MRI Findings in Hip in Juvenile Idiopathic Arthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
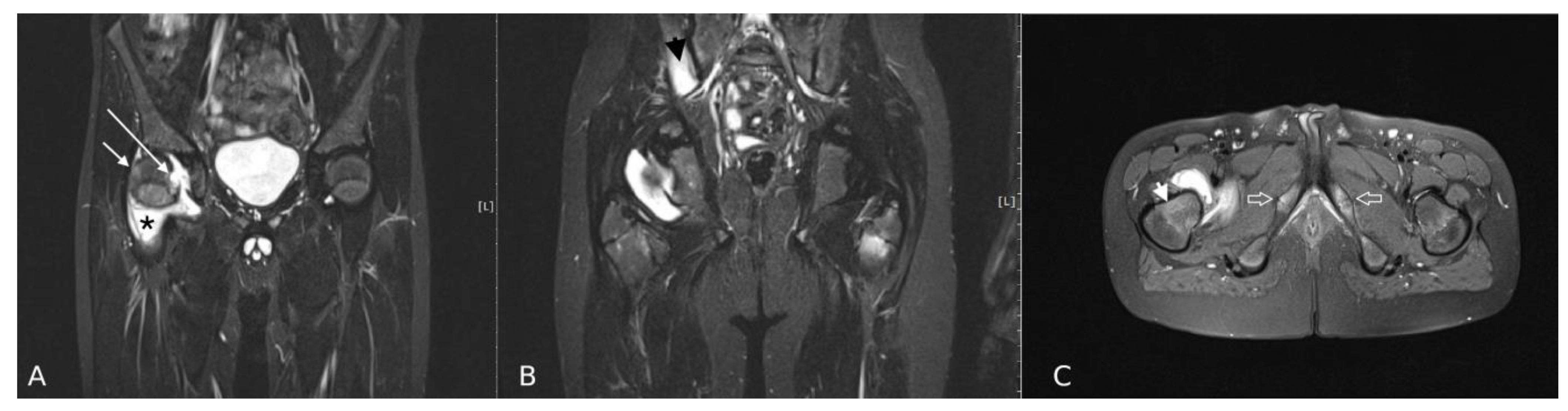
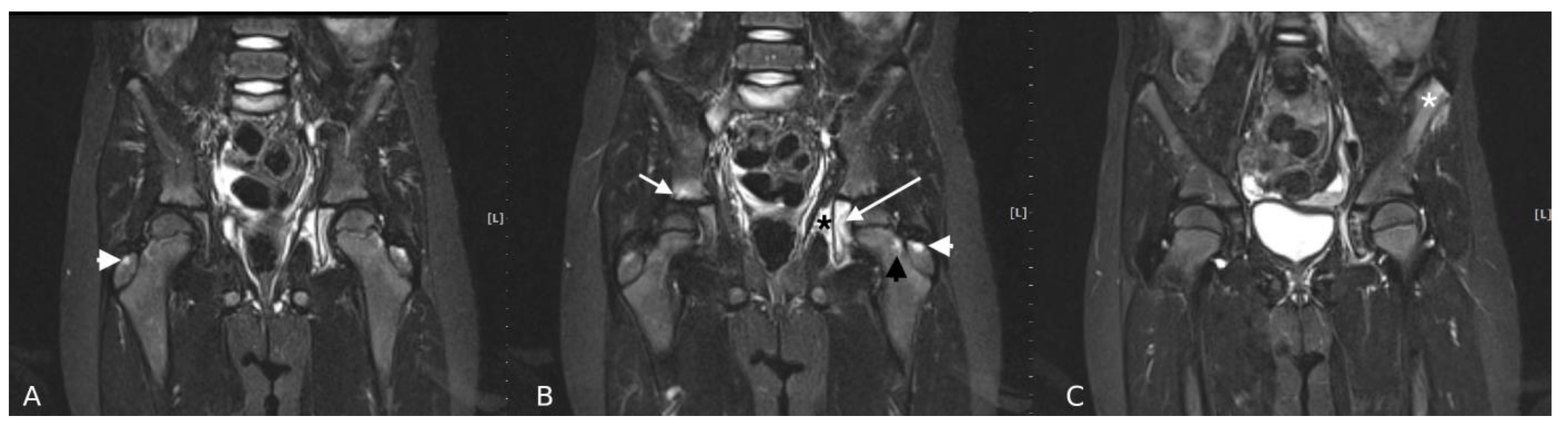
2.2. MRI Protocol and Interpretation of Imaging Features
2.3. Statistical Analysis
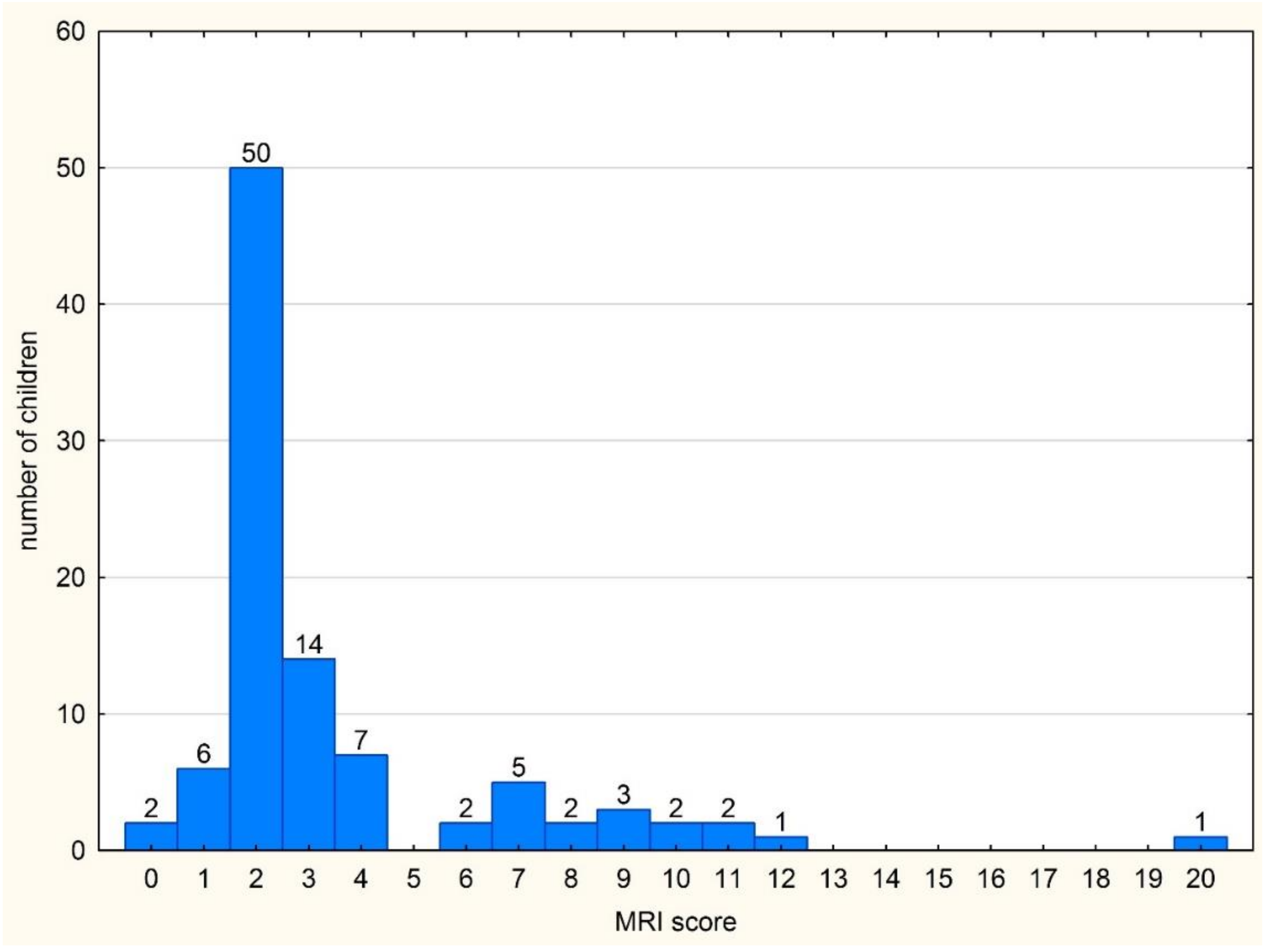
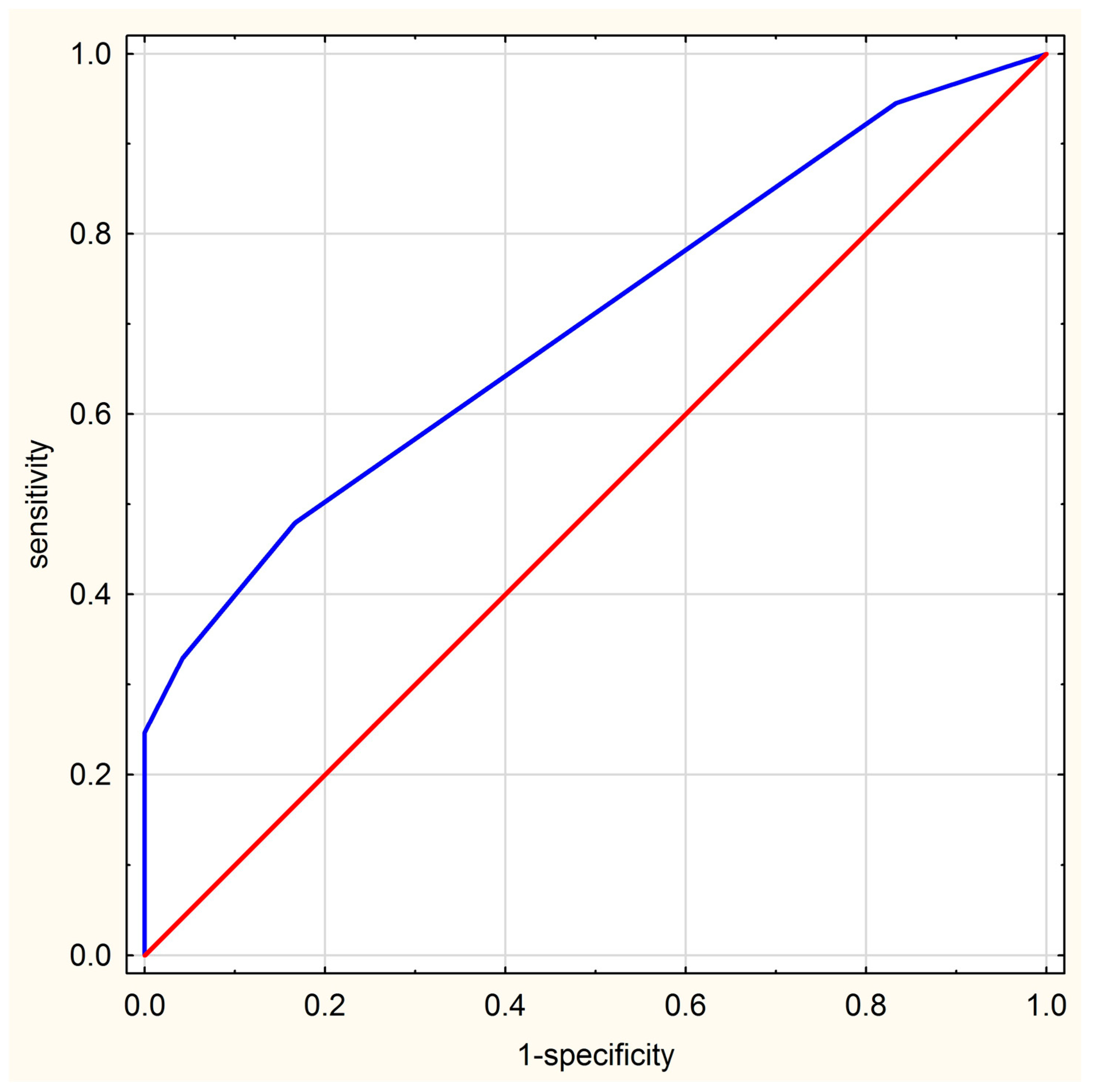
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rostom, S.; Amine, B.; Bensabbah, R.; Abouqal, R.; Hajjaj-Hassouni, N. Hip involvement in juvenile idiopathic arthritis. Clin. Rheumatol. 2008, 27, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Hemke, R.; Kuijpers, T.W.; Berg, J.v.D.; Van Veenendaal, M.; Dolman, K.M.; Van Rossum, M.A.J.; Maas, M. The diagnostic accuracy of unenhanced MRI in the assessment of joint abnormalities in juvenile idiopathic arthritis. Eur. Radiol. 2013, 23, 1998–2004. [Google Scholar] [CrossRef] [PubMed]
- Lovell, D.J. Juvenile idiopathic arthritis: Clinical features. In Primer on the Rheumatic Diseases; Klippel, J.H., Stone, J.H., Crofford, L.J., White, P.F., Eds.; Springer: New York, NY, USA, 2008; pp. 142–148. [Google Scholar]
- El-Azeem, M.I.A.; Taha, H.A.; El-Sherif, A.M. Role of MRI in evaluation of hip joint involvement in juvenile idiopathic arthritis. Egypt. Rheumatol. 2012, 34, 75–82. [Google Scholar] [CrossRef][Green Version]
- I Argyropoulou, M.; Fanis, S.L.; Xenakis, T.; Efremidis, S.C.; Siamopoulou, A. The role of MRI in the evaluation of hip joint disease in clinical subtypes of juvenile idiopathic arthritis. Br. J. Radiol. 2002, 75, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.G.; Ridley, N.T.; Mitchell, N.; Rooney, M. Juvenile chronic arthritis of the hip: Value of contrast-enhanced MR imaging. Clin. Radiol. 1996, 51, 99–102. [Google Scholar] [CrossRef]
- Sudoł-Szopińska, I.; Jans, L.; Jurik, A.G.; Hemke, R.; Eshed, I.; Boutry, N. Imaging Features of the Juvenile Inflammatory Arthropathies. Semin. Musculoskelet. Radiol. 2018, 22, 147–165. [Google Scholar] [CrossRef]
- Malattia, C.; Damasio, M.B.; Basso, C.; Verri, A.; Magnaguagno, F.; Viola, S.; Gattorno, M.; Ravelli, A.; Toma, P.; Martini, A. Dynamic contrast-enhanced magnetic resonance imaging in the assessment of disease activity in patients with juvenile idiopathic arthritis. Rheumatology 2009, 49, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Avenarius, D.F.M.; Nusman, C.; Malattia, C.; de Horatio, L.T.; Rosendahl, K.; Maas, M.; Müller, L.-S.O. Current status of wrist imaging in juvenile idiopathic arthritis. Pediatr. Radiol. 2018, 48, 801–810. [Google Scholar] [CrossRef]
