Cortisol as a Biomarker of Mental Disorder Severity
Abstract
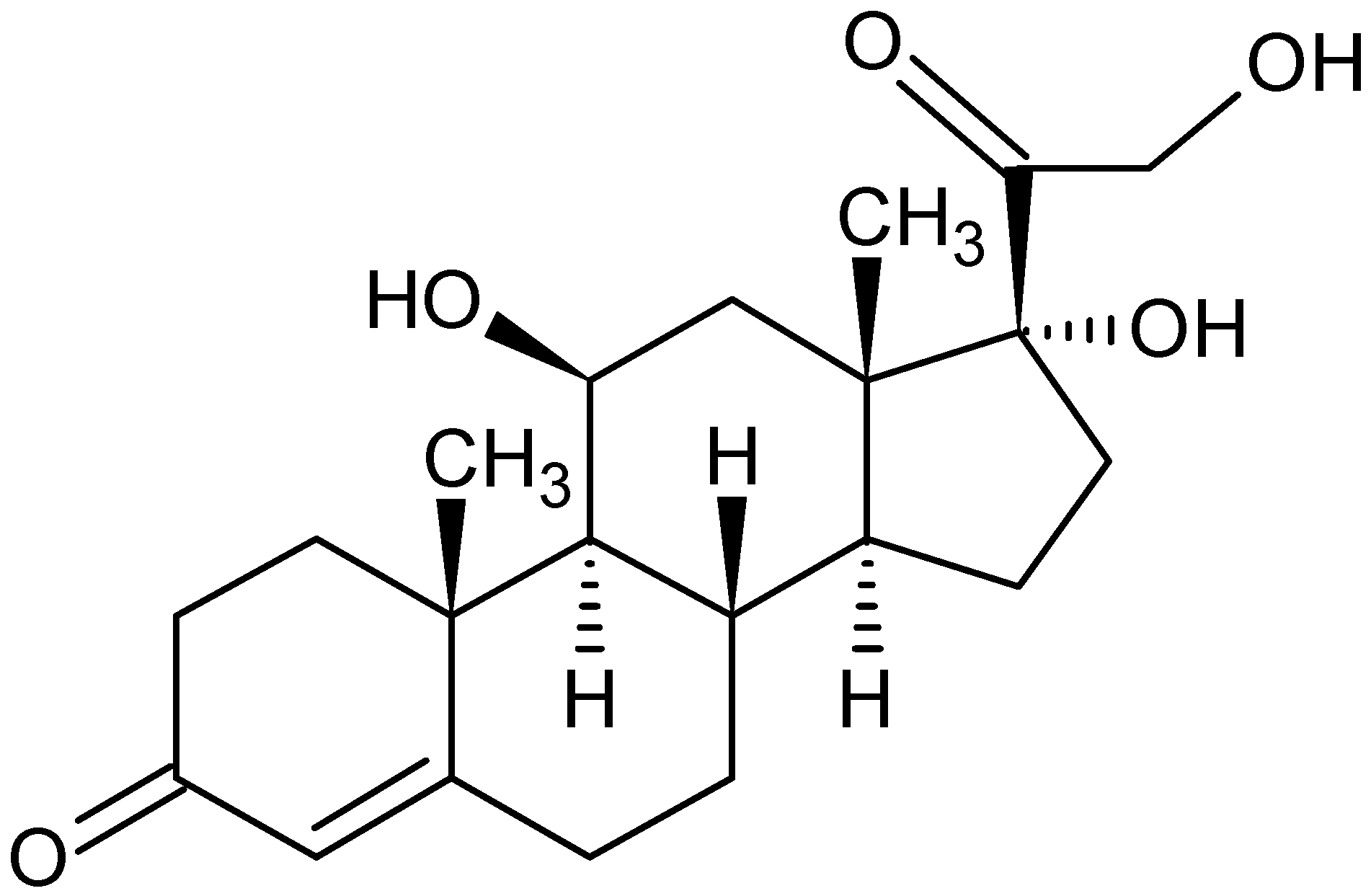
1. Introduction
2. Consequences of Abnormal Cortisol Secretion
3. The Role of Cortisol in the Pathophysiology of Depression
4. Cortisol Secretion Disorders and Bipolar Disorder
5. Cortisol Secretion Disorders and Psychosis
6. Psychotropic Drugs and Cortisol Secretion
6.1. The Effect of Antidepressants on Cortisol Levels
6.2. The Effect of Combined Therapy on Cortisol Levels
6.3. The Effect of Antipsychotics on Cortisol Levels
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 18 June 2021).
