Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. PICOS Framework
2.2. Review Questions
- Is it possible to manage AOB in non-growing patients and adults by means of the intrusion of molar teeth with skeletal anchorage?
- What are the outcomes of AOB treatment by molar teeth intrusion with skeletal anchorage or by orthognathic surgery rated by comparisons of the measurements taken pre-treatment (T1) and post-treatment (T2)?
- Does the treatment of AOB by means of molar intrusion with skeletal anchorage provide the same long-term results as the orthognathic surgery correction assessed by comparisons of the measurements taken post-treatment (T2) and at least one year into retention (T3)?
2.3. Inclusion Criteria
- Human studies;
- Articles concerning adults (over 18 years of age) and non-growing individuals;
- Randomized and non-randomized clinical trials;
- Cohort studies
- Cases series studies with at least 5 cases included;
- Articles assessing long-term results of the treatment.
2.4. Exclusion Criteria
- Case reports and cases series studies with less than 5 cases included;
- Animal studies;
- Review articles;
- Articles with a follow-up period of less than 12 months
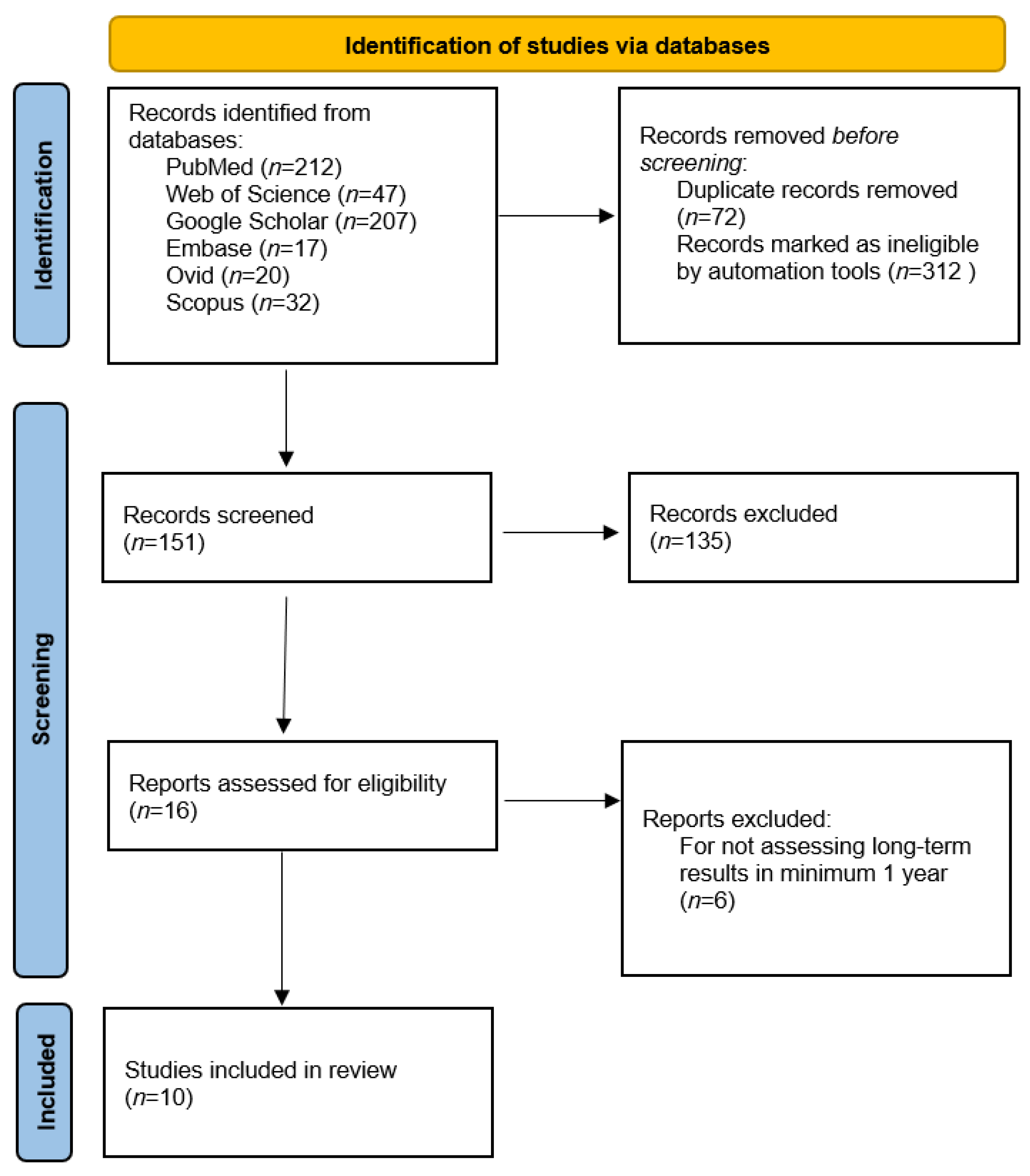
2.5. Article Selection
2.6. Data Extraction
2.7. Assessment of the Risk of Bias
2.8. Assessment of the Strength of Evidence for the Evaluated Outcomes
2.9. Synthesis of the Extracted Data
3. Results
3.1. Characteristics of the Included Studies
3.2. Results of AOB Treatment Assessed by Achieving Positive Overbite on the Incisors and Other Parameters of AFH
3.3. The Effects of AOB Treatment Assessed by Achieving Positive Overbite on the Incisors and Other Parameters of AFH
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sandler, P.J.; Madahar, A.K.; Murray, A. Anterior Open Bite: Aetiology and Management. Dent. Update 2011, 38, 522–524, 527–528, 531–532. [Google Scholar] [CrossRef]
- Baek, M.-S.; Choi, Y.-J.; Yu, H.-S.; Lee, K.-J.; Kwak, J.; Park, Y.-C. Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior Teeth. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 396.e1–396.e9. [Google Scholar] [CrossRef]
- Lopez-Gavito, G.; Wallen, T.R.; Little, R.M.; Joondeph, D.R. Anterior Open-Bite Malocclusion: A Longitudinal 10-Year Postretention Evaluation of Orthodontically Treated Patients. Am. J. Orthod. 1985, 87, 175–186. [Google Scholar] [CrossRef]
- Leite, J.S.; Matiussi, L.B.; Salem, A.C.; Provenzano, M.G.A.; Ramos, A.L. Effects of Palatal Crib and Bonded Spurs in Early Treatment of Anterior Open Bite: A Prospective Randomized Clinical Study. Angle Orthod. 2016, 86, 734–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L. Stability of Anterior Openbite Correction with Multiloop Edgewise Archwire Therapy: A Cephalometric Follow-up Study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teittinen, M.; Tuovinen, V.; Tammela, L.; Schätzle, M.; Peltomäki, T. Long-Term Stability of Anterior Open Bite Closure Corrected by Surgical-Orthodontic Treatment. Eur. J. Orthod. 2012, 34, 238–243. [Google Scholar] [CrossRef] [Green Version]