- Shelmerdine, S.C.; Di Paolo, P.L.; De Horatio, L.T.; Malattia, C.; Magni-Manzoni, S.; Rosendahl, K. Imaging of the hip in juvenile idiopathic arthritis. Pediatr. Radiol. 2018, 48, 811–817. [Google Scholar] [CrossRef]
- Nistala, K.; Babar, J.; Johnson, K.; Campbell-Stokes, P.; Foster, K.; Ryder, C.; McDonagh, J. Clinical assessment and core outcome variables are poor predictors of hip arthritis diagnosed by MRI in juvenile idiopathic arthritis. Rheumatology 2006, 46, 699–702. [Google Scholar] [CrossRef][Green Version]
- Friedman, S.; A Gruber, M. Ultrasonography of the hip in the evaluation of children with seronegative juvenile rheumatoid arthritis. J. Rheumatol. 2002, 29, 629–632. [Google Scholar]
- Packham, J.C.; Hall, M.A. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: Functional outcome. Rheumatology 2002, 41, 1428–1435. [Google Scholar] [CrossRef]
- Janet, M.; Greg, I.; Karl, J. MRI in juvenile idiopathic arthritis and juvenile dermatomyositis. Ann. N. Y. Acad. Sci. 2009, 1154, 52–83. [Google Scholar]
- McKay, G.M.; A Cox, L.; Long, B.W. Imaging juvenile idiopathic arthritis: Assessing the modalities. Radiol. Technol. 2010, 81, 318–327. [Google Scholar] [PubMed]
- Gylys-Morin, V.M.; Graham, T.B.; Blebea, J.S.; Dardzinski, B.J.; Laor, T.; Johnson, N.D.; Oestreich, A.E.; Passo, M.H. Knee in Early Juvenile Rheumatoid Arthritis: MR Imaging Findings. Radiology 2001, 220, 696–706. [Google Scholar] [CrossRef] [PubMed]
- Sudoł-Szopińska, I.; Kontny, E.; Maśliński, W. The pathogenesis of rheumatoid arthritis in radiological studies. Part I: For-mation of inflammatory infiltrates within the synovial membrane. J. Ultrason. 2012, 12, 202–213. [Google Scholar] [CrossRef]
- Ostrowska, M.; Maśliński, W.; Prochorec-Sobieszek, M.; Nieciecki, M.; Sudoł-Szopińska, I. Cartilage and bone damage in rheumatoid arthritis. Reumatologia 2018, 56, 111–120. [Google Scholar] [CrossRef] [PubMed]
