PSYChosomatic Medicine in ONcologIc and Cardiac Disease (PSYCHONIC) Study—A Retrospective and Prospective Observational Research Protocol
Abstract: Introduction
1. Introduction
2. Materials and Methods
2.1. Aims
- (1)
- To prospectively assess the clinical and psychological characteristics at enrollment, and the real-world outcomes at one and five years in patients (pts) with AMI, TTS, and BC who (a) have undergone ontopsychological STP or (b) declined the treatment, as well as (c) a control group of age/sex-matched subjects without major active diseases (for a practical exposition they are referred to as “Healthy Subjects”, HS) not undergoing psychotherapy at enrollment
- (2)
- To assess:
- The perception of their body and emotions in each group at baseline and follow-up;
- Dream symbols and patterns in each group, including retrospective evaluation of past dreams (until childhood and adolescence), at baseline and follow-up;
- The correlation of past dream symbols and patterns with the onset of disease in each group;
- The correlation between baseline psychological data/evaluations and study outcomes.
The Rationale for the Study Aims
- (1)
- Poor awareness of emotions, which may have reflected a lack of the perception of one’s body, or parts of one’s body. Patients seemed to have a painful perception of parts of their body (mainly the head and/or the chest, with particular reference to their heart), whereas they did not have a perception of other parts, as if they were “anesthetized”. In the STEP-IN-AMI pts, there was an improvement of body/emotional perception during psychotherapeutic intervention with body relaxation training [33], conducted both in individual and group meetings. Patients were encouraged to explore their bodily sensations, starting with the visceral zone (i.e., abdomen), with the help of abdominal breathing. From our experience, abdominal breathing seems to act as a strong stimulus to the visceral brain, which is continuously active throughout one’s entire life (even if we have lost our conscious perception of it), and the subjective contact with the visceral zone translates as an important mediator of inner emotions and feelings [34].
- (2)
- An apparent presence of specific dream configurations in the period before AMI (i.e., distressing dreams or repeated nightmares; no memory of dream content; or selective memory only of dreams of childhood and adolescence), which again improved when recovering from the acute event in those undergoing STP [10,11].
2.2. Participants
2.2.1. Inclusion Criteria
- (1)
- Patients with AMI with ST-elevation on the admission electrocardiogram (STEMI) and without ST elevation (NSTEMI) treated with urgent percutaneous coronary intervention (PCI); up to 12 h for STEMI and 48 h for NSTEMI patients.
- (2)
- Patients with TTS
- (3)
- Patients recently operated on for non-metastatic BC treated with radiotherapy and/or chemotherapy and/or hormone therapy.
- (4)
- A control group of subjects without major active diseases (HS), matched for age and sex. This includes subjects without clinical evidence of major diseases that required hospitalization in the last ten years or chronic medical therapy (e.g., anti-neoplastic, immunosuppressant, cortisone, psychiatric, etc.), and not undergoing or scheduled for psychotherapy at enrollment.
2.2.2. Exclusion Criteria
Sample Sizing
2.3. Therapies
3. Endpoints and Outcome Measures
- (A)
- Qualitative psychological endpoints:
- Perception of body and emotions; qualitative analysis will be performed with two questionnaires, administered to all participants: (1) Enrollment body perception questionnaire (Supplementary Material S1); (2) One-year follow-up body perception questionnaire (Supplementary Material S2).
- Subject’s memory of last week, last month, last year, and past years’ dreams only at enrollment. A qualitative analysis will be performed with two questionnaires, administered to all participants: (1) Enrollment dream questionnaire (Supplementary Material S3); (2) One-year follow-up dream questionnaire (Supplementary Material S4).
- 6DT patterns characteristics
- (B)
- Medical endpoints
- -
- In AMI and TTS pts: the cumulative incidence of new cardiac events (i.e., MI, revascularization, life-threatening ventricular arrhythmias, recurrence of typical angina pectoris, stroke, and death all-cause), plus the occurrence of any clinically significant new medical disorder (active diseases requiring hospitalization or chronic medical therapy, or that cause a transient or permanent physical limitation), at the one and five-year follow-up in patients undergoing psychotherapy plus standard medical therapy and those on standard medical therapy only.
