Single-Port versus Multiple-Port Robot-Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
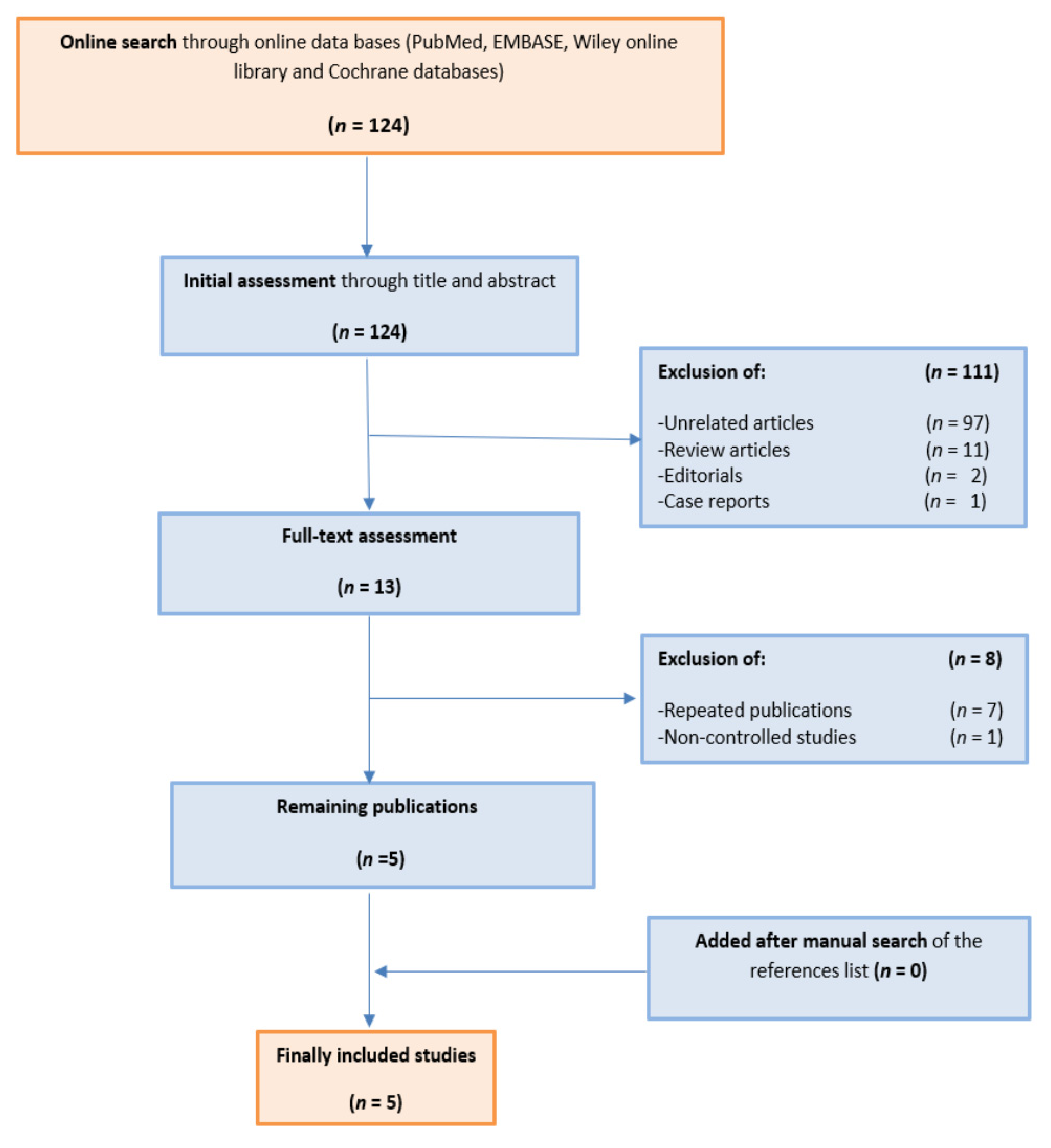
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Primary Outcomes
2.4. Statistical Analysis
2.5. Risk of Bias Assessment
3. Results
3.1. Search Results
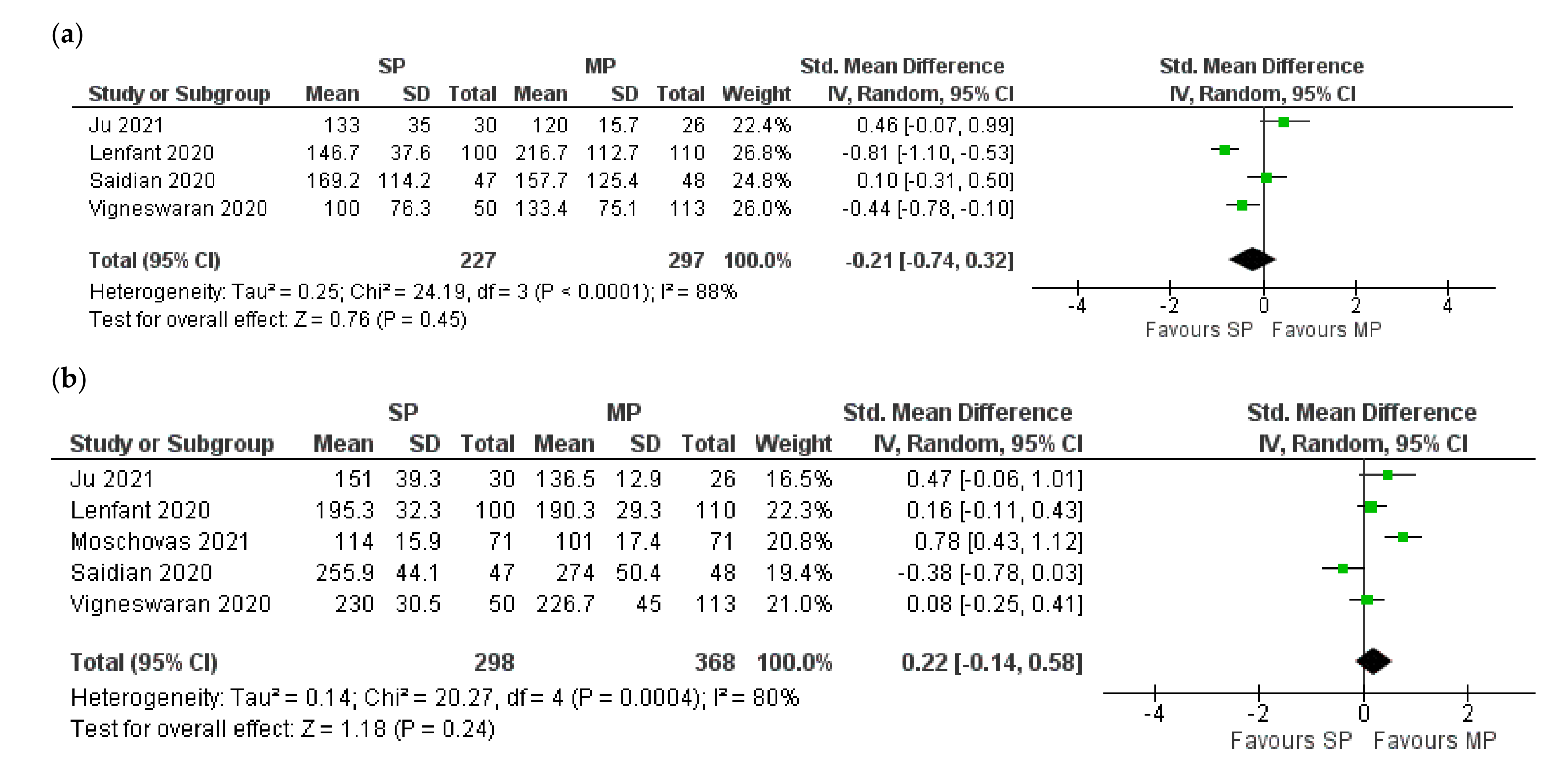
3.2. Perioperative Outcomes
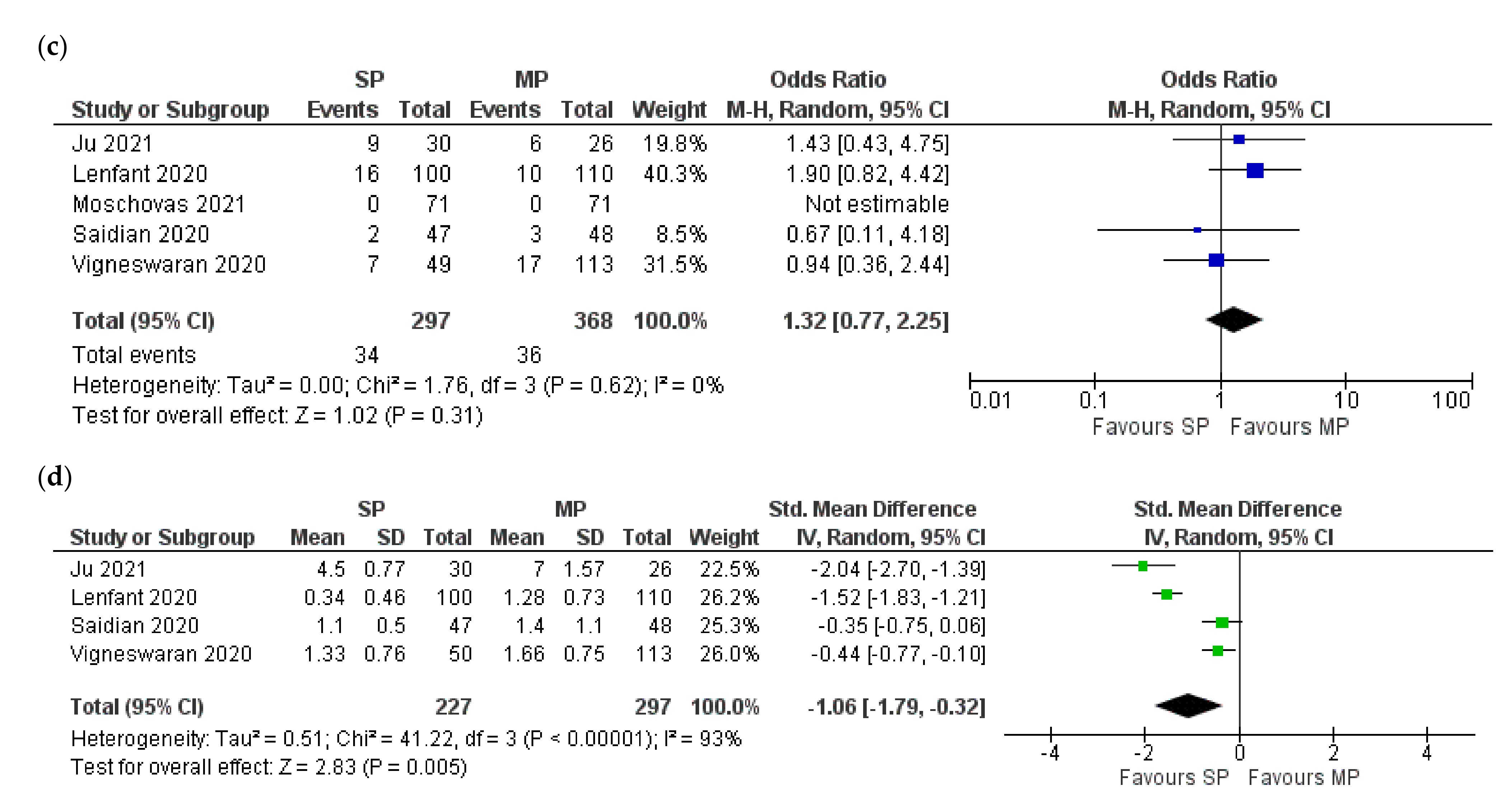
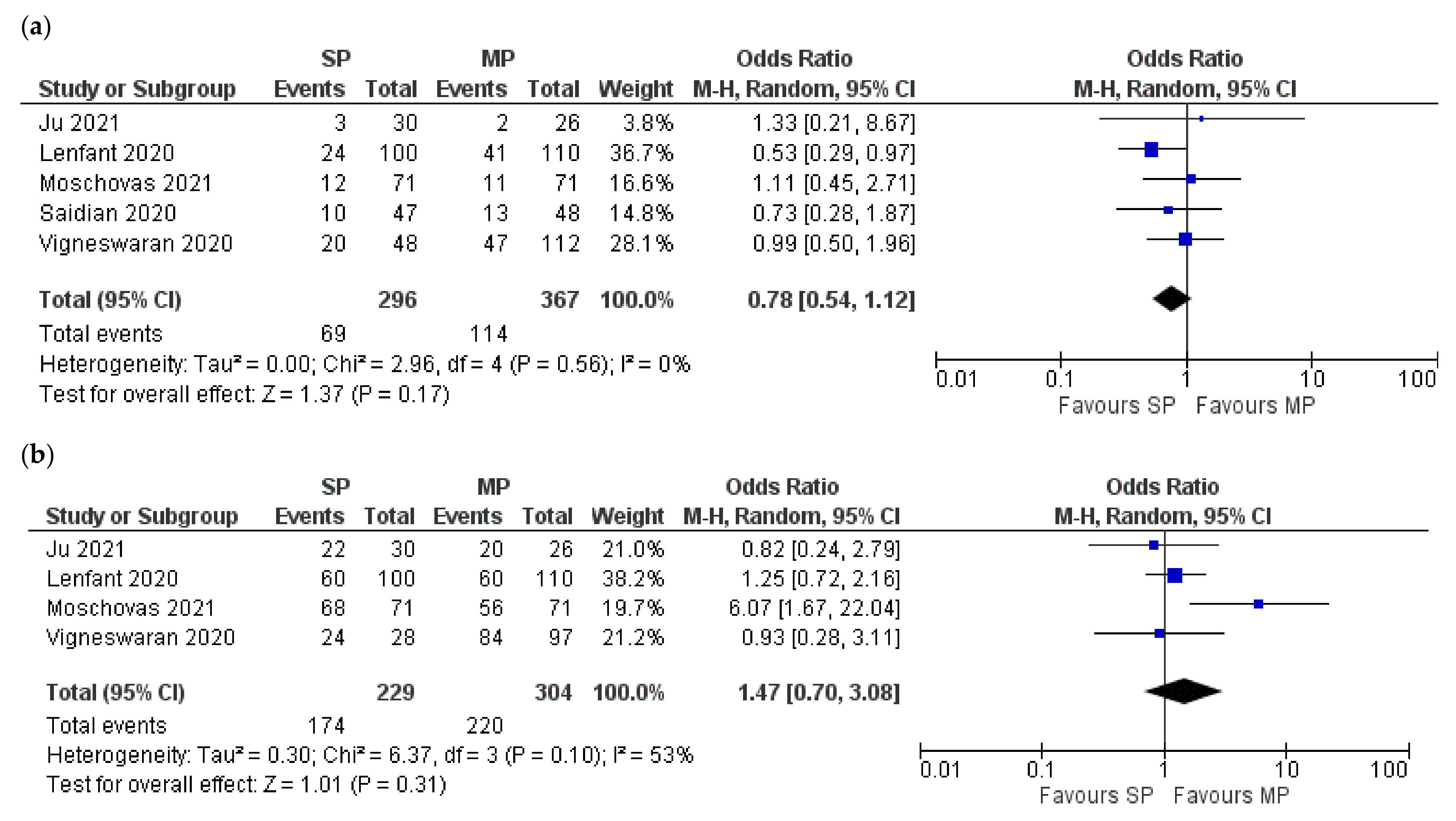
3.3. Oncological Outcomes
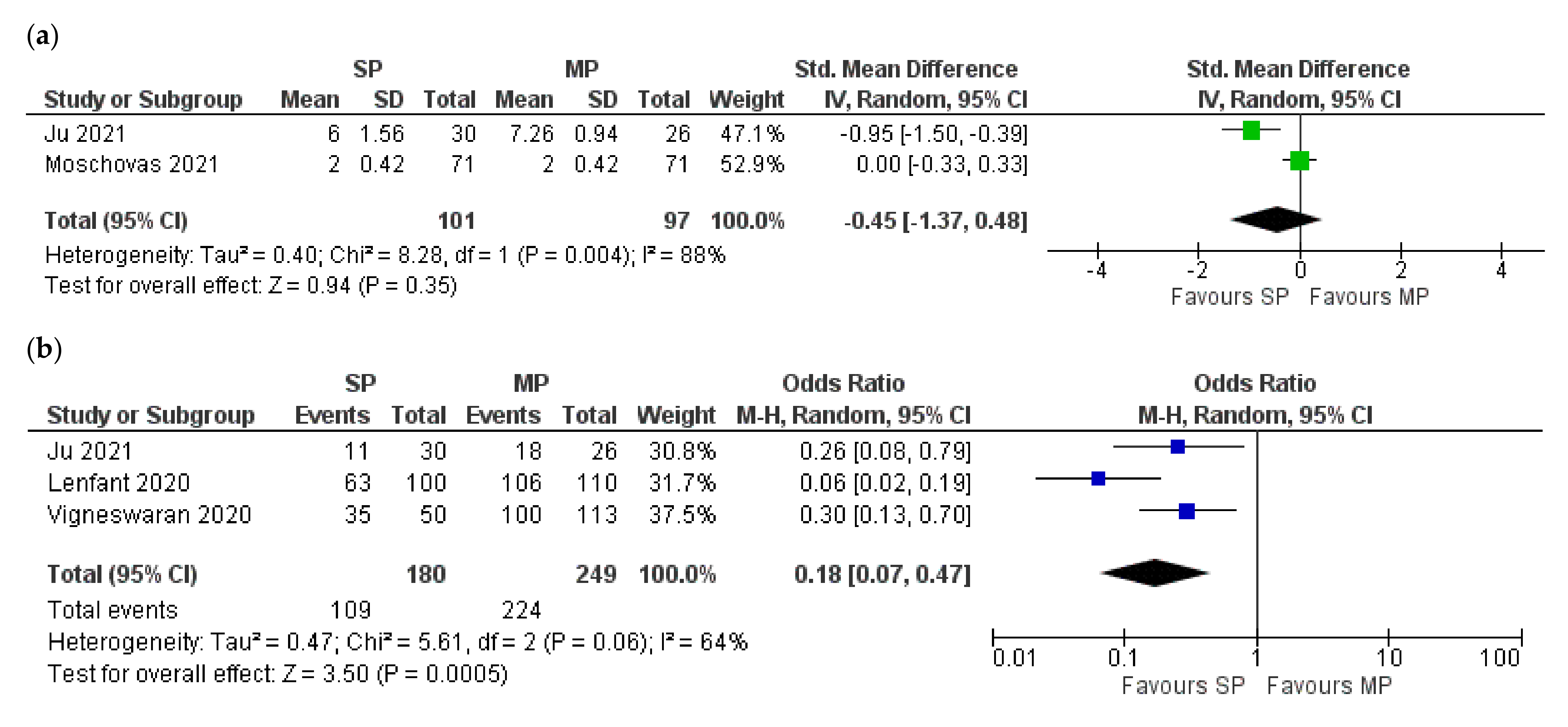
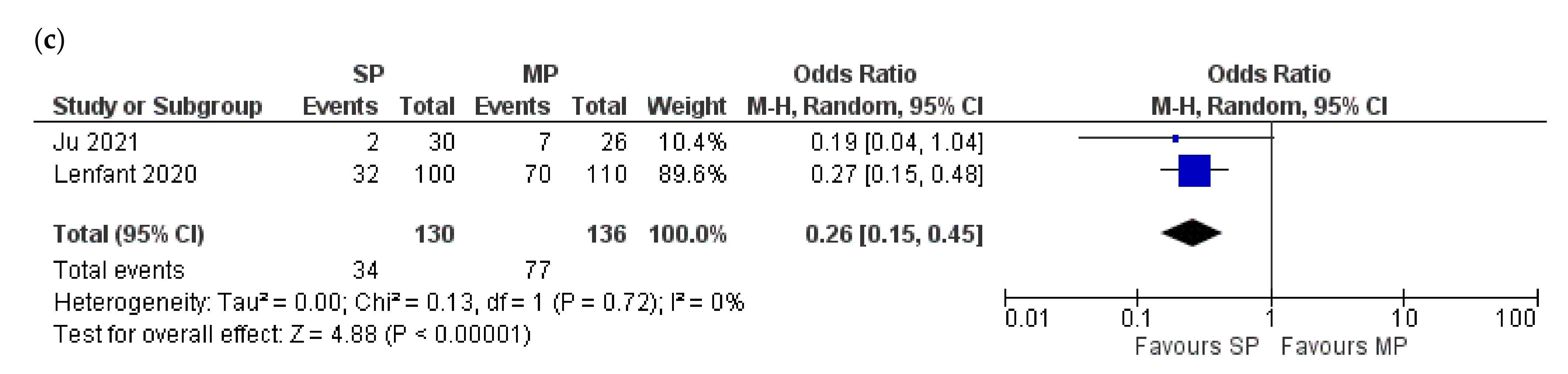
3.4. Functional Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rawla, P. Epidemiology of Prostate Cancer. World J. Oncol. 2019, 10, 63–89. [Google Scholar] [CrossRef] [Green Version]
- Fahmy, O.; Khairul-Asri, M.G.; Hadi, S.H.; Gakis, G.; Stenzl, A. The Role of Radical Prostatectomy and Radiotherapy in Treatment of Locally Advanced Prostate Cancer: A Systematic Review and Meta-Analysis. Urol. Int. 2017, 99, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Gray, P.J.; Lin, C.C.; Cooperberg, M.R.; Jemal, A.; Efstathiou, J.A. Temporal Trends and the Impact of Race, Insurance, and Socioeconomic Status in the Management of Localized Prostate Cancer. Eur. Urol. 2017, 71, 729–737. [Google Scholar] [CrossRef]