- McQueen, F.M. Magnetic resonance imaging in early inflammatory arthritis: What is its role? Rheumatology 2000, 39, 700–706. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gulani, V.; Calamante, F.; Shellock, F.G.; Kanal, E.; Reeder, S.B. International Society for Magnetic Resonance in Medicine. Gadolinium deposition in the brain: Summary of evidence and recommendations. Lancet Neurol. 2017, 16, 564–570. [Google Scholar] [CrossRef]
- Ranga, A.; Agarwal, Y.; Garg, K.J. Gadolinium based contrast agents in current practice: Risks of accumulation and toxicity in patients with normal renal function. Indian J. Radiol. Imaging 2017, 27, 141–147. [Google Scholar] [CrossRef]
- Panwar, J.; Tolend, M.; Redd, B.; Srinivasalu, H.; Colbert, R.A.; Akikusa, J.; Appenzeller, S.; Carrino, J.A.; Herregods, N.; Jans, L.; et al. Consensus-driven conceptual development of a standardized whole body-MRI scoring system for assessment of disease activity in juvenile idiopathic arthritis: MRI in JIA OMERACT working group. Semin. Arthritis Rheum. 2021. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.W.; Velez, N.F.; Lam, C.E.; Femia, A.; Granter, S.R.; Townsend, H.B.; Vleugels, R.A. Dermatomyositis induced by anti-tumour necrosis factor in a patient with juvenile idio-pathic arthritis. JAMA Dermatol. 2013, 149, 1204–1208. [Google Scholar] [CrossRef]
- Gietka, P.; Rutkowska-Sak, L.; Lisowska, B. Myositis in the course of the systemic form juvenile idiopathic arthritis. Reumatologia/Rheumatology 2014, 2, 142–145. [Google Scholar] [CrossRef]
- Lindehammar, H.; Lindvall, B. Muscle involvement in juvenile idiopathic arthritis. Rheumatology 2004, 43, 1546–1554. [Google Scholar] [CrossRef] [PubMed]
- Lindehammar, H.; Bäckman, E. Muscle function in juvenile chronic arthritis. J. Rheumatol. 1995, 22, 1159–1165. [Google Scholar] [PubMed]
- Kirkhus, E.; Flatø, B.; Riise, O.; Reiseter, T.; Smith, H.-J. Differences in MRI findings between subgroups of recent-onset childhood arthritis. Pediatr. Radiol. 2010, 41, 432–440. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Porter-Young, F.M.; Offiah, A.C.; Broadley, P.; Lang, I.; McMahon, A.-M.; Howsley, P.; Hawley, D.P. Inter- and intra-observer reliability of contrast-enhanced magnetic resonance imaging parameters in children with suspected juvenile idiopathic arthritis of the hip. Pediatr. Radiol. 2018, 48, 1891–1900. [Google Scholar] [CrossRef] [PubMed]
