Proportion of Thick versus Thin Melanomas as a Benchmarking Tool
Abstract
1. Introduction
2. Material and Methods
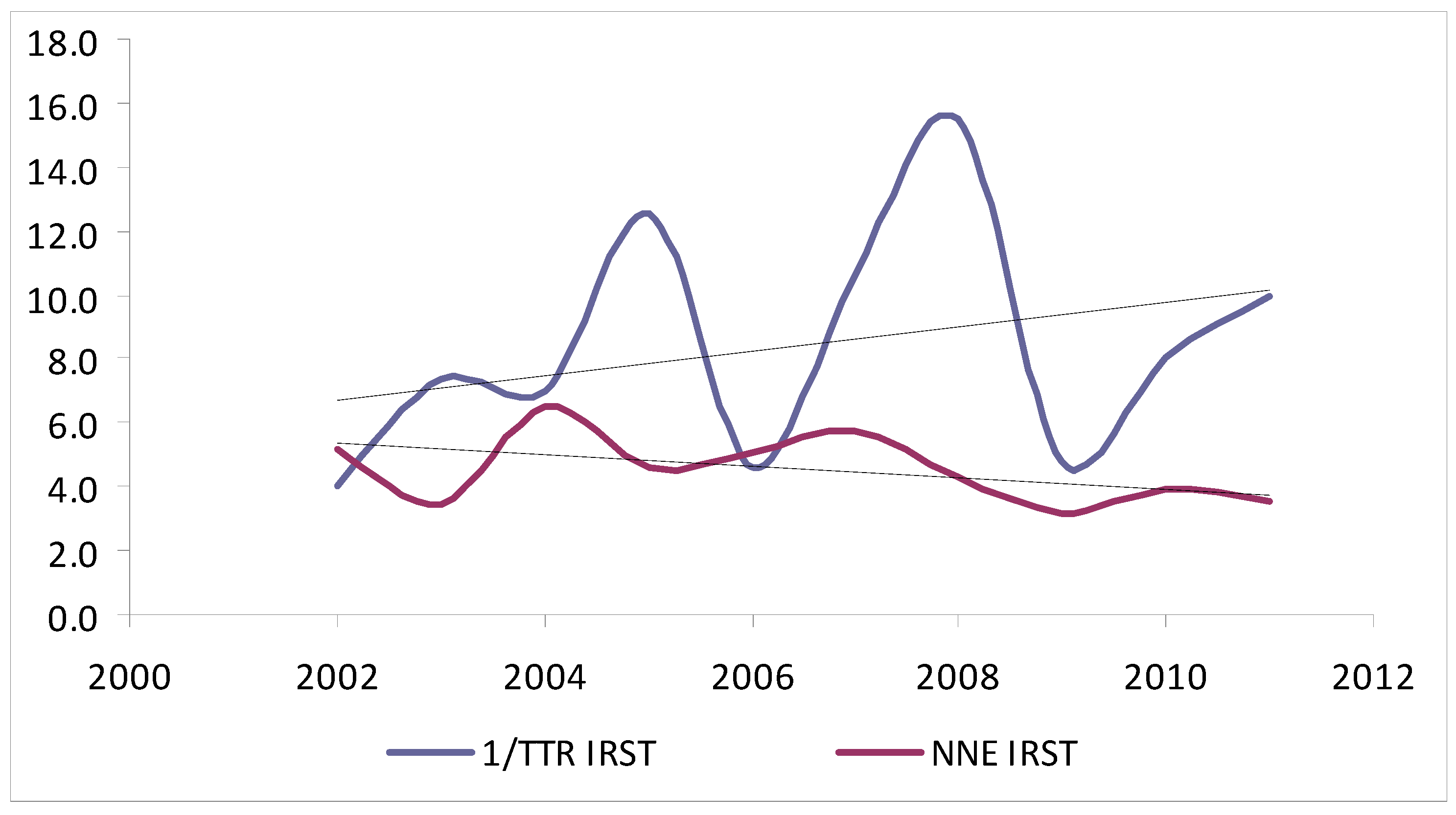
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Osborne, J.E.; Chave, T.A.; Hutchinson, P.E. Comparison of diagnostic accuracy for cutaneous malignant melanoma between general dermatology, plastic surgery and pigmented lesion clinics. Br. J. Dermatol. 2003, 148, 252–258. [Google Scholar] [CrossRef] [PubMed]
- English, D.R.; Del Mar, C.; Burton, R.C. Factors influencing the number needed to excise: Excision rates of pigmented lesions by general practitioners. Med. J. Aust. 2004, 180, 16–19. [Google Scholar] [CrossRef]
- Wilkinson, D.; Askew, D.A.; Dixon, A. Skin cancer clinics in Australia: Workload profile and performance indicators from an analysis of billing data. Med. J. Aust. 2006, 184, 162–164. [Google Scholar] [CrossRef]
- Hansen, C.; Wilkinson, D.; Hansen, M.; Argenziano, G. How good are skin cancer clinics at melanoma detection? Number needed to treat variability across a national clinic group in Australia. J. Am. Acad. Dermatol. 2009, 61, 599–604. [Google Scholar] [CrossRef]
- Sidhu, S.; Bodger, O.; Williams, N.; Roberts, D.L. The number of benign moles excised for each malignant melanoma: The number needed to treat. Clin. Exp. Dermatol. 2012, 37, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Rosendahl, C.; Williams, G.; Eley, D.; Wilson, T.; Canning, G.; Keir, J.; McColl, I.; Wilkinson, D. The impact of subspecialization and dermatoscopy use on accuracy of melanoma diagnosis among primary care doctors in Australia. J. Am. Acad. Dermatol. 2012, 67, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Argenziano, G.; Cerroni, L.; Zalaudek, I.; Staibano, S.; Hofmann-Wellenhof, R.; Arpaia, N.; Bakos, R.M.; Balme, B.; Bandic, J.; Bandelloni, R.; et al. Accuracy in melanoma detection: A 10-year multicenter survey. J. Am. Acad. Dermatol. 2012, 67, 54–59. [Google Scholar] [CrossRef]
