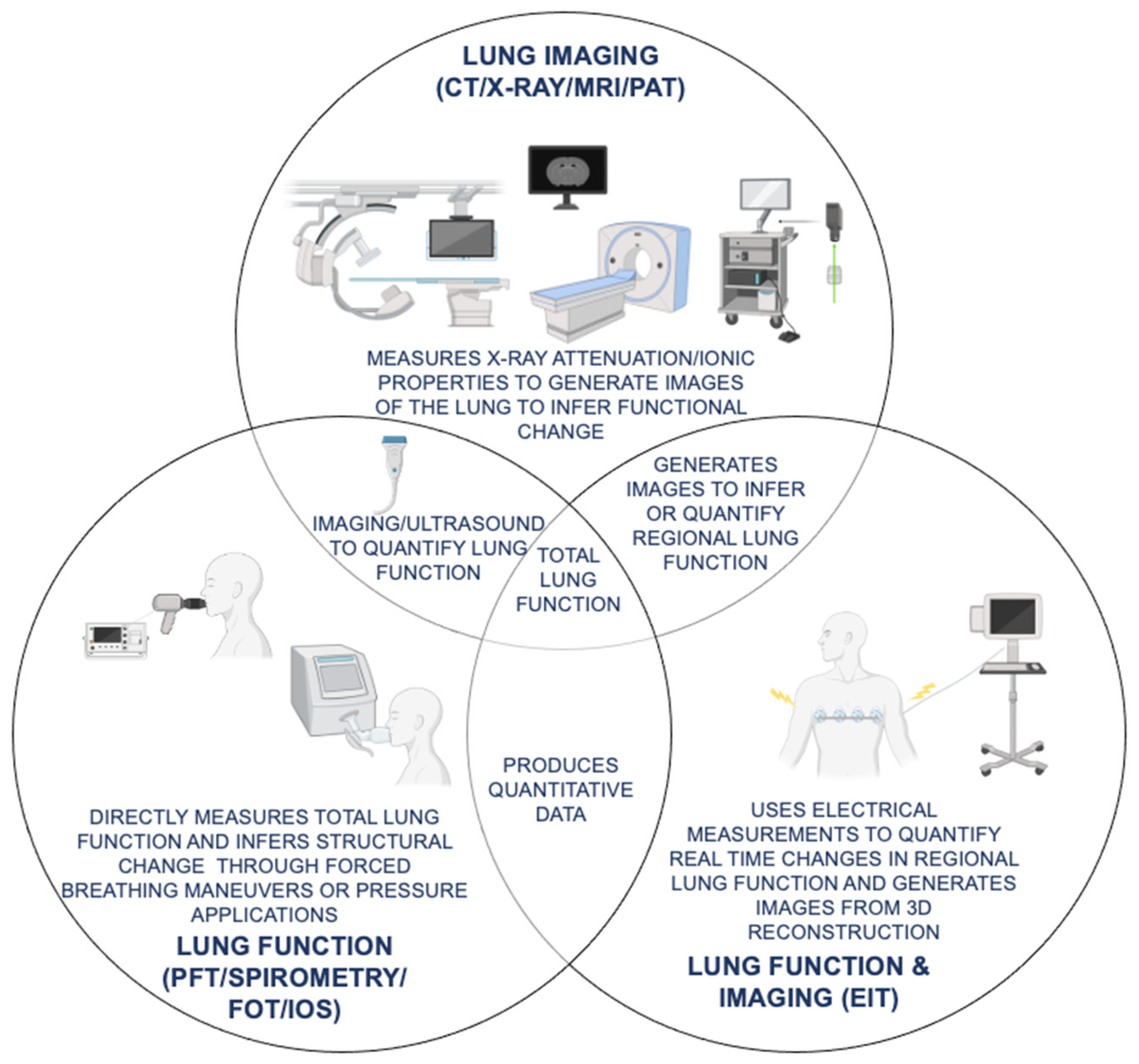
2. COPD Screening Tests for Evaluating Disease Initiation and Progression
2.1. COPD Screening Questionnaires
2.2. Six Minute Walk Test
3. Current COPD Standard of Care Diagnostics
3.1. Spirometry-Based Pulmonary Function Tests for Monitoring COPD Lung Function
3.2. Diffusing Capacity for Carbon Monoxide and Arterial Blood Gas Analysis
3.3. Functional Lung Imaging Modalities for Evaluating COPD Progression
4. Emerging COPD Diagnostics for Real Time Lung Function Assessment
4.1. X-ray Phase Contrast Imaging and Tomography for Functional Lung Imaging
4.2. Force and Impulse Oscillometry Measurements for Lung Function Analysis
4.3. Photoacoustic and Ultrasound Tomography as Emerging Lung Imaging Modalities
4.4. Electrical Impedance Tomography as Novel Diagnostics for Regional Lung Function Analysis
5. Perspective
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Halpin, D.M.G.; Criner, G.J.; Papi, A.; Singh, D.; Anzueto, A.; Martinez, F.J.; Agusti, A.A.; Vogelmeier, C.F. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2021, 203, 24–36. [Google Scholar] [CrossRef]
- Hikichi, M.; Mizumura, K.; Maruoka, S.; Gon, Y. Pathogenesis of chronic obstructive pulmonary disease (COPD) induced by cigarette smoke. J. Thorac. Dis. 2019, 11, S2129–S2140. [Google Scholar] [CrossRef] [PubMed]
- Berend, N. Contribution of air pollution to COPD and small airway dysfunction. Respirology 2016, 21, 237–244. [Google Scholar] [CrossRef]
- Zuo, L.; He, F.; Sergakis, G.G.; Koozehchian, M.S.; Stimpfl, J.N.; Rong, Y.; Diaz, P.T.; Best, T.M. Interrelated role of cigarette smoking, oxidative stress, and immune response in COPD and corresponding treatments. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2014, 307, L205–L218. [Google Scholar] [CrossRef] [PubMed]
- Forey, B.A.; Thornton, A.J.; Lee, P.N. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm. Med. 2011, 11, 36. [Google Scholar] [CrossRef]
- Davis, R.M.; Novotny, T.E. The epidemiology of cigarette smoking and its impact on chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1989, 140, S82–S84. [Google Scholar] [CrossRef]
- Halonen, J.I.; Lanki, T.; Yli-Tuomi, T.; Kulmala, M.; Tiittanen, P.; Pekkanen, J. Urban air pollution, and asthma and COPD hospital emergency room visits. Thorax 2008, 63, 635–641. [Google Scholar] [CrossRef] [PubMed]
- DeVries, R.; Kriebel, D.; Sama, S. Outdoor Air Pollution and COPD-Related Emergency Department Visits, Hospital Admissions, and Mortality: A Meta-Analysis. COPD 2017, 14, 113–121. [Google Scholar] [CrossRef]
- Ko, F.W.; Hui, D.S. Air pollution and chronic obstructive pulmonary disease. Respirology 2012, 17, 395–401. [Google Scholar] [CrossRef] [PubMed]
- McGeachie, M.J. Childhood asthma is a risk factor for the development of chronic obstructive pulmonary disease. Curr. Opin. Allergy Clin. Immunol. 2017, 17, 104–109. [Google Scholar] [CrossRef]
