A Review of Robotic-Assisted Bronchoscopy Platforms in the Sampling of Peripheral Pulmonary Lesions
Abstract
1. Introduction
2. Brief History
3. Robotic-Assisted Bronchoscopy
3.1. Monarch Robotic System
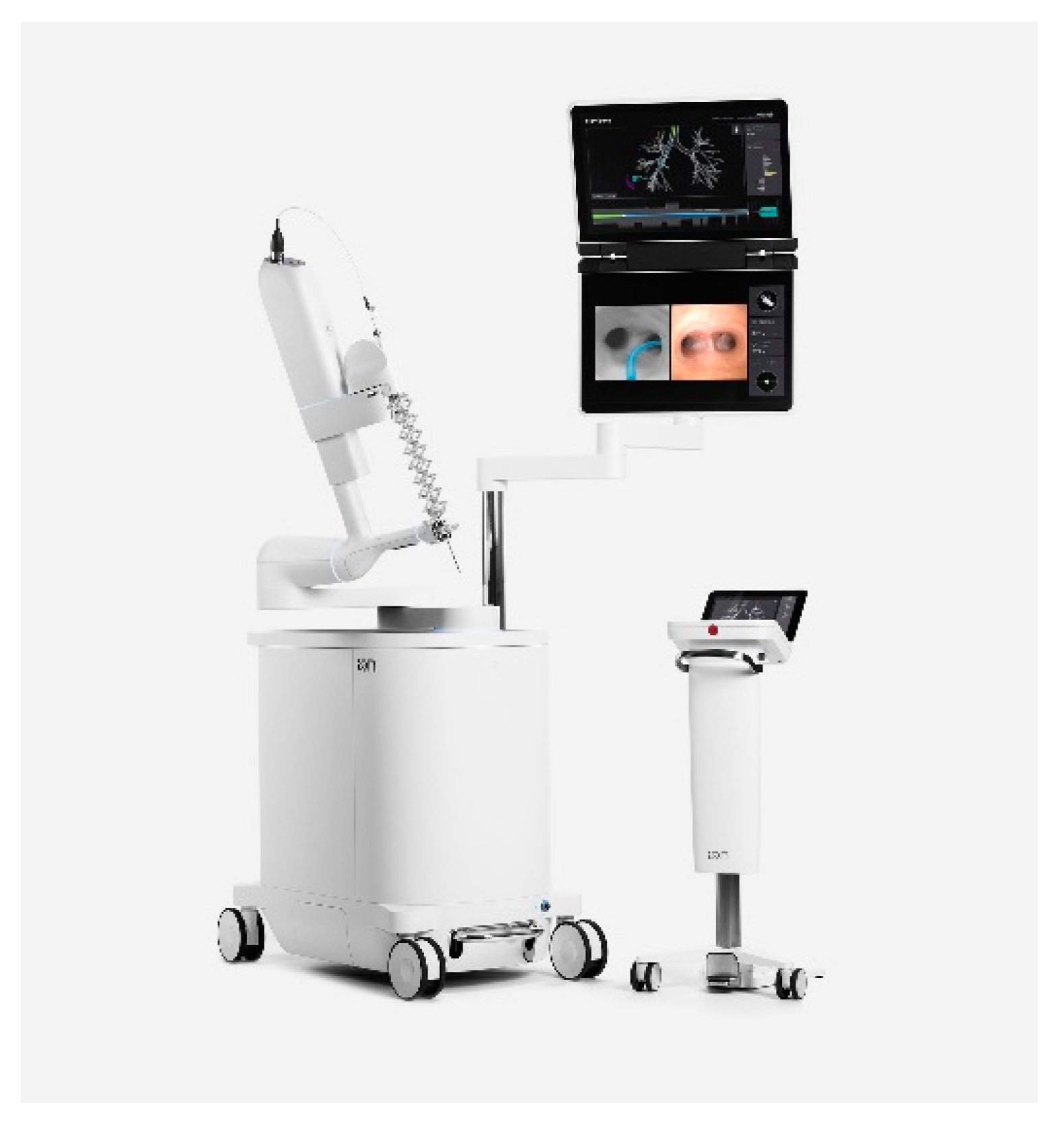
3.2. Ion Endoluminal
4. Further Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- U.S. Cancer Statistics Data Visualizations Tool, Based on 2020 Submission Data (1999–2018). June 2021. Available online: www.cdc.gov/cancer/dataviz (accessed on 9 November 2021).