- Hemke, R.; Herregods, N.; Jaremko, J.L.; Åström, G.; Avenarius, D.; Becce, F.; Bielecki, D.K.; Boesen, M.; Dalili, D.; Giraudo, C.; et al. Imaging assessment of children presenting with suspected or known juvenile idiopathic arthritis: ESSR-ESPR points to consider. Eur. Radiol. 2020, 30, 5237–5249. [Google Scholar] [CrossRef]
- Martini, A.; Ravelli, A.; Avcin, T.; Beresford, M.W.; Burgos-Vargas, R.; Cuttica, R.; Ilowite, N.T.; Khubchandani, R.; Laxer, R.M.; Lovell, D.J.; et al. Toward New Classification Criteria for Juvenile Idiopathic Arthritis: First Steps, Pediatric Rheumatology International Trials Organization International Consensus. J. Rheumatol. 2018, 46, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Petty, R.E.; Southwood, T.R.; Manners, P.; Baum, J.; Glass, D.N.; Goldenberg, J.; He, X.; Maldonado-Cocco, J.; Orozco-Alcala, J.; Prieur, A.-M.; et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: Second revision, Edmonton, 2001. J. Rheumatol. 2004, 31, 390–392. [Google Scholar] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Jurik, A.G.; Eshed, I.; Lennart, J.; Grainger, A.; Østergaard, M.; Klauser, A.; Cotten, A.; Wick, M.C.; Maas, M.; Miese, F.; et al. Recommendations of the ESSR Arthritis Subcommittee for the Use of Magnetic Resonance Imaging in Musculoskeletal Rheumatic Diseases. Semin. Musculoskelet. Radiol. 2015, 19, 396–411. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, A.V.; Whitworth, P.; Baildam, E.M. Use of methotrexate in juvenile idiopathic arthritis. Arch. Dis. Child. 2003, 88, 197–200. [Google Scholar] [CrossRef]
- Mitchell, D.G.; Rao, V.; Dalinka, M.; E Spritzer, C.; Gefter, W.B.; Axel, L.; Steinberg, M.; Kressel, H.Y. MRI of joint fluid in the normal and ischemic hip. Am. J. Roentgenol. 1986, 146, 1215–1218. [Google Scholar] [CrossRef] [PubMed]
- Koski, J.M. Ultrasonographic evidence of hip synovitis in patients with rheumatoid arthritis. Scand. J. Rheumatol. 1989, 18, 127–131. [Google Scholar] [CrossRef]
- Rydholm, U.; Wingstrand, H.; Egund, N.; Elborg, R.; Forsberg, L.; Lidgren, L. Sonography, arthroscopy, and intracapsular pressure in juvenile chronic arthritis of the hip. Acta Orthop. Scand. 1986, 57, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Wechalekar, M.D. The synovium. In Rheumatology, 6th ed.; Mosby: Philadelphia, PA, USA, 2015; pp. 27–32. [Google Scholar]
