The Adverse Impact of the COVID-19 Pandemic on Abdominal Emergencies: A Retrospective Clinico-Pathological Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Collection
2.3. Primary and Secondary Outcome Measures
2.4. Statistical Analyses
3. Results
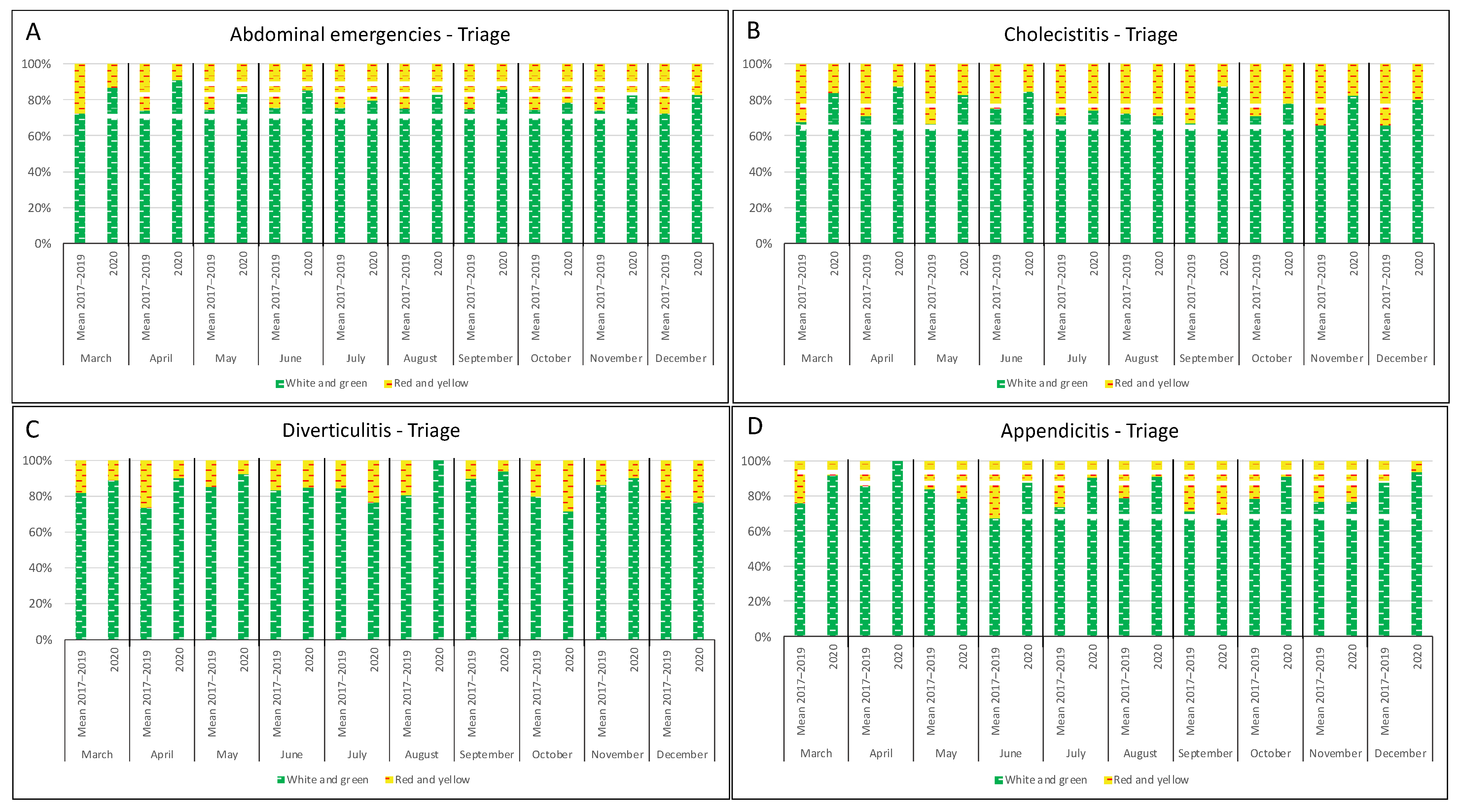