- Oberlin, D.T.; Flum, A.S.; Lai, J.D.; Meeks, J.J. The effect of minimally invasive prostatectomy on practice patterns of American urologists. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 255.e1–255e5. [Google Scholar] [CrossRef] [Green Version]
- Fahmy, O.; Asri, K.; Schwentner, C.; Stenzl, A.; Gakis, G. Current status of robotic assisted radical cystectomy with intracorporeal ileal neobladder for bladder cancer. J. Surg. Oncol. 2015, 112, 427–429. [Google Scholar] [CrossRef]
- Mazzone, E.; Mistretta, F.; Knipper, S.; Tian, Z.; Larcher, A.; Widmer, H.; Zorn, K.; Capitanio, U.; Graefen, M.; Montorsi, F.; et al. Contemporary National Assessment of Robot-Assisted Surgery Rates and Total Hospital Charges for Major Surgical Uro-Oncological Procedures in the United States. J. Endourol. 2019, 33, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, D.K.; Sharma, V.; Toussi, A.; Viers, B.R.; Tollefson, M.K.; Gettman, M.T.; Frank, I. Initial Experience with da Vinci Single-port Robot-assisted Radical Prostatectomies. Eur. Urol. 2020, 77, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Kaouk, J.; Garisto, J.; Bertolo, R. Robotic Urologic Surgical Interventions Performed with the Single Port Dedicated Platform: First Clinical Investigation. Eur. Urol. 2019, 75, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Lenfant, L.; Sawczyn, G.; Aminsharifi, A.; Kim, S.; Wilson, C.A.; Beksac, A.T.; Schwen, Z.; Kaouk, J. Pure Single-site Robot-assisted Radical Prostatectomy Using Single-port Versus Multiport Robotic Radical Prostatectomy: A Single-institution Comparative Study. Eur. Urol. Focus 2020, 7, 964–972. [Google Scholar] [CrossRef]
- Xu, D.-L.; Ju, G.-Q.; Wang, Z.-J.; Shi, J.-Z.; Zhang, Z.-Q.; Wu, Z.-J.; Yin, L.; Liu, B.; Wang, L.-H. A comparison of perioperative outcomes between extraperitoneal robotic single-port and multiport radical prostatectomy with the da Vinci Si Surgical System. Asian J. Androl. 2021, 23, 640. [Google Scholar] [CrossRef]
- Moschovas, M.C.; Bhat, S.; Sandri, M.; Rogers, T.; Onol, F.; Mazzone, E.; Roof, S.; Mottrie, A.; Patel, V. Comparing the Approach to Radical Prostatectomy Using the Multiport da Vinci Xi and da Vinci SP Robots: A Propensity Score Analysis of Perioperative Outcomes. Eur. Urol. 2021, 79, 393–404. