Developing Pulmonary Rehabilitation for COVID-19: Are We Linked with the Present Literature? A Lexical and Geographical Evaluation Study Based on the Graph Theory
Abstract
:1. Introduction
2. Literature Evaluation
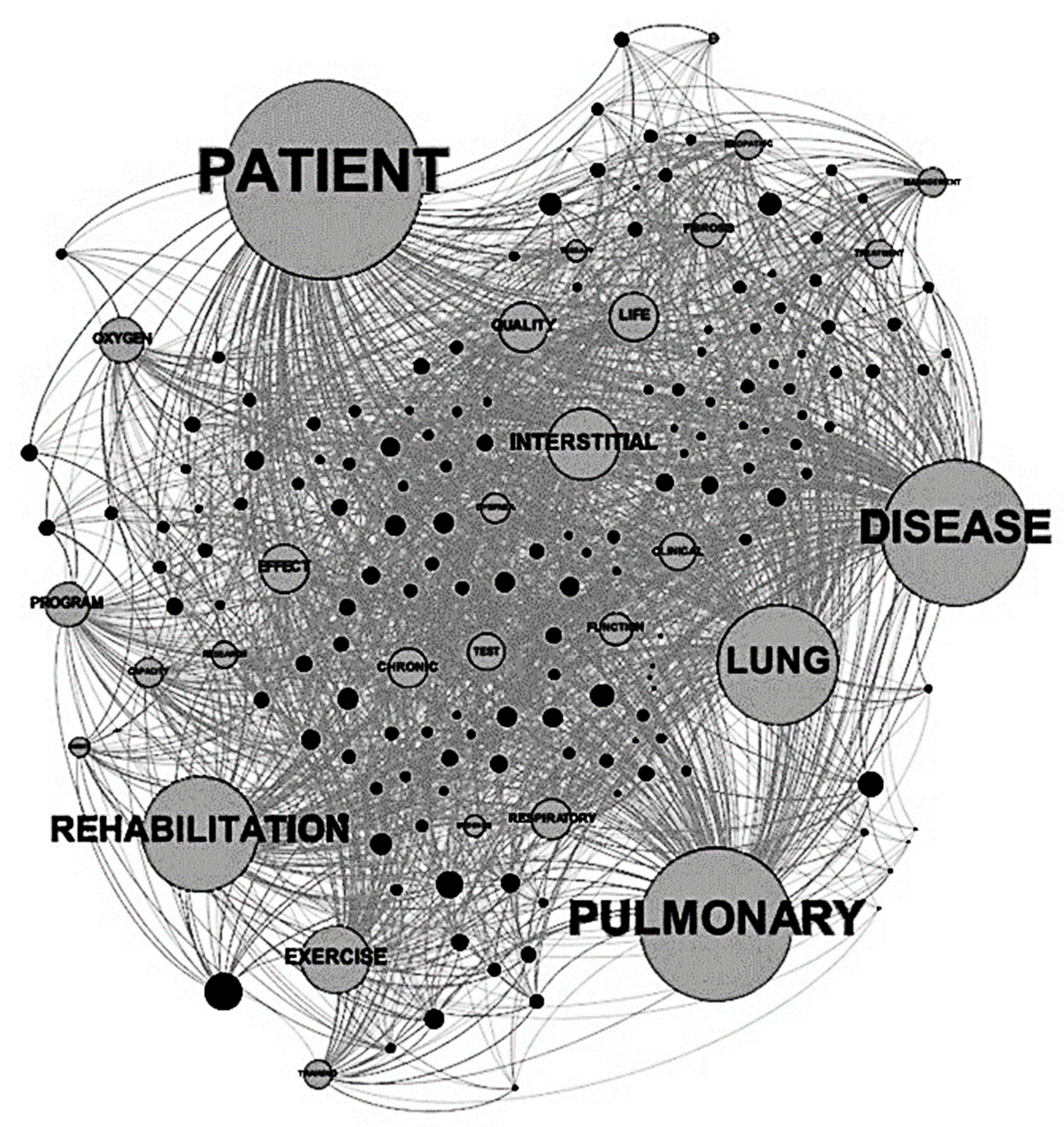
2.1. Lexicon Analysis
2.2. Geographical Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- McCloskey, B.; Zumla, A.; Ippolito, G.; Blumberg, L.; Arbon, P.; Cicero, A.; Endericks, T.; Lim, P.L.; Borodina, M. Mass gathering events and reducing further global spread of COVID-19: A political and public health dilemma. Lancet 2020, 395, 1096–1099. [Google Scholar] [CrossRef]
- Chilamakuri, R.; Agarwal, S. COVID-19: Characteristics and Therapeutics. Cells 2021, 10, 206. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Zha, L.; Xu, X.; Wang, D.; Qiao, G.; Zhuang, W.; Huang, S. Modified rehabilitation exercises for mild cases of COVID-19. Ann. Palliat. Med. 2020, 9, 3100–3106. [Google Scholar] [CrossRef]
- Vitacca, M. Will the COVID tsunami be able to impose tele-rehabilitation as a system opportunity? Pulmonology 2020, 26, 338–339. [Google Scholar] [CrossRef]
- Wang, T.J.; Chau, B.; Lui, M.; Lam, G.; Lin, N.; Humbert, S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am. J. Phys. Med. Rehab. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Dixit, S.; Borghi-Silva, A.; Bairapareddy, K.C. Revisiting pulmonary rehabilitation during COVID-19 pandemic: A narrative review. Rev. Cardiovasc. Med. 2021, 22, 315–327. [Google Scholar] [CrossRef]
- Barker-Davies, R.M.; O’Sullivan, O.; Senaratne, K.P.P.; Baker, P.; Cranley, M.; Dharm-Datta, S.; Ellis, H.; Goodall, D.; Gough, M.; Lewis, S.; et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br. J. Sports Med. 2020, 54, 949–959. [Google Scholar] [CrossRef]
- Schmidt, K.; Gensichen, J.; Gehrke-Beck, S.; Kosilek, R.P.; Kühne, F.; Heintze, C.; Baldwin, L.M.; Needham, D.M. Management of COVID-19 ICU-survivors in primary care: A narrative review. BMC Fam Pract. 2021, 22, 160. [Google Scholar] [CrossRef]
- Onder, G.; Giovannini, S.; Sganga, F.; Manes-Gravina, E.; Topinkova, E.; Finne-Soveri, H.; Garms-Homolová, V.; Declercq, A.; van der Roest, H.G.; Jónsson, P.V.; et al. Interactions between drugs and geriatric syndromes in nursing home and home care: Results from Shelter and IBenC projects. Aging Clin. Exp. Res. 2018, 30, 1015–1021. [Google Scholar] [CrossRef]
- Spruit, M.A.; Holland, A.E.; Singh, S.J.; Tonia, T.; Wilson, K.C.; Troosters, T. COVID-19: Interim Guidance on Rehabilitation in the Hospital and Post-Hospital Phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force. Eur. Respir. J. 2020, 56, 2002197. [Google Scholar] [CrossRef]
- Puhan, M.A.; Gimeno-Santos, E.; Cates, C.J.; Troosters, T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2016, 12, CD005305. [Google Scholar] [CrossRef]
- Wedzicha, J.A.; Miravitlles, M.; Hurst, J.R. Management of COPD exacerbations: A European Respiratory Society/American Thoracic Society guideline. Eur. Respir. J. 2017, 49, 1600791. [Google Scholar] [CrossRef] [Green Version]