- Brode, S.K.; Ling, S.C.; Chapman, K.R. Alpha-1 antitrypsin deficiency: A commonly overlooked cause of lung disease. CMAJ 2012, 184, 1365–1371. [Google Scholar] [CrossRef]
- Silverman, E.K. Genetics of COPD. Annu. Rev. Physiol. 2020, 82, 413–431. [Google Scholar] [CrossRef]
- Waschki, B.; Kirsten, A.M.; Holz, O.; Mueller, K.C.; Schaper, M.; Sack, A.L.; Meyer, T.; Rabe, K.F.; Magnussen, H.; Watz, H. Disease Progression and Changes in Physical Activity in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2015, 192, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, N.; Muro, S.; Hirai, T.; Oguma, T.; Terada, K.; Marumo, S.; Kinose, D.; Ogawa, E.; Hoshino, Y.; Mishima, M. Impact of exacerbations on emphysema progression in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2011, 183, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, G.C.; Seemungal, T.A.; Bhowmik, A.; Wedzicha, J.A. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002, 57, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, A.; Bjerg, A.; Bjerg-Bäcklund, A.; Rönmark, E.; Larsson, L.G.; Lundbäck, B. Prevalence and underdiagnosis of COPD by disease severity and the attributable fraction of smoking Report from the Obstructive Lung Disease in Northern Sweden Studies. Respir. Med. 2006, 100, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Lipworth, B.J.; Jabbal, S. What can we learn about COPD from impulse oscillometry? Respir. Med. 2018, 139, 106–109. [Google Scholar] [CrossRef]
- Amaral, J.L.; Lopes, A.J.; Jansen, J.M.; Faria, A.C.; Melo, P.L. Machine learning algorithms and forced oscillation measurements applied to the automatic identification of chronic obstructive pulmonary disease. Comput. Methods Programs Biomed. 2012, 105, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Wijkstra, P.J.; TenVergert, E.M.; Van Altena, R.; Otten, V.; Postma, D.S.; Kraan, J.; Koëter, G.H. Reliability and validity of the chronic respiratory questionnaire (CRQ). Thorax 1994, 49, 465–467. [Google Scholar] [CrossRef]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M. The St George’s Respiratory Questionnaire. Respir. Med. 1991, 85 (Suppl. B), 25–31; discussion 27–33. [Google Scholar] [CrossRef]
- Gupta, N.; Pinto, L.M.; Morogan, A.; Bourbeau, J. The COPD assessment test: A systematic review. Eur. Respir. J. 2014, 44, 873–884. [Google Scholar] [CrossRef]
- Zhou, Z.; Zhou, A.; Zhao, Y.; Chen, P. Evaluating the Clinical COPD Questionnaire: A systematic review. Respirology 2017, 22, 251–262. [Google Scholar] [CrossRef]
- Tsiligianni, I.G.; van der Molen, T.; Moraitaki, D.; Lopez, I.; Kocks, J.W.; Karagiannis, K.; Siafakas, N.; Tzanakis, N. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm. Med. 2012, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.S.; Yoon, H.I.; Kim, D.K.; Yoo, C.G.; Lee, C.H. Comparison of COPD Assessment Test and Clinical COPD Questionnaire to predict the risk of exacerbation. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 101–107. [Google Scholar] [CrossRef]
