Comparison of Treatment Goals between Users of Biological and Non-Biological Therapies for Treatment of Psoriasis in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Study Survey
2.4. Statistical Analysis
3. Results
3.1. Variable Selection
3.2. Study Population
Results by Biologic vs. Non-Biologic Users
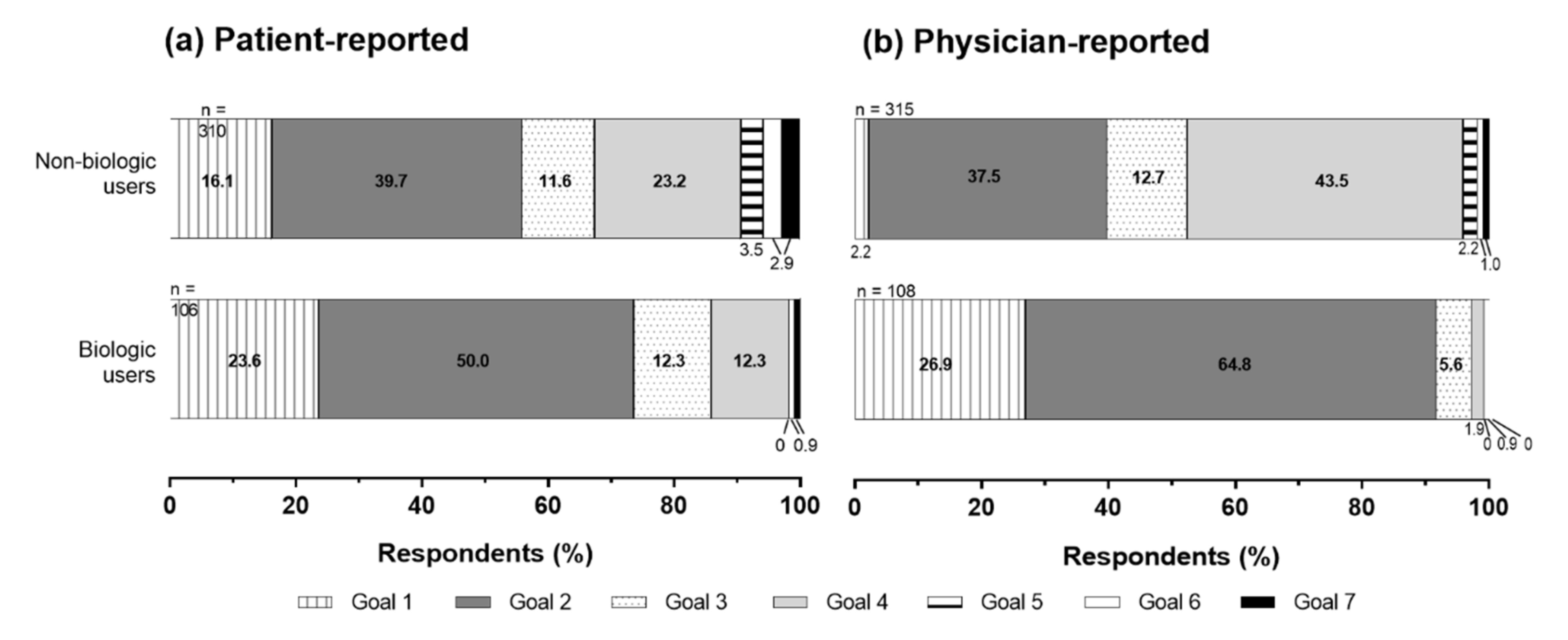
3.3. Treatment Goals by Biologic vs. Non-Biologic Users
3.4. Factors Associated with Treatment Goals by Biologic vs. Non-Biologic Users
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A. List of Participating Institutions
- Department of Dermatology, Asahikawa Medical University
- Department of Dermatology, Jichi Medical University
- Department of Dermatology, Tokyo Women’s Medical University
- Department of Dermatology, School of Medicine, Teikyo University
- Department of Dermatology, Tokyo Medical University
- Department of Dermatology, School of Medicine, Tokai University
- Department of Dermatology, Graduate School of Medicine, Gifu University
- Graduate School of Medical Sciences, Nagoya City University
- Department of Dermatology, School of Medicine, Kindai University
- Department of Dermatology, Graduate School of Medicine, Osaka City University
- Department of Dermatology, Kawasaki Medical School
- Department of Dermatology, Faculty of Medicine, Fukuoka University
- Department of Dermatology, Tokyo Teishin Hospital
- Department of Dermatology, St Luke’s International Hospital
- Department of Dermatology, Yokohama Chuo Hospital
- Public Interest Incorporated Foundation Jiai-kai, Branch of Imamura Hospital
- Department of Dermatology, Ina Central Hospital
- Department of Dermatology, Iida Municipal Hospital
- Department of Dermatology, Osaka Kaisei Hospital
- Medical Corporation Kojin-kai, Sapporo Dermatology Clinic
- Medical Corporation Kojin-kai, Fukuzumi Dermatology Clinic
- Kobayashi Skin Clinic
- Department of Dermatology, EST Clinic
- Sugawara Dermatology Clinic
- Medical Corporation Subaru-kai, Sugai Dermatology Park Side Clinic
- Hattori Dermatology Clinic
- Medical Corporation Koten-kai, Iidabashi Clinic
- Medical Corporation Shohei-kai, Niki Dermatology Clinic
- Clinic of Dermatology, Ningyocho
- Dr. Mariko Skin & Dermatology Clinic
- Tsujimoto Skincare Clinic
- Shirosaki Dermatology & Neurology Clinic
- Kato Dermatology
- Hou Dermatology
- Machino Skin Clinique
- Yasumoto Dermatology Clinic
- Takagi Dermatology Clinic
- Fushimi Skin Clinic
- Omorimachi Dermatology
- Hayashibe Derma Clinic
- Hasegawa Dermatology Clinic
- Medical Corporation Kojin-kai, Ario Sapporo Dermatology Clinic
- Atago Dermatology
- Medical Corporation Shotoku-kai, Hino Clinic
- Nomura Dermatology Clinic
- Zoshiki Dermatology Clinic
- Nakatsu Dermatology Clinic
- Saruwatari Dermatology Clinic