- Sugawara, J.; Baik, U.B.; Umemori, M.; Takahashi, I.; Nagasaka, H.; Kawamura, H.; Mitani, H. Treatment and Posttreatment Dentoalveolar Changes Following Intrusion of Mandibular Molars with Application of a Skeletal Anchorage System (SAS) for Open Bite Correction. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 243–253. [Google Scholar]
- Deguchi, T.; Kurosaka, H.; Oikawa, H.; Kuroda, S.; Takahashi, I.; Yamashiro, T.; Takano-Yamamoto, T. Comparison of Orthodontic Treatment Outcomes in Adults with Skeletal Open Bite between Conventional Edgewise Treatment and Implant-Anchored Orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, S60–S68. [Google Scholar] [CrossRef]
- Ding, Y.; Xu, T.-M.; Lohrmann, B.; Gellrich, N.-C.; Schwestka-Polly, R. Stability Following Combined Orthodontic-Surgical Treatment for Skeletal Anterior Open Bite—A Cephalometric 15-Year Follow-Up Study. J. Orofac. Orthop. 2007, 68, 245–256. [Google Scholar] [CrossRef]
- Chow, L.K.; Singh, B.; Chiu, W.K.; Samman, N. Prevalence of Postoperative Complications after Orthognathic Surgery: A 15-Year Review. J. Oral Maxillofac. Surg. 2007, 65, 984–992. [Google Scholar] [CrossRef]
- Panula, K.; Finne, K.; Oikarinen, K. Incidence of Complications and Problems Related to Orthognathic Surgery: A Review of 655 Patients. J. Oral Maxillofac. Surg. 2001, 59, 1128–1136; discussion 1137. [Google Scholar] [CrossRef] [PubMed]
- Steel, B.J.; Cope, M.R. Unusual and Rare Complications of Orthognathic Surgery: A Literature Review. J. Oral Maxillofac. Surg. 2012, 70, 1678–1691. [Google Scholar] [CrossRef] [PubMed]
- Espeland, L.; Dowling, P.A.; Mobarak, K.A.; Stenvik, A. Three-Year Stability of Open-Bite Correction by 1-Piece Maxillary Osteotomy. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Fontes, A.M.; Joondeph, D.R.; Bloomquist, D.S.; Greenlee, G.M.; Wallen, T.R.; Huang, G.J. Long-Term Stability of Anterior Open-Bite Closure with Bilateral Sagittal Split Osteotomy. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Pikdoken, L.; Erkan, M.; Usumez, S. Gingival Response to Mandibular Incisor Extrusion. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 143.e9–143.e13; discussion 432–433. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; Takano-Yamamoto, T. Treatment of Severe Anterior Open Bite with Skeletal Anchorage in Adults: Comparison with Orthognathic Surgery Outcomes. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-S.; Kwon, O.-W.; Sung, J.-H. Nonextraction Treatment of an Open Bite with Microscrew Implant Anchorage. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 391–402. [Google Scholar] [CrossRef]
- Erverdi, N.; Keles, A.; Nanda, R. The Use of Skeletal Anchorage in Open Bite Treatment: A Cephalometric Evaluation. Angle Orthod. 2004, 74, 381–390. [Google Scholar] [CrossRef]
- Freitas, K.M.S.; de Freitas, M.R.; Henriques, J.F.C.; Pinzan, A.; Janson, G. Postretention Relapse of Mandibular Anterior Crowding in Patients Treated without Mandibular Premolar Extraction. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 480–487. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological Quality (Risk of Bias) Assessment Tools for Primary and Secondary Medical Studies: What Are They and Which Is Better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [Green Version]