- -
- In BC patients: the incidence of breast cancer relapse, metastasis, or the occurrence of any clinically significant new medical disorder (that is an active disease requiring hospitalization or chronic medical therapy, or that cause a transient or permanent physical limitation), at the one and five-year follow-up in patients undergoing psychotherapy plus standard therapy and those on standard therapy only.
- -
- In all pts: new hospital admissions.
3.1. Tests
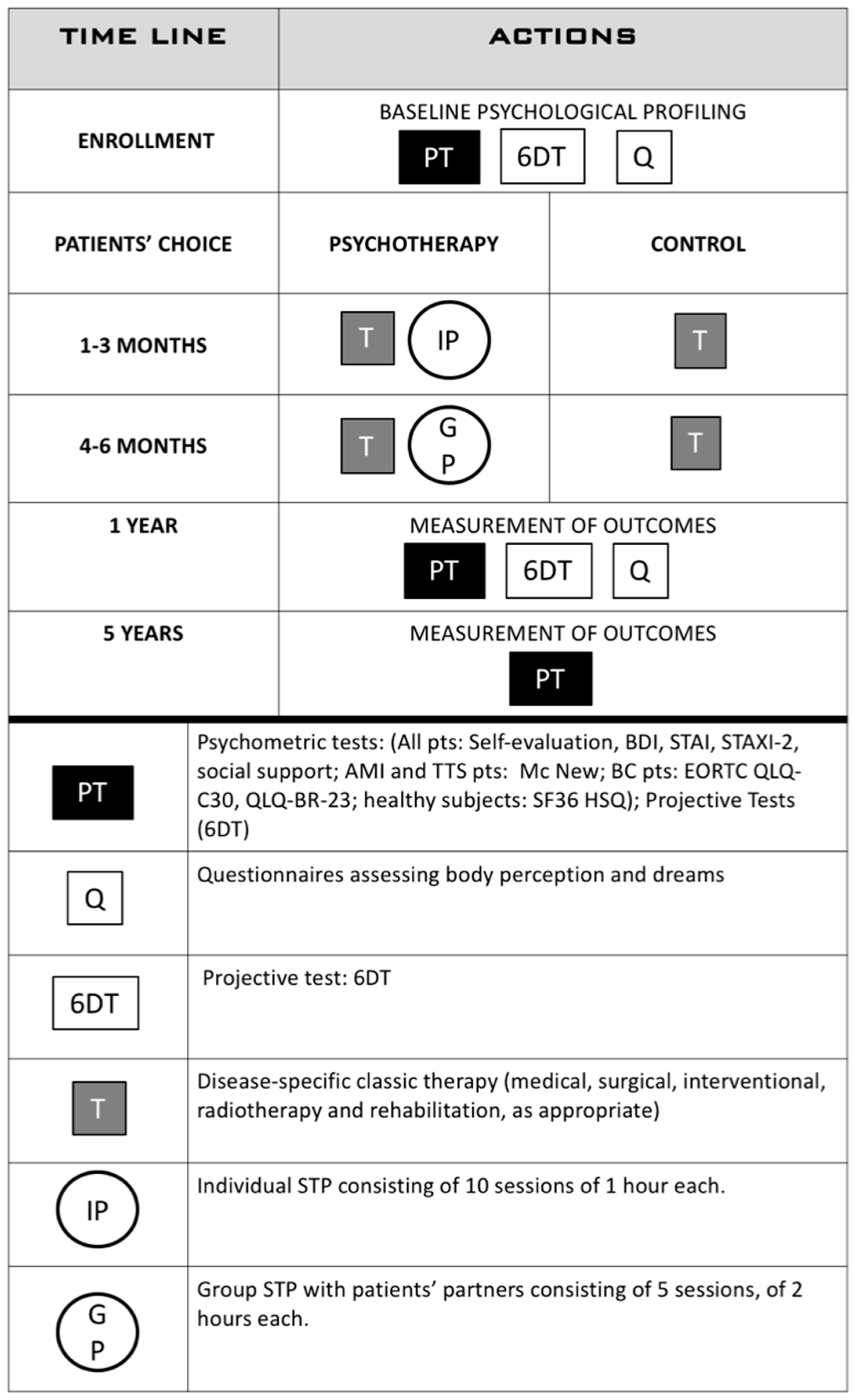
3.2. Study Design
3.2.1. Enrollment
- (a)
- Personal demographics and clinical history;
- (b)
- Personal history: patient’s place and date of birth; details about both parents, whether they are alive or their age of death, cause of death, previous and/or current job, their number of siblings (including birth order), patient’s education; previous and current occupation; marital status and age when married; the age of their partner and his/her name, education, and occupation; their number of children, their names, ages, education level, and occupation; favorite personal hobbies; and any other relationships or information about their personal life that the patient feels is relevant to their health and well being.