- Katzung, B.G.; Kruidering-Hall, M.; Tuan, R.; Vanderah, T.W.; Trevor, A.J. Adrenocorticosteroids & Adrenocortical Antagonists. In Katzung & Trevor’s Pharmacology: Examination & Board Review, 13th ed.; Katzung, B.G., Kruidering-Hall, M., Tuan, R., Vanderah, T.W., Trevor, A.J., Eds.; McGraw-Hill: New York, NY, USA, 2021; Available online: https://accessmedicine-1mhmedical-1com-1aqoxlrin0976.han.gumed.edu.pl/content.aspx?bookid=3058§ionid=255306661 (accessed on 18 June 2021).
- Cedernaes, J.; Ramsey, K.; Bass, J. The Role of Circadian Biology in Health and Disease. In Harrison’s Principles of Internal Medicine, 20e; Jameson, J., Fauci, A.S., Kasper, D.L., Hauser, S.L., Longo, D.L., Loscalzo, J., Eds.; McGraw-Hill: New York, NY, USA, 2021; Available online: https://accesspharmacy.mhmedical.com/content.aspx?bookid=2129§ionid=192536187 (accessed on 18 June 2021).
- Budziszewska, B.; Lasoń, W. Neuroendokrynne Mechanizmy Działania Leków Przeciwdepresyjnych; Triangulum M.B.P.: Wrocław, Poland, 2003. [Google Scholar]
- Carroll, T.B.; Aron, D.C.; Findling, J.W.; Tyrrell, J. Glucocorticoids and Adrenal Androgens. In Greenspan’s Basic & Clinical Endocrinology, 10e; Gardner, D.G., Shoback, D., Eds.; McGraw-Hill: New York, NY, USA, 2017; Available online: https://accessmedicine-1mhmedical-1com-1aqoxlrin0976.han.gumed.edu.pl/content.aspx?bookid=2178§ionid=166249274 (accessed on 18 June 2021).
- Fietta, P.; Fietta, P.; Delsante, G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry Clin. Neurosci. 2009, 63, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Anesthesia for Patients with Neurological & Psychiatric Diseases. In Morgan & Mikhail’s Clinical Anesthesiology, 6e; Butterworth, J.F., IV, Mackey, D.C., Wasnick, J.D., Eds.; McGraw-Hill: New York, NY, USA, 2018; Available online: https://accessmedicine-1mhmedical-1com-1aqoxlrin0976.han.gumed.edu.pl/content.aspx?bookid=2444§ionid=193561247 (accessed on 18 June 2021).
- DeBattista, C. Antidepressant Agents. In Basic & Clinical Pharmacology, 15e; Katzung, B.G., Vanderah, T.W., Eds.; McGraw-Hill: New York, NY, USA, 2021; Available online: https://accessmedicine-1mhmedical-1com-1aqoxlrin0976.han.gumed.edu.pl/content.aspx?bookid=2988§ionid=250598963 (accessed on 18 June 2021).
- McEwen, B.S. Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998, 840, 33–44. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiol. Rev. 2007, 87, 873–904. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.; Fauci, A.S.; Kasper, D.L.; Hauser, S.L.; Longo, D.L.; Loscalzo, J. Adrenal Gland Disorders. In Harrison’s Manual of Medicine, 20e; McGraw Hill: New York, NY, USA, 2020; Available online: https://accessmedicine.mhmedical.com/content.aspx?bookid=2738§ionid=227559717 (accessed on 25 October 2021).
- Read, J.; Perry, B.D.; Moskowitz, A.; Connolly, J. The contribution of early traumatic events to schizophrenia in some patients: A traumagenic neurodevelopmental model. Psychiatry 2001, 64, 319–345. [Google Scholar] [CrossRef]
- Reus, V.I. Depression and Depressive Disorders. In Harrison’s Principles of Internal Medicine, 20e; Jameson, J., Fauci, A.S., Kasper, D.L., Hauser, S.L., Longo, D.L., Loscalzo, J., Eds.; McGraw-Hill: New York, NY, USA, 2018; Available online: https://accessmedicine-1mhmedical-1com-1aqoxlrin0976.han.gumed.edu.pl/content.aspx?bookid=2129§ionid=251889537 (accessed on 18 June 2021).