- Kusuhara Dermatology Clinic
- Medical Corporation Shimizu Dermatology Clinic
- Kokubu Clinic, Abashiri Dermatology Clinic
- Nishide Skin Clinic
- Kazama Skin Clinic
- Shimizu Skin Clinic
References
- Kubota, K.; Kamijima, Y.; Sato, T.; Ooba, N.; Koide, D.; Iizuka, H.; Nakagawa, H. Epidemiology of psoriasis and palmoplantar pustulosis: A nationwide study using the Japanese national claims database. BMJ Open 2015, 5, e006450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, T.; Takahashi, H.; Kawada, A.; Iizuka, H.; Nakagawa, H. Epidemiological survey from 2009 to 2012 of psoriatic patients in Japanese Society for Psoriasis Research. J. Dermatol. 2018, 45, 293–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirabe, M.; Hasegawa, T.; Fujishiro, Y.; Kigawa, M.; Fukuchi, O.; Nakagawa, H. Factors associated with quality of life among patients with psoriasis. Comparison between psoriasis-specific QOL measures and generic QOL measures. Nihon Koshu Eisei Zasshi 2008, 55, 65–74. [Google Scholar]
- Mabuchi, T.; Yamaoka, H.; Kojima, T.; Ikoma, N.; Akasaka, E.; Ozawa, A. Psoriasis affects patient’s quality of life more seriously in female than in male in Japan. Tokai J. Exp. Clin. Med. 2012, 37, 84–88. [Google Scholar] [PubMed]
- Okubo, Y.; Arai, K.; Fujiwara, S.; Amaya, M.; Tsuboi, R. Assessment of the quality of life of patients with psoriasis using Skindex-16 and GHQ-28. Jpn. J. Dermatol. 2007, 117, 2495–2505. [Google Scholar]
- Okubo, Y.; Natsume, S.; Usui, K.; Amaya, M.; Tsuboi, R. Low-dose, short-term ciclosporin (Neoral®) therapy is effective in improving patients’ quality of life as assessed by Skindex-16 and GHQ-28 in mild to severe psoriasis patients. J. Dermatol. 2010, 38, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Florek, A.G.; Wang, C.J.; Armstrong, A.W. Treatment preferences and treatment satisfaction among psoriasis patients: A systematic review. Arch. Dermatol. Res. 2018, 310, 271–319. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.W.; Betts, K.A.; Signorovitch, J.E.; Sundaram, M.; Li, J.; Ganguli, A.X.; Wu, E.Q. Number needed to treat and costs per responder among biologic treatments for moderate-to-severe psoriasis: A network meta-analysis. Curr. Med. Res. Opin. 2018, 34, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Ohtsuki, M.; Terui, T.; Ozawa, A.; Morita, A.; Sano, S.; Takahashi, H.; Komine, M.; Etoh, T.; Igarashi, A.; Torii, H.; et al. Japanese guidance for use of biologics for psoriasis (the 2013 version). J. Dermatol. 2013, 40, 683–695. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.W.; Siegel, M.P.; Bagel, J.; Boh, E.E.; Buell, M.; Cooper, K.D.; Duffin, K.C.; Eichenfield, L.F.; Garg, A.; Gelfand, J.M.; et al. From the Medical Board of the National Psoriasis Foundation: Treatment targets for plaque psoriasis. J. Am. Acad. Dermatol. 2017, 76, 290–298. [Google Scholar] [CrossRef] [Green Version]
