Anterior Cervical Corpectomy with Fusion versus Anterior Hybrid Fusion Surgery for Patients with Severe Ossification of the Posterior Longitudinal Ligament Involving Three or More Levels: A Retrospective Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Methods
2.2. Operative Technique
2.2.1. Anterior Cervical Corpectomy with Fusion (ACCF Group)
2.2.2. Anterior Hybrid Procedure (Corpectomy-Discectomy with Fusion, Hybrid Group)
2.3. Clinical Evaluations
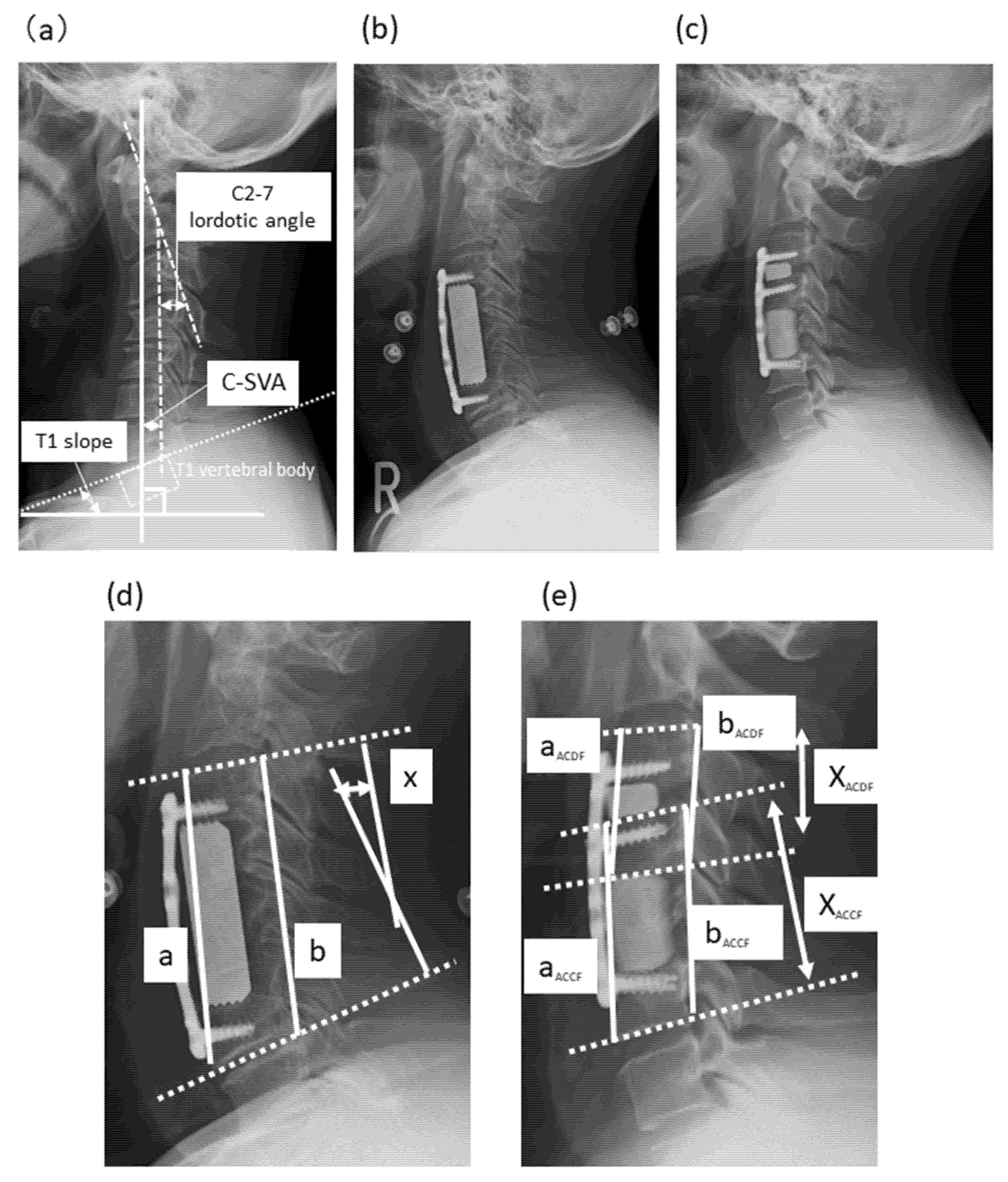
2.4. Radiologic Evaluations
2.5. Statistical Analysis
3. Results
3.1. Demographic Data and Clinical Outcomes
3.2. Radiographic Outcomes
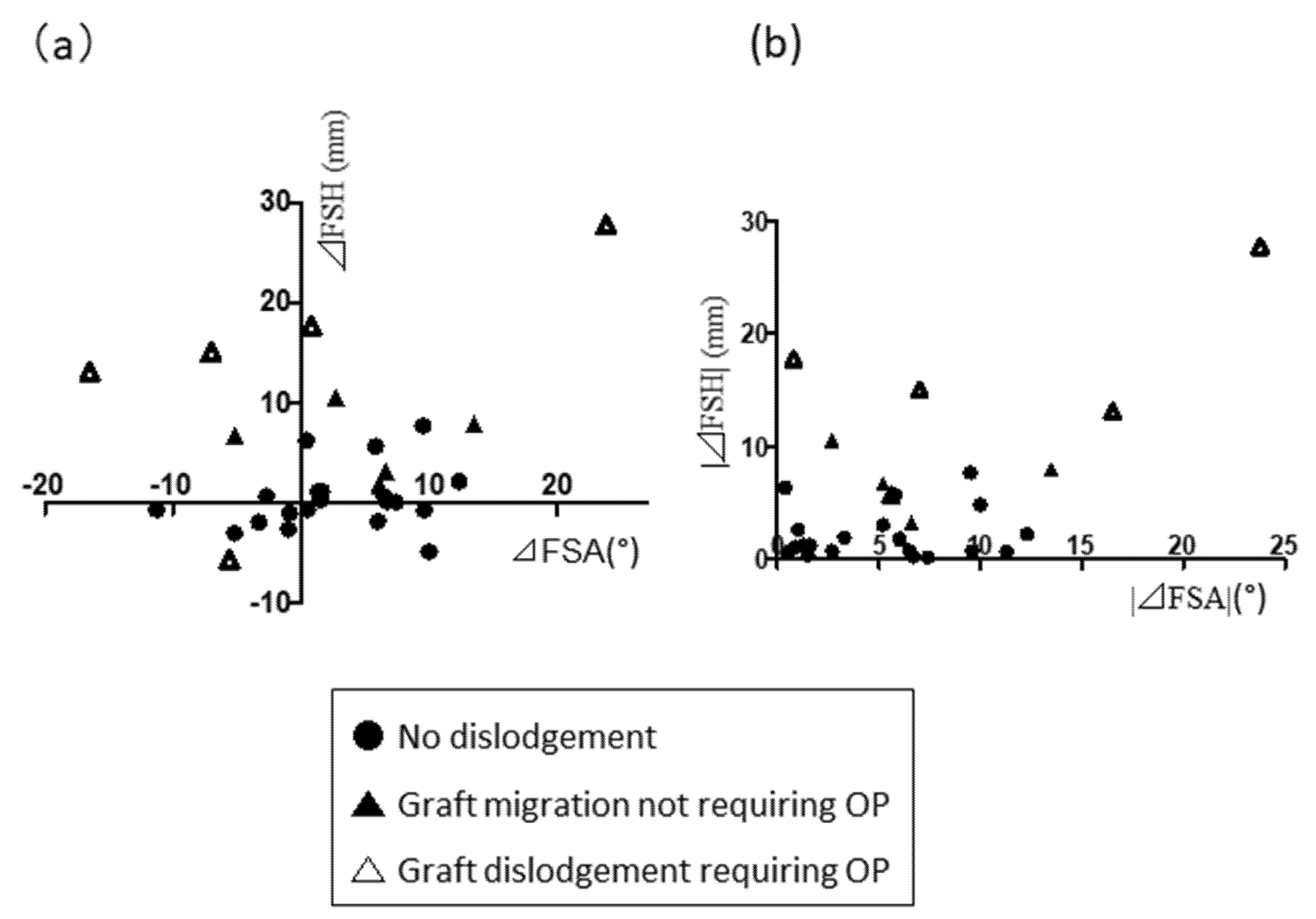
3.3. Association of Change in FSH Immediately Postoperatively with Strut Subsidence in the ACCF Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Matsunaga, S.; Kukita, M.; Hayashi, K.; Shinkura, R.; Koriyama, C.; Sakou, T.; Komiya, S. Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J. Neurosurg. 2002, 96, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Sakou, T. Ossification of the posterior longitudinal ligament of the cervical spine: Etiology and natural history. Spine (Phila Pa 1976) 2012, 37, E309–E314. [Google Scholar] [CrossRef]
- Sasaki, E.; Ono, A.; Yokoyama, T.; Wada, K.; Tanaka, T.; Kumagai, G.; Iwasaki, H.; Takahashi, I.; Umeda, T.; Nakaji, S.; et al. Prevalence and symptom of ossification of posterior longitudinal ligaments in the Japanese general population. J. Orthop. Sci. 2014, 19, 405–411. [Google Scholar] [CrossRef]
- Nouri, A.; Martin, A.R.; Mikulis, D.; Fehlings, M.G. Magnetic resonance imaging assessment of degenerative cervical myelopathy: A review of structural changes and measurement techniques. Neurosurg. Focus 2016, 40, E5. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Okuda, S.; Miyauchi, A.; Sakaura, H.; Mukai, Y.; Yonenobu, K.; Yoshikawa, H. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976) 2007, 32, 647–653. [Google Scholar] [CrossRef]
- Iwasaki, M.; Okuda, S.; Miyauchi, A.; Sakaura, H.; Mukai, Y.; Yonenobu, K.; Yoshikawa, H. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976) 2007, 32, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Sumi, M. Updates on ossification of posterior longitudinal ligament. Conservative treatments for OPLL. Clin. Calcium. 2009, 19, 1480–1485, doi:CliCa091014801485. [Google Scholar] [PubMed]
- Yoshii, T.; Sakai, K.; Hirai, T.; Yamada, T.; Inose, H.; Kato, T.; Enomoto, M.; Tomizawa, S.; Kawabata, S.; Arai, Y.; et al. Anterior decompression with fusion versus posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a ≥50% canal occupying ratio: A multicenter retrospective study. Spine J. 2016, 16, 1351–1357. [Google Scholar] [CrossRef]