- (c)
- Psychometric tests (see above);
- (d)
- The Six Drawing test (6DT).
3.2.2. Treatment Choice, Implementation, and Group Allocation
3.2.3. Follow-Up
4. Statistical Analysis
Enrollment Status
5. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2019; Available online: https://apps.who.int/iris/handle/10665/324835 (accessed on 30 March 2021).
- Shah, A.J.; Vaccarino, V. Psychosocial Risk Factors and Coronary Artery Disease. In Psychotherapy for Ischemic Heart Disease; Roncella, A., Pristipino, C., Eds.; Springer: Cham, Switzerland, 2016; Chapter 2; p. 29. [Google Scholar] [CrossRef]
- Allan, R.; Pace, T.M.; Dorri, Y. Behavioral Cardiology/Cardiac Psychology: Translating research into practice. J. Integr. Cardiol. 2019, 4, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Schouten, B.; Avau, B.; Bekkering, G.T.E.; Vankrunkelsven, P.; Mebis, J.; Hellings, J.; Van Hecke, A.; Cochrane Gynaecological, Neuro-Oncology and Orphan Cancer Group. Systematic screening and assessment of psychosocial well-being and care needs of people with cancer. Cochrane Database Syst. Rev. 2019, 3, CD012387. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Sherwood, A.; Smith, P.J.; Watkins, L.; Mabe, S.; Kraus, W.E.; Ingle, K.; Miller, P.; Hinderliter, A. Enhancing cardiac rehabilitation with stress management training: A randomized clinical efficacy trial. Circulation 2016, 133, 1341–1350. [Google Scholar] [CrossRef] [Green Version]
- Biondi-Zoccai, G.; Mazza, M.; Roever, L.; Roever, L.; van Dixhoorn, J.; Frati, G.; Abbate, A. Evidence-Based Psychotherapy in Ischemic Heart Disease: Umbrella Review and Updated Meta-Analysis. In Psychotherapy for Ischemic Heart Disease; Roncella, A., Pristipino, C., Eds.; Springer: Cham, Switzerland, 2016; Chapter 10; p. 131. [Google Scholar] [CrossRef]
- Richards, S.H.; Anderson, L.; Jenkinson, C.; Whalley, B.; Rees, K.; Davies, P.; Bennett, P.; Liu, Z.; West, R.; Thompson, D.R.; et al. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 2017, 4, CD002902. [Google Scholar] [CrossRef]
- Zambrano, J.; Celano, C.M.; Januzzi, J.L.; Massey, C.N.; Chung, W.J.; Millstein, R.A.; Huffman, J. Psychiatric and Psychological Interventions for Depression in Patients With Heart Disease: A Scoping Review. J. Am. Heart Assoc. 2020, 9, e018686. [Google Scholar] [CrossRef] [PubMed]
- Kabboul, N.N.; Tomlinson, G.; Francis, T.A.; Grace, S.L.; Chaves, G.; Rac, V.; Daou-Kabboul, T.; Bielecki, J.M.; Alter, D.A.; Krahn, M. Comparative Effectiveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J. Clin. Med. 2018, 7, 514. [Google Scholar] [CrossRef] [Green Version]
- Roncella, A.; Pristipino, C.; Cianfrocca, C.; Scorza, S.; Pasceri, V.; Pelliccia, F.; Denollet, J.; Pedersen, S.S.; Speciale, G. One-year results of randomized, controlled, short-term psychotherapy in acute myocardial infarction (STEP-IN-AMI) trial. Int. J. Cardiol. 2013, 170, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Pristipino, C.; Roncella, A.; Pasceri, V.; Speciale, G. Short-TErm Psychotherapy IN Acute Myocardial Infarction (STEP-IN-AMI) Trial: Final Results. Am. J. Med. 2019, 132, 639–646. [Google Scholar] [CrossRef]