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- AMSTAR. Assessing the Methodological Quality of Systematic Reviews. Available online: https://amstar.ca/Amstar_Checklist.php (accessed on 3 June 2020).
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.A.; Shea, B.; O’Connel, D.; Peterson, J.; Welch, V.; Losos, M. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2012. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 10 July 2021).
- Vigneswaran, H.T.; Schwarzman, L.S.; Francavilla, S.; Abern, M.R.; Crivellaro, S. A Comparison of Perioperative Outcomes Between Single-port and Multiport Robot-assisted Laparoscopic Prostatectomy. Eur. Urol. 2020, 77, 671–674. [Google Scholar] [CrossRef] [PubMed]
- Saidian, A.; Fang, A.M.; Hakim, O.; Magi-Galluzzi, C.; Nix, J.W.; Rais-Bahrami, S. Perioperative Outcomes of Single vs Multi-Port Robotic Assisted Radical Prostatectomy: A Single Institutional Experience. J. Urol. 2020, 204, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Curcean, A.; Rescigno, P.; ap Dafydd, D.; Tree, A.; Reid, A.; Koh, D.-M.; Sohaib, A.; Tunariu, N.; Shur, J. Imaging features of the evolving patterns of metastatic prostate cancer. Clin. Radiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Schuessler, W.W.; Schulam, P.G.; Clayman, R.V.; Kavoussi, L.R. Laparoscopic radical prostatectomy: Initial short-term experience. Urology 1997, 50, 854–857. [Google Scholar] [CrossRef]
- Binder, J.; Kramer, W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001, 87, 408–410. [Google Scholar] [CrossRef]
- Abbou, C.C.; Hoznek, A.; Salomon, L.; Olsson, L.E.; Lobontiu, A.; Saint, F.; Cicco, A.; Antiphon, P.; Chopin, D. Laparoscopic Radical Prostatectomy with a Remote Controlled Robot. J. Urol. 2001, 165, 1964–1966. [Google Scholar] [CrossRef]
- Darwich, D.; Darwich, I.; Willeke, F. The TransEnterix European Patient Registry for Robotic-Assisted Laparoscopic Procedures in Urology, Abdominal, Thoracic, and Gynecologic Surgery (“TRUST”). Surg. Technol. Int. 2021, 38. [Google Scholar] [CrossRef]
- Moschovas, M.C.; Bhat, S.; Rogers, T.; Onol, F.; Roof, S.; Mazzone, E.; Mottrie, A.; Patel, V. Technical Modifications Necessary to Implement the da Vinci Single-port Robotic System. Eur. Urol. 2020, 78, 415–423. [Google Scholar] [CrossRef]