- Mrowietz, U.; Kragballe, K.; Reich, K.; Spuls, P.; Griffiths, C.E.M.; Nast, A.; Franke, J.; Antoniou, C.; Arenberger, P.; Balieva, F.; et al. Definition of treatment goals for moderate to severe psoriasis: A European consensus. Arch. Dermatol. Res. 2011, 303, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radtke, M.A.; Reich, K.; Spehr, C.; Augustin, M. Treatment goals in psoriasis routine care. Arch. Dermatol. Res. 2015, 307, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Brezinski, E.A.; Armstrong, A.W. Strategies to maximize treatment success in moderate to severe psoriasis: Establishing treatment goals and tailoring of biologic therapies. Semin. Cutan. Med. Surg. 2014, 33, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Okubo, Y.; Tsuruta, D.; Tang, A.C.; Inoue, S.; Torisu-Itakura, H.; Hanada, T.; Ohtsuki, M. Analysis of treatment goal alignment between Japanese psoriasis patients and their paired treating physicians. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 606–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Education, Culture, Sports, Science and Technology. Ethical Guidelines Concerning Medical Studies in Human Subjects. 2015. Available online: http://www.lifescience.mext.go.jp/files/pdf/n1500_02.pdf (accessed on 18 April 2018).
- Atkinson, M.J.; Sinha, A.; Hass, S.L.; Colman, S.S.; Kumar, R.N.; Brod, M.; Rowland, C.R. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual. Life Outcomes 2004, 2, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finlay, A.Y.; Khan, G.K. Dermatology Life Quality Index (DLQI)—A simple practical measure for routine clinical use. Clin. Exp. Dermatol. 1994, 19, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Kimball, A.B.; Naegeli, A.N.; Edson-Heredia, E.; Lin, C.Y.; Gaich, C.; Nikaï, E.; Wyrwich, K.; Yosipovitch, G. Psychometric properties of the Itch Numeric Rating Scale in patients with moderate-to-severe plaque psoriasis. Br. J. Dermatol. 2016, 175, 157–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finlay, A.Y. Current severe psoriasis and the rule of tens. Br. J. Dermatol. 2005, 152, 861–867. [Google Scholar] [CrossRef]
- Okubo, Y. Hands-on practice manual-illustrations & visual- 46: Plaque psoriasis. Clin. Derma. 2011, 13, 3–6. Available online: http://www.tokyo-med.ac.jp/derma/content/files/topics_okubo_2011clinicalderma.pdf (accessed on 17 June 2018). (In Japanese).
- European Medicines Agency (EMEA); Committee for Medicinal Products for Human Use (CHMP). Guideline on Clinical Investigation of Medicinal Products Indicated for the Treatment of Psoriasis. 2004. Available online: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003329.pdf (accessed on 19 April 2018).