- Celli, B.; Tetzlaff, K.; Criner, G.; Polkey, M.I.; Sciurba, F.; Casaburi, R.; Tal-Singer, R.; Kawata, A.; Merrill, D.; Rennard, S.; et al. The 6-Minute-Walk Distance Test as a Chronic Obstructive Pulmonary Disease Stratification Tool. Insights from the COPD Biomarker Qualification Consortium. Am. J. Respir. Crit. Care Med. 2016, 194, 1483–1493. [Google Scholar] [CrossRef]
- Waatevik, M.; Johannessen, A.; Hardie, J.A.; Bjordal, J.M.; Aukrust, P.; Bakke, P.S.; Eagan, T.M. Different COPD disease characteristics are related to different outcomes in the 6-minute walk test. COPD 2012, 9, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Marin, J.M.; Carrizo, S.J.; Gascon, M.; Sanchez, A.; Gallego, B.; Celli, B.R. Inspiratory capacity, dynamic hyperinflation, breathlessness, and exercise performance during the 6-minute-walk test in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2001, 163, 1395–1399. [Google Scholar] [CrossRef] [PubMed]
- Morakami, F.K.; Morita, A.A.; Bisca, G.W.; Felcar, J.M.; Ribeiro, M.; Furlanetto, K.C.; Hernandes, N.A.; Pitta, F. Can the six-minute walk distance predict the occurrence of acute exacerbations of COPD in patients in Brazil? J. Bras. Pneumol. 2017, 43, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Heresi, G.A.; Dweik, R.A. Strengths and limitations of the six-minute-walk test: A model biomarker study in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2011, 183, 1122–1124. [Google Scholar] [CrossRef]
- Walker, P.P.; Mitchell, P.; Diamantea, F.; Warburton, C.J.; Davies, L. Effect of primary-care spirometry on the diagnosis and management of COPD. Eur. Respir. J. 2006, 28, 945–952. [Google Scholar] [CrossRef]
- Johns, D.P.; Walters, J.A.; Walters, E.H. Diagnosis and early detection of COPD using spirometry. J. Thorac. Dis. 2014, 6, 1557–1569. [Google Scholar] [CrossRef]
- Schermer, T.R.; Robberts, B.; Crockett, A.J.; Thoonen, B.P.; Lucas, A.; Grootens, J.; Smeele, I.J.; Thamrin, C.; Reddel, H.K. Should the diagnosis of COPD be based on a single spirometry test? NPJ Prim. Care Respir. Med. 2016, 26, 16059. [Google Scholar] [CrossRef]
- Enright, P.; Brusasco, V. Counterpoint: Should we abandon FEV₁/FVC < 0.70 to detect airway obstruction? Yes. Chest 2010, 138, 1040–1042; discussion 1042–1044. [Google Scholar] [CrossRef] [PubMed]
- Rogliani, P.; Ora, J.; Puxeddu, E.; Cazzola, M. Airflow obstruction: Is it asthma or is it COPD? Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 3007–3013. [Google Scholar] [CrossRef] [PubMed]
- Modi, P.; Cascella, M. Diffusing capacity of the lungs for carbon monoxide. Available online: https://pubmed.ncbi.nlm.nih.gov/32310609 (accessed on 28 October 2021).