- Team TNLSTR. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef]
- Yousaf-Khan, U.; Van Der Aalst, C.; De Jong, P.A.; Heuvelmans, M.; Scholten, E.; Lammers, J.-W.; van Ooijen, P.; Nackaerts, K.; Weenink, C.; Groen, H.; et al. Final screening round of the NELSON lung cancer screening trial: The effect of a 2.5-year screening interval. Thorax 2017, 72, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Murgu, S.D. Robotic assisted-bronchoscopy: Technical tips and lessons learned from the initial experience with sampling peripheral lung lesions. BMC Pulm. Med. 2019, 19, 89. [Google Scholar] [CrossRef]
- Gould, M.K.; Donington, J.; Lynch, W.R.; Mazzone, P.J.; Midthun, D.E.; Naidich, D.; Wiener, R. Evaluation of Individuals With Pulmonary Nodules: When Is It Lung Cancer? Chest 2013, 143, e93S–e120S. [Google Scholar] [CrossRef] [PubMed]
- Heerink, W.J.; de Bock, G.H.; De Jonge, G.J.; Groen, H.J.; Vliegenthart, R.; Oudkerk, M. Complication rates of CT-guided transthoracic lung biopsy: Meta-analysis. Eur. Radiol. 2017, 27, 138–148. [Google Scholar] [CrossRef]
- Arnold, B.N.; Thomas, D.C.; Narayan, R.; Blasberg, J.D.; Detterbeck, F.C.; Boffa, D.J.; Kim, A.W. Robotic-Assisted Lobectomies in the National Cancer Database. J. Am. Coll. Surg. 2018, 226, 1052–1062.e15. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Han, Y.; Gan, Q.; Xiang, J.; Jin, R.; Chen, K.; Che, J.; Hang, J.; Li, H. Early Outcomes of Robot-Assisted Versus Thoracoscopic-Assisted Ivor Lewis Esophagectomy for Esophageal Cancer: A Propensity Score-Matched Study. Ann. Surg. Oncol. 2019, 26, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Epstein, A.J.; Groeneveld, P.W.; Harhay, M.O.; Yang, F.; Polsky, D. Impact of Minimally Invasive Surgery on Medical Spending and Employee Absenteeism. JAMA Surg. 2013, 148, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Cisu, T.C.F.; Carbonara, U.; Porpiglia, F.; Autorino, R. New robotic surgical systems in urology: An update. Curr. Opin. Urol. 2021, 31, 37–42. [Google Scholar] [CrossRef]
- Chen, K.; MBeeraka, N.; Zhang, J.; Reshetov, I.V.; Nikolenko, V.N.; Sinelnikov, M.Y.; Mikhaleva, L.M. Efficacy of da Vinci robot-assisted lymph node surgery than conventional axillary lymph node dissection in breast cancer—A comparative study. Int. J. Med. Robot. Comput. Assist. Surg. 2021, 17, e2307. [Google Scholar] [CrossRef]
- Panchabhai, T.S.; Mehta, A.C. Historical Perspectives of Bronchoscopy. Connecting the Dots. Ann. Am. Thorac. Soc. 2015, 12, 631–641. [Google Scholar] [CrossRef]
- Hurter, T.; Hanrath, P. Endobronchial sonography: Feasibility and preliminary results. Thorax 1992, 47, 565–567. [Google Scholar] [CrossRef]
- Tanner, N.T.; Yarmus, L.; Chen, A.; Memoli, J.W.; Mehta, H.J.; Pastis, N.J.; Lee, H.; Jantz, M.A.; Nietert, P.J.; Silvestri, G.A. Standard Bronchoscopy with Fluoroscopy vs. Thin Bronchoscopy and Radial Endobronchial Ultrasound for Biopsy of Pulmonary Lesions. Chest 2018, 154, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Gildea, T.R.; Mazzone, P.J.; Karnak, D.; Meziane, M.; Mehta, A.C. Electromagnetic Navigation Diagnostic Bronchoscopy. Am. J. Respir. Crit. Care Med. 2006, 174, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Ost, D.E.; Ernst, A.; Lei, X.; Kovitz, K.L.; Benzaquen, S.; Diaz-Mendoza, J.; Greenhill, S.; Toth, J.; Feller-Kopman, D.; Puchalski, J.; et al. Diagnostic Yield and Complications of Bronchoscopy for Peripheral Lung Lesions. Results of the AQuIRE Registry. Am. J. Respir. Crit. Care Med. 2016, 193, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Gex, G.; Pralong, J.A.; Combescure, C.; Seijo, L.; Rochat, T.; Soccal, P.M. Diagnostic Yield and Safety of Electromagnetic Navigation Bronchoscopy for Lung Nodules: A Systematic Review and Meta-Analysis. Respiration 2014, 87, 165–176. [Google Scholar] [CrossRef]