- Moga, C.; Guo, B.; Schopflocher, D.; Harstall, C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique; Methodology Paper; Institute of Health Economincs: Dhaka, Bangladesh, 2012. [Google Scholar]
- Granholm, A.; Alhazzani, W.; Møller, M.H. Use of the GRADE Approach in Systematic Reviews and Guidelines. Br. J. Anaesth. 2019, 123, 554–559. [Google Scholar] [CrossRef]
- Erverdi, N.; Usumez, S.; Solak, A.; Koldas, T. Noncompliance Open-Bite Treatment with Zygomatic Anchorage. Angle Orthod. 2007, 77, 986–990. [Google Scholar] [CrossRef] [PubMed]
- Akan, S.; Kocadereli, I.; Aktas, A.; Taşar, F. Effects of Maxillary Molar Intrusion with Zygomatic Anchorage on the Stomatognathic System in Anterior Open Bite Patients. Eur. J. Orthod. 2013, 35, 93–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, T.R.; Cousley, R.R.J.; Fishman, L.S.; Tallents, R.H. Dentoskeletal Changes Following Mini-Implant Molar Intrusion in Anterior Open Bite Patients. Angle Orthod. 2015, 85, 941–948. [Google Scholar] [CrossRef] [Green Version]
- Xun, C.; Zeng, X.; Wang, X. Microscrew Anchorage in Skeletal Anterior Open-Bite Treatment. Angle Orthod. 2007, 77, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.A.; Park, Y.C. Treatment and posttreatment changes following intrusion of maxillary posterior teeth with miniscrew implants for open bite correction. Korean J. Orthod. 2013, 38, 31–40. [Google Scholar] [CrossRef] [Green Version]
- Scheffler, N.R.; Proffit, W.R.; Phillips, C. Outcomes and Stability in Patients with Anterior Open Bite and Long Anterior Face Height Treated with Temporary Anchorage Devices and a Maxillary Intrusion Splint. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 594–602. [Google Scholar] [CrossRef] [Green Version]
- Marzouk, E.S.; Kassem, H.E. Evaluation of Long-Term Stability of Skeletal Anterior Open Bite Correction in Adults Treated with Maxillary Posterior Segment Intrusion Using Zygomatic Miniplates. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 78–88. [Google Scholar] [CrossRef]
- Swinnen, K.; Politis, C.; Willems, G.; De Bruyne, I.; Fieuws, S.; Heidbuchel, K.; van Erum, R.; Verdonck, A.; Carels, C. Skeletal and Dento-Alveolar Stability after Surgical-Orthodontic Treatment of Anterior Open Bite: A Retrospective Study. Eur. J. Orthod. 2001, 23, 547–557. [Google Scholar] [CrossRef]
- Fischer, K.; von Konow, L.; Brattström, V. Open Bite: Stability after Bimaxillary Surgery--2-Year Treatment Outcomes in 58 Patients. Eur. J. Orthod. 2000, 22, 711–718. [Google Scholar] [CrossRef] [Green Version]
- Proffit, W.R.; Bailey, L.J.; Phillips, C.; Turvey, T.A. Long-Term Stability of Surgical Open-Bite Correction by Le Fort I Osteotomy. Angle Orthod. 2000, 70, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Zuroff, J.P.; Chen, S.-H.; Shapiro, P.A.; Little, R.M.; Joondeph, D.R.; Huang, G.J. Orthodontic Treatment of Anterior Open-Bite Malocclusion: Stability 10 Years Postretention. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 302.e1–302.e8. [Google Scholar] [CrossRef]