- Carli, P.; De Giorgi, V.; Crocetti, E.; Mannone, F.; Massi, D.; Chiarugi, A.; Giannotti, B. Improvement of malignant/benign ratio in excised melanocytic lesions in the ‘dermoscopy era’: A retrospective study 1997–2001. Br. J. Dermatol. 2004, 150, 687–692. [Google Scholar] [CrossRef]
- Tromme, I.; Sacré, L.; Hammouch, F.; Legrand, C.; Marot, L.; Vereecken, P.; Theate, I.; van Eeckhout, P.; Richez, P.; Baurain, J.; et al. Availability of digital dermoscopy in daily practice dramatically reduces the number of excised melanocytic lesions: Results from an observational study. Br. J. Dermatol. 2012, 167, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Ahnlide, I.; Nielsen, K.; Bjellerup, M. Diagnosis of pigmented skin tumours in a dermatological setting: Different aspects of the number needed to excise as a measure of efficiency. Acta Derm. Venereol. 2014, 94, 683–686. [Google Scholar] [CrossRef]
- Alarcon, I.; Carrera, C.; Palou, J.; Alos, L.; Malvehy, J.; Puig, S. Impact of in vivo reflectance confocal microscopy on the number needed to treat melanoma in doubtful lesions. Br. J. Dermatol. 2014, 170, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Pellacani, G.; Pepe, P.; Casari, A.; Longo, C. Reflectance confocal microscopy as a second-level examination in skin oncology improves diagnostic accuracy and saves unnecessary excisions: A longitudinal prospective study. Br. J. Dermatol. 2014, 171, 1044–1051. [Google Scholar] [CrossRef]
- Balch, C.M.; Gershenwald, J.E.; Soong, S.; Thompson, J.F.; Atkins, M.B.; Byrd, D.R.; Buzaid, A.C.; Cochran, A.J.; Coit, D.G.; Ding, S.; et al. Final Version of 2009 AJCC Melanoma Staging and Classification. J. Clin. Oncol. 2009, 27, 6199–6206. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Menchón, T.; Sánchez-Pedreño, P.; Martínez-Escribano, J.; Corbalán-Vélez, R.; Martínez-Barba, E. Cost analysis of sentinel lymph node biopsy in melanoma. Actas Dermosifiliogr. 2015, 106, 201–207. [Google Scholar] [CrossRef] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology: Melanoma. 2013. Available online: http://www.nccn.org/professionals/physician_gls/pdf/melanoma.pdf (accessed on 5 June 2017).