- Chojnowska, S.; Ptaszyńska-Sarosiek, I.; Kępka, A.; Knaś, M.; Waszkiewicz, N. Salivary Biomarkers of Stress, Anxiety and Depression. J. Clin. Med. 2021, 10, 517. [Google Scholar] [CrossRef]
- Fiksdal, A.; Hanlin, L.; Kuras, Y.; Gianferante, D.; Chen, X.; Thoma, M.V.; Rohleder, N. Associations between symptoms of depression and anxiety and cortisol responses to and recovery from acute stress. Psychoneuroendocrinology 2019, 102, 44–52. [Google Scholar] [CrossRef]
- Powers, S.I.; Laurent, H.K.; Gunlicks-Stoessel, M.; Balaban, S.; Bent, E. Depression and anxiety predict sex-specific cortisol responses to interpersonal stress. Psychoneuroendocrinology 2016, 69, 172–179. [Google Scholar] [CrossRef]
- Høifødt, R.S.; Waterloo, K.; Wang, C.E.A.; Eisemann, M.; Figenschau, Y.; Halvorsen, M. Cortisol levels and cognitive profile in major depression: A comparison of currently and previously depressed patients. Psychoneuroendocrinology 2019, 99, 57–65. [Google Scholar] [CrossRef]
- Cherian, K.; Schatzberg, A.F.; Keller, J. HPA axis in psychotic major depression and schizophrenia spectrum disorders: Cortisol, clinical symptomatology, and cognition. Schizophr. Res. 2019, 213, 72–79. [Google Scholar] [CrossRef]
- Holland, J.M.; Schatzberg, A.F.; O’Hara, R.; Marquett, R.M.; Gallagher-Thompson, D. Pretreatment cortisol levels predict posttreatment outcomes among older adults with depression in cognitive behavioural therapy. Psychiatry Res. 2013, 210, 444–450. [Google Scholar] [CrossRef]
- Misiak, B.; Łoniewski, I.; Marlicz, W.; Frydecka, D.; Szulc, A.; Rudzki, L.; Samochowiec, J. The HPA axis dysregulation in severe mental illness: Can we shift the blame to gut microbiota? Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 102, 109951. [Google Scholar] [CrossRef] [PubMed]
- Jabben, N.; Nolen, W.A.; Smit, J.H.; Vreeburg, S.A.; Beekman, A.T.F.; Penninx, B.W.J.H. Co-occurring manic symptomatology influences HPA axis alterations in depression. J. Psych. Res. 2011, 45, 1208–1213. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.-C.; Chuang, S.-C.; Tseng, M.-C.M.; Chien, Y.-L.; Liao, S.-C.; Chen, H.-C.; Kuo, P.-H. Cortisol awakening response in patients with bipolar disorder during acute episodes and partial remission: A pilot study. Psychiatry Res. 2017, 258, 594–597. [Google Scholar] [CrossRef]
- Ellenbogen, M.A.; Hodgins, S.; Walker, C.-D. High levels of cortisol among adolescent offspring of parents with bipolar disorder: A pilot study. Psychoneuroendocrinology 2004, 29, 99–106. [Google Scholar] [CrossRef]
- Deshauer, D.; Duffy, A.; Meaney, M.; Sharma, S.; Grof, P. Salivary cortisol secretion in remitted bipolar patients and offspring of bipolar parents. Bipolar Disord. 2006, 8, 345–349. [Google Scholar] [CrossRef]
- Goodday, S.M.; Horrocks, J.; Keown-Stoneman, C.; Grof, P.; Duffy, A. Repeated salivary daytime cortisol and onset of mood episodes in offspring of bipolar parents. Int. J. Bipolar Disord. 2016, 4, 12. [Google Scholar] [CrossRef]
- Houtepen, L.C.; Boks, M.P.M.; Kahn, R.S.; Joëls, M.; Vinker, C.H. Antipsychotic use is associated with a blunted cortisol stress response: A study in euthymic bipolar disorder patients and their unaffected siblings. Eur. Neuropsychopharmacol. 2015, 25, 77–84. [Google Scholar] [CrossRef][Green Version]
- Kamali, M.; Saunders, E.F.H.; Prossin, A.R.; Brucksch, C.B.; Harrington, G.J.; Langenecker, S.A.; McInnis, M.G. Associations between suicide attempts and elevated bedtime salivary cortisol levels in bipolar disorder. J. Affect. Disord. 2012, 136, 350–358. [Google Scholar] [CrossRef]
- Keilp, J.G.; Stanley, B.H.; Beers, S.R.; Melhem, N.M.; Burke, A.K.; Cooper, T.B.; Oquendo, M.A.; Brent, D.A.; Mann, J.J. Further evidence of low baseline cortisol levels in suicide attempters. J. Affect. Disord. 2016, 190, 187–192. [Google Scholar] [CrossRef]