- Nusman, C.M.; Hemke, R.; Benninga, M.A.; Schonenberg-Meinema, D.; Kindermann, A.; van Rossum, M.A.J.; van den Berg, J.M.; Maas, M.; Kuijpers, T.W. Contrast-enhanced MRI of the knee in children unaffected by clinical arthritis compared to clinically active juvenile idiopathic arthritis patients. Eur. Radiol. 2016, 26, 1141–1148. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Horton, D.B.; Haynes, K.; Denburg, M.R.; Thacker, M.; Rose, C.D.; E Putt, M.; Leonard, M.B.; Strom, B.L. Oral glucocorticoid use and osteonecrosis in children and adults with chronic inflammatory diseases: A population-based cohort study. BMJ Open 2017, 7, e016788. [Google Scholar] [CrossRef] [PubMed]
- Lambert, R.; Bakker, P.A.C.; Van Der Heijde, D.; Weber, U.; Rudwaleit, M.; Hermann, K.-G.; Sieper, J.; Baraliakos, X.; Bennett, A.; Braun, J.; et al. Defining active sacroiliitis on MRI for classification of axial spondyloarthritis: Update by the ASAS MRI working group. Ann. Rheum. Dis. 2016, 75, 1958–1963. [Google Scholar] [CrossRef]
| MRI Feature | Scoring | |
|---|---|---|
| 1 | Effusion | 0–3 0: no fluid; 1: trace of fluid and maximum thickness of ≤2 mm 2: continual effusion and thickness >2 mm and ≤5 mm 3: effusion with distension of capsule and thickness >5 mm |
| 2 | BME head | 0–2 0: BME not seen 1: BME up to 50% of the head width 2: BME > 50% of the head width |
| 3 | BME neck | 0–2 0: BME not seen 1: BME up to 50% of the neck width 2: BME > 50% of the neck width |
| 4 | BME acetabulum | 0–2 0: BME not seen 1: BME up to 50% of the acetabular width 2: BME > 50% of the acetabular width |
| 5 | BME greater trochanter | 0–1 |
| 6 | Synovitis | 0–1 0: synovium not visible 1: synovium visible regardless the thickness |
| 7 | Bursitis | 0–1 |
| 8 | Enthesitis | 0–1 |
| 9 | Tendinitis | 0–1 |
| 10 | Myositis | 0–1 |
| 11 | Triradiate cartilage involvement | 0–1 |
| 12 | Physeal involvment | 0-1 |
| 13 | Cyst femoral head | 0–1 |
| 14 | Cyst acetabulum | 0–1 |
| 15 | Erosion femoral head | 0–1 |
| 16 | Erosion acetabulum | 0–1 |
| 17 | Chondromalacia | 0–1 |
| 18 | Joint space narrowing | 0–1 |
| 19 | Protrusio acetabuli | 0–1 |
| 20 | Ankylosis | 0–1 |
| 21 | Sclerotization | 0–1 |
| 22 | Osteophytes | 0–1 |
| 23 | Avascular necrosis | 0–1 |
| 24 | Bone remodeling | 0–1 |