- Jensen, R.L.; Crapo, R.O. Diffusing capacity: How to get it right. Respir. Care 2003, 48, 777–782. [Google Scholar]
- Hughes, J.M.; Pride, N.B. Examination of the carbon monoxide diffusing capacity (DL(CO)) in relation to its KCO and VA components. Am. J. Respir. Crit. Care Med. 2012, 186, 132–139. [Google Scholar] [CrossRef]
- Balasubramanian, A.; MacIntyre, N.R.; Henderson, R.J.; Jensen, R.L.; Kinney, G.; Stringer, W.W.; Hersh, C.P.; Bowler, R.P.; Casaburi, R.; Han, M.K.; et al. Diffusing Capacity of Carbon Monoxide in Assessment of COPD. Chest 2019, 156, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Mahut, B.; Chevalier-Bidaud, B.; Plantier, L.; Essalhi, M.; Callens, E.; Graba, S.; Gillet-Juvin, K.; Valcke-Brossollet, J.; Delclaux, C. Diffusing capacity for carbon monoxide is linked to ventilatory demand in patients with chronic obstructive pulmonary disease. COPD 2012, 9, 16–21. [Google Scholar] [CrossRef]
- Sood, P.; Paul, G.; Puri, S. Interpretation of arterial blood gas. Indian J. Crit. Care Med. 2010, 14, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Burri, E.; Potocki, M.; Drexler, B.; Schuetz, P.; Mebazaa, A.; Ahlfeld, U.; Balmelli, C.; Heinisch, C.; Noveanu, M.; Breidthardt, T.; et al. Value of arterial blood gas analysis in patients with acute dyspnea: An observational study. Crit. Care 2011, 15, R145. [Google Scholar] [CrossRef] [PubMed]
- Güell Rous, R. Long-term oxygen therapy: Are we prescribing appropriately? Int. J. Chronic Obstr. Pulm. Dis. 2008, 3, 231–237. [Google Scholar] [CrossRef][Green Version]
- Singh, V.; Khatana, S.; Gupta, P. Blood gas analysis for bedside diagnosis. Natl. J. Maxillofac. Surg. 2013, 4, 136–141. [Google Scholar] [CrossRef]
- Ostridge, K.; Wilkinson, T.M. Present and future utility of computed tomography scanning in the assessment and management of COPD. Eur. Respir. J. 2016, 48, 216–228. [Google Scholar] [CrossRef]
- Labaki, W.W.; Martinez, C.H.; Martinez, F.J.; Galbán, C.J.; Ross, B.D.; Washko, G.R.; Barr, R.G.; Regan, E.A.; Coxson, H.O.; Hoffman, E.A.; et al. The Role of Chest Computed Tomography in the Evaluation and Management of the Patient with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2017, 196, 1372–1379. [Google Scholar] [CrossRef] [PubMed]
- Diaz, A.A.; Come, C.E.; Ross, J.C.; San José Estépar, R.; Han, M.K.; Loring, S.H.; Silverman, E.K.; Washko, G.R.; Investigators, C. Association between airway caliber changes with lung inflation and emphysema assessed by volumetric CT scan in subjects with COPD. Chest 2012, 141, 736–744. [Google Scholar] [CrossRef][Green Version]
- Occhipinti, M.; Bruni, C.; Camiciottoli, G.; Bartolucci, M.; Bellando-Randone, S.; Bassetto, A.; Cuomo, G.; Giuggioli, D.; Ciardi, G.; Fabbrizzi, A.; et al. Quantitative analysis of pulmonary vasculature in systemic sclerosis at spirometry-gated chest CT. Ann. Rheum. Dis. 2020, 79, 1210–1217. [Google Scholar] [CrossRef] [PubMed]
- Washko, G.R. Diagnostic imaging in COPD. Semin. Respir. Crit. Care Med. 2010, 31, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Haruna, A.; Muro, S.; Nakano, Y.; Ohara, T.; Hoshino, Y.; Ogawa, E.; Hirai, T.; Niimi, A.; Nishimura, K.; Chin, K.; et al. CT scan findings of emphysema predict mortality in COPD. Chest 2010, 138, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Biederer, J.; Beer, M.; Hirsch, W.; Wild, J.; Fabel, M.; Puderbach, M.; Van Beek, E.J. MRI of the lung (2/3). Why … when … how? Insights Imaging 2012, 3, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Sverzellati, N.; Molinari, F.; Pirronti, T.; Bonomo, L.; Spagnolo, P.; Zompatori, M. New insights on COPD imaging via CT and MRI. Int. J. Chronic Obstr. Pulm. Dis. 2007, 2, 301–312. [Google Scholar]