3.1. Analysis of ED Admissions
3.2. Analysis of Surgical Procedures
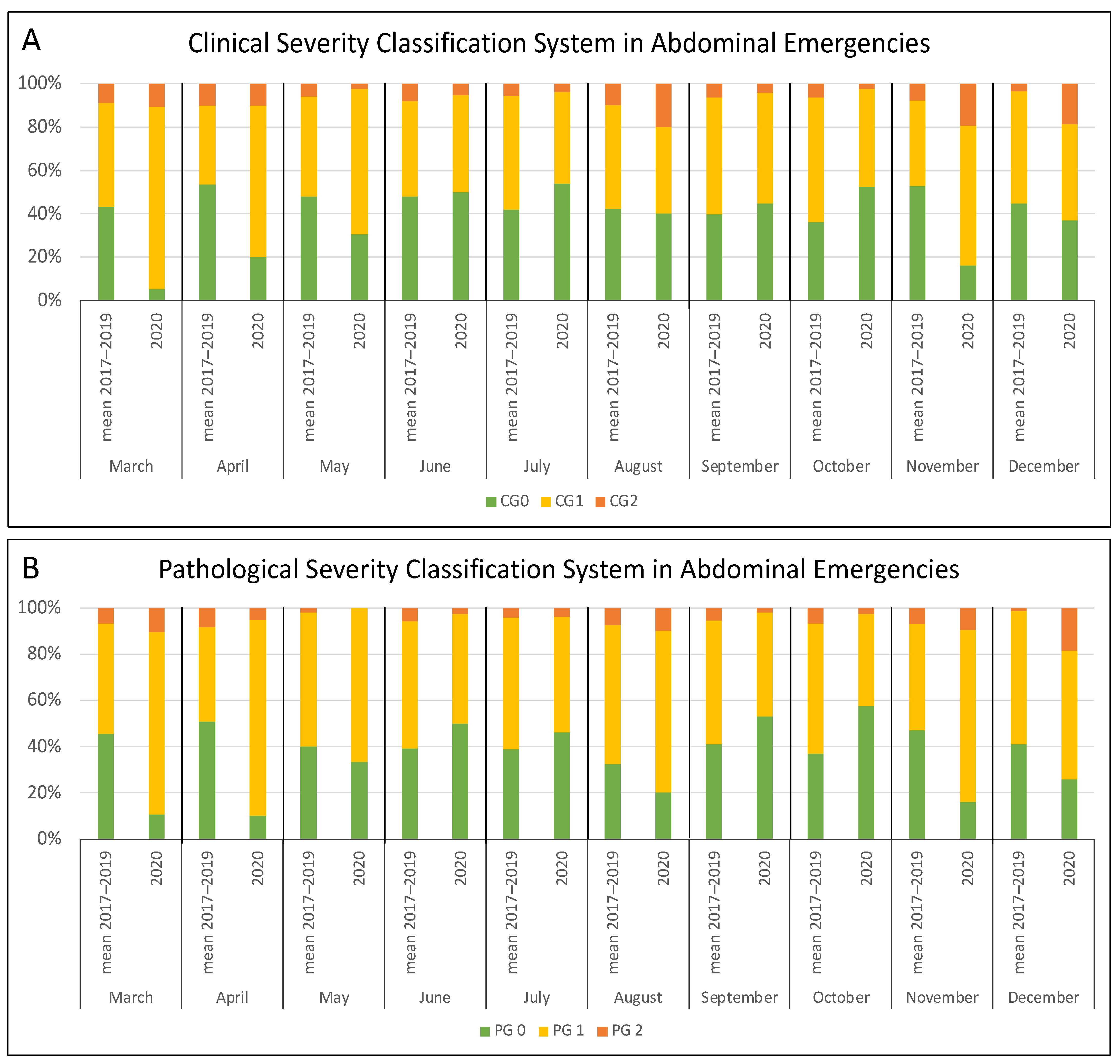
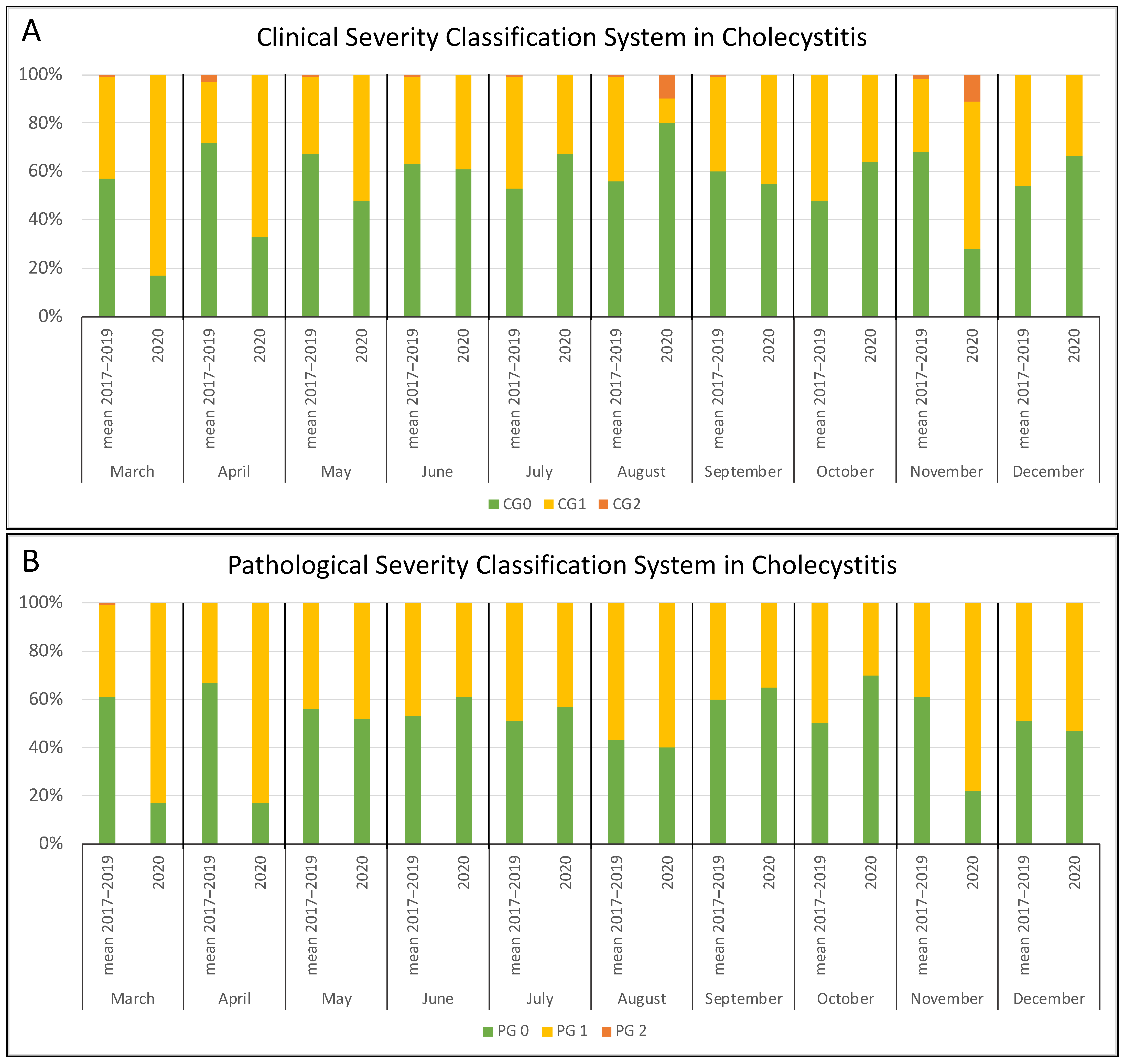
3.3. Analysis of Clinical and Pathological Severity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giovanetti, M.; Benvenuto, D.; Angeletti, S.; Ciccozzi, M. The first two cases of 2019-nCoV in Italy: Where they come from? J. Med. Virol. 2020, 92, 518–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministero Della Salute. Available online: https://www.salute.gov.it/portale/home.html (accessed on 16 August 2021).