| MRI Lesions and Scorings | JIA Confirmed Group n = 73 | Non-JIA Group n = 24 | |||
|---|---|---|---|---|---|
| Number of Lesions | Number of Lesions | ||||
| Left Hip | Right Hip | Left Hip | Right Hip | ||
| 1 | Effusion | ||||
| 0 | 6 | 7 | 3 | 3 | |
| 1 | 59 | 54 | 20 | 20 | |
| 2 | 4 | 6 | 1 | 1 | |
| 3 | 4 | 6 | 0 | 0 | |
| 2 | BME head | ||||
| 0 | 62 | 66 | 24 | 23 | |
| 1 | 9 | 3 | 0 | 1 | |
| 2 | 2 | 4 | 0 | 0 | |
| 3 | BME neck | ||||
| 0 | 66 | 67 | 24 | 24 | |
| 1 | 4 | 4 | 0 | 0 | |
| 2 | 3 | 2 | 0 | 0 | |
| 4 | BME acetabulum | ||||
| 0 | 70 | 68 | 24 | 24 | |
| 1 | 3 | 3 | 0 | 0 | |
| 2 | 0 | 2 | 0 | 0 | |
| 5 | BME greater trochanter | ||||
| 0 | 66 | 69 | 24 | 24 | |
| 1 | 7 | 4 | 0 | 0 | |
| 6 | Synovitis | ||||
| 0 | 67 | 64 | 24 | 24 | |
| 1 | 6 | 9 | 0 | 0 | |
| 7 | Bursitis | ||||
| 0 | 68 | 72 | 23 | 24 | |
| 1 | 5 | 1 | 1 | 0 | |
| 8 | Enthesitis | ||||
| 0 | 65 | 66 | 24 | 24 | |
| 1 | 8 | 7 | 0 | 0 | |
| 9 | Tendinitis | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 10 | Myositis | ||||
| 0 | 72 | 71 | 24 | 24 | |
| 1 | 1 | 2 | 0 | 0 | |
| 11 | Triradiate cartilage involvement | ||||
| 0 | 72 | 72 | 24 | 24 | |
| 1 | 1 | 1 | 0 | 0 | |
| 12 | Physeal involvment | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 13 | Cyst femoral head | ||||
| 0 | 71 | 72 | 24 | 24 | |
| 1 | 2 | 1 | 0 | 0 | |
| 14 | Cyst acetabulum | ||||
| 0 | 72 | 72 | 24 | 24 | |
| 1 | 1 | 1 | 0 | 0 | |
| 15 | Erosion femoral head | ||||
| 0 | 73 | 71 | 24 | 24 | |
| 1 | 0 | 2 | 0 | 0 | |
| 16 | Erosion acetabulum | ||||
| 0 | 72 | 73 | 24 | 24 | |
| 1 | 1 | 0 | 0 | 0 | |
| 17 | Chondromalacia | ||||
| 0 | 68 | 71 | 24 | 24 | |
| 1 | 5 | 2 | 0 | 0 | |
| 18 | Joint space narrowing | ||||
| 0 | 71 | 70 | 24 | 24 | |
| 1 | 2 | 3 | 0 | 0 | |
| 19 | Protrusio acetabuli | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 20 | Ankylosis | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 21 | Sclerotization | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 22 | Osteophytes | ||||
| 0 | 73 | 73 | 24 | 24 | |
| 1 | 0 | 0 | 0 | 0 | |
| 23 | Avascular necrosis | ||||
| 0 | 71 | 72 | 24 | 23 | |
| 1 | 2 | 1 | 0 | 1 | |
| 24 | Bone remodeling | ||||
| 0 | 72 | 72 | 24 | 23 | |
| 1 | 1 | 1 | 0 | 1 | |
| MRI Feature and Scoring at Least in One Hip | JIA Confirmed Group | Non-JIA Group | p * | |