- Youssef, J.A.; Heiner, A.D.; Montgomery, J.R.; Tender, G.C.; Lorio, M.P.; Morreale, J.M.; Phillips, F.M. Outcomes of posterior cervical fusion and decompression: A systematic review and meta-analysis. Spine J. 2019, 19, 1714–1729. [Google Scholar] [CrossRef] [Green Version]
- Hirai, T.; Okawa, A.; Arai, Y.; Takahashi, M.; Kawabata, S.; Kato, T.; Enomoto, M.; Tomizawa, S.; Sakai, K.; Torigoe, I.; et al. Middle-term results of a prospective comparative study of anterior decompression with fusion and posterior decompression with laminoplasty for the treatment of cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2011, 36, 1940–1947. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.D.; Mancini, N.; Karukonda, T.; Cote, M.; Moss, I.L. Comparative and Predictor Analysis of 30-day Readmission, Reoperation, and Morbidity in Patients Undergoing Multilevel ACDF Versus Single and Multilevel ACCF Using the ACS-NSQIP Dataset. Spine (Phila Pa 1976) 2019, 44, E1379–E1387. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, E.; Smorgick, Y.; Rand, N.; Millgram, M.A.; Mirovsky, Y.; Floman, Y. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: A hybrid decompression and fixation technique. J. Neurosurg. Spine 2005, 3, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Qi, M.; Chen, H.; Yang, L.; Wang, X.; Shi, G.; Gao, R.; Wang, C.; Yuan, W. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur. Spine J. 2012, 21, 2428–2435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei-Bing, X.; Wun-Jer, S.; Gang, L.; Yue, Z.; Ming-Xi, J.; Lian-Shun, J. Reconstructive techniques study after anterior decompression of multilevel cervical spondylotic myelopathy. J. Spinal Disord. Tech. 2009, 22, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Badhiwala, J.H.; Leung, S.N.; Ellenbogen, Y.; Akbar, M.A.; Martin, A.R.; Jiang, F.; Wilson, J.R.F.; Nassiri, F.; Witiw, C.D.; Wilson, J.R.; et al. A comparison of the perioperative outcomes of anterior surgical techniques for the treatment of multilevel degenerative cervical myelopathy. J. Neurosurg. Spine 2020, 1–8. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Sakai, K.; Yoshii, T.; Hirai, T.; Arai, Y.; Torigoe, I.; Tomori, M.; Sato, H.; Okawa, A. Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kphotic alignment. Spine (Phila Pa 1976) 2016, 41, 299–305. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.H.; Lee, S.Y.; Kim, Y.C.; Park, M.S.; Kim, S.W. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 2013, 38, E992–E997. [Google Scholar] [CrossRef]