- Dalziel, K.; Round, A.; Stein, K.; Garside, R.; Castelnuovo, E.; Payne, L. Do the Findings of Case Series Studies Vary Significantly According to Methodological Characteristics? Health Technol. Assess. 2005, 9, iii–iv, 1–146. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.; Rodgers, M.; Woolacott, N. Not Only Randomized Controlled Trials, but Also Case Series Should Be Considered in Systematic Reviews of Rapidly Developing Technologies. J. Clin. Epidemiol. 2009, 62, 1253–1260.e4. [Google Scholar] [CrossRef]
- Reyneke, J.P.; Ferretti, C. Anterior Open Bite Correction by Le Fort I or Bilateral Sagittal Split Osteotomy. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 321–338. [Google Scholar] [CrossRef] [PubMed]
| Problem | Intervention Q1 | Intervention Q2 | Outcome |
|---|---|---|---|
| “anterior open bite” | “posterior teeth intrusion” | “orthognathic surgery” | “anterior open bite correction” |
| AOB | “molar intrusion” | LeFort I | “AOB correction” |
| Adult * | “absolute anchorage” | LeFort 1 | “positive overbite” |
| Non-growing | “skeletal anchorage” | “bilateral sagittal split osteotomy” | “mandibular autorotation” |
| Nongrowing | “temporary anchorage” | BSSO | |
| Adolescent * | TAD |
| Deguchi et al. 2011 | |
|---|---|
| 2 |
| 2 |
| 2 |
| 2 |
| 0 |
| 2 |
| 2 |
| 0 |
| 2 |
| 2 |
| 1 |
| 2 |
| TOTAL: | 19 |
| Scheffler et al. 2014 | Marzouk and Kassem 2016 | Teittinen et al. 2012 | Swinnen et al. 2001 | Fischer et al. 2000 | Proffit et al. 2000 | |
|---|---|---|---|---|---|---|
| 2 | 2 | 2 | 2 | 2 | 2 |
| 2 | 1 | 2 | 2 | 1 | 2 |
| 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 1 | 2 | 1 | 1 | 1 |
| 0 | 1 | 0 | 1 | 0 | 0 |
| 2 | 2 | 2 | 2 | 2 | 1 |
| 2 | 1 | 2 | 1 | 1 | 1 |
| 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 1 | 2 | 2 | 2 | 2 |
| 2 | 2 | 2 | 2 | 2 | 0 |
| 2 | 1 | 2 | 2 | 2 | 2 |
| 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 2 | 1 | 1 | 2 | 2 |
| 0 | 0 | 0 | 0 | 0 | 0 |
| TOTAL: | 16 | 14 | 17 | 16 | 15 | 13 |
| Baek et al. 2010 | Sugawara et al. 2002 | Ding et al. 2007 | |
|---|---|---|---|
| 2 | 2 | 2 |
| 2 | 1 | 1 |
| 0 | 0 | 0 |
| 2 | 2 | 2 |
| 1 | 0 | 0 |
| 1 | 1 | 1 |
| 2 | 2 | 2 |
| 0 | 0 | 0 |
| 2 | 2 | 1 |
| 2 | 2 | 2 |
| 2 | 2 | 2 |
| 2 | 2 | 2 |
| 2 | 2 | 2 |
| 2 | 2 | 2 |
| 0 | 0 | 0 |
| 1 | 0 | 1 |
| 2 | 2 | 2 |
| 2 | 2 | 2 |
| TOTAL: | 27 | 24 | 24 |
| Number of Participants | Effect | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Studies | Study Design (s) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Intervention | Alternative Intervention | Relative (95% CI) | Absolute (95% CI) | Quality | Importance |
| The outcomes achieved by molar intrusion with skeletal anchorage | ||||||||||||
| The change in overbite on the incisors | ||||||||||||
| 5 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding | 77 | 15 | 3.2 4.9 | moderate | important | |
| The change in lower facial height | ||||||||||||
| 4 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding, low ss | 51 | 15 | moderate | important | ||