- Lenfant, L.; Aminsharifi, A.; Kim, S.; Kaouk, J. Predictive factors of postoperative complications and hospital readmission after implementation of the single-port robotic platform: A single-center and single-surgeon experience. Int. J. Urol. 2021, 28, 530–537. [Google Scholar] [CrossRef]
- Noël, J.; Moschovas, M.C.; Sandri, M.; Bhat, S.; Rogers, T.; Reddy, S.; Corder, C.; Patel, V. Patient surgical satisfaction after da Vinci® single-port and multi-port robotic-assisted radical prostatectomy: Propensity score-matched analysis. J. Robot. Surg. 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.K.; Jang, W.S.; Kim, S.W.; Kim, S.H.; Han, S.W.; Lee, Y.S. Robot-assisted laparoscopic single-port pyeloplasty using the da Vinci SP® system: Initial experience with a pediatric patient. J. Pediatr. Urol. 2019, 15, 576–577. [Google Scholar] [CrossRef] [PubMed]
- Kaouk, J.; Aminsharifi, A.; Sawczyn, G.; Kim, S.; Wilson, C.A.; Garisto, J.; Fareed, K. Single-Port Robotic Urological Surgery Using Purpose-Built Single-Port Surgical System: Single-Institutional Experience with the First 100 Cases. Urology 2020, 140, 77–84. [Google Scholar] [CrossRef]