- Memoli, J.S.W.; Nietert, P.J.; Silvestri, G.A. Meta-analysis of Guided Bronchoscopy for the Evaluation of the Pulmonary Nodule. Chest 2012, 142, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Aboudara, M.; Roller, L.; Rickman, O.; Lentz, R.J.; Pannu, J.; Chen, H.; Maldonado, F. Improved diagnostic yield for lung nodules with digital tomosynthesis-corrected navigational bronchoscopy: Initial experience with a novel adjunct. Respirology 2019, 25, 206–213. [Google Scholar] [CrossRef]
- Yarmus, L.B.; Arias, S.; Feller-Kopman, D.; Semaan, R.; Wang, K.P.; Frimpong, B.; Burgess, K.O.; Thompson, R.; Chen, A.; Ortiz, R.; et al. Electromagnetic navigation transthoracic needle aspiration for the diagnosis of pulmonary nodules: A safety and feasibility pilot study. J. Thorac. Dis. 2016, 8, 186–194. [Google Scholar] [PubMed]
- DiBardino, D.M.; Yarmus, L.B.; Semaan, R.W. Transthoracic needle biopsy of the lung. J. Thorac. Dis. 2015, 7, S304–S316. [Google Scholar] [PubMed]
- Zhang, W.; Chen, S.; Dong, X.; Lei, P. Meta-analysis of the diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules. J. Thorac. Dis. 2015, 7, 799–809. [Google Scholar] [PubMed]
- Seijo, L.M. Electromagnetic navigation bronchoscopy: Clinical utility in the diagnosis of lung cancer. Lung Cancer Targets Ther. 2016, 7, 111–118. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zuñiga PV, S.; Vakil, E.; Molina, S.; Bassett, R.L., Jr.; Ost, D.E. Sensitivity of Radial Endobronchial Ultrasound-Guided Bronchoscopy for Lung Cancer in Patients With Peripheral Pulmonary Lesions: An Updated Meta-Analysis. Chest 2020, 157, 994–1011. [Google Scholar] [CrossRef]
- Eberhardt, R.; Anantham, D.; Ernst, A.; Feller-Kopman, D.; Herth, F. Multimodality Bronchoscopic Diagnosis of Peripheral Lung Lesions. Am. J. Respir. Crit. Care Med. 2007, 176, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Oki, M.; Saka, H.; Ando, M.; Asano, F.; Kurimoto, N.; Morita, K.; Kitagawa, C.; Kogure, Y.; Miyazawa, T. Ultrathin Bronchoscopy with Multimodal Devices for Peripheral Pulmonary Lesions. A Randomized Trial. Am. J. Respir. Crit. Care Med. 2015, 192, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Chaddha, U.; Kovacs, S.P.; Manley, C.; Hogarth, D.K.; Cumbo-Nacheli, G.; Bhavani, S.V.; Kumar, R.; Shende, M.; Egan, J.P.; Murgu, S. Robot-assisted bronchoscopy for pulmonary lesion diagnosis: Results from the initial multicenter experience. BMC Pulm. Med. 2019, 19, 243. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.C.; Pastis, N.J.; Mahajan, A.K.; Khandhar, S.J.; Simoff, M.J.; Machuzak, M.S.; Cicenia, J.; Gildea, T.R.; Silvestri, G.A. Robotic Bronchoscopy for Peripheral Pulmonary Lesions. Chest 2021, 159, 845–852. [Google Scholar] [CrossRef]
