Portal Vein Thrombosis Is Associated with an Increased Incidence of Depression and Anxiety Disorders
Abstract
1. Introduction
2. Methods
2.1. Database
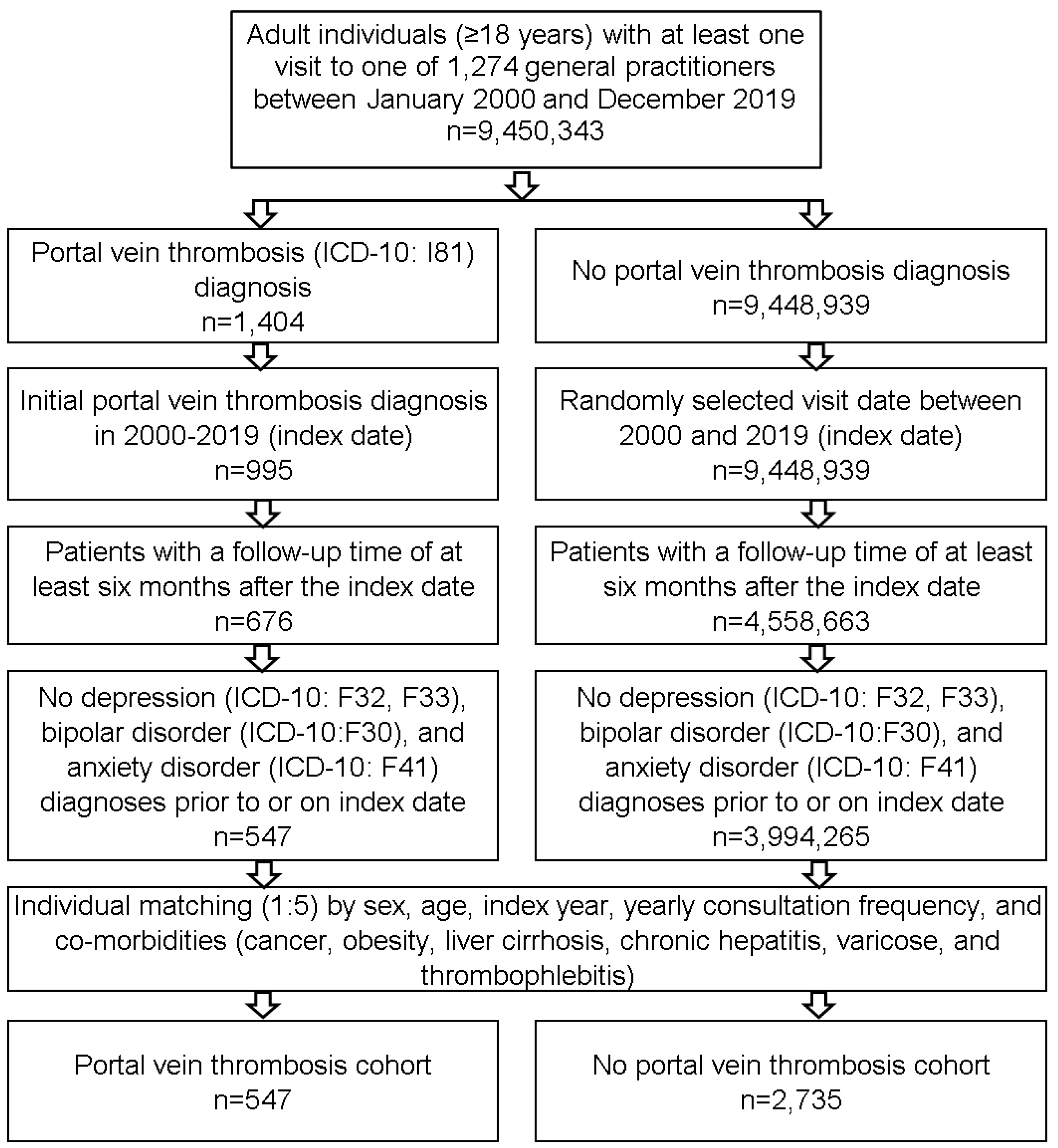
2.2. Study Population
2.3. Ethics Approval
2.4. Study Outcome and Statistical Analyses
3. Results
3.1. Baseline Characteristics
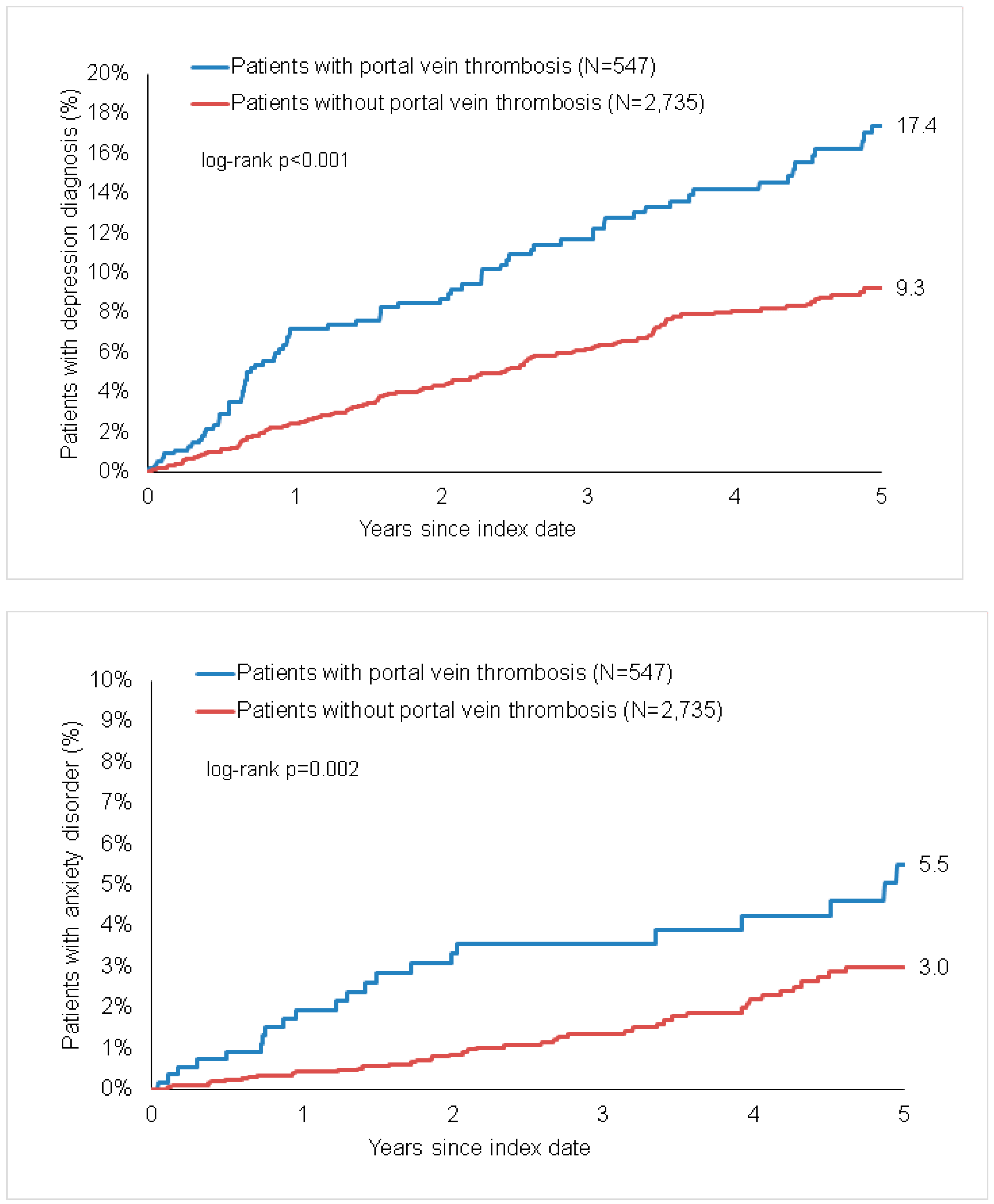
3.2. Incidence of Depression in Patients with and without PVT
3.3. Incidence of Anxiety Disorders in Patients with and without PVT
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Portal vein thrombosis | PVT |
| cardiovascular diseases | CVDs |
| Disease Analyzer database | IQVIA |
| International Classification of Diseases, 10th revision | ICD–10 |
| European Pharmaceutical Market Research Association | EPhMRA |
| Anatomical Therapeutic Chemical Classification | ATC |
| general practitioner | GP |
| Hazard Ratio | HR |
| gamma-aminobutyric acid | GABA |
| brain-derived neurotrophic factor | BDNF |
References
- Tsochatzis, E.A.; Senzolo, M.; Germani, G.; Gatt, A.; Burroughs, A.K. Systematic review: Portal vein thrombosis in cirrhosis. Aliment. Pharmacol. Ther. 2010, 31, 366–374. [Google Scholar] [CrossRef]
- Nery, F.; Carneiro, P.; Correia, S.; Macedo, C.; Gandara, J.; Lopes, V.; Valadares, D.; Ferreira, S.; Oliveira, J.; Gomes, M.T.; et al. Systemic inflammation as a risk factor for portal vein thrombosis in cirrhosis: A prospective longitudinal study. Eur. J. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Nery, F.; Chevret, S.; Condat, B.; de Raucourt, E.; Boudaoud, L.; Rautou, P.-E.; Plessier, A.; Roulot, D.; Chaffaut, C.; Bourcier, V.; et al. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: Results of a longitudinal study. Hepatology 2015, 61, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Plessier, A.; Darwish-Murad, S.; Hernandez-Guerra, M.; Consigny, Y.; Fabris, F.; Trebicka, J.; Heller, J.; Morard, I.; Lasser, L.; Langlet, P.; et al. Acute portal vein thrombosis unrelated to cirrhosis: A prospective multicenter follow-up study. Hepatology 2010, 51, 210–218. [Google Scholar] [CrossRef]
- Tsochatzis, E.A.; Bosch, J.; Burroughs, A.K. Liver cirrhosis. Lancet 2014, 383, 1749–1761. [Google Scholar] [CrossRef]