- Mantica, G.; Riccardi, N.; Terrone, C.; Gratarola, A. Non-COVID-19 visits to emergency departments during the pandemic: The impact of fear. Public Health 2020, 183, 40–41. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child. Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Barten, D.G.; Latten, G.H.P. Re: Non-COVID-19 visits to emergency departments during the pandemic: The impact of fear. Public Health 2020, 185, 47. [Google Scholar] [CrossRef]
- Nunez, J.H.; Sallent, A.; Lakhani, K.; Guerra-Farfan, E.; Vidal, N.; Ekhtiari, S.; Minguell, J. Impact of the COVID-19 pandemic on an emergency traumatology service: Experience at a tertiary trauma Centre in Spain. Injury 2020, 51, 1414–1418. [Google Scholar] [CrossRef] [PubMed]
- Perlini, S.; Canevari, F.; Cortesi, S.; Sgromo, V.; Brancaglione, A.; Contri, E.; Pettenazza, P.; Salinaro, F.; Speciale, F.; Sechi, G.; et al. Emergency department and out-of-hospital emergency system (112-AREU 118) integrated response to Coronavirus Disease 2019 in a Northern Italy Centre. Intern. Emerg. Med. 2020, 15, 825–833. [Google Scholar] [CrossRef]
- Martin-Sanchez, F.J.; Valls Carbo, A.; Lopez Picado, A.; Martinez-Valero, C.; Miranda, J.D.; Leal Pozuleo, J.M.; Gonzalez Del Castillo, J. Impact of Spanish public health measures on emergency visits and COVID-19 diagnosed cases during the pandemic in Madrid. Rev. Esp. Quimioter. 2020, 33, 274–277. [Google Scholar] [CrossRef]
- Bellan, M.; Gavelli, F.; Hayden, E.; Patrucco, F.; Soddu, D.; Pedrinelli, A.R.; Cittone, M.G.; Rizzi, E.; Casciaro, G.F.; Vassia, V.; et al. Pattern of emergency department referral during the Covid-19 outbreak in Italy. Panminerva Med. 2020. ahead of print. [Google Scholar] [CrossRef]
- Wong, L.E.; Hawkins, J.E.; Langness, S.; Murrell, K.L.; Iris, P.; Sammann, A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. Nejm Catal. Innov. Care Deliv. 2020. [Google Scholar] [CrossRef]
- Kurihara, H.; Marrano, E.; Ceolin, M.; Chiara, O.; Faccincani, R.; Bisagni, P.; Fattori, L.; Zago, M. Impact of lockdown on emergency general surgery during first 2020 COVID-19 outbreak. Eur. J. Trauma Emerg. Surg. 2021, 47, 677–682. [Google Scholar] [CrossRef]
- Paganini, M.; Barbiellini Amidei, C.; Valastro, M.F.; Favaro, A.; Saia, M.; Buja, A. Adult emergency department visits during the COVID-19 pandemic in Veneto region, Italy: A time-trend analysis. Intern. Emerg. Med. 2021, 1–5, ahead of print. [Google Scholar] [CrossRef]
- Gormeli Kurt, N.; Camci, M. COVID-19: How do emergency departments fare after normalisation steps? Int. J. Clin. Pract. 2021, 75, e13912. [Google Scholar] [CrossRef]
- Santi, L.; Golinelli, D.; Tampieri, A.; Farina, G.; Greco, M.; Rosa, S.; Beleffi, M.; Biavati, B.; Campinoti, F.; Guerrini, S.; et al. Non-COVID-19 patients in times of pandemic: Emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS ONE 2021, 16, e0248995. [Google Scholar] [CrossRef]
- Steinman, M.; de Sousa, J.H.B.; Tustumi, F.; Wolosker, N. The burden of the pandemic on the non-SARS-CoV-2 emergencies: A multicenter study. Am. J. Emerg. Med. 2021, 42, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Masroor, S. Collateral damage of COVID-19 pandemic: Delayed medical care. J. Card Surg. 2020, 35, 1345–1347. [Google Scholar] [CrossRef]