- Ghadri, J.-R.; Wittstein, I.L.; Prasad, A.; Scott, S.; Dote, K.; Akashi, Y.J.; Camman, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018, 39, 2032–2046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharkey, S.W.; Maron, B.J. Epidemiology and clinical profile of Takotsubo cardiomyopathy. Circ. J. 2014, 78, 2119–2128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurisu, S.; Kihara, Y. Tako-tsubo cardiomyopathy: Clinical presentation and underlying mechanism. J. Cardiol. 2012, 60, 429–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Pace, S.; Parodi, G.; Bellandi, B.; Zampini, L.; Venditti, F.; Ardito, M.; Antoniucci, D.; Gensini, G.F.; Tuscany Registry of Tako-tsubo Cardiomyopathy. Anxiety trait in patients with stress-induced cardiomyopathy: A case-control study. Clin. Res. Cardiol. 2011, 100, 523–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraynak, T.E.; Marsland, A.L.; Gianaros, P.J. Neural Mechanisms Linking Emotion with Cardiovascular Disease. Curr. Cardiol. Rep. 2018, 20, 128. [Google Scholar] [CrossRef]
- Brothers, B.M.; Andersen, B.L. Hopelessness as a predictor of depressive symptoms for breast cancer patients coping with recurrence. Psychooncology 2009, 18, 267–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escalera, C.; Santoyo-Olsson, J.; Stewart, A.L.; Ortiz, C.; Nápoles, A.M. Social support as a moderator in the relationship between intrusive thoughts and anxiety among Spanish-speaking Latinas with breast cancer. Psychooncology 2019, 28, 1819–1828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faye-Schjøll, H.H.; Schou-Bredal, I. Pessimism predicts anxiety and depression in breast cancer survivors: A 5-year follow-up study. Psychooncology 2019, 28, 1314–1320. [Google Scholar] [CrossRef]
- Starreveld, D.E.J.; Markovitz, S.E.; van Breukelen, G.; Peters, M.L. The course of fear of cancer recurrence: Different patterns by age in breast cancer survivors. Psychooncology 2018, 27, 295–301. [Google Scholar] [CrossRef]
- Park, E.M.; Gelber, S.; Rosenberg, S.M.; Seah, D.S.E.; Schapira, L.; Come, S.E.; Partridge, A.H. Anxiety and Depression in Young Women with Metastatic Breast Cancer: A Cross-Sectional Study. Psychosomatics 2018, 59, 251–258. [Google Scholar] [CrossRef]
- Shaw, L.K.; Sherman, K.A.; Fitness, J.; Elder, E. Breast Cancer Network Australia. Factors associated with romantic relationship formation difficulties in women with breast cancer. Psychooncology 2018, 27, 1270–1276. [Google Scholar] [CrossRef]
- Sun, L.; Ang, E.; Ang, W.H.D.; Lopez, V. Losing the breast: A meta-synthesis of the impact in women breast cancer survivors. Psychooncology 2018, 27, 376–385. [Google Scholar] [CrossRef]
- Teo, I.; Reece, G.P.; Huang, S.C.; Mahajan, K.; Andon, J.; Khanal, P.; Sun, C.; Nicklaus, K.; Merchant, F.; Markey, M.K.; et al. Body Image Dissatisfaction in Patients Undergoing Breast Reconstruction: Examining the Roles of Breast Symmetry and Appearance Investment. Psychooncology 2018, 27, 857–863. [Google Scholar] [CrossRef]
- Teo, I.; Reece, G.P.; Christie, I.C.; Guindani, M.; Markey, M.K.; Heinberg, L.J.; Crosby, M.A.; Cororve Fingeret, M. Body Image and Quality of Life of Breast Cancer Patients: Influence of Timing and Stage of Breast Reconstruction. Psychooncology 2016, 25, 1106–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slatman, J. The Meaning of Body Experience Evaluation in Oncology. Health Care Anal. 2011, 19, 295–311. [Google Scholar] [CrossRef] [Green Version]
- Meneghetti, A. L’Immagine e l’Inconscio, 1994–2003; Ontopsicologia Editrice: Roma, Italy, 2003. [Google Scholar]