- Mack, S.; Jacobi, F.; Beesdo-Baum, K.; Gerschler, A.; Strehle, J.; Höfler, M.; Busch, M.A.; Maske, U.; Hapke, U.; Gaebel, W.; et al. Functional disability and quality of life decrements in mental disorders: Results from the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Eur. Psychiatry 2015, 30, 793–800. [Google Scholar] [CrossRef]
- Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx); Institute of Health Metrics and Evaluation: Seattla, WA, USA, 2021. [Google Scholar]
- Hapke, U.; Cohrdes, C.; Nübel, J. Depressive Symptoms in a European Comparison—Results from the European Health Interview Survey (EHIS) 2; Robert Koch-Institut: Berlin, Germany, 2019. [Google Scholar]
- Buganza-Torio, E.; Mitchell, N.; Abraldes, J.G.; Thomas, L.; Ma, M.; Bailey, R.J.; Tandon, P. Depression in cirrhosis—A prospective evaluation of the prevalence, predictors and development of a screening nomogram. Aliment. Pharmacol. Ther. 2019, 49, 194–201. [Google Scholar] [CrossRef]
- Nardelli, S.; Pentassuglio, I.; Pasquale, C.; Ridola, L.; Moscucci, F.; Merli, M.; Mina, C.; Marianetti, M.; Fratino, M.; Izzo, C.; et al. Depression, anxiety and alexithymia symptoms are major determinants of health related quality of life (HRQoL) in cirrhotic patients. Metab. Brain Dis. 2013, 28, 239–243. [Google Scholar] [CrossRef]
- Bianchi, G.; Marchesini, G.; Nicolino, F.; Graziani, R.; Sgarbi, D.; Loguercio, C.; Abbiati, R.; Zoli, M. Psychological status and depression in patients with liver cirrhosis. Dig. Liver Dis. 2005, 37, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Rogal, S.S.; Udawatta, V.; Akpan, I.; Moghe, A.; Chidi, A.; Shetty, A.; Szigethy, E.; Bielefeldt, K.; DiMartini, A. Risk factors for hospitalizations among patients with cirrhosis: A prospective cohort study. PLoS ONE 2017, 12, e0187176. [Google Scholar] [CrossRef]
- Jiang, W.; Krishnan, R.R.K.; O’Connor, C.M. Depression and heart disease: Evidence of a link, and its therapeutic implications. CNS Drugs 2002, 16, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Halaris, A. Inflammation-Associated Co-morbidity Between Depression and Cardiovascular Disease. Curr. Top. Behav. Neurosci. 2017, 31, 45–70. [Google Scholar]
- Lee, C.W.-S.; Liao, C.-H.; Lin, C.-L.; Liang, J.-A.; Sung, F.-C.; Kao, C.-H. Depression and risk of venous thromboembolism: A population-based retrospective cohort study. Psychosom. Med. 2015, 77, 591–598. [Google Scholar] [CrossRef]