- Sarma, A.; Heilbrun, M.E.; Conner, K.E.; Stevens, S.M.; Woller, S.C.; Elliott, C.G. Radiation and chest CT scan examinations: What do we know? Chest 2012, 142, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Smith-Bindman, R.; Lipson, J.; Marcus, R.; Kim, K.P.; Mahesh, M.; Gould, R.; Berrington de González, A.; Miglioretti, D.L. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch. Intern. Med. 2009, 169, 2078–2086. [Google Scholar] [CrossRef]
- Miller, G.W.; Mugler, J.P.; Sá, R.C.; Altes, T.A.; Prisk, G.K.; Hopkins, S.R. Advances in functional and structural imaging of the human lung using proton MRI. NMR Biomed. 2014, 27, 1542–1556. [Google Scholar] [CrossRef]
- Theilmann, R.J.; Arai, T.J.; Samiee, A.; Dubowitz, D.J.; Hopkins, S.R.; Buxton, R.B.; Prisk, G.K. Quantitative MRI measurement of lung density must account for the change in T(2) (*) with lung inflation. J. Magn. Reson. Imaging 2009, 30, 527–534. [Google Scholar] [CrossRef]
- Croton, L.C.P.; Morgan, K.S.; Paganin, D.M.; Kerr, L.T.; Wallace, M.J.; Crossley, K.J.; Miller, S.L.; Yagi, N.; Uesugi, K.; Hooper, S.B.; et al. In situ phase contrast X-ray brain CT. Sci. Rep. 2018, 8, 11412. [Google Scholar] [CrossRef] [PubMed]
- Kitchen, M.J.; Buckley, G.A.; Kerr, L.T.; Lee, K.L.; Uesugi, K.; Yagi, N.; Hooper, S.B. Emphysema quantified: Mapping regional airway dimensions using 2D phase contrast X-ray imaging. Biomed. Opt. Express 2020, 11, 4176–4190. [Google Scholar] [CrossRef] [PubMed]
- Kitchen, M.J.; Lewis, R.A.; Morgan, M.J.; Wallace, M.J.; Siew, M.L.; Siu, K.K.; Habib, A.; Fouras, A.; Yagi, N.; Uesugi, K.; et al. Dynamic measures of regional lung air volume using phase contrast x-ray imaging. Phys. Med. Biol. 2008, 53, 6065–6077. [Google Scholar] [CrossRef]
- Lewis, R.A.; Yagi, N.; Kitchen, M.J.; Morgan, M.J.; Paganin, D.; Siu, K.K.; Pavlov, K.; Williams, I.; Uesugi, K.; Wallace, M.J.; et al. Dynamic imaging of the lungs using x-ray phase contrast. Phys. Med. Biol. 2005, 50, 5031–5040. [Google Scholar] [CrossRef] [PubMed]
- Bravin, A.; Coan, P.; Suortti, P. X-ray phase-contrast imaging: From pre-clinical applications towards clinics. Phys. Med. Biol. 2013, 58, R1–R35. [Google Scholar] [CrossRef]
- Zhou, W.; Majidi, K.; Brankov, J.G. Analyzer-based phase-contrast imaging system using a micro focus X-ray source. Rev. Sci. Instrum. 2014, 85, 085114. [Google Scholar] [CrossRef]
- Vij, N. Prognosis-Based Early Intervention Strategies to Resolve Exacerbation and Progressive Lung Function Decline in Cystic Fibrosis. J. Pers. Med. 2021, 11, 96. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.O.; Faria, A.C.D.; Lopes, A.J.; de Melo, P.L. Forced oscillation technique for early detection of the effects of smoking and COPD: Contribution of fractional-order modeling. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3281–3295. [Google Scholar] [CrossRef] [PubMed]
- Oostveen, E.; MacLeod, D.; Lorino, H.; Farré, R.; Hantos, Z.; Desager, K.; Marchal, F. The forced oscillation technique in clinical practice: Methodology, recommendations and future developments. Eur. Respir. J. 2003, 22, 1026–1041. [Google Scholar] [CrossRef]
- Desiraju, K.; Agrawal, A. Impulse oscillometry: The state-of-art for lung function testing. Lung India 2016, 33, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Bickel, S.; Popler, J.; Lesnick, B.; Eid, N. Impulse oscillometry: Interpretation and practical applications. Chest 2014, 146, 841–847. [Google Scholar] [CrossRef]
- Bhattarai, P.; Myers, S.; Chia, C.; Weber, H.C.; Young, S.; Williams, A.D.; Sohal, S.S. Clinical Application of Forced Oscillation Technique (FOT) in Early Detection of Airway Changes in Smokers. J. Clin. Med. 2020, 9, 2778. [Google Scholar] [CrossRef] [PubMed]