| Mandibular autorotation | ||||||||||||
| 5 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding | 77 | 15 | −2.2 −1.4 | moderate | important | |
| The change in overbite on the incisors (1-year follow-up) | ||||||||||||
| 5 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding | 77 | 15 | moderate | important | ||
| The change in lower facial height (1-year follow-up) | ||||||||||||
| 4 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding, low ss | 18 | 15 | low | not important | ||
| Mandibular distorotation (1-year follow-up) | ||||||||||||
| 4 | non-RCT, Coh, CS | moderate | not serious | not serious | not serious | no blinding, low ss | 44 | 15 | moderate | important | ||
| The outcomes achieved by orthognathic surgery procedures | ||||||||||||
| The change in overbite on the incisors | ||||||||||||
| 4 | Coh, CS | moderate | not serious | not serious | not serious | no blinding | 141 | 2.4 3.6 | moderate | important | ||
| Mandibular autorotation | ||||||||||||
| 4 | Coh, CS | moderate | not serious | not serious | not serious | no blinding | 141 | −4.8 −2.2 | moderate | important | ||
| The change in overbite on the incisors (1-year follow-up) | ||||||||||||
| 2 | Coh | moderate | not serious | not serious | not serious | no blinding | 107 | moderate | important | |||
| Study | Type of Intervention | Study Design | Number of Patients | Mean Age of Patients or Range (Years) | Mean Active Treatment Time (Months) | Analyzed Measurements for This Review | Maximum Follow-Up Time (Years) |
|---|---|---|---|---|---|---|---|
| Baek et al. 2010 | Molar intrusion with mini-implants and elastomeric chain and transpalatal bar | Prospective | 9 | 23.7 | 7.8 | Overbite SN-GoMe anterior face height; U6-PP | 3 |
| Scheffler et al. 2014 | Temporary anchorage devices in the zygomatic buttress area connected to the acrylic splint with NiTi coil springs | Retrospective | 33 | 24.1 | 6.6 | Overbite SN-GoGn lower face height U6-PP | 2 |
| Sugawara et al. 2002 | Zygomatic mini-plates | Retrospective | 9 | 21.1 | 14.9 | Overbite; MP-FH lower face height U6-PP | 1 |
| Deguchi et al. 2011 | Miniscrews on the buccal side of molar area with power chain or ligature wire | Prospective, Non-randomized Clinical trial | 15 | 25.7 | 36 | Overbite SN-MP; U6-PP lower face height | 2 |
| Marzouk and Kassem 2016 | Zygomatic titanium mini-plates fixed with 3 screws | Retrospective | 26 | 22.5 | 7.5 | Overbite SN-MP; U6-PP | 3 |
| Ding et al. 2007 | Surgical-orthodontic, LefFort I and BSSO; fixation with plates and screws | Retrospective | 10 | 24.5 | NA | Overbite SN-MP SN-PP; MP-PP | 15 |
| Teittinen et al. 2012 | surgical-orthodontic, maxillary or bimaxillary | Retrospective | 24 12 maxillary 12 bimaxillary | 29.3 (maxillary) 30.8 (bimaxillary) | NA | Overbite SN-MP SN-PP; MP-PP | 3 |
| Swinnen et al. 2001 | surgical-orthodontic, maxillary or bimaxillary | Retrospective | 49 | 20.9 (women) 20.1 (men) | NA | Overbite SN-PP; N-Me ANS-Me | 1 |
| Fischer et al. 2000 | surgical-orthodontic, LefFort I and BSSO | Retrospective | 58 | 23 | NA | Overbite SN-MP MP-PP | 1 |