- Lambert, J.; Ghislain, P.D.; Lambert, J.; Cauwe, B.; Van den Enden, M. Treatment patterns in moderate-to-severe plaque psoriasis: Results from a Belgian cross-sectional study (DISCOVER). J. Dermatol. Treat. 2017, 28, 394–400. [Google Scholar] [CrossRef]
- Ichiyama, S.; Ito, M.; Funasaka, Y.; Abe, M.; Nishida, E.; Muramatsu, S.; Nishihara, H.; Kato, H.; Morita, A.; Imafuku, S.; et al. Assessment of medication adherence and treatment satisfaction in Japanese patients with psoriasis of various severities. J. Dermatol. 2018, 45, 727–731. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, K.; Oiso, N.; Kawada, A.; Ohtsuki, M. Epidemiological survey of the psoriasis patients in the Japanese Society for Psoriasis Research from 2013 to 2018. J. Dermatol. 2021, 48, 864–875. [Google Scholar] [CrossRef] [PubMed]
- Strohal, R.; Prinz, J.C.; Girolomoni, G.; Nast, A. A patient-centred approach to biological treatment decision making for psoriasis: An expert consensus. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2390–2398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okubo, Y.; Torisu-Itakura, H.; Hanada, T.; Aranishi, T.; Inoue, S.; Ohtsuki, M. Evaluation of treatment satisfaction misalignment between Japanese psoriasis patients and their physicians—Japanese psoriasis patients and their physicians do not share the same treatment satisfaction levels. Curr. Med. Res. Opin. 2021. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
| Variable | Value (n = 414) 5 |
|---|---|
| Male, % | 74.9% |
| Age (range), y | 56.2 ± 13.9 (20.0–93.0) |
| BMI (range), kg/m2 | 24.3 ± 4.6 (16.0–54.9) |
| Age at disease onset (range), y | 37.2 ± 16.2 (0.0–81.0) |
| Age at disease diagnosis (range), y | 40.0 ± 16.2 (4.0–81.0) |
| Disease duration from onset (range), y | 18.8 ± 11.7 (0.0–65.0) |
| Body part affected (top 3 nominated) | |
| Lower limbs | 78.0% |
| Head | 70.8% |
| Back | 67.1% |
| Body surface area affected 1 | |
| <1% | 24.4% |
| 1–2% | 22.0% |
| 3–10% | 37.0% |
| >10% | 16.5% |
| Current treatment received 2 | |
| Topical | 82.4% |
| Oral | 53.6% |
| Ultraviolet light | 19.1% |
| Biologic | 25.6% |
| Other | 1.4% |
| Treatment Satisfaction 3 | 6.75 ± 2.27 |
| PtGA disease severity 4 | 2.54 ± 1.26 |
| Variable | Value 5 (n = 70) |
|---|---|
| Male, % | 64.3% |
| Age (range), y | 50.6 ± 11.7 (30.0–80.0) |
| Specialty 1 Psoriasis Allergy Other | 69.6% 40.6% 41.8% |
| Treatment experience with psoriasis 2 <2 y 2 ≤ 4 y 4 ≤ 6 y 6 ≤ 8 y 8 ≤ 10 y ≥10 y | 0.0% 2.9% 5.9% 4.4% 0.0% 86.8% |
| Number of patients seen per month 2 <5 5–9 10–14 15–19 ≥20 | 1.5% 5.9% 10.3% 7.4% 75.0% |
| Treatment Satisfaction 3 | 6.46 ± 2.08 |
| PGA disease severity 4 | 2.51 ± 1.15 |
| Characteristic 1 | Biologic Users | Non-Biologic Users | p 2 |
|---|---|---|---|
| Patient-reported | n 1 = 104 | n 1 = 292 | |
| Patient age, y | 56.3 ± 15.1 | 55.9 ± 13.4 | 0.807 |
| Lesion site, back, n (%) | 54 (51.9) | 211 (72.3) | <0.001 |
| TSQM score (global satisfaction) | 68.6 ± 19.6 | 57.3 ± 17.1 | <0.001 |
| DLQI | |||
| DLQI total score | 3.2 ± 5.0 | 5.0 ± 5.3 | <0.001 |
| Daily activities | 0.5 ± 1.3 | 1.0 ± 1.5 | <0.001 |
| Leisure | 0.5 ± 1.1 | 0.7 ± 1.3 | 0.044 |
| Personal relationships | 0.2 ± 0.9 | 0.4 ± 1.1 | 0.028 |
| Physician-reported | n 2 = 107 | n 2 = 309 | |
| Patient age, y | 56.9 ± 15.2 | 56.4 ± 13.8 | 0.709 |
| Location of lesion (upper limb), n (%) | 42 (39.3) | 229 (74.1) | <0.001 |
| Physician’s specialty—psoriasis, n (%) | 99 (92.5) | 231 (75) | <0.001 |
| Physician’s workplace, n (%) | <0.001 | ||
| Clinic | 35 (32.7) | 202 (65.4) | |
| University hospital | 47 (43.9) | 81 (26.2) | |