- Roncella, A.; Scorza, S. Projective Tests: The Six-Drawings Test in Ischemic Heart Disease. In Psychotherapy for Ischemic Heart Disease; Roncella, A., Pristipino, C., Eds.; Springer: Cham, Switzerland, 2016; Chapter 15; p. 215. [Google Scholar] [CrossRef]
- Meneghetti, A. Ontopsychology Handbook, 1995–2008; Ontopsicologia Editrice: Roma, Italy, 2008. [Google Scholar]
- Beck, A.T.; Ward, C.H.; Meldelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beck, A.T.; Kovacs, M.; Weissman, A. Assessment of suicidal intention: The scale for suicide ideation. J. Consult. Clin. Psychol. 1979, 47, 343–352. [Google Scholar] [CrossRef]
- Hofer, S.; Lim, L.L.; Guyatt, G.H.; Oldridge, N.B. The MacNew heart disease health related quality of life instrument: A summary. Health Qual. Life Outcomes 2004, 8, 2–3. [Google Scholar] [CrossRef] [Green Version]
- Roncella, A. Short-Term Psychotherapy in Patients with Acute Myocardial Infarction. In Psychotherapy for Ischemic Heart Disease; Roncella, A., Pristipino, C., Eds.; Springer: Cham, Switzerland, 2016; Chapter 13; p. 187. [Google Scholar] [CrossRef]
- Sollazzo, R.; Sanges, M. The Second Brain and Possible Interactions with the Heart. In Psychotherapy for Ischemic Heart Disease; Roncella, A., Pristipino, C., Eds.; Springer: Cham, Switzerland, 2016; Chapter 4; p. 59. [Google Scholar] [CrossRef]
- Roger, V.L.; Killian, J.M.; Weston, S.A.; Roger, V.L.; Killian, J.M.; Weston, S.A.; Jaffe, A.S.; Kors, J.; Santrach, P.J.; Tunstall-Pedoe, H.; et al. Redefinition of myocardial infarction. Circulation 2006, 114, 790–797. [Google Scholar] [CrossRef] [Green Version]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef]
- Templin, C.; Ghadri, J.R.; Diekmann, J.; Napp, L.C.; Bataiosu, D.R.; Jaguszewski, M.; Cammann, V.L.; Sarcon, A.; Geyer, V.; Neumann, C.A.; et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N. Engl. J. Med. 2015, 373, 929–938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghadri, J.-R.; Wittstein, I.S.; Prasad, A.; Sharkey, S.; Dote, K.; Akashi, Y.J.; Cammann, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Cardiomyopathy. N. Engl. J. Med. 2015, 373, 929–938. [Google Scholar] [CrossRef] [Green Version]
- Napp, L.C.; Cammann, V.L.; Jaguszewski, M.; Szawan, K.A.; Wischnewsky, M.; Gili, S.; Knorr, M.; Heiner, S.; Citro, R.; Bossone, E.; et al. Coexistence and outcome of coronary artery disease in Takotsubo syndrome. Eur. Heart J. 2020, 41, 3255–3268. [Google Scholar] [CrossRef] [PubMed]
- Maslow, A.H. Toward a Psychology of Being; Van Nostrand Company Inc.: New York, NY, USA, 1962. [Google Scholar]
- Black, P.H. The inflammatory response is an integral part of the stress response. Brain Behav. Immun. 2003, 17, 350–364. [Google Scholar] [CrossRef]
- Besedovsky, H.O.; Del Rey, A. Psychoneuroimmunology, 3rd ed.; Ader, R., Felten, D., Cohen, N., Eds.; Academic Press: Amsterdam, The Netherlands, 2001. [Google Scholar]
- Huh, J.R.; Veiga-Fernandes, H. Neuroimmune circuits in inter-organ communication. Nat. Rev. Immunol. 2020, 20, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Meneghetti, A. Campo Semantico, 1988–2012; Ontopsicologia Editrice: Roma, Italy, 2012. [Google Scholar]
- Meneghetti, A. Prontuario Onirico, 1981–2012; Ontopsicologia Editrice: Roma, Italy, 2012. [Google Scholar]
- Pignalberi, C.; Patti, G.; Chimenti, C.; Maseri, A. Role of different determinants of psychological distress in acute coronary syndromes. J. Am. Coll. Cardiol. 1998, 32, 613–619. [Google Scholar] [CrossRef] [Green Version]