| Proffit et al. 2000 | surgical-orthodontic, maxillary or bimaxillary | Retrospective | 54 28 maxillary 26 bimaxillary | 21.8 (maxillary) 24.5 (bimaxillary) | NA | Overbite Mandibular plane change Maxillary plane change | 3 |
| Measurement | Type of Measurement | Definition of the Measurement |
|---|---|---|
| Overbite | Linear | Distance between the incisal edges of the upper central incisor (U1) and the lower central incisor (L1) perpendicular to the horizontal reference line (HRL) |
| SN-GoMe | Angular | Angle formed by the line going through cephalometric points sella (S)–nasion (N) and the line passing through the points gonion (Go)–menton (Me) |
| SN-GoGn | Angular | Angle formed by the line passing through cephalometric points sella (S)-nasion (N) and the line passing through the points gonion (Go)–gnathion (Gn) |
| MP-PP | Angular | Angle formed by the mandibular plane (MP) and the palatal plane (PP) |
| FMA | Angular | Angle formed by Frankfort horizontal plane and mandibular plane |
| SN-MP | Angular | Angle formed by the line going through cephalometric points sella (S)–nasion (N) and mandibular plane |
| SN-PP | Angular | Angle formed by the line going through cephalometric points sella (S)–nasion (N) and palatal plane |
| MP-FH | Angular | Angle formed by mandibular plane (MP) and Frankfort horizontal plane (FH); synonym of FMA |
| N-Me | Linear | Distance between nasion (N) and menton (Me) |
| ANS-Me | Linear | Distance between anterior nasal spine (ANS) and menton (Me) |
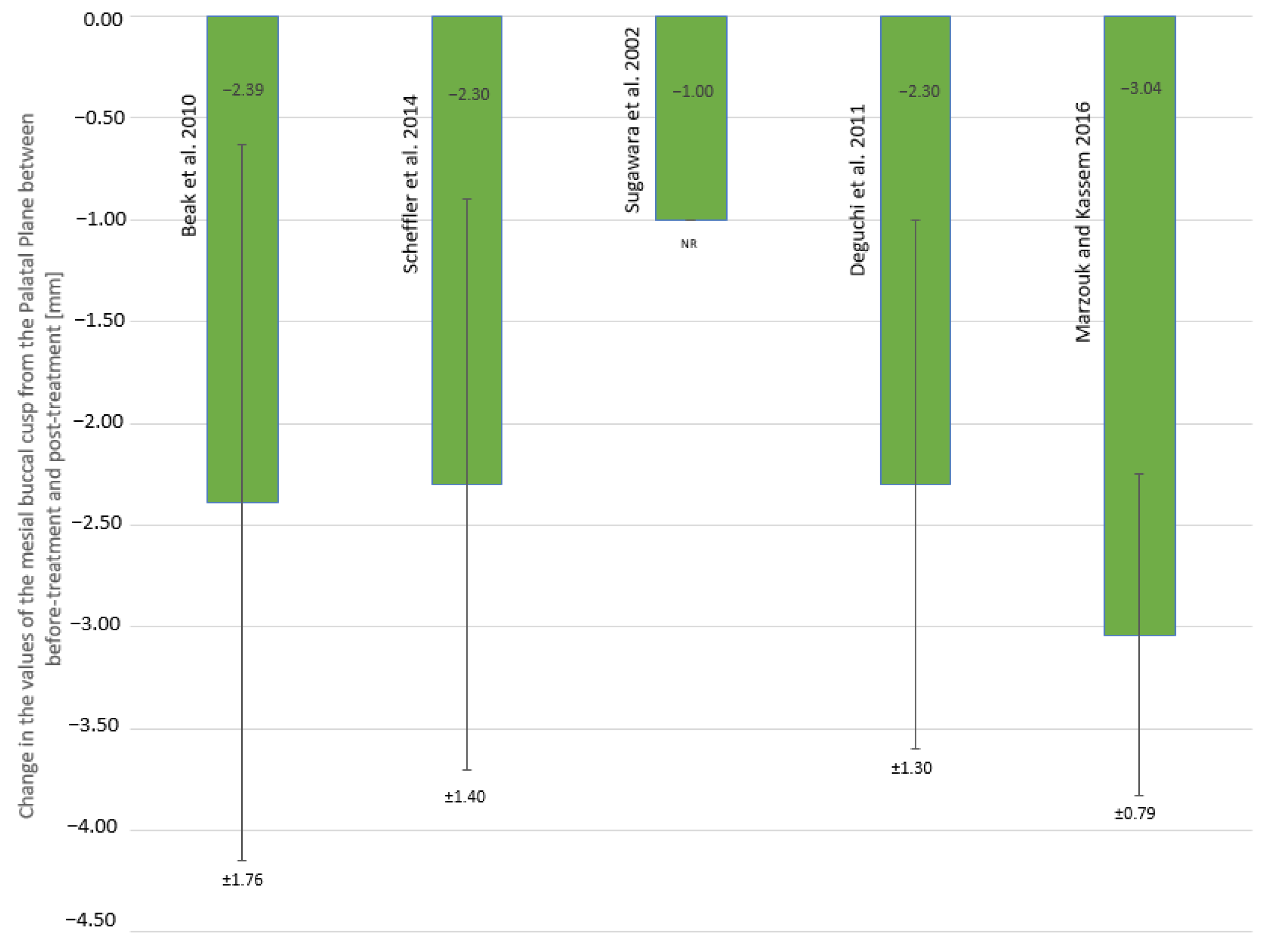
| U6-PP | Liner | Perpendicular distance between mesiobuccal cusp of the upper first molar and palatal plane (PP) |
| U6-HRL | Linear | Perpendicular distance between mesiobuccal cusp of the upper first molar and horizontal reference line (HRL) |
| Anterior face height (AFH) | Linear | Distance between nasion (N) and menton (Me) |
| Lower face height (LFH) | Linear | Distance between anterior nasal spine (ANS) and menton (Me) |
| Study | Pre-Treatment Mean (SD) | Post-Treatment Mean (SD) | Change in Mean (SD) |
|---|---|---|---|
| Baek et al. 2010 | −3.91 (1.65) | 1.65 (0.82) | 5.56 (1.94) * |
| Scheffler et al. 2014 | −1.2 (1.7) | 1.0 (NR) | 2.2 (1.6) SNR |
| Sugawara et al. 2002 | −2.8 (1.8) | 2.1 (0.8) | 4.9 (NR) SNR |
| Deguchi et al. 2011 | −4.4 (1.2) | 1.8 (1.1) | 6.2 (1.7) * |
| Marzouk and Kassem 2016 | −4.7 (2.3) | 2.18 (0.48) | 6.93 (1.99) ** |
| Study | Measurement | Pre-Treatment Mean (SD) | Post-Treatment Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|
| Baek et al. 2010 | AFH | 133.95 (5.55) | 131.41 (6.10) | −2.53 (1.90) |
| Scheffler et al. 2014 | LFH | NR | NR | −1.6 (2.2) |
| Sugawara et al. 2002 | LFH | 76.1 (5.8) | 74.6 (6.0) | −1.5 (NR) |
| Deguchi et al. 2011 | LFH | 74.7 (5.9) | 72.2 (5.1) | −2.6 (2.5) |
| Marzouk and Kassem 2016 | NR | NR | NR | NR |
| Study | Pre-Treatment Mean (SD) | Pre-Surgery Mean (SD) | Post-Surgery Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|
| Ding et al. 2007 | −3.2 (NR) | −3.2 (NR) | 0.6 (NR) | 3.8 (NR) |