- Kaouk, J.; Beksac, A.T.; Zeinab, M.A.; Duncan, A.; Schwen, Z.R.; Eltemamy, M. Single Port Transvesical Robotic Radical Prostatectomy: Initial Clinical Experience and Description of Technique. Urology 2021, 155, 130–137. [Google Scholar] [CrossRef] [PubMed]
| Study | Time Frame | Country | Sample Size | Median (Range) Follow-Up Months | ||
|---|---|---|---|---|---|---|
| SP | MP | SP | MP | |||
| Moschovas 2021 [9] | June 2019–April 2020 | USA | 71 | 71 | 4.4 (1.6–7.2) | 3.2 (1.6–4.8) |
| Ju 2021 [10] | April 2019–March2020 | China | 30 | 26 | 3 | 3 |
| Saidian 2020 [11] | October 2018–June 2019 | USA | 47 | 48 | NA | NA |
| Lenfant 2020 [16] | January 2019–January 2020 | USA | 100 | 110 | 12 | 12 |
| Vigneswaran 2020 [17] | Sepember 2017–November 2019 | USA | 50 | 113 | 4.7 (4.3–4.3) | 7.7 (5.0–12.7) |
| Study | Selection | Comparability | Outcome | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of Exposed Cohort | Selection of Non-Exposed | Ascertainment of Exposure | Outcome Not Present at Start | Assessment of Outcome | Adequate Follow-Up Length | Adequacy of Follow-Up | |||
| Moschovas 2021 [9] | * | * | * | * | ** | * | - | * | 8/9 |