- Dummer, R.; Guggenheim, M.; Arnold, A.W.; Braun, R.; von Moos, R. Task Force Skin Cancer. Updated Swiss guidelines for the treatment and follow-up of cutaneous melanoma. Swiss. Med. Wkly. 2011, 141, w13320. [Google Scholar]
- Garbe, C.; Hauschild, A.; Volkenandt, M.; Schadendorf, D.; Stolz, W.; Reinhold, U.; Kortmann, R.-D.; Kettelhack, C.; Frerich, B.; Keilholz, U.; et al. Evidence and interdisciplinary consense-based German guidelines: Diagnosis and surveillance of melanoma. Melanoma Res. 2007, 17, 393–399. [Google Scholar] [CrossRef]
- Pehamberger, H.; Binder, M.; Knollmayer, S.; Wolff, K. Immediate effects of a public education campaign on prognostic features of melanoma. J. Am. Acad. Dermatol 1993, 29, 106–109. [Google Scholar] [CrossRef]
- Beam, C.A.; Conant, E.F.; Sickles, E.A. Correlation of radiologist rank as a measure of skill in screening and diagnostic interpretation of mammograms. Radiology 2006, 238, 446–453. [Google Scholar] [CrossRef]
- Esdaile, B.; Mahmud, I.; Palmer, A.; Bowling, J. Diagnosing melanoma: How do we assess how good we are? Clin. Exp. Dermatol. 2014, 39, 129–134. [Google Scholar] [CrossRef]
- Betti, R.; Moneghini, L.; Vergani, R.; Cerri, A. Diagnostic performance parameters for melanocytic lesions before and during the dermoscopy era. Eur. J. Dermatol. 2017, 27, 174–175. [Google Scholar] [CrossRef]
- Aires, D.J.; Wick, J.; Shaath, T.S.; Rajpara, A.N.; Patel, V.; Badawi, A.H.; Li, C.; Fraga, G.R.; Doolittle, G.; Liu, D.Y. Economic costs avoided by diagnosing melanoma six months earlier justify >100 benign biopsies. J. Drugs Dermatol. 2016, 15, 527–532. [Google Scholar] [PubMed]
- Pagliarello, C.; Stanganelli, I.; Fabrizi, G.; Feliciani, C.; Nuzzo, S. Digital dermoscopy monitoring: Is it time to define a quality standard? Acta Derm. Venereol. 2017, 97, 864–865. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Buist, D.S.; Anderson, M.L.; Smith, R.A.; Carney, P.A.; Miglioretti, D.L.; Monsees, B.S.; Sickles, E.A.; Taplin, S.H.; Geller, B.M.; Yankaskas, B.C.; et al. Effect of radiologists’ diagnostic work-up volume on interpretive performance. Radiology 2014, 273, 351–364. [Google Scholar] [CrossRef] [PubMed]

| IRST | Parma | p | |
|---|---|---|---|
| OVERALL EXCISED LESION | 1604 | 15,134 | |
| EXCISED NEVI | 1308 | 13,828 | |
| Age (mean ± SD) | 38.57 ± 13.77 | 36.97 ± 15.6 | <0.001 |
| Gender (%) | |||
| Male | 553 (42%) | 5633 (41%) | NS |
| Female | 755 (58%) | 8195 (59%) | |
| Location (%) | |||
| Head and neck | 110 (8.5%) | 2080 (16.5%) | <0.001 |
| Trunk | 846 (65.5%) | 7029 (55%) | |
| Arms | 90 (7%) | 1177 (9.5%) | |
| Legs | 212 (16.5%) | 1400 (11%) | |