- Touskova, T.P.; Bob, P.; Pec, O.; Mishara, A.; Vanickova, Z.; Raboch, J.; Lysaker, P. Insight and cortisol responses in women with first episode psychosis. Schizophr. Res. 2018, 201, 428–429. [Google Scholar] [CrossRef]
- Walker, E.F.; Brennan, P.A.; Esterberg, M.; Brasfield, J.; Pearce, B.; Compton, M.T. Longitudinal changes in cortisol secretion and conversion to psychosis in at-risk youth. J. Abnorm. Psychol. 2010, 119, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Labad, J.; Stojanovic-Pérez, A.; Montalvo, I.; Solé, M.; Cabezas, A.; Ortega, L.; Moreno, I.; Vilella, E.; Martorell, L.; Reynolds, R.M.; et al. Stress biomarkers as predictors of transition to psychosis in at-risk mental states: Roles for cortisol, prolactin and albumin. J. Psych. Res. 2015, 60, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.L.; Malla, A.K. Much ado about much: Stress, dynamic biomarkers and HPA axis dysregulation along the trajectory to psychosis. Schizophr. Res. 2015, 162, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Chaumette, B.; Kebir, O.; Mam-Lam-Fook, C.; Morvan, Y.; Bourgin, J.; Godsil, B.P.; Plaze, M.; Gaillard, R.; Jay, T.M.; Krebs, M.O. Salivary cortisol in early psychosis: New findings and meta-analysis. Psychoneuroendocrinology 2016, 63, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Nordholm, D.; Rostrup, E.; Mondelli, V.; Randers, L.; Nielsen, M.Ø.; Wulff, S.; Nørbak-Emig, H.; Broberg, B.V.; Krakauer, K.; Dazzan, P.; et al. Multiple measures of HPA axis function in ultra high risk and first-episode schizophrenia patients. Psychoneuroendocrinology 2018, 92, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, C.M.; Smith, C.; McLaughlin, D.; Auther, A.; Malaspina, D.; Cornblatt, B. HPA axis function and symptoms in adolescents at clinical high risk for schizophrenia. Schizophr. Res. 2012, 135, 170–174. [Google Scholar] [CrossRef]
- Cullen, A.E.; Zunszain, P.A.; Dickson, H.; Roberts, R.E.; Fisher, H.L.; Pariante, C.M.; Laurens, K.R. Cortisol awakening response and diurnal cortisol among children at elevated risk for schizophrenia: Relationship to psychosocial stress and cognition. Psychoneuroendocrinology 2014, 46, 1–13. [Google Scholar] [CrossRef]
- Lange, C.; Huber, C.G.; Fröhlich, D.; Borgwardt, S.; Lang, U.E.; Walter, M. Modulation of HPA axis response to social stress in schizophrenia by childhood trauma. Psychoneuroendocrinology 2017, 82, 126–132. [Google Scholar] [CrossRef]
- Streit, F.; Memic, A.; Hasandedić, L.; Rietschel, L.; Frank, J.; Lang, M.; Witt, S.H.; Forstner, A.J.; Degenhardt, F.; Wüst, S.; et al. Perceived stress and hair cortisol: Differences in bipolar disorder and schizophrenia. Psychoneuroendocrinology 2016, 69, 26–34. [Google Scholar] [CrossRef]
- Duval, F.; Mokrani, M.-C.; Erb, A.; Danila, V.; Gonzalez Lopera, F.; Jeanjean, L. Dopaminergic, noradrenergic, adrenal, and thyroid abnormalities in psychotic and affective disorders. Front. Psychiatry 2020, 11, 533872. [Google Scholar] [CrossRef]
- Nater, U.M.; Bohus, M.; Abbruzzese, E.; Ditzen, B.; Gaab, J.; Kleindienst, N.; Ebner-Priemer, U.; Mauchnik, J.; Ehlert, U. Increased psychological and attenuated cortisol and alpha-amylase responses to acute psychosocial stress in female patients with borderline personality disorder. Psychoneuroendocrinology 2010, 35, 1565–1572. [Google Scholar] [CrossRef] [PubMed]
- Okugawa, G.; Omori, K.; Suzukawa, J.; Fujiseki, Y.; Kinoshita, T.; Inagaki, C. Long-term treatment with antidepressants increases glucocorticoid receptor binding and gene expression in cultured rat hippocampal neurones. Neuroendocrinology 1999, 11, 887–895. [Google Scholar] [CrossRef] [PubMed]
- Attenburrow, M.-J.; Mitter, P.R.; Whale, R.; Terao, T.; Cowen, P.J. Low-dose citalopram as a 5-HT neuroendocrine probe. Psychopharmacology 2001, 155, 323–326. [Google Scholar] [PubMed]
- Harmer, C.J.; Bhagwagar, Z.; Shelley, N.; Cowen, P.J. Contrasting effects of citalopram and reboxetine on waking salivary cortisol. Psychopharmacology 2003, 167, 112–114. [Google Scholar] [CrossRef]