- Kim, M.K.; Kim, S.M.; Jeon, K.M.; Kim, T.S. Radiographic comparison of four anterior fusion procedures in two level cervical disc diseases: Autograft plate fixation versus cage plate fixation versus stand-alone cage fusion versus corpectomy and plate fixation. J. Korean Neurosurg. Soc. 2012, 51, 135–140. [Google Scholar] [CrossRef]
- Hirai, T.; Yoshii, T.; Egawa, S.; Sakai, K.; Inose, H.; Yuasa, M.; Yamada, T.; Ushio, S.; Kato, T.; Arai, Y.; et al. Increased height of fused segments contributes to early-phase strut dislodgement after anterior cervical corpectomy with fusion for multilevel ossification of the posterior longitudinal ligament. Spine Surg. Relat. Res. 2020, 4, 294–299. [Google Scholar] [CrossRef] [Green Version]
- Sakai, K.; Okawa, A.; Takahashi, M.; Arai, Y.; Kawabata, S.; Enomoto, M.; Kato, T.; Hirai, T.; Shinomiya, K. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: A prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976) 2012, 37, 367–376. [Google Scholar] [CrossRef]
- Fujiyoshi, T.; Yamazaki, M.; Kawabe, J.; Endo, T.; Furuya, T.; Koda, M.; Okawa, A.; Takahashi, K.; Konishi, H. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: The K-line. Spine (Phila Pa 1976) 2008, 33, E990–E993. [Google Scholar] [CrossRef]
- Hirai, T.; Kawabata, S.; Enomoto, M.; Kato, T.; Tomizawa, S.; Sakai, K.; Yoshii, T.; Sakaki, K.; Shinomiya, K.; Okawa, A. Presence of anterior compression of the spinal cord after laminoplasty inhibits upper extremity motor recovery in patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012, 37, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Caspar, W.; Pitzen, T.; Papavero, L.; Geisler, F.H.; Johnson, T.A. Anterior cervical plating for the treatment of neoplasms in the cervical vertebrae. J. Neurosurg. 1999, 90, 27–34. [Google Scholar] [CrossRef]
- Hou, Y.; Liang, L.; Shi, G.D.; Xu, P.; Xu, G.H.; Shi, J.G.; Yuan, W. Comparing effects of cervical anterior approach and laminoplasty in surgical management of cervical ossification of posterior longitudinal ligament by a prospective nonrandomized controlled study. Orthop. Traumatol. Surg. Res. 2017, 103, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Li, Y.; Chen, Y.; Wu, W.; Zou, D. Cervical curvature, spinal cord MRIT2 signal, and occupying ratio impact surgical approach selection in patients with ossification of the posterior longitudinal ligament. Eur. Spine J. 2013, 22, 1480–1488. [Google Scholar] [CrossRef] [Green Version]
- Tani, T.; Ushida, T.; Ishida, K.; Iai, H.; Noguchi, T.; Yamamoto, H. Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine (Phila Pa 1976) 2002, 27, 2491–2498. [Google Scholar] [CrossRef]