- Santoro, G.A.; Grossi, U.; Murad-Regadas, S.; Nunoo-Mensah, J.W.; Mellgren, A.; Di Tanna, G.L.; Gallo, G.; Tsang, C.; Wexner, S.D.; Group, D.-C. DElayed COloRectal cancer care during COVID-19 Pandemic (DECOR-19): Global perspective from an international survey. Surgery 2021, 169, 796–807. [Google Scholar] [CrossRef] [PubMed]
- Maringe, C.; Spicer, J.; Morris, M.; Purushotham, A.; Nolte, E.; Sullivan, R.; Rachet, B.; Aggarwal, A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol. 2020, 21, 1023–1034. [Google Scholar] [CrossRef]
- Greenwood, E.; Swanton, C. Consequences of COVID-19 for cancer care-a CRUK perspective. Nat. Rev. Clin. Oncol. 2021, 18, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Pogorelic, Z.; Milanovic, K.; Versic, A.B.; Pasini, M.; Divkovic, D.; Pavlovic, O.; Lucev, J.; Zufic, V. Is there an increased incidence of orchiectomy in pediatric patients with acute testicular torsion during COVID-19 pandemic?—A retrospective multicenter study. J. Pediatr. Urol. 2021, 17, 479.e1–479.e6. [Google Scholar] [CrossRef]
- Martellucci, J.; Damigella, A.; Bergamini, C.; Alemanno, G.; Pantalone, D.; Coratti, A.; Muiesan, P.; Cianchi, F.; Prosperi, P. Emergency surgery in the time of Coronavirus: The pandemic effect. Minerva Chir. 2020, 76, 382–387. [Google Scholar] [CrossRef]
- Zintsmaster, M.P.; Myers, D.T. Patients avoided important care during the early weeks of the coronavirus pandemic: Diverticulitis patients were more likely to present with an abscess on CT. Emerg. Radiol. 2021, 28, 279–282. [Google Scholar] [CrossRef]
- Romero, J.; Valencia, S.; Guerrero, A. Acute appendicitis during Coronavirus Disease 2019 (COVID-19): Changes in clinical presentation and CT findings. J. Am. Coll. Radiol. 2020, 17, 1011–1013. [Google Scholar] [CrossRef]
- Gibson, A.L.; Chen, B.Y.; Rosen, M.P.; Paez, S.N.; Lo, H.S. Impact of the COVID-19 pandemic on emergency department CT for suspected diverticulitis. Emerg. Radiol. 2020, 27, 773–780. [Google Scholar] [CrossRef]
- Hossain, N.; Naidu, V.; Hosny, S.; Khalifa, M.; Mathur, P.; Al Whouhayb, M. Hospital presentations of acute diverticulitis during COVID-19 pandemic may be more likely to require surgery due to increased severity: A Single-Centre experience. Am. Surg. 2020, 3134820982560. [Google Scholar] [CrossRef]
- Morelli, N.; Rota, E.; Terracciano, C.; Immovilli, P.; Spallazzi, M.; Colombi, D.; Zaino, D.; Michieletti, E.; Guidetti, D. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 Era. Eur. Neurol. 2020, 83, 213–215. [Google Scholar] [CrossRef]
- Hubner, M.; Zingg, T.; Martin, D.; Eckert, P.; Demartines, N. Surgery for non-Covid-19 patients during the pandemic. PLoS ONE 2020, 15, e0241331. [Google Scholar] [CrossRef] [PubMed]
- Rosa, F.; Covino, M.; Sabia, L.; Quero, G.; Fiorillo, C.; Cozza, V.; Sganga, G.; Gasbarrini, A.; Franceschi, F.; Alfieri, S. Surgical emergencies during SARS-CoV-2 pandemic lockdown: What happened? Eur Rev. Med. Pharmacol. Sci. 2020, 24, 11919–11925. [Google Scholar] [CrossRef]
- Giamello, J.D.; Abram, S.; Bernardi, S.; Lauria, G. The emergency department in the COVID-19 era. Who are we missing? Eur. J. Emerg. Med. 2020, 27, 305–306. [Google Scholar] [CrossRef]
- Metzger, K.B.; Tolbert, P.E.; Klein, M.; Peel, J.L.; Flanders, W.D.; Todd, K.; Mulholland, J.A.; Ryan, P.B.; Frumkin, H. Ambient air pollution and cardiovascular emergency department visits. Epidemiology 2004, 15, 46–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cauchemez, S.; Ferguson, N.M.; Wachtel, C.; Tegnell, A.; Saour, G.; Duncan, B.; Nicoll, A. Closure of schools during an influenza pandemic. Lancet Infect. Dis. 2009, 9, 473–481. [Google Scholar] [CrossRef]