- Alison, J.A.; McKeough, Z.J.; Johnston, K.; McNamara, R.J.; Spencer, L.M.; Jenkins, S.C.; Hill, C.J.; McDonald, V.M.; Frith, P.; Cafarella, P.; et al. Australian and New Zealand Pulmonary Rehabilitation Guidelines. Respirology 2017, 22, 800–819. [Google Scholar] [CrossRef] [Green Version]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]
- Coraci, D.; Giovannini, S.; Loreti, C.; Fusco, A.; Padua, L. Management of neuropathic pain: A graph theory-based presentation of literature review. Breast J. 2020, 26, 581–582. [Google Scholar] [CrossRef]
- Coraci, D.; Giovannini, S.; Fusco, A.; Loreti, C.; Padua, L. Low Back Pain: Literature Review Based on Graph Theory. Pain Pract. 2020, 20, 946–947. [Google Scholar] [CrossRef]
- Coraci, D.; Loreti, C.; Fusco, A.; Giovannini, S.; Padua, L. Peripheral Neuropathies Seen by Ultrasound: A Literature Analysis through Lexical Evaluation, Geographical Assessment and Graph Theory. Brain Sci. 2021, 11, 113. [Google Scholar] [CrossRef]
- Pachayappan, M.; Venkatesakumar, R. A graph theory based systematic literature network analysis. Theor. Econ. Lett. 2018, 8, 960–980. [Google Scholar] [CrossRef] [Green Version]
- Brunson, J.C.; Laubenbacher, R.C. Applications of network analysis to routinely collected health care data: A systematic review. J. Am. Med. Inform. Assoc. 2018, 25, 210–221. [Google Scholar] [CrossRef]
- Wijsenbeek, M.; Cottin, V. Spectrum of fibrotic lung diseases. N. Engl. J. Med. 2020, 383, 958–968. [Google Scholar] [CrossRef]
- Podolanczuk, A.J.; Richeldi, L. COVID-19 and Interstitial Lung Disease: Keep Them Separate. Am. J. Respir. Crit. Care Med. 2020, 202, 1614–1616. [Google Scholar] [CrossRef]
- Heiden, S. The TXM platform: Building open-source textual analysis software compatible with the TEI encoding scheme. In Proceedings of the 24th Pacific Asia Conference on Language, Information and Computation, Sendai, Japan, 4–7 November 2010; pp. 389–398. [Google Scholar]
- Bastian, M.; Heymann, S.; Jacomy, M. Gephi: An open source software for exploring and manipulating networks. In Proceedings of the International AAAI Conference on Weblogs and Social Media, San Jose, CA, USA, 17–20 May 2009; pp. 361–362. [Google Scholar]
- Zhang, W.; Chien, J.; Yong, J.; Kuang, R. Network-based machine learning and graph theory algorithms for precision oncology. NPJ Precis. Oncol. 2017, 1, 25. [Google Scholar] [CrossRef] [Green Version]
- Xu, Y.; Yu, P.; Zheng, J.; Wang, C.; Hu, T.; Yang, Q.; Xu, Z.; Guo, F.; Tang, X.; Ren, F.; et al. Classifying Vulnerability to Sleep Deprivation Using Resting-State Functional MRI Graph Theory Metrics. Front. Neurosci. 2021, 15, 660365. [Google Scholar] [CrossRef]
- Mirakhorli, J.; Amindavar, H.; Mirakhorli, M. A new method to predict anomaly in brain network based on graph deep learning. Rev. Neurosci. 2020, 31, 681–689. [Google Scholar] [CrossRef]