- Fielding, D.I.; Bashirzadeh, F.; Son, J.H.; Todman, M.; Chin, A.; Tan, L.; Steinke, K.; Windsor, M.N.; Sung, A.W. First Human Use of a New Robotic-Assisted Fiber Optic Sensing Navigation System for Small Peripheral Pulmonary Nodules. Respiration 2019, 98, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Kalchiem-Dekel, O.; Connolly, J.G.; Lin, I.-H.; Husta, B.C.; Adusumilli, P.S.; Beattie, J.A.; Buonocore, D.J.; Dycoco, J.; Fuentes, P.; Jones, D.R.; et al. Shape-Sensing Robotic-Assisted Bronchoscopy in the Diagnosis of Pulmonary Parenchymal Lesions. Chest 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.C.; Gillespie, C.T. Robotic Endoscopic Airway Challenge: REACH Assessment. Ann. Thorac. Surg. 2018, 106, 293–297. [Google Scholar] [CrossRef]
- Chen, A.C.; Pastis, N.J.; Machuzak, M.S.; Gildea, T.R.; Simoff, M.J.; Gillespie, C.T.; Mahajan, A.K.; Oh, S.S.; Silvestri, G.A. Accuracy of a Robotic Endoscopic System in Cadaver Models with Simulated Tumor Targets: ACCESS Study. Respiration 2020, 99, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Solano, J.R.; Ugalde-Gamboa, L.; Machuzak, M. Robotic Bronchoscopy for Diagnosis of Suspected Lung Cancer. J. Bronchol. Interv. Pulmonol. 2018, 25, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Yarmus, L.; Akulian, J.; Wahidi, M.; Chen, A.; Steltz, J.P.; Solomon, S.L.; Yu, D.; Maldonado, F.; Cardenas-Garcia, J.; Molena, D.; et al. A Prospective Randomized Comparative Study of Three Guided Bronchoscopic Approaches for Investigating Pulmonary Nodules: The PRECISION-1 Study. Chest 2020, 157, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Coyan, G.N.; Lu, M.; Ruppert, K.M.; Baker, N.; Levy, R.M.; Luketich, J.D.; Schuchert, M.J.; Sarkaria, I.S. Activity-Based Cost Analysis of Robotic Anatomic Lung Resection During Program Implementation. Ann. Thorac. Surg. 2021, 21, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Ekeke, C.N.; Vercauteren, M.; Istvaniczdravkovic, S.; Semaan, R.; Dhupar, R. Lung Nodule Evaluation Using Robotic-Assisted Bronchoscopy at a Veteran’s Affairs Hospital. J. Clin. Med. 2021, 10, 3671. [Google Scholar] [CrossRef] [PubMed]

| Lesion Size (mm) | Diagnostic Sensitivity | Pneumothorax Rate | |
|---|---|---|---|
| Guided Bronchoscopy * [18] | NS | 70% | 1.5% |
| CT-guided Transthoracic Needle Biopsy [21] | NS | 92.1% | 20.5% |
| Robotic Platform Studies | |||
| Chaddha et al. [27] (n = 165) | 25.0 ± 15.0 | 69.1–77% | 3.6% |
| Chen et al. (BENEFIT study) [28] (n = 54) | 23.2 ± 10.8 | 74.1% | 3.7% |
| Fielding et al. [29] (n = 29) | 15.3 ± 4.8 | 79.3% | 0% |
| Kalchiem-Dekel et al. [30] (n = 130) | 18.0 ± 9.0 | 79.8% | 1.5% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, M.; Nath, S.; Semaan, R.W. A Review of Robotic-Assisted Bronchoscopy Platforms in the Sampling of Peripheral Pulmonary Lesions. J. Clin. Med. 2021, 10, 5678. https://doi.org/10.3390/jcm10235678
Lu M, Nath S, Semaan RW. A Review of Robotic-Assisted Bronchoscopy Platforms in the Sampling of Peripheral Pulmonary Lesions. Journal of Clinical Medicine. 2021; 10(23):5678. https://doi.org/10.3390/jcm10235678
Chicago/Turabian StyleLu, Michael, Sridesh Nath, and Roy W. Semaan. 2021. "A Review of Robotic-Assisted Bronchoscopy Platforms in the Sampling of Peripheral Pulmonary Lesions" Journal of Clinical Medicine 10, no. 23: 5678. https://doi.org/10.3390/jcm10235678
APA StyleLu, M., Nath, S., & Semaan, R. W. (2021). A Review of Robotic-Assisted Bronchoscopy Platforms in the Sampling of Peripheral Pulmonary Lesions. Journal of Clinical Medicine, 10(23), 5678. https://doi.org/10.3390/jcm10235678