- Ryu, W.H.A.; Platt, A.; Deutsch, H. Hybrid decompression and reconstruction technique for cervical spondylotic myelopathy: Case series and review of the literature. J. Spine Surg. 2020, 6, 181–195. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.M.; Peng, H.W.; Liu, Z.L.; Long, X.H.; Yu, Y.Q.; Huang, S.H. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: Which one is better? World Neurosurg. 2015, 84, 2022–2029. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Tian, X.M.; Liu, S.K.; Wang, H.; Zhang, Y.-Z.; Ding, W.-Y. Prevalence of complications after surgery in treatment for cervical compressive myelopathy: A meta-analysis for last decade. Medicine (Baltimore) 2017, 96, e6421. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Falatyn, S.P.; Scuderi, G.J.; Eismont, F.J.; McGuire, R.A.; Singh, K.; Garfin, S.R. Early failure of long segment anterior cervical plate fixation. J. Spinal Disord. 1998, 11, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Okawa, A.; Sakai, K.; Hirai, T.; Kato, T.; Tomizawa, S.; Enomoto, M.; Kawabata, S.; Takahashi, M.; Shinomiya, K. Risk factors for early reconstruction failure of multilevel cervical corpectomy with dynamic plate fixation. Spine (Phila Pa 1976) 2011, 36, E582–E587. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Vaccaro, A.R.; Kim, J.; Lorenz, E.P.; Lim, T.-H.; An, H.S. Enhancement of stability following anterior cervical corpectomy: A biomechanical study. Spine (Phila Pa 1976) 2004, 29, 845–849. [Google Scholar] [CrossRef]
- Nishimura, S.; Nagoshi, N.; Iwanami, A.; Takeuchi, A.; Hirai, T.; Yoshii, T.; Takeuchi, K.; Mori, K.; Yamada, T.; Seki, S.; et al. Prevalence and Distribution of Diffuse Idiopathic Skeletal Hyperostosis on Whole-spine Computed Tomography in Patients With Cervical Ossification of the Posterior Longitudinal Ligament: A Multicenter Study. Clin. Spine Surg. 2018, 31, E460–E465. [Google Scholar] [CrossRef]
- Hirai, T.; Nishimura, S.; Yoshii, T.; Nagoshi, N.; Hashimoto, J.; Mori, K.; Maki, S.; Katsumi, K.; Takeuchi, K.; Ushio, S.; et al. Associations between Clinical Findings and Severity of Diffuse Idiopathic Skeletal Hyperostosis in Patients with Ossification of the Posterior Longitudinal Ligament. J. Clin. Med. 2021, 10, 4137. [Google Scholar] [CrossRef]
- Hirai, T.; Yoshii, T.; Iwanami, A.; Takeuchi, K.; Mori, K.; Yamada, T.; Wada, K.; Koda, M.; Matsuyama, Y.; Takeshita, K.; et al. Prevalence and distribution of ossified lesions in the whole spine of patients with cervical ossification of the posterior longitudinal ligament a multicenter study (JOSL CT study). PLoS ONE 2016, 11, e0160117. [Google Scholar] [CrossRef] [Green Version]