- Yeh, C.H.; Jones, D.K.; Liang, X.; Descoteaux, M.; Connelly, A. Mapping Structural Connectivity Using Diffusion MRI: Challenges and Opportunities. J. Magn. Reson. Imaging 2021, 53, 1666–1682. [Google Scholar] [CrossRef]
- Ries, A.L.; Bauldoff, G.S.; Carlin, B.W.; Casaburi, R.; Emery, C.F.; Mahler, D.A.; Make, B.; Rochester, C.L.; ZuWallack, R.; Herrerias, C. Pulmonary rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007, 131, 4S–42S. [Google Scholar] [CrossRef]
- Gutenbrunner, C.; Meyer, T.; Melvin, J.; Stucki, G. Towards a conceptual description of Physical and Rehabilitation medicine. J. Rehabil. Med. 2011, 43, 760–764. [Google Scholar] [CrossRef] [Green Version]
- Lage, S.M.; Jácome, C.; Oliveira, A.; Araújo, A.G.; Pereira, D.A.G.; Parreira, V.F. Validation of the International Classification of Functioning, Disability and Health Core Set for obstructive pulmonary diseases in the perspective of adults with asthma. Disabil. Rehabil. 2020, 42, 86–92. [Google Scholar] [CrossRef]
- Sun, J.; Liu, J.; Li, H.; Shang, C.; Li, T.; Ji, W.; Wu, J.; Han, X.; Shi, Z. Pulmonary rehabilitation focusing on the regulation of respiratory movement can improve prognosis of severe patients with COVID-19. Ann. Palliat. Med. 2021, 10, 4262–4272. [Google Scholar] [CrossRef]
- Rees, E.M.; Nightingale, E.S.; Jafari, Y.; Waterlow, N.R.; Clifford, S.; Pearson, C.A.B.; Cmmid Working Group; Jombart, T.; Procter, S.R.; Knight, G.M. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020, 18, 270. [Google Scholar] [CrossRef]
- Leclerc, Q.J.; Fuller, N.M.; Keogh, R.H.; Diaz-Ordaz, K.; Sekula, R.; Semple, M.G.; ISARIC4C Investigators; CMMID COVID-19 Working Group; Atkins, K.E.; Procter, S.R.; et al. Importance of patient bed pathways and length of stay differences in predicting COVID-19 hospital bed occupancy in England. BMC Health Serv. Res. 2021, 21, 566. [Google Scholar] [CrossRef] [PubMed]
- Vekaria, B.; Overton, C.; Wiśniowski, A.; Ahmad, S.; Aparicio-Castro, A.; Curran-Sebastian, J.; Eddleston, J.; Hanley, N.A.; House, T.; Kim, J.; et al. Hospital length of stay for COVID-19 patients: Data-driven methods for forward planning. BMC Infect. Dis. 2021, 21, 700. [Google Scholar] [CrossRef] [PubMed]
- Greening, N.J.; Williams, J.E.; Hussain, S.F.; Harvey-Dunstan, T.C.; Bankart, M.J.; Chaplin, E.J.; Vincent, E.E.; Chimera, R.; Morgan, M.D.; Singh, S.J.; et al. An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: Randomised controlled trial. BMJ 2014, 349, g4315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coraci, D.; Fusco, A.; Frizziero, A.; Giovannini, S.; Biscotti, L.; Padua, L. Global approaches for global challenges: The possible support of rehabilitation in the management of COVID-19. J. Med. Virol. 2020, 92, 1739–1740. [Google Scholar] [CrossRef] [Green Version]
- Giovannini, S.; Tamburrano, A.; Sganga, F.; Serra, M.L.; Loreti, C.; Coraci, D.; Padua, L.; Caliandro, P.; Zega, M.; Tafani, A.; et al. A new model of multidimensional discharge planning: Continuity of care for frail and complex inpatients. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 13009–13014. [Google Scholar] [CrossRef]