- Cano-Valderrama, O.; Morales, X.; Ferrigni, C.J.; Martin-Antona, E.; Turrado, V.; Garcia, A.; Cunarro-Lopez, Y.; Zarain-Obrador, L.; Duran-Poveda, M.; Balibrea, J.M.; et al. Acute care surgery during the COVID-19 pandemic in Spain: Changes in volume, causes and complications. A multicentre retrospective cohort study. Int. J. Surg. 2020, 80, 157–161. [Google Scholar] [CrossRef]
- Alemanno, G.; Tomaiuolo, M.; Peris, A.; Batacchi, S.; Nozzoli, C.; Prosperi, P. Surgical perspectives and patways in an emergency department during the COVID-19 pandemic. Am. J. Surg. 2020, 220, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Vissio, E.; Falco, E.C.; Collemi, G.; Borella, F.; Papotti, M.; Scarmozzino, A.; Cassoni, P.; Bertero, L. Impact of COVID-19 lockdown measures on oncological surgical activity: Analysis of the surgical pathology caseload of a tertiary referral hospital in Northwestern Italy. J. Surg. Oncol. 2021, 123, 24–31. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef] [PubMed]
- Willms, A.G.; Oldhafer, K.J.; Conze, S.; Thasler, W.E.; von Schassen, C.; Hauer, T.; Huber, T.; Germer, C.T.; Gunster, S.; Bulian, D.R.; et al. Appendicitis during the COVID-19 lockdown: Results of a multicenter analysis in Germany. Langenbecks Arch. Surg. 2021, 406, 367–375. [Google Scholar] [CrossRef]
- Tartaglia, N.; Pavone, G.; Lizzi, V.; Vovola, F.; Tricarico, F.; Pacilli, M.; Ambrosi, A. How emergency surgery has changed during the COVID-19 pandemic: A cohort study. Ann. Med. Surg. 2020, 60, 686–689. [Google Scholar] [CrossRef]
- Sell, N.M.; Stafford, C.E.; Goldstone, R.N.; Kunitake, H.; Francone, T.D.; Cauley, C.E.; Hodin, R.A.; Bordeianou, L.G.; Ricciardi, R. Delay to intervention for complicated diverticulitis is associated with higher inpatient mortality. J. Gastrointest. Surg. 2021. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vissio, E.; Falco, E.C.; Scozzari, G.; Scarmozzino, A.; Trinh, D.A.A.; Morino, M.; Papotti, M.; Bertero, L.; Cassoni, P. The Adverse Impact of the COVID-19 Pandemic on Abdominal Emergencies: A Retrospective Clinico-Pathological Analysis. J. Clin. Med. 2021, 10, 5254. https://doi.org/10.3390/jcm10225254
Vissio E, Falco EC, Scozzari G, Scarmozzino A, Trinh DAA, Morino M, Papotti M, Bertero L, Cassoni P. The Adverse Impact of the COVID-19 Pandemic on Abdominal Emergencies: A Retrospective Clinico-Pathological Analysis. Journal of Clinical Medicine. 2021; 10(22):5254. https://doi.org/10.3390/jcm10225254
Chicago/Turabian StyleVissio, Elena, Enrico Costantino Falco, Gitana Scozzari, Antonio Scarmozzino, Do An Andrea Trinh, Mario Morino, Mauro Papotti, Luca Bertero, and Paola Cassoni. 2021. "The Adverse Impact of the COVID-19 Pandemic on Abdominal Emergencies: A Retrospective Clinico-Pathological Analysis" Journal of Clinical Medicine 10, no. 22: 5254. https://doi.org/10.3390/jcm10225254
APA StyleVissio, E., Falco, E. C., Scozzari, G., Scarmozzino, A., Trinh, D. A. A., Morino, M., Papotti, M., Bertero, L., & Cassoni, P. (2021). The Adverse Impact of the COVID-19 Pandemic on Abdominal Emergencies: A Retrospective Clinico-Pathological Analysis. Journal of Clinical Medicine, 10(22), 5254. https://doi.org/10.3390/jcm10225254