| Other | 25 (23.4) | 26 (8.4) | |
| Physician’s experience—biologics, n (%) | <0.001 | ||
| None | 0 (0.0) | 77 (24.9) | |
| <1 y | 0 (0.0) | 10 (3.2) | |
| 1 ≤ 2 y | 9 (8.4) | 25 (8.1) | |
| 2 ≤ 3 y | 4 (3.7) | 14 (4.5) | |
| 3 ≤ 4 y | 13 (12.2) | 19 (6.2) | |
| 4 ≤ 5 y | 35 (32.7) | 58 (18.8) | |
| >5 y | 46 (43) | 106 (34.3) | |
| Physician’s perspective on patient’s understanding of disease, n (%) | 0.001 | ||
| Understands very well | 42 (39.3) | 64 (20.7) | |
| Somewhat understands | 55 (51.4) | 215 (69.6) | |
| Neither | 7 (6.5) | 27 (8.7) | |
| Does not understand very well | 3 (2.8) | 3 (1.0) | |
| Does not understand at all | 0 (0.0) | 0 (0.0) | |
| Physician’s perspective on patient’s understanding of treatment choice, n (%) | <0.001 | ||
| Understands very well | 45 (42.1) | 69 (22.3) | |
| Somewhat understands | 49 (45.8) | 209 (67.6) | |
| Neither | 10 (9.4) | 27 (8.7) | |
| Does not understand very well | 3 (2.8) | 4 (1.3) | |
| Does not understand at all | 0 (0.0) | 0 (0.0) | |
| PGA disease severity | 2.0 ± 1.5 | 2.7 ± 1.0 | <0.001 |
| Treatment Satisfaction (0–10 scale) | 7.8 ± 1.7 | 6.0 ± 2.0 | <0.001 |
| Variables 1,2 | Odds Ratio (95% CI) | p |
|---|---|---|
| Patient-reported variables v 3 | n = 383 | |
| Biologic vs. non-biologic | 1.820 (1.154, 2.868) | 0.010 |
| Age, y | 0.983 (0.970, 0.997) | 0.016 |
| Lesion site, back | 0.544 (0.358, 0.825) | 0.004 |
| TSQM score (global satisfaction) | 1.014 (1.002, 1.026) | 0.021 |
| DLQI score | ||
| Daily activities | 1.106 (0.900, 1.360) | 0.336 |
| Leisure | 1.132 (0.886, 1.446) | 0.321 |
| Personal relationships | 1.085 (0.858, 1.373) | 0.497 |
| Physician-reported variables 4 | n = 413 | |
| Biologic vs. non-biologic user | 10.967 (5.723, 21.014) | <0.001 |
| Patient age, y | 1.003 (0.989, 1.017) | 0.664 |
| Location of lesion (upper limb) | 0.870 (0.549, 1.377) | 0.552 |
| Physician’s specialty—psoriasis | 1.042 (0.602, 1.803) | 0.884 |
| Physician’s workplace | ||
| University hospital | 0.696 (0.429, 1.128) | 0.141 |
| Other | 0.663 (0.342, 1.284) | 0.223 |
| Physician’s experience—biologics | 1.096 (0.991, 1.212) | 0.073 |
| Patient’s understanding of disease (physician perspective) | 1.390 (0.839, 2.303) | 0.202 |
| Patient’s understanding of treatment choice (physician perspective) | 0.631 (0.386, 1.032) | 0.067 |
| PGA disease severity | 0.720 (0.584, 0.887) | 0.002 |
| Treatment Satisfaction | 1.285 (1.139, 1.449) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okubo, Y.; Tang, A.C.; Inoue, S.; Torisu-Itakura, H.; Ohtsuki, M. Comparison of Treatment Goals between Users of Biological and Non-Biological Therapies for Treatment of Psoriasis in Japan. J. Clin. Med. 2021, 10, 5732. https://doi.org/10.3390/jcm10245732
Okubo Y, Tang AC, Inoue S, Torisu-Itakura H, Ohtsuki M. Comparison of Treatment Goals between Users of Biological and Non-Biological Therapies for Treatment of Psoriasis in Japan. Journal of Clinical Medicine. 2021; 10(24):5732. https://doi.org/10.3390/jcm10245732
Chicago/Turabian StyleOkubo, Yukari, Ann Chuo Tang, Sachie Inoue, Hitoe Torisu-Itakura, and Mamitaro Ohtsuki. 2021. "Comparison of Treatment Goals between Users of Biological and Non-Biological Therapies for Treatment of Psoriasis in Japan" Journal of Clinical Medicine 10, no. 24: 5732. https://doi.org/10.3390/jcm10245732
APA StyleOkubo, Y., Tang, A. C., Inoue, S., Torisu-Itakura, H., & Ohtsuki, M. (2021). Comparison of Treatment Goals between Users of Biological and Non-Biological Therapies for Treatment of Psoriasis in Japan. Journal of Clinical Medicine, 10(24), 5732. https://doi.org/10.3390/jcm10245732