- Choen, S.; Syme, S.L. Social Support and Health; Orlando University: Orlando, FL, USA, 1985. [Google Scholar]
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologist Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Spielberger, C.D. Manual for the State-Trait Anger Expression Inventory (STAXI); Psychological Assessment Resources: Odessa, Ukraine, 1988. [Google Scholar] [CrossRef]
- Aaranson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trial in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Sprangers, M.A.; Groenvold, M.; Arraras, J.I.; Franklin, J.; te Velde, A.; Muller, M.; Franzini, L.; Williams, A.; de Haes, H.C.; Hopwood, P.; et al. The European Organization for Research and Treatment of Cancer breast cancer specific quality of life questionnaire module: First results from a three-country field study. J. Clin. Oncol. 1996, 14, 2756–2768. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36) 1: Conceptual frameworkand item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Jenkinson, C.; Coulter, A.; Wright, L. Short form 36 (SF 36) health survey questionnaire: Normative data for adults of working age. BMJ 1993, 306, 1437–1440. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-36 Physical and Mental Summary Scales: A User’s Manual; The Health Institute: Boston, MA, USA; New England Medical Center: Boston, MA, USA, 1994. [Google Scholar]
- Khatcheressian, J.L.; Hurley, P.; Bantug, E.; Esserman, L.J.; Grunfeld, E.; Halberg, F.; Hantel, A.; Henry, N.L.; Muss, H.B.; Smith, T.J.; et al. Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2013, 31, 961–965. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roncella, A.; Pristipino, C.; Di Carlo, O.; Ansuini, M.; Corbosiero, A.; Di Fusco, S.A.; Palumbo, G.; Gigantesco, A.; Mirabella, F.; De Angelis, R.; et al. PSYChosomatic Medicine in ONcologIc and Cardiac Disease (PSYCHONIC) Study—A Retrospective and Prospective Observational Research Protocol. J. Clin. Med. 2021, 10, 5786. https://doi.org/10.3390/jcm10245786
Roncella A, Pristipino C, Di Carlo O, Ansuini M, Corbosiero A, Di Fusco SA, Palumbo G, Gigantesco A, Mirabella F, De Angelis R, et al. PSYChosomatic Medicine in ONcologIc and Cardiac Disease (PSYCHONIC) Study—A Retrospective and Prospective Observational Research Protocol. Journal of Clinical Medicine. 2021; 10(24):5786. https://doi.org/10.3390/jcm10245786
Chicago/Turabian StyleRoncella, Adriana, Christian Pristipino, Oretta Di Carlo, Matteo Ansuini, Angela Corbosiero, Stefania Angela Di Fusco, Gabriella Palumbo, Antonella Gigantesco, Fiorino Mirabella, Rosanna De Angelis, and et al. 2021. "PSYChosomatic Medicine in ONcologIc and Cardiac Disease (PSYCHONIC) Study—A Retrospective and Prospective Observational Research Protocol" Journal of Clinical Medicine 10, no. 24: 5786. https://doi.org/10.3390/jcm10245786
APA StyleRoncella, A., Pristipino, C., Di Carlo, O., Ansuini, M., Corbosiero, A., Di Fusco, S. A., Palumbo, G., Gigantesco, A., Mirabella, F., De Angelis, R., Pasceri, V., Cancellara, L., Colivicchi, F., Allan, R., Mirri, M. A., & Speciale, G. (2021). PSYChosomatic Medicine in ONcologIc and Cardiac Disease (PSYCHONIC) Study—A Retrospective and Prospective Observational Research Protocol. Journal of Clinical Medicine, 10(24), 5786. https://doi.org/10.3390/jcm10245786