|---|---|---|---|---|
| 1 | Effusion | |||
| 0 | 12 (16%) | 5 (21%) | 0.856 | |
| 1 | 66 (90%) | 22 (92%) | 0.825 | |
| 2 | 8 (11%) | 1 (4%) | 0.555 | |
| 3 | 10 (14%) | 0 (0%) | 0.127 | |
| 2 or 3 | 17 (23%) | 1 (4%) | 0.074 | |
| 2 | BME head | |||
| 0 | 71 (97%) | 24 (100%) | 0.993 | |
| 1 | 11 (15%) | 1 (4%) | 0.294 | |
| 2 | 6 (8%) | 0 (0%) | 0.336 | |
| 1 or 2 | 16 (22%) | 1 (4%) | 0.094 | |
| 3 | BME neck | |||
| 0 | 72 (99%) | 24 (100%) | 0.556 | |
| 1 | 8 (11%) | 0 (0%) | 0.206 | |
| 2 | 5 (7%) | 0 (0%) | 0.433 | |
| 1 or 2 | 12 (16%) | 0 (0%) | 0.078 | |
| 4 | BME acetabulum | |||
| 0 | 72 (99%) | 24 (100%) | 0.556 | |
| 1 | 6 (8%) | 0 (0%) | 0.336 | |
| 2 | 2 (3%) | 0 (0%) | 0.993 | |
| 1 or 2 | 7 (10%) | 0 (0%) | 0.263 | |
| 5 | BME greater trochanter | |||
| 0 | 70 (96%) | 24 (100%) | 0.742 | |
| 1 | 8 (11%) | 0 (0%) | 0.206 | |
| 6 | Synovitis | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 15 (21%) | 0 (0%) | 0.037 | |
| 7 | Bursitis | |||
| 0 | 72 (99%) | 24 (100%) | 0.556 | |
| 1 | 5 (7%) | 1 (4%) | 0.988 | |
| 8 | Enthesitis | |||
| 0 | 72 (99%) | 24 (100%) | 0.556 | |
| 1 | 14 (19%) | 0 (0%) | 0.047 | |
| 9 | Tendinitis | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 10 | Myositis | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 3 (4%) | 0 (0%) | 0.742 | |
| 11 | Triradiate cartilage involvement | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 1 (1%) | 0 (0%) | 0.556 | |
| 12 | Physeal involvment | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 13 | Cyst femoral head | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 3 (4%) | 0 (0%) | 0.742 | |
| 14 | Cyst acetabulum | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 2 (3%) | 0 (0%) | 0.993 | |
| 15 | Erosion femoral head | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 2 (3%) | 0 (0%) | 0.993 | |
| 16 | Erosion acetabulum | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 1 (1%) | 0 (0%) | 0.556 | |
| 17 | Chondromalacia | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 7 (10%) | 0 (0%) | 0.263 | |
| 18 | Joint space narrowing | |||
| 0 | 72 (99%) | 24 (100%) | 0.556 | |
| 1 | 4 (5%) | 0 (0%) | 0.562 | |