- Li, L.Y.; Yan, T.S.; Yang, J.; Li, Y.Q.; Fu, L.X.; Lan, L.; Liang, B.M.; Wang, M.Y.; Luo, F.M. Impulse oscillometry for detection of small airway dysfunction in subjects with chronic respiratory symptoms and preserved pulmonary function. Respir. Res. 2021, 22, 68. [Google Scholar] [CrossRef]
- Faria, A.C.; Lopes, A.J.; Jansen, J.M.; Melo, P.L. Evaluating the forced oscillation technique in the detection of early smoking-induced respiratory changes. Biomed. Eng. Online 2009, 8, 22. [Google Scholar] [CrossRef]
- Amaral, J.L.; Lopes, A.J.; Faria, A.C.; Melo, P.L. Machine learning algorithms and forced oscillation measurements to categorise the airway obstruction severity in chronic obstructive pulmonary disease. Comput. Methods Programs Biomed. 2015, 118, 186–197. [Google Scholar] [CrossRef]
- Malmberg, L.P.; Mieskonen, S.; Pelkonen, A.; Kari, A.; Sovijärvi, A.R.; Turpeinen, M. Lung function measured by the oscillometric method in prematurely born children with chronic lung disease. Eur. Respir. J. 2000, 16, 598–603. [Google Scholar] [CrossRef]
- Kalhoff, H.; Breidenbach, R.; Smith, H.J.; Marek, W. Impulse oscillometry in preschool children and association with body mass index. Respirology 2011, 16, 174–179. [Google Scholar] [CrossRef]
- Uchida, A.; Ito, S.; Suki, B.; Matsubara, H.; Hasegawa, Y. Influence of cheek support on respiratory impedance measured by forced oscillation technique. Springerplus 2013, 2, 342. [Google Scholar] [CrossRef]
- Kim, C.W.; Kim, J.S.; Park, J.W.; Hong, C.S. Clinical applications of forced oscillation techniques (FOT) in patients with bronchial asthma. Korean J. Intern. Med. 2001, 16, 80–86. [Google Scholar] [CrossRef]
- Xia, J.; Yao, J.; Wang, L.V. Photoacoustic tomography: Principles and advances. Electromagn. Waves 2014, 147, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Hou, R.; Le, T.; Murgu, S.D.; Chen, Z.; Brenner, M. Recent advances in optical coherence tomography for the diagnoses of lung disorders. Expert Rev. Respir. Med. 2011, 5, 711–724. [Google Scholar] [CrossRef]
- Beard, P. Biomedical photoacoustic imaging. Interface Focus 2011, 1, 602–631. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.; Jokerst, J.V. Strategies for Image-Guided Therapy, Surgery, and Drug Delivery Using Photoacoustic Imaging. Theranostics 2019, 9, 1550–1571. [Google Scholar] [CrossRef]
- Zhao, Y.; Liu, W.; Tian, Y.; Yang, Z.; Wang, X.; Zhang, Y.; Tang, Y.; Zhao, S.; Wang, C.; Liu, Y.; et al. Anti-EGFR Peptide-Conjugated Triangular Gold Nanoplates for Computed Tomography/Photoacoustic Imaging-Guided Photothermal Therapy of Non-Small Cell Lung Cancer. ACS Appl. Mater. Interfaces 2018, 10, 16992–17003. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, D.; Jung, U.; Kim, C. Photoacoustic imaging platforms for multimodal imaging. Ultrasonography 2015, 34, 88–97. [Google Scholar] [CrossRef]
- Burgholzer, P.; Bauer-Marschallinger, J.; Reitinger, B.; Berer, T. Resolution Limits in Photoacoustic Imaging Caused by Acoustic Attenuation. J. Imaging 2019, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Upputuri, P.K.; Pramanik, M. Fast photoacoustic imaging systems using pulsed laser diodes: A review. Biomed. Eng. Lett. 2018, 8, 167–181. [Google Scholar] [CrossRef]
- Jago, J.R.; Whittingham, T.A. Experimental studies in transmission ultrasound computed tomography. Phys. Med. Biol. 1991, 36, 1515–1527. [Google Scholar] [CrossRef]
- Liu, C.; Xue, C.; Zhang, B.; Zhang, G.; He, C. The Application of an Ultrasound Tomography Algorithm in a Novel Ring 3D Ultrasound Imaging System. Sensors 2018, 18, 1332. [Google Scholar] [CrossRef] [PubMed]