| Acral | 34 (2.5%) | 1033 (8%) | |
| EXCISED MELANOMA | 296 | 1306 | |
| Gender (%) | |||
| Male | 139 (47%) | 592 (45%) | NS |
| Female | 157 (53%) | 714 (55%) | |
| Mean age ± SD | 53.8 ± 18 | 56.3 ± 18 | <0.05 |
| Mean Breslow ± SD | 0.56 ± 0.89 | 1.07 ± 2.2 | NS |
| Median Breslow (range) | 0.4 (9) | 0.4 (30) | NS |
| Melanoma type (%) | <0.001 | ||
| In situ | 94 (31.8%) | 510 (39.1%) | |
| Breslow ≤ 1 mm | 166 (56.1%) | 482 (36.9%) | |
| Breslow >1 mm | 36 (12.2%) | 314 (24%) | |
| Thin melanoma (%) | 260 (87.8%) | 992 (76%) | <0.001 |
| Thick melanoma (%) | 36 (12.2%) | 314 (24%) | |
| Gender (%) | |||
| Male | |||
| Thin melanoma | 124 (89.2%) | 421 (71.1%) * | |
| Thick melanoma | 15 (10.8%) | 171 (28.9%) * | |
| Female | |||
| Thin melanoma | 136 (86.6%) | 571 (80%) * | |
| Thick melanoma | 21 (13.4%) | 143 (20%) * | |
| Location (%) | <0.001 | ||
| Head and neck | 29 (10%) | 220 (18%) | |
| Trunk | 156 (53%) | 458 (38%) | |
| Arms | 41 (14%) | 171 (14%) | |
| Legs | 64 (22%) | 280 (23%) | |
| Acral | 3 (1%) | 90 (7%) | |
| Head and neck (%) | NS | ||
| Thin melanoma | 26 (89.7%) | 178 (80.9%) | |
| Thick melanoma | 3 (10.3%) | 42 (19.1%) | |
| Trunk (%) | NS | ||
| Thin melanoma | 136 (87.2%) | 368 (80.3%) | |
| Thick melanoma | 20 (12.8%) | 90 (19.7%) | |
| Arms (%) | <0.01 | ||
| Thin melanoma | 38 (92.7%) | 125 (73.1%) | |
| Thick melanoma | 3 (7.3%) | 46 (26.9%) | |
| Legs (%) | NS | ||
| Thin melanoma | 55 (85.9%) | 218 (77.9%) | |
| Thick melanoma | 9 (14.1%) | 62 (22.1%) | |
| Acral (%) | NS | ||
| Thin melanoma | 3 (100%) | 43 (47.8%) | |
| Thick melanoma | 0 (0%) | 47 (52.2%) | |
| OVERALL NNE | 4.42 | 10.6 | |
| Male NNE | 3.98 | 9.52 | |
| Female NNE | 4.81 | 11.48 | |
| Head and neck NNE | 3.79 | 9.45 | |
| Trunk NNE | 5.42 | 15.35 | |
| Arms NNE | 2.19 | 6.88 | |
| Legs NNE | 3.31 | 5 | |
| Acral NNE | 11.33 | 11.47 |
| Thick vs. Thin | Thick vs. Thin | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | |||||
| OR | 95% CI | p | OR | 95% CI | p | |
| Centre | ||||||
| IRST | 1 | – | <0.001 | 1 | – | <0.01 |
| Parma | 2.3 | 1.6–3.3 | 1.8 | 1.2–2.7 | ||
| Gender | ||||||
| Female | 1 | – | <0.001 | 1 | – | <0.01 |
| Male | 1.5 | 1.1–1.9 | 1.5 | 1.2–2 | ||
| Location | ||||||
| Head and neck | 1 | – | <0.001 | 1 | – | <0.001 |
| Trunk | 0.9 | 0.7–1.4 | 1.5 | 0.9–2.2 | ||
| Arms | 1.4 | 0.9–2.1 | 1.8 | 1.1–2.9 | ||
| Legs | 1.2 | 0.8–18 | 2 | 1.2–3 | ||
| Acral | 4.6 | 2.7–7.8 | 5.6 | 3.3–9.6 | ||
| Age (for each ten-year increase) | 1.2 | 1.2-1.3 | <0.001 | 1.2 | 1.1–1.3 | <0.001 |
| RCM | <0.01 | NS | ||||
| No | 3.4 | 1.3–8.5 | 1.9 | 0.7–5.2 | ||
| Yes | – | – | – | – | ||