- Mori, K.; Yoshii, T.; Hirai, T.; Iwanami, A.; Takeuchi, K.; Yamada, T.; Seki, S.; Tsuji, T.; Fujiyoshi, K.; Furukawa, M.; et al. Prevalence and distribution of ossification of the supra/interspinous ligaments in symptomatic patients with cervical ossification of the posterior longitudinal ligament of the spine: A CT-based multicenter cross-sectional study. BMC Musculoskelet. Disord. 2016, 17, 492. [Google Scholar] [CrossRef]
- Yoshii, T.; Hirai, T.; Iwanami, A.; Nagoshi, N.; Takeuchi, K.; Mori, K.; Yamada, T.; Seki, S.; Tsuji, T.; Fujiyoshi, K.; et al. Co-existence of ossification of the nuchal ligament is associated with severity of ossification in the whole spine in patients with cervical ossification of the posterior longitudinal ligament -A multi-center CT study. J. Orthop. Sci. 2019, 24, 35–41. [Google Scholar] [CrossRef]
- Aramomi, M.; Masaki, Y.; Koshizuka, S.; Kadota, R.; Okawa, A.; Koda, M.; Yamazaki, M. Anterior pedicle screw fixation for multilevel cervical corpectomy and spinal fusion. Acta Neurochir. 2008, 150, 575–582. [Google Scholar] [CrossRef] [PubMed]

| I Upper extremity motor function | ||
| 0: | Unable to feed oneself with any tableware including chopsticks, spoon, or fork, and/or unable to fasten buttons of any size | |
| 1: | Can manage to feed oneself with spoon and/or fork but not chopsticks | |
| 2: | Either chopsticks feeding or writing is possible but not practical, and/or large buttons can be fastened | |
| 3: | Either chopsticks feeding or writing is clumsy but practical, and/or cuff buttons can be fastened | |
| 4: | Normal | |
| II Lower extremity motor function | ||
| 0: | Unable to stand up and walk by any means | |
| 0.5: | Able to stand up but unable to walk | |
| 1: | Unable to walk without a cane or other support on level ground | |
| 1.5: | Able to walk without support but with a clumsy gait | |
| 2: | Walks independently on level ground but needs support on stairs | |
| 2.5: | Walks independently when going upstairs, but needs support when going downstairs | |
| 3: | Capable of walking fast but clumsily | |
| 4: | Normal | |
| III Sensory function | ||
| A. Upper extremity | ||
| 0: | Complete loss of touch and pain sensation | |
| 0.5: | 50% or below of normal sensation and/or severe pain or numbness | |
| 1: | Over 60% of normal sensation and/or moderate pain or numbness | |
| 1.5: | Subjective numbness of a slight degree without any objective sensory deficit | |
| 2: | Normal | |
| B. Lower extremity | ||
| Same as A | ||
| C. Trunk | ||
| Same as A | ||
| IV Bladder function | ||
| 0: | Urinary retention and/or incontinence | |