| Teittinen et al. 2021 | NR NR | −2.55 (1.41) M −2.19 (1.44) B | 1.23 (1.05) M 0.98 (1.53) B | 3.78 (NR) M 3.17 (NR) B |
| Swinnen et al. 2001 | −0.7 MI −2.1 ME | −0.6 MI −1.9 ME | 1.3 MI 0.2 ME | 1.9 MI 2.1 ME |
| Fischer et al. 2000 | NR | −0.9 (2.6) | 1.3 (1.1) | 2.2 (2.4) |
| Proffit et al. 2000 | NR | NR | NR | NR |
| Study | Measurement | Pre-Treatment Mean (SD) | Pre-Surgery Mean (SD) | Post-Surgery Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|---|
| Swinnen et al. 2001 | N-Me | 139.1 MI 135.9 ME | 139.7 MI 137.1 ME | 134.2 MI 136.3 ME | −5.5 MI −0.8 ME |
| ANS-Me | 139.1 MI 135.9 ME | 139.7 MI 137.1 ME | 134.2 MI 136.3 ME | −5.5 MI −0.8 ME |
| Study | Measurement | Pre-Treatment Mean (SD) | Post-Treatment Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|
| Baek et al. 2010 | SN-GoMe | 45.44 (4.11) | 43.41 (4.41) | −2.03 (1.59) |
| Scheffler et al. 2014 | SN-GoGn | NR | NR | −1.2 (1.0) |
| Sugawara et al. 2002 | MP-FH | 33.1 (2.1) | 31.7 (2.4) | −1.3 (NR) |
| Deguchi et al. 2011 | MP-SN | 45.8 (6.0) | 42.2 (6.7) | −3.6 (2.1) |
| Marzouk and Kassem 2016 | MP-SN | 49.1 (3.1) | 46.9 (3.9) | −2.13 (0.21) |
| Study | Measurement | Pre-Treatment Mean (SD) | Pre-Surgery Mean (SD) | Post-Surgery Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|---|
| Ding et al. 2007 | PP-SN | 11.0 (NR) | 11.0 (NR) | 15.8 (NR) | 4.8 (NR) |
| MP-SN | 42.0 (NR) | 42.5 (NR) | 41.2 (NR) | −1.3 (NR) | |
| MP-PP | 31.1 (NR) | 31.1 (NR) | 25.0 (NR) | −6.1 (NR) | |
| Teittinen et al. 2021 | PP-SN | NR | 5.15 (2.16) M | 9.59 (3.23) M | 4.44 (NR) M |
| 5.49 (3.91) B | 8.27 (3.91) B | 2.78 (NR) B | |||
| MP-SN | NR | 38.15 (6.33) M | 34.17 (7.30) M | −3.95 (NR) M | |
| 42.08 (9.27) B | 37.48 (8.47) B | −4.6 (NR) B | |||
| MP-PP | NR | 32.98 (6.57) M | 26.17 (5.78) M | −6.81 (NR) M | |
| 36.57 (9.40) B | 29.24 (7.10) B | −7.33 (NR) B | |||
| Swinnen et al. 2001 | PP-SN | 7.9 (NR) MI | 7.8 (NR) MI | 9.2 (NR) MI | 1.4 (NR) MI |
| 8.9 (NR) ME | 9.4 (NR) ME | 11.8 (NR) ME | 2.4 (NR) ME | ||
| Fischer et al. 2000 | MP-SN | 46.2 (6.8) | 42.2 (6.7) | −4.0 (3.1) | |
| MP-PP | 39.6 (6.0) | 35.0 (6.6) | −4.6 (4.6) | ||
| Proffit et al. 2000 | NR | NR | NR | NR | NR |
| Study | Measurement | Pre-Treatment Mean (SD) | 1-Year Follow-Up Mean (SD) | Change in Mean (SD) | 2-Year Follow-Up Mean (SD) | Change in Mean (SD) | 3-Year Follow-Up Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|---|---|---|---|
| Baek et al. 2010 | Overbite | 1.65 (0.82) | 0.66 (0.79) | −0.99 * | NR | NR | 0.45 (1.09) | −0.44 * |
| AFH | 131.41 (6.10) | 131.86 (5.54) | 0.45 * | NR | NR | 132.32 (5.87) | 0.91 * | |
| SN-GoMe | 43.41 (4.41) | 43.68 (4.88) | 0.29 * | NR | NR | 43.98 (4.76) | 0.57 * | |
| U6-PP | 24.50 (1.64) | 24.89 (1.69) | 0.39 * | NR | NR | 24.94 (1.68) | 0.44 * | |
| Scheffler et al. 2014 | Overbite | 1.0 (NR) | 0.7 (NR) | −0.3 * | 0.3 (NR) | −0.7 * | NR | NR |
| LFH | NR | NR | 0.2 (1.4) | NR | 0.3 (1.4) | NR | NR | |
| SN-GoGn | NR | NR | 0.0 (NR) | NR | 0.0 (NR) | NR | NR | |
| U6-PP | NR | NR | 0.5 (1.1) | NR | 1.0 * (1.1) | NR | NR | |
| Sugawara et al. 2002 | Overbite | 2.1 (0.8) | 1.2 (0.8) | −0.9 * | NR | NR | NR | NR |