- Milne, S.; Huvanandana, J.; Nguyen, C.; Duncan, J.M.; Chapman, D.G.; Tonga, K.O.; Zimmermann, S.C.; Slattery, A.; King, G.G.; Thamrin, C. Time-based pulmonary features from electrical impedance tomography demonstrate ventilation heterogeneity in chronic obstructive pulmonary disease. J. Appl. Physiol. 2019, 127, 1441–1452. [Google Scholar] [CrossRef]
- Trenk, F.; Mendes, L.; Carvalho, P.; Paiva, R.P.; Henriques, J.; Maglaveras, N.; Chouvarda, I.; Tsara, V.; Teixeira, C.A. Evaluation of lung ventilation distribution in chronic obstructive pulmonary disease patients using the global inhomogeneity index. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; 2016, pp. 5286–5289. [Google Scholar] [CrossRef]
- Vogt, B.; Deuß, K.; Hennig, V.; Zhao, Z.; Lautenschläger, I.; Weiler, N.; Frerichs, I. Regional lung function in nonsmokers and asymptomatic current and former smokers. ERJ Open Res. 2019, 5, 240. [Google Scholar] [CrossRef]
- Schullcke, B.; Gong, B.; Krueger-Ziolek, S.; Soleimani, M.; Mueller-Lisse, U.; Moeller, K. Structural-functional lung imaging using a combined CT-EIT and a Discrete Cosine Transformation reconstruction method. Sci. Rep. 2016, 6, 25951. [Google Scholar] [CrossRef] [PubMed]
- Braun, F.; Proença, M.; Lemay, M.; Bertschi, M.; Adler, A.; Thiran, J.P.; Solà, J. Limitations and challenges of EIT-based monitoring of stroke volume and pulmonary artery pressure. Physiol. Meas. 2018, 39, 014003. [Google Scholar] [CrossRef] [PubMed]
- Vij, N.; Chandramani-Shivalingappa, P.; Van Westphal, C.; Hole, R.; Bodas, M. Cigarette smoke-induced autophagy impairment accelerates lung aging, COPD-emphysema exacerbations and pathogenesis. Am. J. Physiol. Cell Physiol. 2018, 314, C73–C87. [Google Scholar] [CrossRef]
- Mercado, N.; Ito, K.; Barnes, P.J. Accelerated ageing of the lung in COPD: New concepts. Thorax 2015, 70, 482–489. [Google Scholar] [CrossRef]
- Ito, K.; Barnes, P.J. COPD as a disease of accelerated lung aging. Chest 2009, 135, 173–180. [Google Scholar] [CrossRef] [PubMed]
- De Ramón Fernández, A.; Ruiz Fernández, D.; Marcos-Jorquera, D.; Gilart Iglesias, V. Support System for Early Diagnosis of Chronic Obstructive Pulmonary Disease Based on the Service-Oriented Architecture Paradigm and Business Process Management Strategy: Development and Usability Survey Among Patients and Health Care Providers. J. Med. Internet. Res. 2020, 22, e17161. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, T.M.; Donaldson, G.C.; Hurst, J.R.; Seemungal, T.A.; Wedzicha, J.A. Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2004, 169, 1298–1303. [Google Scholar] [CrossRef]
- Agarwal, A.; Ressler, D.; Snyder, G. The current and future state of companion diagnostics. Pharmgenomics Pers. Med. 2015, 8, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, J.T. Companion diagnostics: The key to personalized medicine. Foreword. Expert Rev. Mol. Diagn. 2015, 15, 153–156. [Google Scholar] [CrossRef]
- Myers, M.B. Targeted therapies with companion diagnostics in the management of breast cancer: Current perspectives. Pharmgenomics Pers. Med. 2016, 9, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.; Kinzler, K.W.; Vogelstein, B. The role of companion diagnostics in the development and use of mutation-targeted cancer therapies. Nat. Biotechnol. 2006, 24, 985–995. [Google Scholar] [CrossRef]
- Franssen, F.M.; Alter, P.; Bar, N.; Benedikter, B.J.; Iurato, S.; Maier, D.; Maxheim, M.; Roessler, F.K.; Spruit, M.A.; Vogelmeier, C.F.; et al. Personalized medicine for patients with COPD: Where are we? Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 1465–1484. [Google Scholar] [CrossRef]