- Moretti, R.; Bernobich, E.; Esposito, F.; Torre, P.; Antonello, R.M.; de Angelis, L.; Bellini, G. Depression in vascular pathologies: The neurologist’s point of view. VHRM 2011, 7, 433–443. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, C.-H.; Giuliani, F. The Role of Inflammation in Depression and Fatigue. Front. Immunol. 2019, 10, 1696. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Fan, X.; Zhang, R.; Jiang, S.; Yang, K.; Chen, S. Systemic inflammation and portal vein thrombosis in cirrhotic patients with gastroesophageal varices. Eur. J. Gastroenterol. Hepatol. 2020, 32, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Rathmann, W.; Bongaerts, B.; Carius, H.-J.; Kruppert, S.; Kostev, K. Basic characteristics and representativeness of the German Disease Analyzer database. Int. J. Clin. Pharmacol. Ther. 2018, 56, 459–466. [Google Scholar] [CrossRef]
- Hare, D.L.; Toukhsati, S.R.; Johansson, P.; Jaarsma, T. Depression and cardiovascular disease: A clinical review. Eur. Heart J. 2014, 35, 1365–1372. [Google Scholar] [CrossRef]
- Beutel, M.E.; Brähler, E.; Wiltink, J.; Kerahrodi, J.G.; Burghardt, J.; Michal, M.; Schulz, A.; Wild, P.S.; Münzel, T.; Schmidtmann, I.; et al. New onset of depression in aging women and men: Contributions of social, psychological, behavioral, and somatic predictors in the community. Psychol. Med. 2019, 49, 1148–1155. [Google Scholar] [CrossRef]
- Ernst, M.; Wiltink, J.; Tibubos, A.N.; Brähler, E.; Schulz, A.; Wild, P.S.; Burghardt, J.; Münzel, T.; König, J.; Lackner, K.; et al. Linking cancer and mental health in men and women in a representative community sample. J. Psychosom. Res. 2019, 124, 109760. [Google Scholar] [CrossRef]
- Naylor, C.; Parsonage, M.; McDaid, D.; Knapp, M.; Fossey, M.; Galea, A. Long-Term Conditions and Mental Health: The Cost of Co-Morbidities; The Kings Fund: UK, 2012. [Google Scholar]
- Thom, R.; Silbersweig, D.A.; Boland, R.J. Major Depressive Disorder in Medical Illness: A Review of Assessment, Prevalence, and Treatment Options. Psychosom. Med. 2019, 81, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Woo, A.K. Depression and Anxiety in Pain. Rev. Pain 2010, 4, 8–12. [Google Scholar] [CrossRef] [PubMed]