- Daffner-Bugia, C.; Laakmann, G.; Voderholzer, U.; Haag, C.; Baghai, T.; Kolmsee, S.; Schroder, U.; Munz, T. The neuroendocrine effects of venlafaxine in healthy subjects. Hum. Psychopharmacol. 1996, 11, 1–9. [Google Scholar] [CrossRef]
- Hallam, K.T.; Begg, D.P.; Olver, J.S.; Norman, T.R. An investigation of the effect of immediate and extended release vanlafaxine on nocturnal malatonin and cortisol release in healthy adult volunteers. Hum. Psychopharmacol. Clin. Exp. 2008, 23, 129–137. [Google Scholar] [CrossRef]
- Jezova, D.; Duncko, R. Enhancement of stress-induced pituitary release and cardiovascular activity by antidepressant treatment in healthy men. J. Psychopharmacol. 2002, 16, 235–240. [Google Scholar] [CrossRef]
- Knorr, U.; Vinberg, M.; Gether, U.; Winkel, P.; Gluud, C.; Wetterslev, J.; Kessing, L.V. The effect of escitalopram versus placebo on perceived stress and salivary cortisol in healthy first-degree relatives of patients with depression—A randomised trial. Psychiatry Res. 2012, 200, 354–360. [Google Scholar] [CrossRef]
- Handley, R.; Mondelli, V.; Zelaya, F.; Marques, T.; Taylor, H.; Reinders, A.A.T.S.; Chaddock, C.; McQueen, G.; Hubbard, K.; Papadopoulos, A.; et al. Effects of antipsychotics on cortisol, interleukin-6 and hippocampal perfusion in healthy volunteers. Schizophr. Res. 2016, 174, 99–105. [Google Scholar] [CrossRef]
- Cohrs, S.; Röher, C.; Jordan, W.; Meier, A.; Huether, G.; Wuttke, W.; Rüther, E.; Rodenbeck, A. The atypical antipsychotics olanzapine and quetiapine, but not haloperidol, reduce ACTH and cortisol secretion in healthy subjects. Psychopharmacology 2006, 185, 11–18. [Google Scholar] [CrossRef]
- Rota, E.; Broda, R.; Cangemi, L.; Migliaretti, G.; Paccotti, P.; Rosso, C.; Torre, E.; Zeppegno, P.; Portaleone, P. Neuroendocrine (HPA axis) and clinical correlates during fluvoxamine and amitriptyline treatment. Psychiatry Res. 2005, 133, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Weber-Hamann, B.; Kratzsch, J.; Kopf, D.; Lederbogen, F.; Gilles, M.; Heuser, I.; Deuschle, M. Resistin and adiponectin in major depression: The association with free cortisol and effects of antidepressant treatment. J. Psychiatr. Res. 2007, 41, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Kunzel, H.; Ackl, N.; Hatzinger, M.; Held, K.; Holsboer-Trachsler, E.; Ising, M.; Kaschka, W.; Kasper, S.; Konstantinidis, A.; Sonntag, A.; et al. Outcome in delusional depression comparing trimipramine monotherapy with a combination of amitriptyline and haloperidol—A double-blind multicenter trial. J. Psychiatr. Res. 2009, 43, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Dziurkowska, E.; Wesolowski, M. Multivariate Statistical Analysis as a Supplementary Tool for Interpretation of Variations in Salivary Cortisol Level in Women with Major Depressive Disorder. Scientific. World J. 2015, 2015, 987435. [Google Scholar] [CrossRef]
- Aihara, M.; Ida, I.; Yuuki, N.; Oshima, A.; Kumano, H.; Takahashi, K.; Fukuda, M.; Oriuchi, N.; Endo, K.; Matsuda, H.; et al. HPA axis dysfunction in unmedicated major depressive disorder and its normalization by pharmacotherapy correlates with alteration of neural activity in prefrontal cortex and limbic/paralimbic regions. Psychiatry Res. 2007, 155, 245–256. [Google Scholar] [CrossRef]
- Manthey, L.; Leeds, C.; Giltay, E.J.; van Veen, T.; Vreeburg, S.A.; Penninx, B.W.; Zitman, F.G. Antidepressant use and salivary cortisol in depressive and anxiety disorders. Eur. Neuropsychopharmacol. 2011, 21, 691–699. [Google Scholar] [CrossRef]
- Nikisch, G.; Mathe, A.A.; Czernik, A.; Thiele, J.; Bohner, J.; Eap, C.B.; Agren, H.; Baumann, P. Long-term citalopram administration reduces responsiveness of HPA axis in patients with major depression: Relationship with S-citalopram concentrations in plasma and cerebrospinal fluid (CSF) and clinical response. Psychopharmacology 2005, 181, 751–760. [Google Scholar] [CrossRef]