| 19 | Protrusio acetabuli | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 20 | Ankylosis | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 21 | Sclerotization | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 22 | Osteophytes | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 0 (0%) | 0 (0%) | 1 | |
| 23 | Avascular necrosis | |||
| 0 | 73 (100%) | 24 (100%) | 1 | |
| 1 | 3 (4%) | 1 (4%) | 0.562 | |
| 24 | Bone remodeling | |||
| 0 | 72 (99%) | 23 (96%) | 0.556 | |
| 1 | 1 (1%) | 1 (4%) | 0.993 |
| MRI Summarised Score | JIA | Non-JIA | True Pos. | False Pos. | False Neg. | True Neg. | Sens. | Spec. | PPV | NPV |
|---|---|---|---|---|---|---|---|---|---|---|
| 20 | 1 | 0 | 1 | 0 | 72 | 24 | 0.014 | 1.000 | 1.000 | 0.250 |
| 12 | 1 | 0 | 2 | 0 | 71 | 24 | 0.027 | 1.000 | 1.000 | 0.253 |
| 11 | 2 | 0 | 4 | 0 | 69 | 24 | 0.055 | 1.000 | 1.000 | 0.258 |
| 10 | 2 | 0 | 6 | 0 | 67 | 24 | 0.082 | 1.000 | 1.000 | 0.264 |
| 9 | 3 | 0 | 9 | 0 | 64 | 24 | 0.123 | 1.000 | 1.000 | 0.273 |
| 8 | 2 | 0 | 11 | 0 | 62 | 24 | 0.151 | 1.000 | 1.000 | 0.279 |
| 7 | 5 | 0 | 16 | 0 | 57 | 24 | 0.219 | 1.000 | 1.000 | 0.296 |
| 6 | 2 | 0 | 18 | 0 | 55 | 24 | 0.247 | 1.000 | 1.000 | 0.304 |
| 4 | 6 | 1 | 24 | 1 | 49 | 23 | 0.329 | 0.958 | 0.960 | 0.319 |
| 3 | 11 | 3 | 35 | 4 | 38 | 20 | 0.479 | 0.833 | 0.897 | 0.345 |
| 2 | 34 | 16 | 69 | 20 | 4 | 4 | 0.945 | 0.167 | 0.775 | 0.500 |
| 1 | 3 | 3 | 72 | 23 | 1 | 1 | 0.986 | 0.042 | 0.758 | 0.500 |
| 0 | 1 | 1 | 73 | 24 | 0 | 0 | 1.000 | 0.000 | 0.753 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ostrowska, M.; Gietka, P.; Mańczak, M.; Michalski, E.; Sudoł-Szopińska, I. MRI Findings in Hip in Juvenile Idiopathic Arthritis. J. Clin. Med. 2021, 10, 5252. https://doi.org/10.3390/jcm10225252
Ostrowska M, Gietka P, Mańczak M, Michalski E, Sudoł-Szopińska I. MRI Findings in Hip in Juvenile Idiopathic Arthritis. Journal of Clinical Medicine. 2021; 10(22):5252. https://doi.org/10.3390/jcm10225252
Chicago/Turabian StyleOstrowska, Monika, Piotr Gietka, Małgorzata Mańczak, Emil Michalski, and Iwona Sudoł-Szopińska. 2021. "MRI Findings in Hip in Juvenile Idiopathic Arthritis" Journal of Clinical Medicine 10, no. 22: 5252. https://doi.org/10.3390/jcm10225252
APA StyleOstrowska, M., Gietka, P., Mańczak, M., Michalski, E., & Sudoł-Szopińska, I. (2021). MRI Findings in Hip in Juvenile Idiopathic Arthritis. Journal of Clinical Medicine, 10(22), 5252. https://doi.org/10.3390/jcm10225252