| 1: | Sensory of retention, dribbling, thin stream and/or incomplete continence | |
| 2: | Urinary retardation and/or pollakiuria | |
| 3: | Normal | |
| ACCF Group (n = 30) | Hybrid Group (n = 23) | p | |
|---|---|---|---|
| Age (years) | 61.7 ± 9.1 | 62.9 ± 10.5 | 0.71 |
| Male:Female | 24:6 | 17:6 | 0.74 |
| Diabetes mellitus (%) | 10 (33.3) | 6 (26.1) | 0.57 |
| History of smoking (%) | 12 (40) | 7 (30.4) | 0.47 |
| Preoperative JOA score (points) | 11.9 ± 2.1 | 11.1 ± 3.8 | 0.39 |
| Postoperative JOA score (points) | 15.0 ± 1.4 | 14.6 ± 2.3 | 0.50 |
| Recovery rate of JOA score (%) | 56.3 ± 32.1 | 70.4 ± 27.0 | 0.12 |
| No. of fused segments | 3.3 ± 0.6 | 3.5 ± 0.7 | 0.33 |
| Graft type in ACCF part | Artificial bone 20 Fibular graft 6 Iliac graft 4 | Artificial bone 20 Fibular graft 3 | 0.28 |
| Graft type in ACDF part | - | Artificial bone 20 fusion cage 3 | - |
| Estimated blood loss (mL) | 437 ± 778 | 197 ± 151 | 0.20 |
| Operating time (h) | 6.5 ± 2.4 | 6.0 ± 2.4 | 0.40 |
| Duration of ICU stay (days) | 2.8 ± 1.4 | 3.3 ± 2.6 | 0.39 |
| Time to postoperative extubation (days) | 0.5 ± 1.1 | 0.9 ± 2.6 | 0.55 |
| Hospital stay (days) | 24.2 ± 10.7 | 29.3 ± 12.3 | 0.55 |
| ACCF Group | Hybrid Group | p | |
|---|---|---|---|
| (n = 30) | (n = 23) | ||
| Complications, n (%) | |||
| Total | 12 (40%) | 4 (17.4%) | 0.08 |
| Dysphagia | 4 (13.3%) | 0 (0%) | 0.07 |
| Aspiration pneumonitis | 3 (10%) | 1 (4.3%) | 0.44 |
| Delirium | 2 (6.7%) | 1 (4.3%) | 0.72 |
| Segmental paralysis | 2 (6.7%) | 1 (4.3%) | 0.72 |
| DVT | 1 (3.3%) | 0 (0%) | 0.37 |
| Dyspnea (internal hematoma) | 0 (0%) | 1 (4.3%) | 0.24 |
| Revision surgery, n (%) | |||
| Total | 5 (16.7%) | 1 (5.3%) | 0.16 |
| Graft dislodgement | 5 (16.7%) | 0 (0%) | 0.04 * |
| Segmental paralysis | 0 (0%) | 1 (5.3%) | 0.24 |
| ACCF Group (n = 30) | Hybrid Group (n = 23) | p | ||||
|---|---|---|---|---|---|---|
| C2–7 angle (°) | Preoperative | 11.2 ± 11.4 | 9.7 ± 12.0 | 0.76 | ||
| Immediate postoperative | 13.0 ± 10.1 | 13.0 ± 11.7 | 0.94 | |||
| 1 year | 11.9 ± 9.8 | 12.6 ± 9.9 | 0.66 | |||
| C-SVA (mm) | Preoperative | 23.4 ± 14.9 | 21.4 ± 15.5 | 0.97 | ||
| Immediate postoperative | 27.6 ± 16.0 | 26.0 ± 13.5 | 0.59 | |||
| 1 year | 20.9 ± 13.5 | 16.9 ± 9.5 | 0.39 | |||
| T1 slope (°) | Preoperative | 21.2 ± 6.3 | 26.2 ± 9.1 | 0.77 | ||
| Immediate postoperative | 23.3 ± 7.8 | 26.4 ± 7.2 | 0.27 | |||
| 1 year | 21.9 ± 6.4 | 25.5 ± 7.3 | 0.61 | |||
| ACCF | ACDF part | ACCF part | Overall | |||
| FSA (°) | Preoperative | 2.9 ± 11.6 | 1.1 ± 5.9 | −1.6 ± 8.9 | 1.9 ± 11.3 | 0.77 # |
| Immediate postoperative | 5.7 ± 10.0 | 4.2 ± 10.9 | 1.8 ± 6.0 | 4.7 ± 10.8 | 0.27 # | |