- Navines, R.; Martin-Santos, R.; Gomez-Gil, E.; Martinez de Osaba, M.J.; Imaz, M.L.; Gasto, C. Effects of citalopram treatment on hypothermic and hormonal responses to the 5-HT1A receptor agonist buspirone in patients with major depression and therapeutic response. Psychoneuroendocrinology 2007, 32, 411–416. [Google Scholar] [CrossRef]
- Bschor, T.; Ising, M.; Erbe, S.; Winkelmann, P.; Ritter, D.; Uhr, M.; Lewitzka, U. Impact of citalopram on the HPA system. A study of the combined DEX/CRH test in 30 unipolar depressed patients. J. Psychiatr. Res. 2012, 46, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Papakostas, G.I.; Chuzi, S.E.; Sousa, J.L.; Fava, M. 5-HT1A-mediated stimulation of cortisol release in major depression: Use of non-invasive cortisol measurements to predict clinical response. Eur. Arch. Psychiatry Clin. Neurosci. 2010, 260, 175–180. [Google Scholar] [CrossRef]
- Lenze, E.J.; Dixon, D.; Mantella, R.C.; Dore, P.M.; Andreescu, C.; Reynolds, C.F., 3rd; Newcomer, J.W.; Butters, M.A. Treatment-related alteration of cortisol predicts change in neuropsychological function during acute treatment of late-life anxiety disorder. Int. J. Geriatr. Psychiatry 2012, 27, 454–462. [Google Scholar] [CrossRef]
- Ventura-Juncá, R.; Symon, A.; López, P.; Fiedler, J.L.; Rojas, G.; Heskia, C.; Lara, P.; Marín, F.; Guajardo, V.; Araya, A.V.; et al. Relationship of cortisol levels and genetic polymorphisms to antidepressant response to placebo and fluoxetine in patients with major depressive disorder: A prospective study. BMC Psychiatry 2014, 14, 220. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hinkelmann, K.; Moritz, S.; Botzenhardt, J.; Muhtz, C.; Wiedemann, K.; Kellner, M.; Otte, C. Changes in cortisol secretion during antidepressive treatment and cognitive improvement in patients with major depression: A longitudinal study. Psychoneuroendocrinology 2012, 37, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Dziurkowska, E.; Wesolowski, M.; Dziurkowski, M. Salivary cortisol in women with major depressive disorder under selective serotonin reuptake inhibitors therapy. Arch. Womens Ment. Health. 2013, 16, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.-T.; Hsiao, F.-H.; Wang, K.-C.; Ng, S.-M.; Ho, R.T.H.; Chan, C.L.W.; Lai, Y.-M.; Chen, Y.-T. The effect of psychotherapy added to pharmacotherapy on cortisol responses in outpatients with major depressive disorder. J. Nerv. Ment. Dis. 2009, 197, 401–406. [Google Scholar] [CrossRef]
- Ruhé, H.G.; Khoenkhoen, S.J.; Ottenhof, K.W.; Koeter, M.W.; Mocking, R.J.; Schene, A.H. Longitudinal effects of the SSRI paroxetine on salivary cortisol in Major Depressive Disorder. Psychoneuroendocrinology 2015, 52, 261–271. [Google Scholar] [CrossRef]
- Dziurkowska, E.; Wesolowski, M.; Dziurkowski, M. Changes of salivary cortisol level after venlafaxine treatment. Acta Pol. Pharm.-Drug Res. 2015, 72, 1279–1287. [Google Scholar]
- Araya, A.V.; Rojas, P.; Fritsch, R.; Rojas, R.; Herrera, L.; Rojas, G.; Gatica, H.; Silva, H.; Fiedler, J.L. Early response to venlafaxine antidepressant correlates with lower ACTH levels prior to pharmacological treatment. Endocrine 2006, 30, 289–297. [Google Scholar] [CrossRef]
- Römer, B.; Lewicka, S.; Kopf, D.; Lederbogen, F.; Hamann, B.; Gilles, M.; Schilling, C.; Onken, V.; Frankhauser, P.; Deuschle, M. Cortisol metabolism in depressed patients and healthy controls. Neuroendocrinology 2009, 90, 301–306. [Google Scholar]
- Laakmann, G.; Hennig, J.; Baghai, T.; Schüle, C. Influence of mirtazapine on salivary cortisol in depressed patients. Neuropsychobiology 2003, 47, 31–36. [Google Scholar] [CrossRef]
- Schüle, C.; Baghai, T.C.; Eser, D.; Schwarz, M.; Bondy, B.; Rupprecht, R. Effects of mirtazapine on dehydroepiandrosterone-sulfate and cortisol plasma concentrations in depressed patients. J. Psychiatr. Res. 2009, 43, 538–545. [Google Scholar] [CrossRef]