| LFH | 74.6 (6.0) | 75.2 (5.8) | 0.6 * | NR | NR | NR | NR | |
| MP-FH | 31.7 (2.4) | 32.2 (3.0) | 0.5 * | NR | NR | NR | NR | |
| U6-PP | 25.0 (2.8) | 25.1 (2.5) | 0.1 * | NR | NR | NR | NR | |
| Deguchi et al. 2011 | Overbite | 1.8 (1.1) | 1.0 (0.9) | −0.8 | NR | NR | NR | NR |
| LFH | 72.2 (5.1) | 72.2 (5.1) | 0.0 * | NR | NR | NR | NR | |
| MP-SN | 42.2 (6.7) | 43.8 (6.5) | 1.6 * | NR | NR | NR | NR | |
| U6-PP | 24.6 (2.5) | 25.1 (2.8) | 0.5 * | NR | NR | NR | NR | |
| Marzouk and Kassem 2016 | Overbite | 2.18 (0.48) | 1.61 (0.42) | −0.57 * | NR | NR | 1.41 (0.39) | −0.2 * |
| MP-SN | 46.9 (3.9) | 47.2 (3.9) | 0.3 * | NR | NR | 47.4 (3.9) | 0.2 * | |
| U6-PP | 25.23 (2.14) | 25.54 (2.17) | 0.31 | NR | NR | 25.64 (2.17) | 0.10 * |
| Study | Observation Time (Years) | Measurement | Post-Surgery Mean (SD) | Follow-Up Mean (SD) | Change in Mean (SD) |
|---|---|---|---|---|---|
| Ding et al. 2007 | 15 | Overbite | 0.6 (NR) | 1.5 (NR) | 0.9 (NR) |
| PP-SN | 15.8 (NR) | 13 (NR) | −2.6 (NR) | ||
| MP-SN | 41.2 (NR) | 42.1 (NR) | 0.9 (NR) | ||
| MP-PP | 25.0 (NR) | 28 (NR) | 2.9 (NR) | ||
| Teittinen et al. 2021 | 3.5 | Overbite | 1.23 (1.05) M | 1.85 (0.93) M | 0.62 * M |
| 0.98 (1.53) B | 0.73 (0.93) B | −0.25 B | |||
| PP-SN | 9.59 (3.23) M | 7.45 (3.08) M | −2.14 M | ||
| 8.27 (3.91) B | 7.06 (4.14) B | −1.21 B | |||
| MP-SN | 34.17 (7.30) M | 35.84 (5.95) M | 1.67 M | ||
| 37.48 (8.47) B | 41.25 (10.37) M | 3.77 B | |||
| MP-PP | 26.17 (5.78) M | 28.38 (5.80) B | 2.21 M | ||
| 29.24 (7.10) B | 34.20 (8.78) M | 4.96 B | |||
| Swinnen et al. 2001 | 1 | Overbite | 1.3 (NR) MI | 1.8 (NR) MI | 0.5 * MI |
| 0.2 (NR) ME | 0.8 (NR) ME | 0.6 * ME | |||
| PP-NS | 9.2 (NR) MI | 8.0 (NR) MI | −1.2 * MI | ||
| 11.8 (NR) ME | 9.3 (NR) ME | −2.5 * ME | |||
| N-Me | 134.2 (NR) MI | 133.6 (NR) MI | −0.6 * MI | ||
| 136.3 (NR) ME | 134.2 (NR) ME | −2.1 * ME | |||
| ANS-Me | 81.3 (NR) MI | 81.7 (NR) MI | 0.4 * MI | ||
| 76.3 (NR) ME | 75.4 (NR) ME | −0.9 * ME | |||
| Fischer et al. 2000 | 1 | Overbite | 1.3 (2.6) | 0.8 (1.4) | −0.5 (1.3) |
| MP-SN | 42.2 (6.7) | 43.7 (6.7) | 1.4 (2.0) | ||
| MP-PP | 35.0 (6.6) | 36.7 (6.3) | 1.7 (2.8) | ||
| Proffit et al. 2000 | 3 | Overbite | NR | NR | 0.02 (1.21) M |
| NR | NR | −0.25 (1.25) B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malara, P.; Bierbaum, S.; Malara, B. Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review. J. Clin. Med. 2021, 10, 5682. https://doi.org/10.3390/jcm10235682
Malara P, Bierbaum S, Malara B. Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review. Journal of Clinical Medicine. 2021; 10(23):5682. https://doi.org/10.3390/jcm10235682
Chicago/Turabian StyleMalara, Piotr, Susanne Bierbaum, and Beata Malara. 2021. "Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review" Journal of Clinical Medicine 10, no. 23: 5682. https://doi.org/10.3390/jcm10235682
APA StyleMalara, P., Bierbaum, S., & Malara, B. (2021). Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review. Journal of Clinical Medicine, 10(23), 5682. https://doi.org/10.3390/jcm10235682