| Variable | Patients with Portal Vein Thrombosis (n = 547) | Patients without Portal Vein Thrombosis (n = 2735) | p Value |
|---|---|---|---|
| Women | 38.9 | 38.7 | 0.907 |
| Men | 61.1 | 61.3 | |
| Mean age in years (standard deviation) | 57.3 (16.1) | 57.5 (16.0) | 0.898 |
| Age ≤50 years | 32.2 | 32.3 | 0.998 |
| Age 51–60 years | 22.7 | 22.3 | |
| Age 61–70 years | 21.2 | 21.1 | |
| Age >70 years | 24.0 | 24.2 | |
| Mean number of consultations per year | 5.3 (7.4) | 4.9 (6.7) | 0.411 |
| Diagnoses documented within 12 months prior to the index date | |||
| Cancer | 21.9 | 21.3 | 0.727 |
| Obesity | 10.6 | 10.3 | 0.835 |
| Liver cirrhosis or chronic hepatitis | 18.8 | 16.4 | 0.125 |
| Thrombophlebitis | 16.8 | 15.4 | 0.406 |
| Varicose | 27.6 | 25.4 | 0.275 |
| Depression | Anxiety Disorder | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| Overall | 2.01 (1.53–2.64) | <0.001 | 2.16 (1.35–3.46) | 0.001 |
| Women | 1.62 (1.30–2.54) | 0.017 | 1.82 (0.89–3.73) | 0.101 |
| Men | 2.45 (1.68–3.57) | <0.001 | 2.42 (1.30–4.54) | 0.005 |
| Patients with liver cirrhosis | 2.27 (1.27–4.04) | 0.006 | 2.31 (0.55–9.68) | 0.253 |
| Patients without liver cirrhosis | 1.93 (1.42–2.63) | <0.001 | 2.18 (1.26–3.77) | 0.006 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gairing, S.J.; Galle, P.R.; Schattenberg, J.M.; Kostev, K.; Labenz, C. Portal Vein Thrombosis Is Associated with an Increased Incidence of Depression and Anxiety Disorders. J. Clin. Med. 2021, 10, 5689. https://doi.org/10.3390/jcm10235689
Gairing SJ, Galle PR, Schattenberg JM, Kostev K, Labenz C. Portal Vein Thrombosis Is Associated with an Increased Incidence of Depression and Anxiety Disorders. Journal of Clinical Medicine. 2021; 10(23):5689. https://doi.org/10.3390/jcm10235689
Chicago/Turabian StyleGairing, Simon Johannes, Peter Robert Galle, Jörn M. Schattenberg, Karel Kostev, and Christian Labenz. 2021. "Portal Vein Thrombosis Is Associated with an Increased Incidence of Depression and Anxiety Disorders" Journal of Clinical Medicine 10, no. 23: 5689. https://doi.org/10.3390/jcm10235689
APA StyleGairing, S. J., Galle, P. R., Schattenberg, J. M., Kostev, K., & Labenz, C. (2021). Portal Vein Thrombosis Is Associated with an Increased Incidence of Depression and Anxiety Disorders. Journal of Clinical Medicine, 10(23), 5689. https://doi.org/10.3390/jcm10235689