- Scharnholz, B.; Weber-Hamann, B.; Lederbogen, F.; Schilling, C.; Gilles, M.; Onken, V.; Frankhauser, P.; Kopf, D.; Deuschle, M. Antidepressant treatment with mirtazapine, but not venlafaxine, lowers cortisol concentrations in saliva: A randomised open trial. Psychiatry Res. 2010, 177, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Schüle, C.; Baghai, T.C.; Eser, D.; Zwanzger, P.; Jordan, M.; Buechs, R.; Rupprecht, R. Time course of hypothalamic-pituitary-adrenocortical axis activity during treatment with reboxetine and mirtazapine in depressed patients. Psychopharmacology 2006, 186, 601–611. [Google Scholar] [CrossRef] [PubMed]
- Mück-Šeler, D.; Pivac, N.; Sagud, M.; Jakovljević, M.; Mihaljević-Peles, A. The effects of paroxetine and tianeptine on peripheral biochemical markers in major depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 2002, 26, 1235–1243. [Google Scholar] [CrossRef]
- Sugranyes, G.; Thompson, J.L.; Corcoran, C.M. HPA-axis function, symptoms, and medication exposure in youths at clinical high risk for psychosis. J. Psychiatr. Res. 2012, 46, 1389–1393. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nothdurfter, C.; Schmotz, C.; Sarubin, N.; Baghai, T.C.; Laenger, A.; Lieb, M.; Bondy, B.; Rupprecht, R.; Schüle, C. Effects of escitalopram/quetiapine combination therapy versus escitalopram monotherapy on hypothalamic-pituitary-adrenal-axis activity in relation to antidepressant effectiveness. J. Psychiatr. Res. 2014, 52, 15–20. [Google Scholar] [CrossRef]
- Mondelli, V.; Dazzan, P.; Hepgul, N.; Di Forti, M.; Aas, M.; D’Albenzio, A.; Di Nicola, M.; Fisher, H.; Handley, R.; Marques, T.R.; et al. Abnormal cortisol levels during the day and cortisol awakening response in first-episode psychosis: The role of stress and of antipsychotic treatment. Schizophr. Res. 2010, 116, 234–242. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Zhou, D.F.; Cao, L.Y.; Wu, G.Y.; Shen, Y.C. Cortisol and cytokines in chronic and treatment-resistant patients with schizophrenia: Association with psychopathology and response to antipsychotics. Neuropsychopharmacology 2005, 30, 1532–1538. [Google Scholar] [CrossRef]
| The Patient’s Condition | Terms of Sampling | Cortisol Secretion | Additional Insights | Ref. |
|---|---|---|---|---|
| Undiagnosed depression | saliva/afternoon before and after TSST | ↑ | - | [11] |
| Depression | saliva/afternoon | ↑ | - | [13] |
| Anxiety disorders | ||||
| Depression in remission | saliva/morning, evening | N | cognitive decline | [14] |
| Depression | ↑ | |||
| Schizophrenia spectrum disorders | blood/afternoon | ↑ | cognitive decline, verbal memory decline | [15] |
| Psychotic major depression | ||||
| Elderly depressed | saliva/afternoon | ↑ | less responsive to cognitive behavioral therapy | [16] |
| Bipolar disorder | - | ↑ | increase in cortisol secretion associated with the manic phase | [17] review |
| Unipolar depression | saliva/CAR, evening | ↑ | elevated CAR | [18] |
| Bipolar disorder | ||||
| Bipolar disorder | saliva/CAR | ↑ | elevated CAR | [19] |
| Offspring of parents with bipolar disorder | saliva/CAR, bedtime | ↑ | HPA axis disorders as an early BD anomaly | [20] |
| Offspring of parents with bipolar disorder in remission | saliva/CAR, evening | N | HPA axis normalization in remission | [21,22] |
| Bipolar disorder in remission | saliva/afternoon | N | weaker response to TSST | [23] |
| Siblings of person with bipolar disorder in remission | N | no family risk of bipolar disorder | ||
| Suicide attempts in bipolar disorder | saliva/awakening, bedtime | ↑ | weaker response to stress after a suicide attempt | [24] |
| saliva/various times of day | [25] | |||
| People at risk of developing psychosis | saliva/3 times a day | ↑ | - | [27] |
| blood/morning saliva/CAR | [28] | |||
| First-episode psychosis | - | ↑ | cortisol–symptoms correlation only in the initial phase of psychosis | [29] review |