- Bafadhel, M.; McKenna, S.; Terry, S.; Mistry, V.; Pancholi, M.; Venge, P.; Lomas, D.A.; Barer, M.R.; Johnston, S.L.; Pavord, I.D.; et al. Blood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: A randomized placebo-controlled trial. Am. J. Respir. Crit. Care Med. 2012, 186, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Pompe, E.; van Rikxoort, E.M.; Schmidt, M.; Rühaak, J.; Estrella, L.G.; Vliegenthart, R.; Oudkerk, M.; de Koning, H.J.; van Ginneken, B.; de Jong, P.A.; et al. Parametric response mapping adds value to current computed tomography biomarkers in diagnosing chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2015, 191, 1084–1086. [Google Scholar] [CrossRef]
- Pompe, E.; Galbán, C.J.; Ross, B.D.; Koenderman, L.; Ten Hacken, N.H.; Postma, D.S.; van den Berge, M.; de Jong, P.A.; Lammers, J.J.; Mohamed Hoesein, F.A. Parametric response mapping on chest computed tomography associates with clinical and functional parameters in chronic obstructive pulmonary disease. Respir. Med. 2017, 123, 48–55. [Google Scholar] [CrossRef]
- Hope, T.A.; Iles, S.E. Technology review: The use of electrical impedance scanning in the detection of breast cancer. Breast Cancer Res. 2004, 6, 69–74. [Google Scholar] [CrossRef] [PubMed]
| Lung Diagnostics and Monitoring | Status | Regional Lung Function | Quantitative Output | CDx Use | Early Exacerbation | Diagnostic Setting | Risks |
|---|---|---|---|---|---|---|---|
| 6MWT | Current | No | No/Limited | Low | Limited | Bedside | No |
| COPD Questionnaire | Current | No | Yes | Low | Yes | Bedside | No |
| PFT/Spirometry | Current | No | Yes | Low | No | PFT Lab/Bedside | No |
| CT/MRI | Current | Yes/Inference | Yes/Inference | Low | No | Radiology | High |
| ABG and DLCO | Current | No | Yes | Low | No | Bedside | Minimal |
| FOT/IOS | Emerging | No | Yes | Medium | No | Bedside | Minimal |
| PAT | Emerging | Yes | Yes/Inference | Low | No | Radiology/Clinic | Minimal |
| UCT/XPC | Emerging | No | Yes/Inference | Low | No | Radiology/Clinic | Medium |
| EIT | Emerging | Yes | Yes | High | Yes | Bedside | No |
| COPD Diagnostic Comparison | Disease Details | Diagnostic Accuracy | Risks | Patient Compliance | Time |
|---|---|---|---|---|---|
| X-ray/XPC | Low | Low | Low radiation | No | 15 min |
| CT/MRI | High | High | Radiation/Contrast Agents | No | 20 min–2 h |
| PFT/Spirometry | Low | Moderate | Low | Yes | 30 min–1 h |
| ABG/DLCO | Low | Moderate | Low | No | 15 min |
| FOT/IOS | Low | Moderate | NA | No | Real Time |
| PAT | Moderate | Moderate | NA | No | Real time |
| UCT | Low | Moderate | Low | No | Real time |
| EIT | Moderate | High | NA | No | Real Time |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, T.; Vij, N. Early Diagnosis and Real-Time Monitoring of Regional Lung Function Changes to Prevent Chronic Obstructive Pulmonary Disease Progression to Severe Emphysema. J. Clin. Med. 2021, 10, 5811. https://doi.org/10.3390/jcm10245811
Jung T, Vij N. Early Diagnosis and Real-Time Monitoring of Regional Lung Function Changes to Prevent Chronic Obstructive Pulmonary Disease Progression to Severe Emphysema. Journal of Clinical Medicine. 2021; 10(24):5811. https://doi.org/10.3390/jcm10245811
Chicago/Turabian StyleJung, Tony, and Neeraj Vij. 2021. "Early Diagnosis and Real-Time Monitoring of Regional Lung Function Changes to Prevent Chronic Obstructive Pulmonary Disease Progression to Severe Emphysema" Journal of Clinical Medicine 10, no. 24: 5811. https://doi.org/10.3390/jcm10245811
APA StyleJung, T., & Vij, N. (2021). Early Diagnosis and Real-Time Monitoring of Regional Lung Function Changes to Prevent Chronic Obstructive Pulmonary Disease Progression to Severe Emphysema. Journal of Clinical Medicine, 10(24), 5811. https://doi.org/10.3390/jcm10245811