| 0–9 | 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | 90–99 | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EXCISED NEVI | |||||||||||
| IRST (%) | 14 (1.1) | 82 (6.3) | 213 (16.3) | 438 (33.6) | 319 (24.5) | 125 (9.6) | 72 (5.5) | 34 (2.6) | 7 (0.5) | 0 (0) | <0.001 |
| Parma (%) | 218 (1.6) | 1622 (11.8) | 2679 (19.4) | 3916 (28.4) | 2647 (19.2) | 1361 (9.9) | 890 (6.5) | 355 (2.6) | 84 (0.6) | 10 (0.1) | |
| EXCISED MELANOMA | |||||||||||
| Overall | |||||||||||
| IRST (%) | 0 (0) | 1 (0.3) | 27 (9.2) | 54 (18.3) | 56 (19) | 41 (13.9) | 37 (12.5) | 57 (19.3) | 21 (7.1) | 1 (0.3) | <0.05 |
| Parma (%) | 0 (0) | 11 (0.8) | 71 (5.4) | 207 (15.8) | 218 (16.7) | 210 (16.1) | 217 (16.6) | 222 (17) | 132 (10.1) | 18 (1.4) | |
| Thin | |||||||||||
| IRST (%) | 0 (0) | 1 (0.4) | 25 (9.7) | 46 (17.8) | 51 (19.7) | 36 (13.9) | 34 (13.1) | 49 (18.9) | 16 (6.2) | 1 (0.4) | NS |
| Parma (%) | 0 (0) | 8 (0.8) | 63 (6.4) | 182 (18.3) | 169 (17) | 160 (16.1) | 166 (16.7) | 152 (15.3) | 88 (8.9) | 4 (0.4) | |
| Thick | |||||||||||
| IRST (%) | 0 (0) | 0 (0) | 2 (5.6) | 8 (22.2) | 5 (13.9) | 5 (13.9) | 3 (8.3) | 8 (22.2) | 5 (13.9) | 0 (0) | NS |
| Parma (%) | 0 (0) | 3 (1) | 8 (2.5) | 25 (8) | 49 (15.6) | 50 (15.9) | 51 (16.2) | 70 (22.3) | 44 (14) | 14 (4.5) | |
| NNE IRST | NA | 82 | 7.9 | 8.1 | 5.7 | 3 | 1.9 | 0.6 | 0.3 | NA | <0.001 |
| Thick/thin (TTR) IRST | n/a | n/a | 0.08 | 0.17 | 0.10 | 0.14 | 0.09 | 0.16 | 0.31 | n/a | NS |
| NNE Parma | NA | 147 | 37.7 | 18.9 | 12.1 | 6.5 | 4.1 | 0.6 | 0.6 | 0.55 | <0.001 |
| Thick/Thin (TTR) Parma | n/a | 0.37 | 0.13 | 0.14 | 0.29 | 0.31 | 0.30 | 0.45 | 0.50 | 3.33 | <0.001 |
| Excised melanoma IRST | |||||||||||
| Thin (%) | 0 (0) | 1 (0.4) | 25 (9.7) | 46 (17.8) | 51 (19.7) | 36 (13.9) | 34 (13.1) | 49 (18.9) | 16 (6.2) | 1 (0.4) | NS |
| Thick (%) | 0 (0) | 0 (0) | 2 (5.6) | 8 (22.2) | 5 (13.9) | 5 (13.9) | 3 (8.3) | 8 (22.2) | 5 (13.9) | 0 (0) | |
| Excised melanoma Parma | |||||||||||
| Thin (%) | 0 | 8 (0.8) | 63 (6.4) | 182 (18.3) | 169 (17) | 160 (16.1) | 166 (16.7) | 152 (15.3) | 88 (8.9) | 4 (0.4) | <0.001 |
| Thick (%) | 0 | 3 (1) | 8 (2.5) | 25 (8) | 49 (15.6) | 50 (15.9) | 51 (16.2) | 70 (22.3) | 44 (14) | 14 (4.5) |
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EXCISED NEVI | |||||||||||
| IRST (%) | 157 (12) | 142 (10.9) | 157 (12) | 124 (9.5) | 144 (11) | 131 (10) | 141 (10.8) | 92 (7) | 105 (8) | 115 (8.8) | <0.001 |
| Parma (%) | 765 (5.5) | 1018 (7.4) | 1235 (8.9) | 1637 (11.8) | 1415 (10.2) | 1482 (10.7) | 1589 (11.5) | 1537 (11.1) | 1553 (11.2) | 1597 (11.5) | |
| EXCISED MELANOMA | |||||||||||
| Overall | |||||||||||