| 1 year | 5.1 ± 9.4 | 4.2 ± 1.3 | 1.7 ± 6.0 | 4.3 ± 10.4 | 0.36 # | |
| FSH (mm) | Preoperative | 66.6 ± 15.7 | 37.4 ± 5.8 | 59.6 ± 9.6 | 69.4± 16.3 | 0.66 # |
| Immediate postoperative | 68.4 ± 17.1 | 37.0 ± 7.7 | 59.0 ±9.9 | 69.1 ± 15.4 | 0.54 # | |
| 1 year | 66.4 ± 15.0 | 36.8 ± 7.4 | 58.4 ± 8.6 | 68.8 ± 15.1 | 0.37 # | |
| ΔC2–7 angle (°) | 1.8 ± 8.2 | 3.3 ± 8.2 | 0.53 | |||
| ΔFSA (°) | 2.8 ± 7.9 | 2.6 ± 8.1 | 2.8 ± 7.5 | 2.8 ± 8.4 | 0.96 # | |
| ΔFSH (mm) | 3.2 ± 7.1 * | −0.4 ± 3.0 | −0.6 ± 3.5 | 1.4 ± 7.7 | 0.23 # | |
| Graft subsidence (cases) | 8 (26.7%) | 3 (13.0%) | 0.22 | |||
| Fusion rate | 80% | 100% * | 0.02 * | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirai, T.; Yoshii, T.; Sakai, K.; Inose, H.; Yuasa, M.; Yamada, T.; Matsukura, Y.; Ushio, S.; Morishita, S.; Egawa, S.; et al. Anterior Cervical Corpectomy with Fusion versus Anterior Hybrid Fusion Surgery for Patients with Severe Ossification of the Posterior Longitudinal Ligament Involving Three or More Levels: A Retrospective Comparative Study. J. Clin. Med. 2021, 10, 5315. https://doi.org/10.3390/jcm10225315
Hirai T, Yoshii T, Sakai K, Inose H, Yuasa M, Yamada T, Matsukura Y, Ushio S, Morishita S, Egawa S, et al. Anterior Cervical Corpectomy with Fusion versus Anterior Hybrid Fusion Surgery for Patients with Severe Ossification of the Posterior Longitudinal Ligament Involving Three or More Levels: A Retrospective Comparative Study. Journal of Clinical Medicine. 2021; 10(22):5315. https://doi.org/10.3390/jcm10225315
Chicago/Turabian StyleHirai, Takashi, Toshitaka Yoshii, Kenichiro Sakai, Hiroyuki Inose, Masato Yuasa, Tsuyoshi Yamada, Yu Matsukura, Shuta Ushio, Shingo Morishita, Satoru Egawa, and et al. 2021. "Anterior Cervical Corpectomy with Fusion versus Anterior Hybrid Fusion Surgery for Patients with Severe Ossification of the Posterior Longitudinal Ligament Involving Three or More Levels: A Retrospective Comparative Study" Journal of Clinical Medicine 10, no. 22: 5315. https://doi.org/10.3390/jcm10225315
APA StyleHirai, T., Yoshii, T., Sakai, K., Inose, H., Yuasa, M., Yamada, T., Matsukura, Y., Ushio, S., Morishita, S., Egawa, S., Onuma, H., Kobayashi, Y., Utagawa, K., Hashimoto, J., Kawabata, A., Tanaka, T., Motoyoshi, T., Takahashi, T., Hashimoto, M., ... Okawa, A. (2021). Anterior Cervical Corpectomy with Fusion versus Anterior Hybrid Fusion Surgery for Patients with Severe Ossification of the Posterior Longitudinal Ligament Involving Three or More Levels: A Retrospective Comparative Study. Journal of Clinical Medicine, 10(22), 5315. https://doi.org/10.3390/jcm10225315