- Castelli, L.; Loreti, C.; Coraci, D.; Fusco, A.; Biscotti, L.; Giovannini, S.; Padua, L. Deprescribing in older adults during COVID-19 pandemic, opportunity or risk? Res. Soc. Adm. Pharm. 2021, 17, 1024–1025. [Google Scholar] [CrossRef]
- Wallaert, B.; Duthoit, L.; Drumez, E.; Behal, H.; Wemeau, L.; Chenivesse, C.; Grosbois, J.-M. Long-term evaluation of home-based pulmonary rehabilitation in patients with fibrotic idiopathic interstitial pneumonias. ERJ Open Res. 2019, 5, 00045–02019. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, S.; van der Roest, H.G.; Carfì, A.; Finne-Soveri, H.; Garms-Homolová, V.; Declercq, A.; Jónsson, P.V.; van Hout, H.; Vetrano, D.L.; Gravina, E.M.; et al. Polypharmacy in Home Care in Europe: Cross-Sectional Data from the IBenC Study. Drugs Aging 2018, 35, 145–152. [Google Scholar] [CrossRef]
- Chen, Y.Z.; Huang, S.T.; Wen, Y.W.; Chen, L.K.; Hsiao, F.Y. Combined effects of frailty and polypharmacy on health outcomes in older adults: Frailty outweighs polypharmacy. J. Am. Med. Dir. Assoc. 2021, 22, 606.e7–606.e18. [Google Scholar] [CrossRef] [PubMed]
- Jesus, T.S.; Bright, F.A.; Pinho, C.S.; Papadimitriou, C.; Kayes, N.M.; Cott, C.A. Scoping review of the person-centered literature in adult physical rehabilitation. Disabil. Rehabil. 2021, 43, 1626–1636. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fusco, A.; Padua, L.; Coraci, D.; Loreti, C.; Castelli, L.; Costantino, C.; Frizziero, A.; Serafini, E.; Biscotti, L.; Bernabei, R.; et al. Developing Pulmonary Rehabilitation for COVID-19: Are We Linked with the Present Literature? A Lexical and Geographical Evaluation Study Based on the Graph Theory. J. Clin. Med. 2021, 10, 5763. https://doi.org/10.3390/jcm10245763
Fusco A, Padua L, Coraci D, Loreti C, Castelli L, Costantino C, Frizziero A, Serafini E, Biscotti L, Bernabei R, et al. Developing Pulmonary Rehabilitation for COVID-19: Are We Linked with the Present Literature? A Lexical and Geographical Evaluation Study Based on the Graph Theory. Journal of Clinical Medicine. 2021; 10(24):5763. https://doi.org/10.3390/jcm10245763
Chicago/Turabian StyleFusco, Augusto, Luca Padua, Daniele Coraci, Claudia Loreti, Letizia Castelli, Cosimo Costantino, Antonio Frizziero, Elisabetta Serafini, Lorenzo Biscotti, Roberto Bernabei, and et al. 2021. "Developing Pulmonary Rehabilitation for COVID-19: Are We Linked with the Present Literature? A Lexical and Geographical Evaluation Study Based on the Graph Theory" Journal of Clinical Medicine 10, no. 24: 5763. https://doi.org/10.3390/jcm10245763
APA StyleFusco, A., Padua, L., Coraci, D., Loreti, C., Castelli, L., Costantino, C., Frizziero, A., Serafini, E., Biscotti, L., Bernabei, R., & Giovannini, S. (2021). Developing Pulmonary Rehabilitation for COVID-19: Are We Linked with the Present Literature? A Lexical and Geographical Evaluation Study Based on the Graph Theory. Journal of Clinical Medicine, 10(24), 5763. https://doi.org/10.3390/jcm10245763