| saliva/morning | cortisol–symptoms correlation with positive symptoms | [30] | ||
| saliva/morning | cortisol–symptoms correlation with severe anxiety | [32] | ||
| saliva/CAR | - | [31] | ||
| Children at elevated risk for schizophrenia | saliva/CAR | ↑ | blunted CAR | [33] |
| First-episode schizophrenia | saliva/6 times after TSST | ↑ | blunted CAR | [34] |
| Borderline personality disorder | saliva/before and after TSST | ↑ | - | [37] |
| The Patient’s Condition | Pharmacological Intervention | Biological Matrix | Cortisol Secretion | Additional Insights | Ref. |
|---|---|---|---|---|---|
| Healthy volunteers | citalopram | blood | ↑ | increase in cortisol concentration proportional to the applied dose | [39] |
| saliva | [40] | ||||
| reboxetine | saliva | NI | - | [40] | |
| venlafaxine | blood | ↑ | increase in cortisol concentration proportional to the applied dose | [41] | |
| saliva | - | [42] | |||
| tianeptine | blood | ↑ | - | [43] | |
| escitalopram | saliva | ↓ | stressful situation | [44] | |
| haloperidol | saliva | ↓ | - | [45] | |
| aripiprazole | NI | ||||
| quetiapine/olanzapine | blood | ↓ | - | [46] | |
| Depression | amitriptyline | blood | ↓ | normalization occurs after a few weeks of therapy | [47,49] |
| saliva | [48,50] | ||||
| amitriptyline/fluvoxamine/mianserine | blood | ↓ | reduction of anomalies in the brain, in particular, in the limbic and paralimbic areas | [51] | |
| citalopram | blood | ↓ | reduction of cortisol concentration proportional to the administered dose | [53] | |
| blood | therapeutic effect proportional to the concentration of cortisol | [54] | |||
| blood | - | [55] | |||
| escitalopram | saliva | NI | - | [56] | |
| escitalopram | saliva | ↓ | improvement of immediate and delayed memory correlated with the concentration of cortisol | [57] | |
| SSRI | saliva | ↓ | effects visible in people with severe depression, late responders, or non-responders | [58,59,60] | |
| sertraline | saliva | ↓ | - | [61] | |
| paroxetine | saliva | ↓/NI | effects seen in late responders and non-responders/no effect on CAR | [62] | |
| venlafaxine | saliva | ↓ | - | [63] | |
| saliva | lack of full normalization of HPA axis functions | [64] | |||
| venlafaxine/mirtazapine | urine | ↓ | increasing the bioavailability of cortisol in tissues and activation of degrading enzymes | [65] | |
| mirtazapine | saliva | ↓ | - | [66] | |
| [68] | |||||
| blood | [67] | ||||
| mirtazapine | blood | ↓/↑ | decrease in cortisol level after the first week of treatment, slight increase after the fifth week of treatment | [69] | |
| reboxetine | ↓ | lowering cortisol levels in the fifth week of therapy | |||
| escitalopram, escitalopram + quetiapine | blood | ↓ | stronger reduction of the cortisol level in combination therapy | [72] | |
| People at risk of developing psychosis | antipsychotics | saliva | ↓ | - | [71] |
| SSRI | |||||
| First-episode psychosis | quetiapine/risperidone/aripiprazole/haloperidol/olanzapine | saliva | ↓ | blunted CAR in patients | [73] |
| Schizophrenia | risperidone/haloperidol | blood | ↓ | - | [74] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dziurkowska, E.; Wesolowski, M. Cortisol as a Biomarker of Mental Disorder Severity. J. Clin. Med. 2021, 10, 5204. https://doi.org/10.3390/jcm10215204
Dziurkowska E, Wesolowski M. Cortisol as a Biomarker of Mental Disorder Severity. Journal of Clinical Medicine. 2021; 10(21):5204. https://doi.org/10.3390/jcm10215204
Chicago/Turabian StyleDziurkowska, Ewelina, and Marek Wesolowski. 2021. "Cortisol as a Biomarker of Mental Disorder Severity" Journal of Clinical Medicine 10, no. 21: 5204. https://doi.org/10.3390/jcm10215204
APA StyleDziurkowska, E., & Wesolowski, M. (2021). Cortisol as a Biomarker of Mental Disorder Severity. Journal of Clinical Medicine, 10(21), 5204. https://doi.org/10.3390/jcm10215204