| IRST (%) | 30 (0) | 42 (0.3) | 24 (9.2) | 27 (18.3) | 28 (19) | 23 (13.9) | 33 (12.5) | 29 (19.3) | 27 (7.1) | 33 (0.3) | <0.001 |
| Parma (%) | 57 (4.4) | 91 (7) | 105 (8) | 133 (10.2) | 150 (11.5) | 154 (11.8) | 120 (9.2) | 158 (12.1) | 149 (11.4) | 189 (14.5) | |
| Thin | |||||||||||
| IRST (%) | 24 (9.2) | 37 (14.2) | 21 (8.1) | 25 (9.6) | 23 (8.8) | 21 (8.1) | 31 (11.9) | 24 (9.2) | 24 (9.2) | 30 (11.5) | <0.001 |
| Parma (%) | 35 (3.5) | 70 (7.1) | 64 (6.5) | 100 (10.1) | 117 (11.8) | 113 (11.4) | 85 (8.6) | 120 (12.1) | 126 (12.7) | 162 (16.3) | |
| Thick | |||||||||||
| IRST (%) | 6 (16.7) | 5 (13.9) | 3 (8.3) | 2 (5.6) | 5 (13.9) | 2 (5.6) | 2 (5.6) | 5 (13.9) | 3 (8.3) | 3 (8.3) | NS |
| Parma (%) | 22 (7) | 21 (6.7) | 41 (13.1) | 33 (10.5) | 33 (10.5) | 41 (13.1) | 35 (11.1) | 38 (12.1) | 23 (7.3) | 27 (8.6) | |
| NNE IRST | 5.2 | 3.4 | 6.5 | 4.6 | 5.1 | 5.7 | 4.3 | 3.2 | 3.9 | 3.5 | NS |
| TTR IRST | 0.25 | 0.14 | 0.14 | 0.08 | 0.22 | 0.09 | 0.06 | 0.21 | 0.12 | 0.10 | NS |
| NNE Parma | 13.4 | 11.2 | 11.8 | 12.3 | 9.4 | 9.6 | 13.2 | 9.7 | 10.4 | 8.4 | <0.01 |
| TTR Parma | 0.62 | 0.30 | 0.62 | 0.33 | 0.29 | 0.36 | 0.42 | 0.31 | 0.18 | 0.17 | <0.01 |
| Excised melanoma IRST | |||||||||||
| Thin | 24 (9.2) | 37 (14.2) | 21 (8.1) | 25 (9.6) | 23 (8.8) | 21 (8.1) | 31 (11.9) | 24 (9.2) | 24 (9.2) | 30 (11.5) | NS |
| Thick | 6 (16.7) | 5 (13.9) | 3 (8.3) | 2 (5.6) | 5 (13.9) | 2 (5.6) | 2 (5.6) | 5 (13.9) | 3 (8.3) | 3 (8.3) | |
| Excised melanoma Parma | |||||||||||
| Thin | 35 (3.5) | 70 (7.1) | 64 (6.5) | 100 (10.1) | 117 (11.8) | 113 (11.4) | 85 (8.6) | 120 (12.1) | 126 (12.7) | 162 (16.3) | <0.001 |
| Thick | 22 (7) | 21 (6.7) | 41 (13.1) | 33 (10.5) | 33 (10.5) | 41 (13.1) | 35 (11.1) | 38 (12.1) | 23 (7.3) | 27 (8.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pagliarello, C.; Magi, S.; Mazzoni, L.; Stanganelli, I. Proportion of Thick versus Thin Melanomas as a Benchmarking Tool. J. Clin. Med. 2021, 10, 5545. https://doi.org/10.3390/jcm10235545
Pagliarello C, Magi S, Mazzoni L, Stanganelli I. Proportion of Thick versus Thin Melanomas as a Benchmarking Tool. Journal of Clinical Medicine. 2021; 10(23):5545. https://doi.org/10.3390/jcm10235545
Chicago/Turabian StylePagliarello, Calogero, Serena Magi, Laura Mazzoni, and Ignazio Stanganelli. 2021. "Proportion of Thick versus Thin Melanomas as a Benchmarking Tool" Journal of Clinical Medicine 10, no. 23: 5545. https://doi.org/10.3390/jcm10235545
APA StylePagliarello, C., Magi, S., Mazzoni, L., & Stanganelli, I. (2021). Proportion of Thick versus Thin Melanomas as a Benchmarking Tool. Journal of Clinical Medicine, 10(23), 5545. https://doi.org/10.3390/jcm10235545