| Ju 2021 [10] | * | * | * | * | ** | * | - | * | 8/9 |
| Saidian 2020 [11] | * | * | * | * | *- | * | - | * | 7/9 |
| Lenfant 2020 [16] | * | * | * | * | *- | * | * | * | 8/9 |
| Vigneswaran 2020 [17] | * | * | * | * | *- | * | - | * | 7/9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fahmy, O.; Fahmy, U.A.; Alhakamy, N.A.; Khairul-Asri, M.G. Single-Port versus Multiple-Port Robot-Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5723. https://doi.org/10.3390/jcm10245723
Fahmy O, Fahmy UA, Alhakamy NA, Khairul-Asri MG. Single-Port versus Multiple-Port Robot-Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(24):5723. https://doi.org/10.3390/jcm10245723
Chicago/Turabian StyleFahmy, Omar, Usama A. Fahmy, Nabil A. Alhakamy, and Mohd Ghani Khairul-Asri. 2021. "Single-Port versus Multiple-Port Robot-Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 24: 5723. https://doi.org/10.3390/jcm10245723
APA StyleFahmy, O., Fahmy, U. A., Alhakamy, N. A., & Khairul-Asri, M. G. (2021). Single-Port versus Multiple-Port Robot-Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(24), 5723. https://doi.org/10.3390/jcm10245723






